Abstract
Background and Objectives:
Maricopa Medical Center (MMC) was found to have higher charges and length-of-stays than 16 other regional hospitals in an analysis of DRG categories for gallbladder disease. These comparative figures identified MMC as being inefficient and demanded review to determine the reasons for the inefficiencies.
Methods:
In an attempt to determine the reason for inefficiency of charges and length-of-stay for the laparoscopic portion of laparoscopic cholecystectomy, matched pairs of open cholecystectomy and converted laparoscopic cholecystectomy from a data base of 633 patients with cholecystectomies were reviewed. Thirty-five matches for age, sex and similar diagnosis were successful.
Results:
Matched pair evaluation disclosed a $6,880 difference in charges, which was attributed solely to the charge for laparoscopy. Subsequent chart analysis showed a high charge for instrumentation, prolonged anesthesia and operative times and longer preoperative delays before surgery. Moreover, no matter what the conversion rate is, open cholecystectomy was more cost effective. However, if there is a conversion rate of 5%, total hospital charges for laparoscopic cholecystectomy would have to be reduced to $12,679 (a reduction of $3,332 from $16,011) to make laparoscopic cholecystectomy cost-effective.
Conclusions:
Cost-effective decision tree analysis of matched pair comparisons and sensitivity analysis proves to be an effective technique in evaluating the cost-effectiveness of laparoscopic cholecystectomy in a hospital population.
Keywords: Laparoscopic cholecystectomy, Managed care contracts
INTRODUCTION
Approximately 20 million people (10-15% of the adult population) have gallstones and 1 million new patients are diagnosed with cholelithiasis every year. As a result, the treatment of cholelithiasis has become the most costly digestive disease, with an estimated annual cost of more than $5 billion.1,2
In September, 1992, the National Institute of Health convened a consensus development conference to discuss the treatment of cholelithiasis and laparoscopic cholecystectomy.1 After considerable discussion and review of the current literature, the panel concluded that laparoscopic cholecystectomy offered substantial advantages over the traditional open cholecystectomy with no apparent increase in morbidity or mortality. Because of the reduction in pain and disability, the conference concluded that treatment costs would be equal to or slightly less than the cost of open cholecystectomy and that there would be substantial savings to patients and society because of the shortened period of disability.
The disability and loss of income following standard open cholecystectomy further increase cost, but these items are generally not measured by traditional appraisal methods. This convalescent period and, consequently, costs have been greatly reduced by laparoscopic cholecystectomy. This example of cost analysis should be requested by business and possibly patients, as they are impacted the most.
Indeed, charges (not costs) for laparoscopic cholecystectomy often surpass those of open cholecystectomy. This is surprising because charges should reflect the costs resulting from increased length-of-stay (LOS), nursing and hospital support required by open cholecystectomy. The charges for equipment and other technical requirements for laparoscopic procedures probably explain the excess charges noted in laparoscopic cholecystectomies.
Surgeons at Maricopa Medical Center (MMC) identified excessive LOS and charges by comparing the cholecystectomy DRG (Diagnostic Related Group) 195 with 16 other hospitals in the region.3 Eleven of 20 cases (55%) were converted laparoscopic cholecystectomies. The remainder were either old patients with complications or young patients with advanced disease and complicated courses. Little could be done to reduce charges except to either lessen the conversion rates or costs for laparoscopic cholecystectomy.
In order to get a precise estimate of laparoscopic charges, match pair comparisons from the same data base of charges between open cholecystectomy and converted laparoscopic cholecystectomy were accomplished. Since the comparisons matched age, sex and similar diagnosis (ex.: acute vs. chronic cholecystitis, pancreatitis, etc.), many confounding variables could be eliminated. This suggested that the only reasons for the increased charges were the charges for laparoscopy. Other reasons for conversion, such as intraoperative complications, were eliminated because none of the matched pairs had serious complications or concomitant disease. Therefore, this comparison provided a relatively straightforward technique for statistical comparison to determine the charges for laparoscopy.
MATERIALS AND METHODS
A retrospective review of 70 cholecystectomy patients was conducted from a four-year data base of 633 patients who had undergone cholecystectomy. Thirty-five patients with converted laparoscopic cholecystectomies and thirty-five patients with open cholecystectomies were selected from the data by matching for age, sex and similar diagnosis. A paired sample t-test was used for statistical analysis with significance at the p=0.05 level. Decision tree and sensitivity analyses were then used to choose the most cost-effective operation and then determine what the limitation of charges would be needed to make laparoscopic cholecystectomy cost-effective.
RESULTS
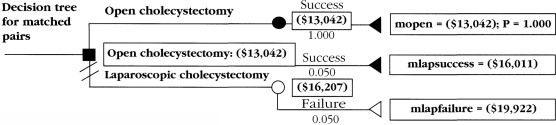
Twelve males and 58 females matched successfully. The average age was 37 years (range = 15-70 years) (standard deviation [sd] = 15.9). The average charge for converted laparoscopic cholecystectomies was $19,922 (sd = $7,134), and that of open cholecystectomies, $13,042 (sd = $9,715) (p=<0.01). The amount attributed to laparoscopy was $6,880 ($19,922 - $13,042). Decision tree analysis showed that, regardless of the rate of conversion, open cholecystectomy was more cost-effective. However, if charges could be reduced to certain levels, depending on the conversion rate, laparoscopic cholecystectomy would become cost-effective.
DISCUSSION
Steiner reviewed surgical rates and operative mortality for open and laparoscopic cholecystectomy in Maryland and found the overall mortality rate had been reduced by 33%. However, the total number of cholecystectomy-related deaths had not fallen because of a 28% increase in the rate of cholecystectomies.4 This study and the NIH Consensus Conference support the value of laparoscopic cholecystectomy.
Now that the technique has proven to be beneficial, the current challenge to all health providers is to improve these results by further reducing mortality and morbidity, while improving cost-efficiency. To achieve this, databases for cholecystectomies must be studied to determine which aspects of the preoperative evaluation, surgery and postoperative treatment could be modified to achieve these goals. This paper attempts to address these goals with studying the charges for open, laparoscopic and converted laparoscopic cholecystectomy by evaluating matched pairs of patients in a large data set.
Matched-pair comparisons of open and converted laparoscopic cholecystectomy provide a simple method of determining the true charges for laparoscopic cholecystectomy (including increased operative time, anesthesia time, cholangiograms, instruments, etc.). With similar length-of-stay (LOS), and averaging the charges over a large number of matched pairs, the main independent variable remaining is that of the charge for the laparoscopy.
In this comparative series, that charge equaled $6,880 ($19,922 - $13,042). Reduction of this charge by applying reusable instruments and having surgeons with advanced laparoscopic skills operate on patients that have a higher probability of conversion would make laparoscopic cholecystectomy more cost-effective.
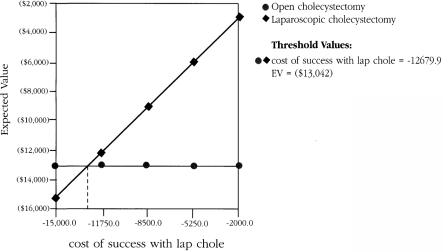
Consider that the average charge for laparoscopic cholecystectomy in the 633 patients equaled $16,011 and the average charge for open cholecystectomy was $13,042. A decision-tree analysis of these values shows that managed-care contractors would prefer open cholecystectomy for all patients with cholecystitis at MMC (Figure 1). However, most patients would not enroll in a health plan or go to a hospital which did not provide laparoscopic cholecystectomy, so an evaluation of what could be done to reduce the charges for laparoscopic cholecystectomy must be done to make laparoscopic cholecystectomy attractive to the buyer. The most important question is, "How much of a reduction in charge (cost) would be necessary to make laparoscopic cholecystectomy cost-efficient?" This depends not only on a reduction in charges but on the percentage of conversions (because of the high cost of conversions). Sensitivity analysis of these data shows that if the conversion rate equals 5%, a charge of < $12,679.90 would be needed to make laparoscopic cholecystectomy cost-effective (Figure 2). Therefore, a $3,331 ($16,011 - $12,680) reduction in the charge of laparoscopic cholecystectomy would be needed before all patients could be considered for laparoscopic cholecystectomy.
Figure 1.
Decision tree for 5% conversion rate.
Figure 2.
Sensitivity analysis for conversion rates of 5%.
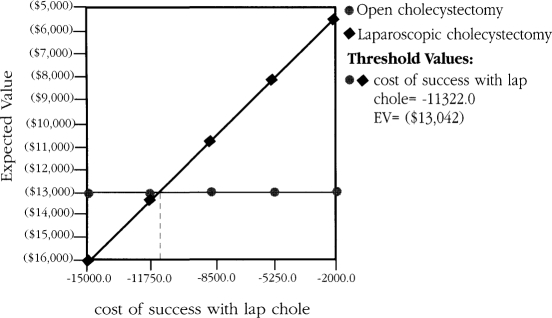
If the conversion rate equals 20%, then a charge of < $11,322 would be necessary to develop cost-efficiency (Figure 3). Therefore, a $4,689 ($16,011 - $11,322) reduction would be needed to consider all patients for laparoscopic cholecystectomy. Therefore, the greater the amount of reduction needed, the less likely efficiency can be achieved by reducing laparoscopic cholecystectomy charges.
Figure 3.
Sensitivity analysis for conversion rates of 20%.
Vanek and Borguet reviewed the cost of laparoscopic versus open cholecystectomy in a community hospital.5 They demonstrated that conversion from laparoscopic to open cholecystectomy resulted in a 57% increase in total charges over laparoscopic cholecystectomy. They suggested that this is due to the increase in hospital LOS of 4.7 days. They further demonstrated a charge for open cholecystectomy of $8,160 versus $10,210 (p<0.001) for laparoscopic cholecystectomy. Furthermore, the mean total hospital charge for converted laparoscopic cholecystectomies was $16,070. Given the literature average of return to work of 8.4 days for laparoscopic cholecystectomy and 27.5 days for open cholecystectomy, a savings of $2,483 accrues with the selection of laparoscopic cholecystectomy.
Comparative analysis is difficult because many of these studies include all cholecystectomy categories while other studies were limited to elective laparoscopic cholecystectomy patients. Furthermore, these studies reflect marked geographical and socioeconomic factors as well as severity of disease mixes. It therefore becomes advisable that health care payers evaluate charge data for each of the regional hospitals before contracting with them for medical services.
Since laparoscopic cholecystectomy is demanded by most patients, knowledge based on laparoscopic charges and conversion rates give the hospital or health care provider information to use in evaluating surgical costs. Lower costs give health care providers more flexibility in negotiating lower charges. Obviously, the lower the charge, all else being equal, the more likely the contract.
CONCLUSIONS
The charges of laparoscopic cholecystectomy are variable among institutions. These differences occur both regionally and locally. Health care providers, including HMOs, are looking for the most cost-effective provider and institutions which wish to compete must evaluate their procedures to inform health care providers that they are cost-efficient. Matched-pair analysis, decision-tree and sensitivity analyses, similar to those described above, facilitate appraisal by each institution as to what can be done to improve care, reduce charges and become cost-efficient in performing laparoscopic cholecystectomy. Laparoscopic cholecystectomy clearly offers several benefits over open cholecystectomy. Since there is reduced LOS and short-term dis-ability, hospital charges should not be in excess of that for open cholecystectomy. Only evaluation and modification of the charges which contribute to the excess will lead to validated cost efficiencies and subsequent recruitment by providers for hospital service.
References:
- 1. Anonymous. National Institutes of Health consensus development conference statement on gallstones and laparoscopic cholecystectomy. Amer J Surg. 1993; l65: 390–398 [DOI] [PubMed] [Google Scholar]
- 2. Zuker KA. Surgical laparoscopy. St Louis: Quality Medical Publishing, Inc, 1991: 115–200 [Google Scholar]
- 3. Weiland DE, Malone JM, Garren R, Bay RC. Is academic managed care an oxymoron? Amer J Surg. 1995; 170: 651–655 [DOI] [PubMed] [Google Scholar]
- 4. Steiner CA, Bass EB, Talmina MA, et al. Surgical rates and operative mortality for open and laparoscopic cholecystectomy in Maryland. N Eng J Med. 1994; 300(6):403–408 [DOI] [PubMed] [Google Scholar]
- 5. Vanek VW, Bourgeut CC. The cost of laparoscopic versus open cholecystectomy in a community hospital. Surg Endo. 1995; 9: 3l4–323 [DOI] [PubMed] [Google Scholar]