Abstract
Somatic mosaicism has been observed previously in the lymphocyte population of patients with Fanconi anemia (FA). To identify the cellular origin of the genotypic reversion, we examined each lymphohematopoietic and stromal cell lineage in an FA patient with a 2815–2816ins19 mutation in FANCA and known lymphocyte somatic mosaicism. DNA extracted from individually plucked peripheral blood T cell colonies and marrow colony-forming unit granulocyte–macrophage and burst-forming unit erythroid cells revealed absence of the maternal FANCA exon 29 mutation in 74.0%, 80.3%, and 86.2% of colonies, respectively. These data, together with the absence of the FANCA exon 29 mutation in Epstein–Barr virus-transformed B cells and its presence in fibroblasts, indicate that genotypic reversion, most likely because of back mutation, originated in a lymphohematopoietic stem cell and not solely in a lymphocyte population. Contrary to a predicted increase in marrow cellularity resulting from reversion in a hematopoietic stem cell, pancytopenia was progressive. Additional evaluations revealed a partial deletion of 11q in 3 of 20 bone marrow metaphase cells. By using interphase fluorescence in situ hybridization with an MLL gene probe mapped to band 11q23 to identify colony-forming unit granulocyte–macrophage and burst-forming unit erythroid cells with the 11q deletion, the abnormal clone was exclusive to colonies with the FANCA exon 29 mutation. Thus, we demonstrate the spontaneous genotypic reversion in a lymphohematopoietic stem cell. The subsequent development of a clonal cytogenetic abnormality in nonrevertant cells suggests that ex vivo correction of hematopoietic stem cells by gene transfer may not be sufficient for providing life-long stable hematopoiesis in patients with FA.
Fanconi anemia (FA) is an autosomal recessive disorder characterized by congenital abnormalities, bone marrow failure, and a predisposition to malignancies, including myelodysplastic syndrome and acute myelogenous leukemia (1). Seven FA complementation groups (FA-A through FA-G) have been reported (2), with FA-A (Online Mendelian Inheritance in Man, OMIM no. 227650) constituting approximately two-thirds of the patients. The FANCA, FANCC, FANCE, FANCF, and FANCG genes have been cloned and mapped to chromosomes 16q24.3, 9q22.3, 6p21.2–21.3, 11p15, and 9p13, respectively (3–8). However, the specific function of these genes remains unclear.
FA cells are uniquely hypersensitive to DNA cross-linking agents such as diepoxybutane (DEB) and mitomycin C (MMC) (9). This cellular phenotype can be demonstrated in cultured T cells, B cells, fibroblasts, and fetal cells cultured from amniotic fluid or chorionic villi (10). Hypersensitivity of phytohemagglutinin (PHA)-stimulated peripheral blood lymphocytes (PBLs) to DEB is used routinely as a diagnostic test for the syndrome (11). At a DEB concentration that has a minimal effect on normal PBLs (0.1 μg/ml), 80–100% of PBLs analyzed will have chromatid breaks and exchanges in the typical FA patient. However, in a small group of patients, DEB-resistant PBLs comprise >50% of the cells analyzed (12). Cultured Epstein–Barr virus-transformed B lymphocytes (lymphoblastoid cell lines, LCLs) are completely resistant to DEB and MMC in least a third of FA patients (13). The mechanism for this spontaneous functional correction has been elucidated in cultured LCLs from several FA subjects (14, 15). Such revertant mosaicism has been noted in several other diseases in the context of an attenuated phenotype and shown to be attributable to restoration of a functional allele in the reverted cells (16–20). The clinical significance of somatic mosaicism in FA is not well understood. Although a milder phenotype has been suggested in FA patients with somatic mosaicism, subjects with revertant mosaicism frequently develop bone marrow failure and leukemia (21).
Although revertant mosaicism in FA has been demonstrated in cultured T cells and LCLs (12–15), the question remains whether genetic reversion ever occurs in the pluripotent lymphohematopoietic stem cell. We therefore examined hematopoietic progenitor cells from an FA-A patient with lymphoid somatic mosaicism.
Materials and Methods
Cytogenetics.
PBLs were cultured for 96 h with PHA under routine conditions for evaluation of baseline chromosomal breakage rates and in the presence of MMC (20 ng/ml) and/or DEB (0.1 μg/ml) to test for DNA crosslink sensitivity (11). PBL cultures from a control individual were established concurrently and treated identically in vitro. Fifty G banded (University of Minnesota) or unbanded (Rockefeller University, RU) metaphase cells were examined for each condition. Bone marrow aspirates were cultured for 24 h, and metaphase chromosomes were prepared and analyzed by using standard cytogenetic techniques. Twenty G banded metaphase cells were analyzed. Sequential G banding to fluorescence in situ hybridization (FISH) was performed on prepared metaphase cells from bone marrow by using a technique previously reported (22). FISH was performed with an MLL gene probe (ONCOR) mapped to band 11q23. Interphase FISH on individually plucked colonies was performed by using a modification of the method reported by Xu et al. (23). Briefly, colony-forming unit granulocyte–macrophage (CFU-GM) and burst-forming unit erythroid (BFU-E) colonies (see below) each were received in 10 μl of medium, to which 10 μl of hypotonic solution (0.068 M KCl with BSA) was added. Ten microliters of 0.001 M HCl and 0.1% Nonidet P-40 were applied to the slide, and spreading was monitored with an inverted microscope. The slide was air-dried, washed in 1× PBS, dehydrated in an ethanol series, and incubated at 63°C for 10 min before application of probe mixture containing both the MLL gene probe labeled with digoxigenin and a probe specific to the centromere of chromosome 11 labeled with spectrum green (Vysis, Downers Grove, IL). The slide was placed in a Hybrite for denaturation (5 min at 75°C) and overnight hybridization (37°C). Slides were washed in 2× SSC, treated with rhodamine for 6 min for detection of MLL, washed in buffer, and counterstained with 4′,6-diamidino-2-phenylindole. Each slide was examined with an Olympus scope outfitted for fluorescence with 4′,6-diamidino-2-phenylindole, FITC, Texas Red, and Triple-band filter sets. As many cells as possible were examined for each colony, ranging from 2 to 186. Only those cells with two detectable centromere 11 signals were scored for the presence of MLL.
Hematopoietic Progenitor Assay.
Bone marrow or peripheral blood mononuclear cells (MNC) were prepared by using standard techniques. Bone marrow MNC then were suspended at three concentrations, 0.5, 5, and 50 × 105 cells per ml, in Iscove's modified Dulbecco's medium (IMDM)/2% FBS. Four hundred microliters of suspension was added to 4-ml aliquots of Methocult H-4434 (StemCell Technologies, Vancouver). Suspension (1.1 ml) was placed in three 35-mm tissue culture plates and incubated at 37°C in 5% CO2 for 14 days. CFU-GM and BFU-E containing >50 cells were plucked individually and placed into separate microcentrifuge tubes containing 10 μl of RPMI/10% FBS. Samples were placed in −80°C until further analysis. Peripheral blood MNC were adjusted to 1.5 × 106 cells per ml in IMDM. Two hundred microliters of suspension was added to 2 ml of Methocult H-4531 supplemented with 5 units/ml erythropoietin (R & D Systems) and plated in two 35-mm culture plates. Plates were incubated at 37°C in 5% CO2 for 14 days. As above, individual colonies were plucked and stored until further analysis.
T Cell Colonies.
Peripheral blood MNC were treated with ammonium chloride lysing solution for 5 min at 22°C to remove remaining red blood cells. Lysed cells were washed and 20 × 106 cells were resuspended in 100 μl of PBS. Cells were stained with CD3 FITC (Coulter) for 20 min on ice. Two 5 × 105 aliquots of the cells were stained with isotype control antibodies. Stained cells were selected on the FACSVantage Cell Sorter (Becton Dickinson). CD3-enriched cells then were placed in 96-well plates in limiting dilution. The cells were grown in RPMI 1640 medium supplemented with 25 mM Hepes/penicillin/streptomycin/l-glutamine/10% pooled human serum/5 μg/ml PHA-p (Difco)/20 units/ml IL-2 (R & D Systems) at 37°C, 10% CO2. After 7 days, individual colonies were removed and placed in microcentrifuge tubes containing 100 μl of RPMI 1640/10% FBS. Colonies were kept at −80°C and stored until analysis.
DNA Preparation.
Genomic DNA was extracted from PBLs, LCLs, and fibroblasts by standard methods. PCR on the individually plucked CFU-GM, BFU-E, and T cell colonies was performed directly on lysed cells. Colonies suspended in RPMI 1640 were pelleted by centrifugation for 10 min at 13,000 rpm and resuspended in 50 mM NaOH. Samples were heated at 95°C for 5 min, chilled, and neutralized by the addition of 1/10 vol of 1.0 M Tris⋅Cl, pH 7.8; lysed colonies were stored at −20°C. Preparation of DNA from individually plucked colonies spread on microscopic slides for the FISH studies was performed by a modification of the method of Choi et al. (24). After the collection of the supernatant, the procedure for DNA preparation from colonies, as described above, was applied.
PCR Analysis.
FANCA exon 29 was amplified from genomic DNA obtained from PBLs, LCLs, fibroblasts, and BFU-E, CFU-GM, and CD3+ colonies. PCRs contained 10 ng of genomic DNA (or 5 μl of lysed cell suspension), 10 mM Tris⋅HCl (pH 8.3), 50 mM KCl, 1.5 mM MgCl2, 0.25 mM spermidine, 0.2 mM dNTP, 0.6 μM forward (29F: 5′-GTGTGTTCTGTCCTCATTG-3′) and reverse (29R: 5′-GATTCAAGAGATCTCCTGCC-3′) primers and 0.5 units of Taq DNA polymerase (Boehringer Mannheim). PCR conditions were: denaturation for 3 min at 95°C followed by 35 cycles of 30 sec at 94°C, 30 sec at 60°C, and 40 sec at 72°C. Amplification of FANCA exon 29 by PCR in normal individuals results in a single band on agarose gel electrophoresis migrating at 214 bp. When patients carry one normal exon 29 allele and one allele that has the exon 29 mutation 2815–2816ins19, PCR amplification results in two bands on agarose gel electrophoresis migrating at 214 and 233 bp, respectively. In some cases, a second round of heminested PCR was required to visualize the PCR products on agarose gels; heminested PCR was performed exactly as described above, with the substitution of primer 29R1 (5′-GGCCAGGGTAGCTCTTTTCAAC-3′) as the reverse primer. Rare polymorphisms in FANCA were screened by direct sequencing. Allele-specific reactions for the common polymorphisms IVS23+8T/C, IVS32–42G/A, IVS39–16C/T, and IVS42+29T/C were performed exactly as described (25).
Results
Subject IFAR 557–2.
This subject was born 10/26/82. He was diagnosed July 1992 by family screening after a sibling (IFAR 557–1) who presented with bone marrow failure was diagnosed with FA at age 7 years. Physical examination was significant for short stature, bifid thumbs, and skin pigmentation abnormalities. Peripheral blood count revealed a total white blood cell count of 3.6 × 109/liter, absolute neutrophil count of 1.2 × 109/liter, hemoglobin of 14.9 g/dl, and platelet count of 64 × 109/liter. Bone marrow cellularity was 20–25%. He has not required steroid or androgen treatment.
Several cytogenetic studies of crosslink-induced chromosomal breakage in PBLs from IFAR557–2 revealed the presence of a stable population of DNA crosslink-sensitive cells over a period of 5 years with consistency in two independent laboratories: (i) May 1994 (University of Minnesota), 34% DEB-sensitive cells, 39% MMC-sensitive cells; (ii) May 1994 (RU), 32% DEB-sensitive cells; (iii) September 1997 (RU), 32% DEB-sensitive cells; (iv) February 1999 (RU), 32% DEB-sensitive cells; and (v) July 1999 (RU), 26% DEB-sensitive cells. Concurrent testing of this patient's affected sibling in 1994 revealed 96% (University of Minnesota) and 84% (RU) of DEB-sensitive cells, typical results in FA patients.
IFAR 557–2 was determined to be a compound heterozygote for mutations in FANCA. The maternal allele, a 19-bp insertion in exon 29, 2815–2816ins19 (25), was identified by single-strand conformational polymorphism (SSCP) studies of PBLs. Upon sequencing, the signal of the mutant allele was of lower intensity compared with the normal allele in IFAR 557–2. This intensity difference was not observed in his heterozygous mother, subject IFAR 557–12, or in an unrelated subject with the same mutation, IFAR 571–1. The difference in signal intensity was consistent with somatic mosaicism, as indicated by the two populations of lymphoid cells upon DEB testing of PB.
Cultured fibroblasts (RA2023) from IFAR 557–2 retain the maternally inherited 2815–2816ins19 mutation and are DEB-sensitive, whereas his LCL (RA2026) no longer exhibits the mutation, and is DEB-resistant. Both the fibroblasts and the LCL from the patient remain heterozygous for markers flanking exon 29, indicating that a back mutation or a gene-conversion event, rather than a mitotic recombination event, is the most likely mechanism of the reversion (Fig. 1).
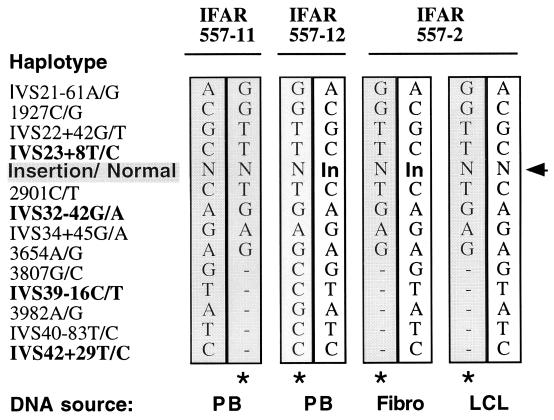
Figure 1.
Haplotypes for SNPs segregating in family IFAR 557. Both common and rare polymorphisms were typed on genomic DNA extracted from PB from the father (IFAR 557–11) and the mother (IFAR 557–12) and on DNA extracted from the LCL and fibroblasts from the patient (IFAR 557–2). N, normal allele; In, 2815–2816ins19; bold type, common polymorphisms; regular type, rare polymorphisms; *, rare haplotype. Phase is deduced from data from other subjects, indicating that the rare SNPs are found only as a single haplotype with the common variants as shown.
The paternal mutation was not discovered in this patient by SSCP analysis of all 43 exons of FANCA; analysis of single-nucleotide polymorphisms (SNPs) within FANCA suggests that the father's mutation is a large genomic deletion of the 3′ end of the gene (Fig. 1). One FANCA allele in each of the parents of IFAR 557–2 carries a set of single-nucleotide polymorphism (SNPs) that segregate together as a haplotype, including several rare, nonpathogenic variants, IVS21–61G, 1927G, IVS22+42T, 2901T, IVS34+45A, 3654G, 3807C, 3982G, and IVS40–83C (O.L., unpublished data). As rare polymorphisms, they typically are found to be heterozygous. In this case, the patient's mother (IFAR 557–12) carries the complete set of polymorphisms on her nonmutated FANCA allele, and the father (IFAR 557–11) and the proband (IFAR 557–2) carry the six 5′ rare variants but do not carry 3807C, 3982G, and IVS40–83C.
Hematopoietic Colonies.
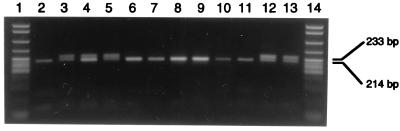
FANCA exon 29 was amplified by PCR in individually plucked hematopoietic precursors from a bone marrow sample obtained on 09/24/97 to screen for the maternal mutation, 2815–2816ins19. Samples heterozygous for the insertion generated two products, a 214-bp fragment representing the normal allele, and a 233-bp fragment representing the insertion, whereas samples homozygous for the normal allele generated a single, 214-bp fragment (Fig. 2). Both products were found in 8 of 58 BFU-E colonies (13.8%), whereas only the normal product was found in the other 50 BFU-E colonies (86.2%). Twelve of 61 CFU-GM colonies (19.7%) retained the insertion mutation, with the remaining 49 colonies (80.3%) producing only the normal product. Similarly, 7 of 27 CD3+ T cell colonies (26%) retained the insertion mutation. PCR products from a colony that produced the normal allele and from one that produced both the normal and mutant alleles were sequenced to confirm the interpretation of these results. BFU-E and CFU-GM colonies from IFAR 557–12 (mother of IFAR 557–2) were used as a positive control for the PCR assay; as expected, IFAR 557–12 carried the mutation in all colonies. Of the 40 BFU-E colonies that were analyzed, 37 were positive for the mutation and 3 samples failed. All six of six CFU-GM colonies were positive for the mutation, and the PCR product from one colony was sequenced to confirm the presence of the mutation.
Figure 2.
Mutation screening of individually plucked hematopoietic precursors. FANCA exon 29 was PCR-amplified from individually plucked hematopoietic precursors. Presence of the normal allele is indicated by a 214-bp product, and the presence of the 2815–2816ins19 mutation is indicated by a 233-bp product. Lanes: 1 and 14, pBR322 MspI markers; 2, IFAR 557–11 PB; 3, IFAR 557–12 PB; 4, IFAR 557–2 PB; 5–9, IFAR 557–2 BFU-E; 10–12, IFAR 557–2 CFU-GM; 13, IFAR 557–12 BFU-E.
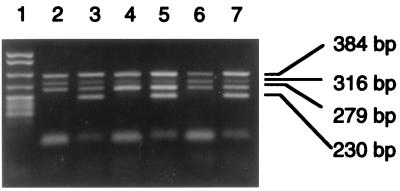
Two BFU-E colonies, one positive for the mutation and one negative for the mutation, and a PB sample were screened for the common flanking polymorphisms in introns 23, 32, and 42 (Fig. 3). The intron 42 polymorphism, IVS42+29T/C, appears to be homozygous in all samples tested, because of the apparent paternal deletion. The intron 23 polymorphism, IVS23+8T/C, proximal to the mutation, and the intron 32 polymorphism, IVS32–42G/A, distal to the mutation, are heterozygous in all samples, indicating that there is no loss of heterozygosity in the cell that has lost 2815–2819ins19. These findings were consistent with that seen in the revertant LCL.
Figure 3.
FANCA polymorphism screening in flow-sorted colonies. Paired multiplex allele-specific PCRs for each allele of three FANCA polymorphisms were performed on a BFU-E colony positive for 2815–2816ins19 (lanes 2 and 3), PB (lanes 4 and 5), and a BFU-E colony negative for 2815–2816ins19 (lanes 6 and 7). Reaction 1 (lanes 2, 4, and 6) results in PCR products in the presence of the IVS23+8T (279 bp), IVS32–42G (316 bp), and IVS42+29T (230 bp) alleles. Reaction 2 (lanes 3, 5, and 7) results in PCR products in the presence of the IVS23+8C, IVS32–42A, and IVS42+29C alleles. Homozygosity for a polymorphism for a given sample is indicated by the presence of a band in one reaction but not the other, whereas heterozygosity for a given sample is indicated by the presence of a band in both reactions. A 384-bp control product from exon 6 of FANCA is present in both reactions. Lane 1, pBR322 MspI markers.
Clonal Cytogenetic Abnormality.
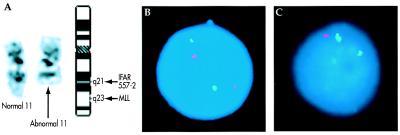
Cytogenetic analysis of bone marrow samples from IFAR 557–2 demonstrated a normal karyotype, 46,XY, in May 1992 and 1994. On 09/24/97, however, an abnormal clone was identified, comprising 15% of the metaphases examined. This clone was characterized by an abnormal chromosome 11 deleted from band 11q21 to 11qter, with a small amount of additional chromosomal material of unknown origin in its place (Fig 4A).
Figure 4.
(A) G banded chromosome 11 homologs from IFAR 557–2 bone marrow sample. (Left) Normal chromosome 11. (Center) Abnormal chromosome 11 resulting in loss of material distal to the breakpoint in band 11q21. (Right) Idiogram showing normal G banding pattern of chromosome 11 at approximately 400-band-level resolution and the position of the MLL locus. (B) Image of a normal interphase cell from an IFAR 557–2 colony. FISH shows two chromosome 11 centromere signals (green) and two MLL gene signals (red). (C) Image of a cell harboring the abnormal chromosome 11 from an IFAR 557–2 colony. FISH shows two chromosome 11 centromere signals (green), but only one MLL signal (red).
Sequential G banding to FISH on marrow metaphases from 07/19/99 confirmed that the MLL locus within band 11q23 was deleted in the abnormal chromosome 11 and, thus, could be used to monitor this clone in interphase cells (Fig. 4 B and C). To determine whether the rearrangement occurred in a reverted cell or in a cell that retained the 2815–16ins19 mutation, plucked CFU-GM and BFU-E colonies from this sample were screened both for 2815–2816ins19 by PCR and for the deletion of MLL by interphase FISH. Twenty-seven (59%) of the 46 plucked colonies yielded results by FISH; four of these were uninterpretable because of contamination between colonies. Of the 23 colonies with technically good FISH results, 3 colonies (2 CFU-GM and 1 BFU-E) demonstrated a single MLL signal in conjunction with two centromere signals, indicative of the clonal abnormality characterized by G banding. The remaining 20 colonies (14 CFU-GM and 6 BFU-E) demonstrated two MLL and centromere signals, indicative of a nondeleted cell.
Mutation screening was performed successfully in a blinded fashion on 20 of 23 colonies that yielded results by FISH analysis. All 16 of the revertant colonies with two normal FANCA alleles and 2 of the colonies with the 2815–1816ins19 mutation were cytogenetically normal by FISH. Two of the colonies with the 2815–1816ins19 mutation exhibited the 11q deletion, indicating that the cytogenetic abnormality occurred in a nonrevertant cell.
Discussion
By examining each lymphohematopoietic lineage, we have presented evidence of a genetic event in a hematopoietic stem cell leading to correction of a 19-bp insertion, 2815–2816ins19, in exon 29 of the FANCA gene of subject IFAR 557–2. 2815–2816ins19 created a 19-bp tandem repeat in close proximity to the tetranucleotide CCTG (CAGG) motif, previously identified to be a mutation hot spot consensus sequence in FANCA (25) as well as other syndromes (26). Although hypothesized by others, we present evidence supporting a somatic reversion event in a pluripotential hematopoietic stem cell. Revertant mosaicism has been reported in various diseases including severe combined immunodeficiency [both X linked and adenosine deaminase (ADA) deficiency; refs. 16, 17, and 27], Duchenne muscular dystrophy (28), tyrosinemia (20), Bloom syndrome (19), and epidermolysis bullosa (18, 29) among others. In each of these cases, restoration of a normal allele was demonstrated in cells of a single lineage. In some of these reports, evidence suggesting a mechanism for the reversion was presented, including mitotic gene conversion (18), back mutation (20, 27), intragenic mitotic recombination (19), and the introduction of compensatory mutations (28, 29). Each of these mechanisms can result in the restoration of one allele coding for a functional product.
Somatic mosaicism in Fanconi anemia has been reported to result from a variety of mechanisms. In three compound heterozygous patients in whom a molecular mechanism was investigated, it was proposed that one case was attributable to a single intragenic mitotic recombination, whereas gene conversion was suggested to be the mechanism in the other two cases (14). Most recently, the introduction of compensatory mutations was demonstrated for three different cases in which the FA patients were homozygous for different mutations and a different type of compensatory change was found in each (15). Two of these individuals had frameshift mutations in FANCA that were compensated for by downstream mutations. The third case is perhaps the most interesting: a pair of FA siblings, homozygous for the FANCC missense mutation 1749G→T, independently developed the same compensatory mutation, 1748C→T.
We have demonstrated loss of the maternal exon 29 mutation, 2815–2816ins19, in the majority of hematopoietic precursors from subject IFAR 557–2. We suggest that back mutation in a hematopoietic precursor is the most likely mechanism for the revertant mosaicism in this case. We previously have shown data to suggest that slipped-strand mispairing (30), a mutational mechanism recognized as important for the generation of both germ-line and somatic mutations in a variety of cancer-related genes, may be a major mechanism for FANCA mutagenesis (25). Because the 2815–2816ins19 creates a 19-bp tandem repeat in close proximity to a deletion hot spot consensus sequence (26), it is easy to see how one DNA strand could be misaligned by chance with the downstream repeat of the complementary strand. The resulting loop subsequently would be excised, fixing the deletion before the next round of replication. A gene-conversion event over a short conversion tract also could theoretically explain our finding of a revertant maternal allele in subject IFAR 557–2. We cannot rule this out, because the distance between the heterozygous variants in intron 23 and exon 30 flanking the maternal mutation in exon 29 (see Fig. 1) was approximate 12 kb (31), whereas the most common gene-conversion tract lengths demonstrated in an experimental mammalian system were 58 bp or less (32). However, spontaneous gene-conversion events are rare, and slipped-strand mispairing, which is thought to be responsible for a significant proportion of spontaneous mutations in mammalian cells (33), is more likely to be the mechanism responsible for our findings in our patient. Intragenic mitotic recombination between paternally and maternally derived mutated sites within the FANCA gene can be ruled out as a causative mechanism in our case, because the SNPs in FANCA exons distal to the recombination site would be expected to become homozygous (19), and this was not observed.
Somatic mosaicism originating in a pluripotential stem cell can be viewed as spontaneous “natural” gene therapy and has many implications for FA patients. A main premise of gene therapy in FA patients is that corrected FA cells will have a proliferative advantage over noncorrected cells. Therefore, mosaic patients can serve as a model for the potential success of gene therapy in FA. IFAR 557–2 demonstrated 74–87% reverted cells and has maintained adequate, although not normal, hematopoiesis at age 16; an affected sibling had severe bone marrow failure by age 6.8 years. Although the onset of bone marrow failure in FA is not well understood and is probably multifactorial, these differences in clinical course between siblings could be explained by somatic mosaicism in IFAR 557–2. This would appear to support expectations for the potential success of gene therapy, but questions remain about the long-term ability of corrected cells to sustain hematopoiesis. Some FA patients who have severe bone marrow failure are found to be somatic mosaics based on DEB testing of fresh T lymphocytes (9, 10). However, the extent of the mosaicism in the stem cell pool of these patients is unknown, and clearly the mosaicism must extend beyond the lymphoid compartment to protect the patient from bone marrow failure.
The risk of malignancy in a chimeric state of FA cells and reverted cells is another open question for somatic mosaic patients and, by extension, for patients treated with gene therapy. Although these patients may have an improved prognosis because of the presence of a population of normal cells, it is unknown whether they remain at high risk for malignancy because of the presence of a nonreverted population of cells. Conversely, it has been suggested that the presence of a population of reverted cells with a growth advantage over the native population of FA cells actually might suppress the development of malignancy. Alternately, if the reverted cell already had accumulated genetic damage in cancer-related genes before undergoing reversion, malignancy eventually might develop within the cell population derived from a single, reverted hematopoietic stem cell. We describe here the development of a clonal abnormality within the nonreverted FA population of cells that has serious implications for the long-term success of gene therapy in FA patients. These results suggest that it may be necessary to eradicate the nonreverted FA cell population with low-dose chemotherapy.
Another major issue for this group of FA patients is the effect of somatic mosaicism on the need for and success of bone marrow transplantation. Indications for bone marrow transplantation in FA patients regardless of mosaic status include bone marrow failure, clonal abnormalities on bone marrow cytogenetic testing, and leukemia. Although more cases need to be evaluated, at least a proportion of mosaic FA patients still develop bone marrow failure and potentially will require bone marrow transplantation. If populations of both DEB-sensitive and DEB-resistant lymphocytes exist in a patient, a low-dose conditioning regimen that is standard therapy for FA patients may provide inadequate immunosuppression for the resistant population (21).
In summary, we have presented a demonstration of somatic reversion of a hematopoietic stem cell. By defining the spectrum of mosaicism in all hematopoietic lineages and not simply within the lymphoid lineage, a clearer picture of the relevance of mosaicism to prognosis and therapy of FA now can be established.
Acknowledgments
This work was supported by National Institutes of Health Grant HL32987 (A.D.A.), The Fanconi Anemia Research Fund (J.E.W., C.R.E.), the Leukemia Task Force (B.H., A.S.), and the Children's Cancer Research Fund (J.E.W.).
Abbreviations
- FA
Fanconi anemia
- DEB
diepoxybutane
- LCL
lymphoblastoid cell line
- PBL
peripheral blood lymphocyte
- MNC
mononuclear cell
- CFU-GM
colony-forming unit granulocyte–macrophage
- BFU-E
burst-forming unit erythroid
- RU
Rockefeller University
- FISH
fluorescence in situ hybridization
- SNP
single-nucleotide polymorphism
References
- 1.Auerbach A D, Buchwald M, Joenje H. In: The Metabolic and Molecular Basis of Inherited Diseases. 8th Ed. Scriver C R, Beadet A L, Sly W S, Valle D, Childs B, Vogelstein B, editors. New York: McGraw–Hill; 2001. pp. 753–768. [Google Scholar]
- 2.Joenje H, Levitus M, Waisfisz Q, D'Andrea A, Garcia-Higuera I, Pearson T, van Berkel C G, Rooimans M A, Morgan N, Mathew C G, et al. Am J Hum Genet. 2000;67:759–762. doi: 10.1086/303067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lo Ten Foe J R, Rooimans M A, Bosnoyan-Collins L, Alon N, Wijker M, Parker L, Lightfoot J, Carreau M, Callen D F, Savoia A, et al. Nat Genet. 1996;14:320–323. doi: 10.1038/ng1196-320. [DOI] [PubMed] [Google Scholar]
- 4.Fanconi Anemia/Breast Cancer Consortium. Nat Genet. 1996;14:324–328. [Google Scholar]
- 5.Strathdee C A, Duncan A M, Buchwald M. Nat Genet. 1992;1:196–198. doi: 10.1038/ng0692-196. [DOI] [PubMed] [Google Scholar]
- 6.de Winter J P, Léveillé F, van Berkel C G M, Rooimans M A, van der Weel L, Steltenpool J, Demuth I, Morgan N V, Alon N, Bosnoyan-Collins L, et al. Am J Hum Genet. 2000;67:1306–1308. doi: 10.1016/s0002-9297(07)62959-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Winter J P, Rooimans M A, van Der Weel L, van Berkel C G, Alon N, Bosnoyan-Collins L, de Groot J, Zhi Y, Waisfisz Q, Pronk J C, et al. Nat Genet. 2000;24:15–16. doi: 10.1038/71626. [DOI] [PubMed] [Google Scholar]
- 8.de Winter J P, Waisfisz Q, Rooimans M A, van Berkel C G, Bosnoyan-Collins L, Alon N, Carreau M, Bender O, Demuth I, Schindler D, et al. Nat Genet. 1998;20:281–283. doi: 10.1038/3093. [DOI] [PubMed] [Google Scholar]
- 9.Auerbach A D, Rogatko A, Schroeder-Kurth T M. Blood. 1989;73:391–396. [PubMed] [Google Scholar]
- 10.Auerbach A D, Ghosh R, Pollio P C, Zhang M. In: Fanconi. Anemia, Clinical, Cytogenetic and Experimental Aspects. Schroeder T M, Auerbach A D, Obe G, editors. Heidelberg: Springer; 1989. pp. 71–82. [Google Scholar]
- 11.Auerbach A D. Exp Hematol. 1993;21:731–733. [PubMed] [Google Scholar]
- 12.Auerbach A D, Rogatko A, Schroeder T M. In: Fanconi. Anemia, Clinical, Cytogenetic and Experimental Aspects. Schroeder T M, Auerbach A D, Obe G, editors. Heidelberg: Springer; 1989. pp. 3–17. [Google Scholar]
- 13.Auerbach A D, Koorse R E, Ghosh R, Venkatraj V S, Zhang M, Chiorazzi N. In: Fanconi. Anemia, Clinical, Cytogenetic and Experimental Aspects. Schroeder T M, Auerbach A D, Obe G, editors. Heidelberg: Springer; 1989. pp. 213–225. [Google Scholar]
- 14.Lo Ten Foe J R, Kwee M L, Rooimans M A, Oostra A B, Veerman A J, van Weel M, Pauli R M, Shahidi N T, Dokal I, Roberts I, et al. Eur J Hum Genet. 1997;5:137–148. [PubMed] [Google Scholar]
- 15.Waisfisz Q, Morgan N V, Savino M, de Winter J P, van Berkel C G, Hoatlin M E, Ianzano L, Gibson R A, Arwert F, Savoia A, et al. Nat Genet. 1999;22:379–383. doi: 10.1038/11956. [DOI] [PubMed] [Google Scholar]
- 16.Stephan V, Wahn V, Le Deist F, Dirksen U, Broker B, Muller-Fleckenstein I, Horneff G, Schroten H, Fischer A, de Saint Basile G. N Eng J Med. 1996;335:1563–1567. doi: 10.1056/NEJM199611213352104. [DOI] [PubMed] [Google Scholar]
- 17.Hirschhorn R, Yang D R, Israni A, Huie M L, Ownby D R. Am J Hum Genet. 1994;55:59–68. [PMC free article] [PubMed] [Google Scholar]
- 18.Jonkman M F, Scheffer H, Stulp R, Pas H H, Nijenhuis M, Heeres K, Owaribe K, Pulkkinen L, Uitto J. Cell. 1997;88:543–551. doi: 10.1016/s0092-8674(00)81894-2. [DOI] [PubMed] [Google Scholar]
- 19.Ellis N A, Lennon D J, Proytcheva M, Alhadeff B, Henderson E E, German J. Am J Hum Genet. 1995;57:1019–1027. , and erratum (1996) 58, 254. [PMC free article] [PubMed] [Google Scholar]
- 20.Kvittingen E A, Rootwelt H, Berger R, Brandtzaeg P. J Clin Invest. 1994;94:1657–1661. doi: 10.1172/JCI117509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.MacMillan M L, Auerbach A D, Davies S M, DeFor T E, Gillio A, Giller R, Harris R, Cairo M, Dusenbery K, Hirsch B, et al. Brit J Haematol. 2000;109:121–129. doi: 10.1046/j.1365-2141.2000.01955.x. [DOI] [PubMed] [Google Scholar]
- 22.Fink J M, Dobyns W B, Guerrini R, Hirsch B A. Am J Hum Genet. 1997;61:379–387. doi: 10.1086/514863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu K, Huang T, Liu T, Shi Z, Rosenwaks Z J. Assist Reprod Genet. 1998;15:570–574. doi: 10.1023/A:1022542406056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Choi S K, Kim J W, Park S Y, Kim Y M, Kim J M, Ryu H M, Yang J S, Yoon R. Exp Mol Med. 1999;31:36–41. doi: 10.1038/emm.1999.6. [DOI] [PubMed] [Google Scholar]
- 25.Levran O, Erlich T, Magdalena N, Gregory J J, Batish S D, Verlander P C, Auerbach A D. Proc Natl Acad Sci USA. 1997;94:13051–13056. doi: 10.1073/pnas.94.24.13051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huff V, Jaffe N, Saunders G F, Strong L C, Villalba F, Ruteshouser E C. Am J Hum Genet. 1995;56:84–90. [PMC free article] [PubMed] [Google Scholar]
- 27.Hirschhorn R, Yang D R, Puck J M, Huie M L, Jiang C K, Kurlandsky L E. Nat Genet. 1996;13:290–295. doi: 10.1038/ng0796-290. [DOI] [PubMed] [Google Scholar]
- 28.Klein C J, Coovert D D, Bulman D E, Ray P N, Mendell J R, Burghes A H. Am J Hum Genet. 1992;50:950–959. [PMC free article] [PubMed] [Google Scholar]
- 29.Darling T N, Yee C, Bauer J W, Hintner H, Yancey K B. J Clin Invest. 1999;103:1371–1377. doi: 10.1172/JCI4338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Streisinger G, Okada Y, Emrich J, Newton J, Tsugita A, Terzaghi E, Inouye M. Cold Spring Harbor Symp Quant Biol. 1966;31:77–84. doi: 10.1101/sqb.1966.031.01.014. [DOI] [PubMed] [Google Scholar]
- 31.Centra M, Memeo E, d'Apolito M, Savino M, Ianzano L, Notarangelo A, Liu J, Doggett N A, Zelante L, Savoia A. Genomics. 1998;51:463–467. doi: 10.1006/geno.1998.5353. [DOI] [PubMed] [Google Scholar]
- 32.Elliott B, Richardson C, Winderbaum J, Nickoloff J A, Jasin M. Mol Cell Biol. 1998;18:93–101. doi: 10.1128/mcb.18.1.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kimura H, Iyehara-Ogawa H, Kato T. Mutagenesis. 1994;9:395–400. doi: 10.1093/mutage/9.5.395. [DOI] [PubMed] [Google Scholar]