Abstract
Background:
Intraoperative ultrasound has been used extensively during open surgery to assess bowel viability, to identify vascular structures, and to assess for congenital abnormalities. The extension of this technology in laparoscopic procedures has been hampered by the size of the equipment and the significant learning curve that accompanies its use.
Methods:
Using a readily available Parks Inst. Co. Doppler Probe (8.1 MHz) and a 15-inch section of thick-walled, 9.5-mm OD Stainless Steel tubing, a Laparoscopic Doppler Probe was constructed. The parts were separately gas-sterilized, and a small segment of Penrose drain was used to create an airtight seal. The probe was passed through a 10-mm port, allowing assessment of vascular structures.
Results:
Two Laparoscopic Doppler Probes were available for evaluation during a 1-month period at our hospital. Surgeons were then surveyed at the end of the 1-month period as to the utility of the devices.
Conclusions:
The Laparoscopic Doppler probe was used to identify the cystic artery during gallbladder dissection, to assess mesenteric blood vessels during laparoscopic colectomy, and to identify femoral vessels during laparoscopic preperitoneal hernia repair. It was found to be quick to construct, easy to use, and provided useful information to the operating surgeon.
Keywords: Laparoscopic Doppler Probe, Doppler ultrasound, Vascular identification, Laparoscopic Ultrasound
INTRODUCTION
One of the key tools for the operating surgeon is the sense of touch. Through that, the surgeon is often able to determine inflammation and induration, create dissection planes, and identify vascular structures. When vascularity is in question, intraoperative Doppler examination has historically been used. The circumstances are wide ranging from the assessment of bowel viability in preparation for a bowel resection and reanastomosis to assessing patency after vascular reconstruction, from identifying arterial blood vessels to detecting stenoses or other abnormalities. Extension of this technology to laparoscopic surgery is a logical step, particularly in view of the lack of tactile sensation available during laparoscopy. Laparoscopic ultrasound has been used in the detection and staging of abdominal malignancies,1–3 identification of common bile duct stones,4 and in the prevention of injuries during laparoscopic cholecystectomy.5–8 Most reports, however, comment on the significant learning curve associated with the technique and use of the equipment. What is needed is a simple method to apply laparoscopically, what the general surgeon is comfortable performing during open surgery.
MATERIALS AND METHODS
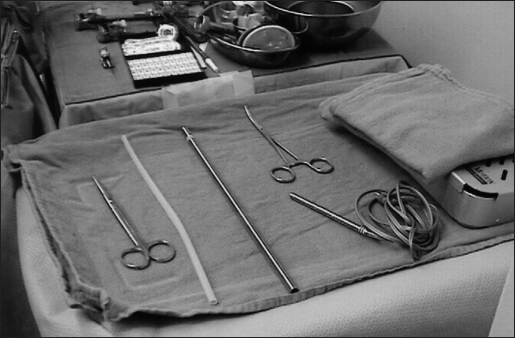
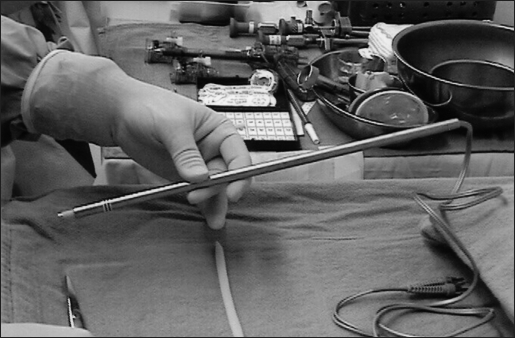
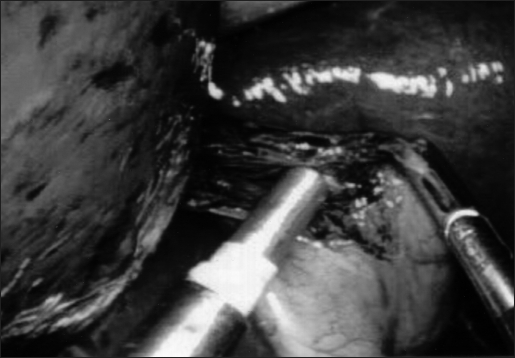
Using a readily available Parks Inst. Co. Doppler probe (8.1 MHz) and a 15-inch section of thick-walled, 9.5-mm OD Stainless Steel tubing, a Laparoscopic Doppler Probe (LDP) was constructed. The parts were separately gas-sterilized, and a small segment of Penrose drain was used to create an airtight seal (Figure 1). The probe was constructed in the first few minutes of the operative cases by the first assistant, while the primary surgeons were scrubbing (Figure 2). The LDP thus constructed was passed through a 10-mm port, allowing positive identification and assessment of vascular structures (Figure 3).
Figure 1.
All the materials necessary for construction of the Laparoscopic Doppler Probe.
Figure 2.
The constructed Laparoscopic Doppler Probe.
Figure 3.
Laparoscopic Doppler being used to identify cystic artery in difficult Triangle of Calot dissection.
RESULTS
The Laparoscopic Doppler Probe was used during a 1-month trial period at our institution. The probe was used to identify liver hemangiomas, iliac vessels during pelvic dissection, and mesenteric vessels during hemi-colectomies. Surgeons using the probe were surveyed, and all agreed that the probe was simple to use and added valuable information to their dissections.
DISCUSSION
Ultrasound is a valuable intraoperative tool for the general surgeon. Laparoscopic ultrasound has found utility in identifying tumors and assessing vascular structures. Its use in preventing complications during laparoscopic cholecystectomy has been extensively studied. Until just recently, however, its widespread application has been somewhat limited because of the size of the probe, the size of the ultrasound machinery, and the lack of, until recently, an “end-on-probe.” Similarly, the unfamiliarity of ultrasound to general surgeons has created a significant learning curve when ultrasound is being applied, not to mention being applied in a laparoscopic fashion. What is needed is a convenient, simple, cost-effective way to get some of the advantages that ultrasound offers at the disposal of the laparoscopic surgeon.
The LDP fits that need. The LDP described herein can be easily made during a laparoscopic procedure on a back table with low-cost materials just before the procedure begins, or any time during the procedure that a Doppler may be of use. It provides useful information on the location of vascular structures as in during a laparoscopic colectomy where identification of the inferior mesenteric vessels is readily accomplished and eliminates any misunderstanding of the vascular anatomy. It has also been used by our surgeons in preperitoneal hernia dissection where both the femoral artery and vein are identified relatively simply by compressing the overlying soft tissues onto the vasculature. The LDP may also provide information on the patency and flow characteristics of vascular anastomoses as laparoscopic techniques evolve to include more vascular procedures.
The LDP was originally constructed to identify a hemangioma on the surface of the liver during a routine laparoscopic cholecystectomy by using a Penrose drain to create an airtight seal and the delivery portion of an endoscopic retrieval bag as the delivery “tube.” Since its inception, the LDP has been applied to a variety of general surgical procedures by a number of surgeons at our institution. During the 1-month trial period, it was used to positively identify the cystic artery during gallbladder dissection, the mesenteric blood vessels during laparoscopic colectomy, and the femoral vessels during laparoscopic hernia repair. It was found to be quick to construct, easy to use, and provided useful information to the operating surgeon. It is now available for routine use by any surgeon at our institution.
To our knowledge, only 2 reports8, 9 of similar devices being used have been published. The first device, the Endoscopic Pulse Detector, was designed to aid the surgeon in identifying the cystic artery during dissection in the triangle of Calot.8 No erroneous assessments were made, and Glavic et al8 found the device safe, reliable, and easy to use. We agree with their conclusions that an instrument to identify vascular structures during laparoscopic surgery should be part of the standard instrumentation of an advanced laparoscopic tray; however, we do not see the need to reinvent the wheel with an Endoscopic Pulse Detector. The second report,9 concerns the use of a Smart Needle—a Doppler flow transducer used to identify the testicular artery during laparoscopic varicocelectomy. These authors sought to preserve the testicular artery and ligate only the testicular vein; they therefore used ultrasound assessment to achieve that goal. While we applaud their procedure, again, we do not feel that new equipment is necessary to be developed or purchased. The LDP is simply the extrapolation of a device used in open surgery, applied to laparoscopy, through an inexpensive delivery system. It can be placed through a 10-mm port and will likely become one of the cheapest instruments used during laparoscopic surgery.
CONCLUSION
The LDP can be easily constructed from readily available materials at low cost. Further, the LDP can be utilized to identify vascular structures and provide valuable information to the laparoscopic surgeon. With experience, multiple other applications are sure to suggest themselves.
Acknowledgments:
We wish to acknowledge the Department of Surgery, the Operating Room staff, and the Minimally Invasive Learning Center at St. Peter's University Hospital for their assistance in completion of this project.
Footnotes
Disclosure: The authors have no commercial interest in any of the equipment or instrument manufacturers mentioned in this article.
Contributor Information
Marc Neff, Department of Surgery and Minimally Invasive Learning Center, St. Peter's University Hospital, New Brunswick, NJ, USA..
Brian Cantor, Department of Surgery and Minimally Invasive Learning Center, St. Peter's University Hospital, New Brunswick, NJ, USA..
James Koren, Department of Surgery and Minimally Invasive Learning Center, St. Peter's University Hospital, New Brunswick, NJ, USA..
W. Peter Geis, Department of Surgery and Minimally Invasive Learning Center, St. Peter's University Hospital, New Brunswick, NJ, USA..
Steven Curtiss, Department of Surgery, St. Peter's University Hospital, New Brunswick, NJ, USA..
Scott Rosen, Department of Surgery, St. Peter's University Hospital, New Brunswick, NJ, USA..
Stephen Konigsberg, Department of Surgery, St. Peter's University Hospital, New Brunswick, NJ, USA..
References:
- 1. John TG, Greig JD, Carter DC, et al. Carcinoma of the pancreatic head and periampullary region. Tumor staging with laparoscopy and laparoscopic ultrasonography. Ann Surg. 1995:221:156–164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hartley JE, Kumar H, Drew PJ, et al. Laparoscopic ultrasound for the detection of hepatic metastases during laparoscopic colorectal cancer surgery. Dis Colon Rectum. 2000;43(3):320–324 [DOI] [PubMed] [Google Scholar]
- 3. Tsioulias GJ, Wood TF, Chung MH, Morton DL, Bilchik A. Diagnostic laparoscopy and laparoscopic ultrasonography optimize the staging and resectability of intraabdominal neoplasms. Surg Endosc. 2001;15(9):1016–1019 [DOI] [PubMed] [Google Scholar]
- 4. Catheline J, Rizk N, Champault G. A comparison of laparoscopic ultrasound versus cholangiography in the evaluation of the biliary tree during laparoscopic cholecystectomy. Eur J Ultrasound. 1999;10(1):1–9 [DOI] [PubMed] [Google Scholar]
- 5. Tomonaga T, Filipi CJ, Lowham A, Martinez T. Laparoscopic intracorporeal ultrasound cystic duct length measurement: a new technique to prevent common bile duct injuries. Surg Endosc. 1999;13(2):183–185 [DOI] [PubMed] [Google Scholar]
- 6. Birth M, Lossin P, Brugmans F, Weiser HF. Vascular injuries within the hepatoduodenal ligament: recognition by laparoscopic color Doppler ultrasound. Surg Endosc. 2000;14(3):246–249 [DOI] [PubMed] [Google Scholar]
- 7. Machi J, Oishi AJ, Uchida S, Furumoto NL, Oishi RH. Simple laparoscopic ultrasound technique for prevention of bile duct injuries. J Laparoendosc Adv Surg Tech A. 2000;10(3):165–168 [DOI] [PubMed] [Google Scholar]
- 8. Glavic Z, Begie L, Rozman R. A new device for the detection and recognition of blood vessels in laparoscopic surgery. Surg Endosc. 2002;16:1197–1200 [DOI] [PubMed] [Google Scholar]
- 9. Cohen RC. Laparoscopic varicocelectomy with preservation of the testicular artery in adolescents. J Pediatr Surg. 2001;36(2):394–396 [DOI] [PubMed] [Google Scholar]