Nephrotic syndrome is a broad group of disorders with diverse etiologies. In common, all have proteinuria, edema, hypercholesterolemia, and hypoalbuminemia. Steroids have proven effective in some histologic groups, but many are resistant to steroids and progress to end-stage renal disease. Transplant glomerulopathy and chronic rejection also contribute heavily to renal transplant-related nephrotic syndrome. Previous studies with cyclosporine (CyA)1,2 and FK 5063 suggest that the clinical manifestations of nephrotic syndrome may be controlled with these agents, in native kidneys and in renal allografts. FK 506 is a potent macrolide immunosuppressant agent, which has proven effective in transplantation of the liver, kidney, and heart.4–6 We have previously reported successful treatment of two patients with steroid-resistant nephrotic syndrome with FK 506.3 We report, herein, our preliminary experience treating steroid-resistant nephrotic syndrome and nephrotic syndrome after transplantation with FK 506.
CASE MATERIAL
Native Kidney Disease
Seven patients with nephrotic syndrome, who had proved to be resistant to steroid therapy, were enrolled. The patients’ ages ranged from 2.5 to 40 years. Three patients had failed CyA therapy in addition to having been nonresponsive to other therapies. Four patients had focal segmental sclerosis (FSGS), one had mesangial proliferative glomerulonephritis (GN) due to hepatitis B, one had membranoproliferative GN (MPGN), and 1 had membranous GN.
Transplanted Kidneys
Seventeen patients with nephrotic syndrome after renal transplantation were converted from CyA to FK 506 in an attempt to correct the clinical manifestations of the nephrotic syndrome. Graft biopsies were obtained on all patients prior to entry into this study. Based upon the allograft biopsies, the patients could be divided into those with chronic rejection (eight patients) and those with other histologic findings (nine patients).
METHODS
Patients with steroid-resistant nephrotic syndrome were uniformly treated with an FK 506 starting dose of 0.15 mg/kg, twice a day, orally. Patients without active rejection and long-standing allografts were started on the lower doses. All other immunosuppressant agents were discontinued prior to starting FK 506. Later, FK 506 was tapered to the minimal dose required to control the proteinuria. Preexisting prednisone was tapered and withdrawn in most patients. All patients were treated with acyclovir and bacterium prophylaxis.
RESULTS
Native Kidneys
Three of the seven patients rapidly responded to FK 506 therapy, reducing proteinuria 600 mg/d or less within 2 months. Mean pretreatment values were 4400 ± 3500 mg/d. Two pediatric patients had FSGS and an adult had mesangial proliferative GN. One child had previously failed CyA, cytoxan, and steroids. Remission has been maintained for greater than 1 year in two of the three patients. Three additional patients decreased protein excretion by at least 50% after starting FK 506. Mean pretreatment protein excretion was 13,900 ± 11,300 mg/d.
Only one patient was classified as a failure. Although protein excretion decreased by approximately 50%, this was not sustained. This patient, with FSGS, had failed high-dose steroids, chlorambucil, and CyA therapy. After stopping FK 506, a trial of cytoxan therapy was attempted without success.
Creatinine clearance decreased in all patients after initiating FK 506, but tended to improve as the dose was reduced. Two patients temporarily stopped taking FK 506. Both noted a prompt return of nephrotic syndrome within days. The nephrotic syndrome was rapidly controlled when the drug was reinstituted.
Transplanted Kidneys
Patients Without Chronic Rejection
There were nine patients without chronic rejection on pretreatment biopsies. The demographic and histologic characteristics of these biopsied kidneys are displayed in Table 1. FSGS was the most common finding in allograft biopsies. In two cases the FSGS was de novo. One patient had both transplant glomerulopathy and early chronic rejection.
Table 1.
Transplant Glomerulopathy: Patient Demographics
| Patient | Age | Native Disease | Transplant Bx |
|---|---|---|---|
| JP | 49 | PCKD | FSGS (prdlif. GN) |
| WD | 46 | Hypertension | FSGS (mild ACR) |
| EL | 59 | FSGS | FSGS |
| AM | 24 | SLE | Mesangial Exp. |
| PM | 14 | CGN | FSGS |
| AP | 47 | Diabetes | FSGS |
| AT | 18 | FSGS | FSGS |
| RW | 5 | FSGN | FSGS |
| GD | 50 | CGN | Tx glom/chronic rej. |
Six of the nine patients (66.6%) decreased proteinuria by 50% or greater and had resolution of the signs of proteinuria. Table 2 summarizes the response to FK 506. The response to FK 506 was dramatic in some patients, as illustrated by our first patient, JP (Fig 1). Although the response was usually rapid, a progressive decline in proteinuria, over many months, was also seen. Our second patient (WD) initially experienced an increase in proteinuria, followed by a slow progressive decline without a reduction in renal function (Fig 2). Two patients (AT, RW) failed FK 506 therapy. Both had FSGS which had recurred within weeks of transplantation, and were referred prior to nephrectomy for intractable nephrotic syndrome. Both patients experienced an increase in proteinuria after conversion to FK 506. The allograft has been removed in one patient (AT).
Table 2.
Transplant-Related Nephrotic Syndrome
| SCR |
Proteinuria |
F/U (Months) | |||
|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||
| JP | 1.4 | 0.9 | 9766 | 284 | 16 |
| WD | 1.2 | 1.1 | 5400 | 792 | 13 |
| EL | 1.7 | 1.9 | 10,366 | 3172 | 9 |
| AM | 1.5 | 1.3 | 2844 | 1856 | 5 |
| PM | 1.6 | 2.6 | 9620 | 1309 | 12 |
| AP | 1.9 | 2.0 | 3323 | 1763 | 2 |
| AT | 2.4 | 3.5 | 9600 | 12,155 | 3* |
| RW | 1.3 | 2.7 | 8600 | 16,000 | 6* |
| GD | 1.4 | 1.1 | 4400 | 5400 | 1.5 |
Failed.
Proteinura in milligrams per day.
Fig 1.
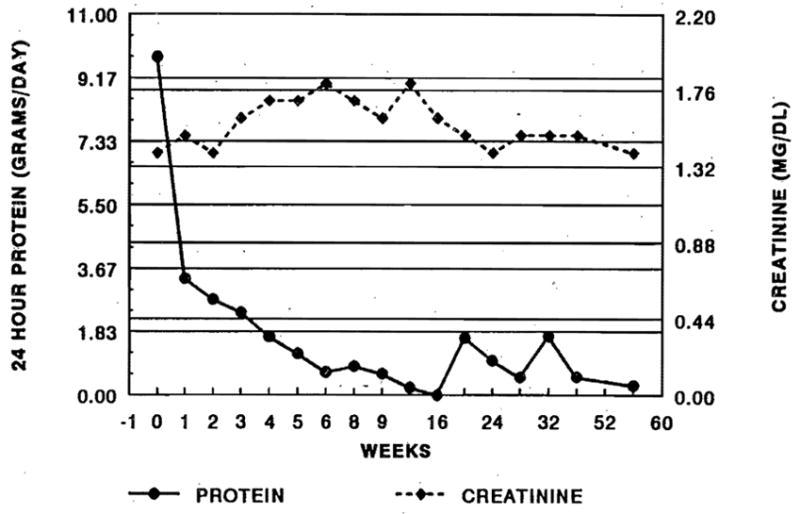
Rapid reduction in protein excretion after conversion to FK 506 without significant increase in SCr (patient 1).
Fig 2.
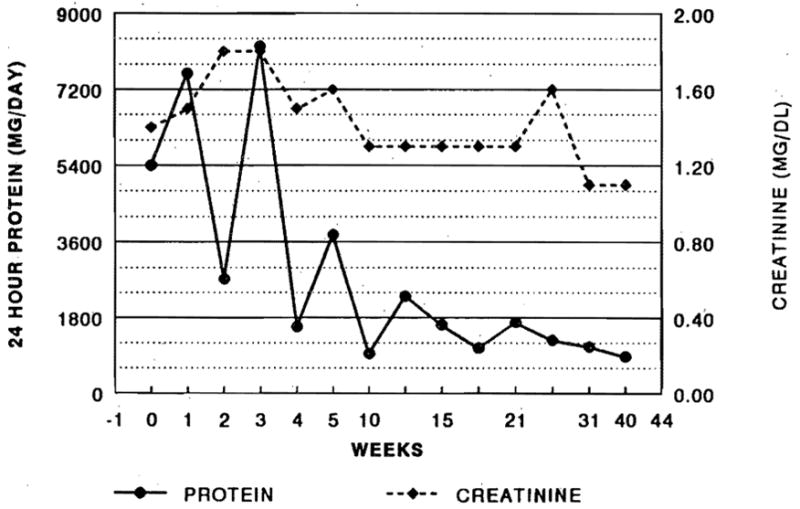
Early exacerbation of proteinuria followed by progressive improvement (patient 2).
Patients With Chronic Rejection
Patients with chronic rejection experienced little benefit from FK 506. At latest follow-up, four of the eight patients have had nephrectomies or have started dialysis. Three patients have poorly functioning grafts with persistent nephrotic range proteinuria in two. One patient died of an intracerebral hemorrhage unrelated to nephrotic syndrome.
DISCUSSION
FK 506 appears to be an effective treatment for some patients with steroid-resistant nephrotic syndrome and transplant-related nephrotic syndrome. It is likely that FK 506 causes a functional change in the basement membrane and not a permanent change in the primary immunological origin of glomerulonephritis, since recurrence of nephrotic syndrome was rapid with drug withdrawal. A similar response has been noted in trials with CyA.1,2 FK 506 was, interestingly, effective in patients who had previously failed CyA therapy.
Patients with nephrotic syndrome after transplantation have previously been susceptible to no therapy. Our preliminary experience suggests that FK 506 may be
effective in patients without negative prognostic indicators such as (1) chronic rejection, (2) advanced renal failure, or (3) rapidly recurrent FSGS. Typically, patients respond within weeks to treatment with FK 506. However, some patients may require months to attain a sustained progressive reduction in proteinuria. A transient rise in SCr is to be expected after conversion from CyA to FK 506 and should not necessarily lead to a reduction in FK 506 dosage.
References
- 1.Ponticelli C, Rivolta E. Am J Nephrol. 1990;1:105. doi: 10.1159/000168206. [DOI] [PubMed] [Google Scholar]
- 2.Banfi G, Colturi C, Montagnino G, et al. Transplantation. 1990;50:594. doi: 10.1097/00007890-199010000-00013. [DOI] [PubMed] [Google Scholar]
- 3.McCauley J, Bronster, Fung JJ, et al. Lancet. 1990;335:8690. doi: 10.1016/0140-6736(90)90471-g. [DOI] [PubMed] [Google Scholar]
- 4.Starzl TE, Todo S, Fung JJ, et al. Lancet. 1989;ii:1000. doi: 10.1016/s0140-6736(89)91014-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Starzl TE, Abu-Elmagd K, Tzakis A, et al. Transplant Proc. 1991;23:914. [PubMed] [Google Scholar]
- 6.Fung JJ, Todo S, Jain A, et al. Transplant Proc. 1990;22:6. [PMC free article] [PubMed] [Google Scholar]


