Abstract
Objective:
The purpose of this study was to demonstrate a minimally invasive, novel variation, microlaparoscopic-assisted vaginal hysterectomy (MAVH) of a previously established technique, laparoscopic-assisted vaginal hysterectomy (LAVH), in the morbidly obese patient.
Methods:
This was a prospective, descriptive feasibility study (Canadian Task Force classification 11-2) conducted at a university-affiliated hospital and private community hospital. Seven morbidly obese women with an average body mass index of 45.8 kg/m2 (range, 40.6 to 51.5) underwent microlaparoscopic-assisted vaginal hysterectomy (MAVH). Microlaparoscopic-assisted vaginal hysterectomy (MAVH), classified as Type 1B, including unilateral or bilateral occlusion and division of the ovarian artery(ies), either medial or lateral to the ovary(ies), with or without dissection of the adjacent broad ligament under microlaparoscopic guidance, in addition to incision of the vesicouterine peritoneum.
Results:
The median duration of surgery was 109.1 minutes (range, 86 to 134), median blood loss was 207 mL (range, 100 to 350), and average length of stay in the hospital was 33.7 hours (range, 23 to 48). The complication rate was 0%.
Conclusion:
Microlaparoscopic-assisted vaginal hysterectomy (MAVH) is a safe and effective, more minimally invasive method of performing laparoscopic hysterectomies in select morbidly obese patients.
Keywords: Microlaparoscopy, Morbid obesity, Hysterectomy, Minimally invasive surgery
INTRODUCTION
Morbid obesity is associated with significant surgical morbidity. The morbidly obese patient in need of a hysterectomy manifests significant challenges for the laparoendoscopic surgeon. Special considerations are necessary for this group of high-risk patients undergoing a laparoscopic hysterectomy. Laparoscopic risks include herniation of the trocar site, hemorrhage, wound infections, and conversion to laparotomy.
Laparoscopic techniques for facilitating hysterectomies are continuing to evolve. Recent refinements in surgical technique and instrumentation have focused attention on minimally invasive microlaparoscopic surgery.1–3 Through the use of 2-mm trocars as the primary trocar through the umbilicus as well as the secondary lateral trocars, morbidly obese patients can benefit from the advantages of minimally invasive surgery. The potential for decreased wound morbidity from the smaller incisions is significant. A new minimally invasive approach for performing laparoscopic-assisted vaginal hysterectomy in the morbidly obese patient by using microlaparoscopy is presented.
METHODS
Between August 2001 and January 2003, 7 morbidly obese women (median age, 36.9 years, range, 28 to 47; median weight, 121.2 kg, range 100.4 to 131; median body mass index (BMI) 45.8 kg/m2, range 40.6 to 51.5) requiring a hysterectomy underwent a microlaparoscopic-assisted vaginal hysterectomy (MAVH) at a university-affiliated hospital or private community hospital. BMI was calculated as weight in kilograms divided by height in meters2. Selected patients had a component of chronic pelvic pain, or requested removal of their adnexa, or both, after appropriate counseling. Table 1 summarizes the preoperative indications for the hysterectomy. Contraindications for the use of this technique included patients with endometrial, ovarian, and cervical cancer, those with stage IV endometriosis, greater than a 14-week size uterus, or a pelvic mass that could not be removed intact through a culdotomy incision. All patients had failed medical treatment, one or more conservative surgical procedures including dilatation and curettage, hysteroscopy, and laparoscopy, or all of these.
Table 1.
Indications for Microlaparoscopic-assisted Vaginal Hysterectomy (MAVH)
| Indication | Number of Patients |
|---|---|
| Myoma | 4 |
| Menorrhagia | 7 |
| Endometriosis | 1 |
| Chronic pelvic pain | 5 |
| Suspected adhesions | 1 |
| Difficult uterine descent | 2 |
Operative Procedure
A preoperative bowel prep is recommended to improve visualization of the pelvis by decompressing the bowel and to decrease morbidity in the event of bowel injury. A prophylactic antibiotic is administered intravenously. After undergoing general anesthesia with endotracheal intubation, the patient is positioned in the dorsal lithotomy position using candy-cane stirrups to obtain better hip flexion. Examination is preformed with the patient anesthetized. The patient is then prepared and draped, and a Foley catheter inserted. A uterine manipulator is inserted in-utero. With the angle of the operating table at 0°, the umbilicus is incised by using a number 11 scalpel blade. After elevating the abdominal skin, an interlocking 2-mm trocar and a Veress needle are introduced transumbilically into the abdominal cavity at a 90° angle from the horizontal. Patency is confirmed using the saline drop test and a pneumoperitoneum is established with high-flow CO2 insufflation, up to 15 liters per minute. After creating the pneumoperitoneum, a 2-mm microlaparoscope is inserted. The patient is then placed in a steep Trendelenburg position. Under direct visualization, a second 2-mm trocar is inserted lateral to the left rectus abdominis muscle at the level of the umbilicus. The microlaparoscope is then inserted into this lateral trocar. The first 2-mm trocar is then removed from the umbilicus and inserted lateral to the right rectus abdominis muscle at the level of the umbilicus. Since the initial umbilical incision was small to accommodate the 2-mm trocar only, pneumoperitoneum should not be lost. Once both lateral 2-mm trocars are in place, the umbilical incision is extended elliptically within the umbilicus and a 5- to 12-mm trocar (depending on the surgeon's preference for using bipolar desiccation, Harmonic scalpel, or stapling device) is inserted. Figure 1 details the trocar placements. A fourth suprapubic trocar is not necessary with this technique. The pelvic anatomy is then carefully inspected. Any adhesions can be lysed and peritoneal endometriosis implants excised. The assistant inserts the microlaparoscope into the right 2-mm port and is responsible for elevating the uterus as necessary via the uterine manipulator. The surgeon introduces a 2-mm grasper into the left port for grasping the adnexa and manipulating any pelvic structures. If one or both adnexa are to be removed, the ovarian artery pedicles, the infundibulopelvic ligament or pedicle including the fallopian tube, the round ligament, and the ovarian artery is occluded and divided using a stapling device (or instrument of choice) introduced through the umbilical trocar. Once the pedicles are divided, the vesicouterine peritoneum is grasped with the 2-mm grasper and incised using scissors introduced through the umbilical port. Occlusion and division of the uterine arteries is accomplished vaginally. Removal of the uterus is performed vaginally. Following closure of the vaginal cuff, pneumoperitoneum is created and the microlaparoscope reinserted. The pelvis is irrigated and inspected to assure hemostasis. Following release of the CO2 with the patient in the Trendelenburg position, both of the lateral 2-mm trocar sites are closed with a Steri-Strip. The larger umbilical trocar site is closed with a 1-0 Vicryl fascial suture, and the skin with a subcuticular stitch of 4-0 Vicryl. Postoperatively, patients receive intravenous narcotic pain medication with a meperidine patient-controlled analgesia pump.
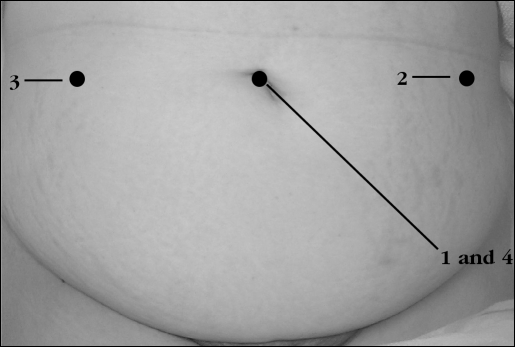
Figure 1.
Primary 2-mm trocars and secondary umbilicus trocar placement sites for microlaparoscopic assisted vaginal hysterectomy (MAVH). Primary 2-mm umbilicus trocar (1). Left lateral rectus abdominis 2-mm trocar (2). Right lateral rectus abdominis 2-mm trocar (3). Secondary umbilicus 5-mm to 12-mm trocar (4).
RESULTS
All 7 women had their procedures performed with a 2-mm microlaparoscope. The use of a larger laparoscope was not necessary. None of the patients had complications or required conversion to a laparotomy; and no patient returned to the operating room for reexploration, blood transfusions, or hospital readmission within 6 weeks following surgery. Pathologic findings are presented in Table 2. Four patients were discharged within 23 hours; the remaining 3 were discharged at 48 hours. Overall average length of stay was 33.7 hours (range, 23 to 48). Average uterine weight was 141.4 g (range, 96 to 362). Median blood loss was 207.1 mL (range, 100 to 350). The mean duration of surgery was 109.1 minutes (range, 86 to 134).
Table 2.
Summary of Pathologic Findings
| Finding | Number of Patients |
|---|---|
| Myomas | 4 |
| Endometriosis | 2 |
| Adenomyosis | 1 |
| Adhesions | 2 |
| Ovarian cyst | 2 |
DISCUSSION
Morbid obesity is the most common chronic disease in the Western world.4 It is diagnosed when the BMI, which correlates to adipose deposition, is ≥40%. In this high-risk population, the hysterectomy technique must be weighed against individual surgical skills, available instrumentation, potential risks to the patient, and postoperative recovery. Major laparoscopic risks include herniation of the trocar site, hemorrhage, wound infections, and conversion to laparotomy. The indications for hysterectomy for morbidly obese patients are similar to those for patients who are not obese.
In 1989, Reich and coworkers first described laparoscopic hysterectomy.5 Variations of their technique have resulted in multiple approaches to the procedure, giving rise to a classification system for laparoscopic hysterectomy.6 In selected cases, microlaparoscopic-assisted vaginal hysterectomy (MAVH)7 offers morbidly obese patients in need of a hysterectomy the advantages of minimally invasive surgery. Benefits of minimally invasive surgery include decreased morbidity, shorter hospital stays, and quicker recovery. Insertion of the primary and secondary trocars is the most critical aspect of laparoscopy, and most injuries occur during this part of the procedure. Trocar placement and incision closure may present problems in morbidly obese patients. Although a 45° caudad angle is preferred with the initial Veress needle and trocar placement in a thin patient, a 90° angle is usually required to enter the peritoneal cavity in the morbidly obese patient. In these patients, the umbilicus is generally well below the aortic bifurcation thus decreasing the risk for injury during vertical cannula entry.8 Fascial closure of the lateral trocar incisions may be difficult in a morbidly obese patient. This significantly increases the risk for wound morbidity since the 7-mm or larger trocars are commonly used at the lateral trocar sites, and herniation of the omentum or small bowel can occur. Incisional hernia risk is increased with the use of 12-mm trocars in the lateral sites.9 Using this technique, the lateral 2-mm trocar sites can be closed with Steri-Strips, further decreasing operating time.
Because of advances in technique and instrumentation, microlaparoscopy continues to infiltrate laparoscopic procedures traditionally done with larger endoscopic instruments.10 Microlaparoscopy refers to the use of small-diameter laparoscopes (<2 mm in diameter) that are made of microfiberoptic bundles measured in micrometers.11 Operative microlaparoscopic-assisted procedures utilize at least 1 larger trocar to accommodate large laparoscopic instruments such as stapling devices and for the removal of surgical specimens, ie, the ovary, appendix, or gallbladder.12 The incorporation of 2-mm microinstrumentation, when possible, makes the procedures more minimally invasive. The 2-mm lateral trocar sites do not require suturing, and the incisional hernia risk seen with the use of larger trocars is absent. Inferior epigastric vessel injury is the most common complication cited with LAVH.13 The small diameter of the 2-mm trocars makes their placement rapid and very precise, thus decreasing the risk for such injury. In addition, bowel perforations resulting from 2-mm instrumentation can be managed conservatively without suturing if the site of injury is not actively leaking stool or bleeding.14
Selection of the umbilical trocar size (5 mm to 12 mm) is dependent primarily on the surgeon's preference. I prefer to use the expandable 12-mm trocar because the laparoscopic stapling device with the articulating head facilitates angle placement over the adnexa in the morbidly obese patient.
It should be emphasized that patient selection is very important because laparoscopic hysterectomies are not indicated in situations where a vaginal hysterectomy alone can accomplish the preoperative goal of the procedure. Indications for microlaparoscopic-assisted vaginal hysterectomy (MAVH) primarily involve cases in which there is difficulty in performing adnexectomy by the vaginal approach, cases requiring pelvic and abdominal adhesiolysis, difficult uterine descent cases, cases in which myomas are less than 14-week size, cases in which there has been a previous Cesarean delivery, and cases in which there would be excision of endometriosis less than Stage IV.
The average operating time for an LAVH has been reported to be 115 minutes,15 compared with 109.1 minutes in the current MAVH study that included only morbidly obese patients. Possible factors contributing to this decrease may be a direct result of this miniaturized technology. First, using the interlocking 2-mm trocar and Veress needle for creation of the pneumoperitoneum precludes the necessity of a “second-pass” trocar placement and allows the immediate insertion of the microlaparoscope. A second reason for the decreased operating time is that the 2-mm trocar sites do not require suturing at the conclusion of the surgical procedure.
In this study, length of hospital stay was short. Average hospitalization was 33.7 hours. Postoperative pain management was achieved with the use of a meperidine patient-controlled analgesia pump. No patient required being seen in the office prior to their scheduled 1-week postoperative visit. Following the 6-week follow-up visit, all patients were able to resume their activities without limitations. I do not feel that this technique requires much of an additional learning curve for the laparoendoscopic surgeon already performing LAVH. MAVH can also be performed in the thin patient, offering excellent cosmetic results. The greatest challenge will be getting accustomed to using the smaller diameter microlaparoscope and microinstrumentation. As a result of the positive outcomes in this study, selected morbidly obese patients who are candidates for LAVH may be able to have their procedures performed in a more minimally invasive manner with MAVH.
Footnotes
Presented at the 12th International Congress and Endo Expo 2003, SLS Annual Meeting, Las Vegas, Nevada, USA, September 22-25, 2003.
References:
- 1. Palter SF. Microlaparoscopy under local anesthesia and conscious pain mapping for the diagnosis and management of pelvic pain. Curr Opinion Obstet Gynecol. 1999;11:387–393 [DOI] [PubMed] [Google Scholar]
- 2. Almeida OD, Jr, Val-Gallas JM, Rizk B. Appendectomy under local anaesthesia following conscious pain mapping with micro-laparoscopy. Human Reprod. 1998;13:588–590 [DOI] [PubMed] [Google Scholar]
- 3. Almeida OD., Jr. Microlaparoscopic equipment. In: Almeida OD, Jr., ed. Microlaparoscopy. New York, New York: Wiley-Liss; 2000;11–18 [Google Scholar]
- 4. Wolf AM, Colditz GA. Social and economic effects of body weight in the United States. Am J Clin Nutr. 1996;63(S):466S–469S [DOI] [PubMed] [Google Scholar]
- 5. Reich H, DeCaprio J, McGlynn F. Laparoscopic hysterectomy. J Gynecol Surg. 1989;5:213–217 [Google Scholar]
- 6. Olive DL, Parker WH, Cooper JM, Levine RL. The AAGL classification system for laparoscopic hysterectomy. J Am Assoc Gynecol Laparosc. 2000;7(1):9–15 [DOI] [PubMed] [Google Scholar]
- 7. Almeida OD., Jr. A new microlaparoscopic technique: Microlaparoscopic-assisted vaginal hysterectomy (MAVH). J Am Assoc Gynecol Laparosc. 2001;8(3):3S [Google Scholar]
- 8. Hurd WW, Bude RO, Delancey JOL, Gauvin JM, Aisen AM. Abdominal wall characterization with magnetic resonance imaging and computed tomography: The effect of obesity on the laparoscopic approach. J Reprod Med. 1991;36:473–476 [PubMed] [Google Scholar]
- 9. Nezhat C, Nezhat F, Seidman DS, Nezhat C. Incisional hernias after laparoscopy. J Laparosc Advanced Surg Tech. 1997;7:111–115 [DOI] [PubMed] [Google Scholar]
- 10. Almeida OD., Jr. Current state of office laparoscopic surgery. J Am Assoc Gynecol Laparosc. 2000;7(4):545–546 [DOI] [PubMed] [Google Scholar]
- 11. Rizquez F. Microlaparoscopy: indications and applications. In: Mempers RD, Cohen J, Haney AF, Younger JB. eds. Fertility and Reproductive Medicine. Amsterdam: Elsevier Science; 1998:71–72 [Google Scholar]
- 12. Almeida OD., Jr. Microlaparoscopy in the 21st Century. Laparoscopy and SLS Report. 2003;2(1):8–11 [Google Scholar]
- 13. Hulka JF, Levy BS, Parker WH, Phillips JM. Laparoscopic-assisted vaginal hysterectomy: American Association of Gynecologic Laparoscopists' 1995 membership survery. J Am Assoc Gynecol Laparosc. 1997;4(2):167–171 [DOI] [PubMed] [Google Scholar]
- 14. Almeida OD, Jr, Val-Gallas JM. Small trocar perforation of the small bowel: A case report. J Soc Laparoendosc Surg. 1998;2:289–290 [PMC free article] [PubMed] [Google Scholar]
- 15. Ben-Hur H, Phipps JH. Laparoscopic hysterectomy. J Am Assoc Gynecol Laparosc. 2000;7(1):103–106 [DOI] [PubMed] [Google Scholar]