Abstract
The current study investigated the main and interactive effects of a nonclinical panic attack history and distress tolerance in relation to PTSD symptoms. The sample consisted of 91 adults (62.6% women; Mage = 23.45, SD = 9.56) who met DSM-IV criteria for trauma exposure, 53.8% of whom met criteria for a recent (past two years) history of nonclinical panic attacks. Results indicated that distress tolerance, as measured by the Distress Tolerance Scale (Simons & Gaher, 2005), was significantly related to all PTSD symptom clusters, and a nonclinical panic attack history was significantly related to PTSD re-experiencing and hyperarousal symptoms. The interaction of a nonclinical panic attack history and distress tolerance significantly predicted unique variance in only PTSD hyperarousal symptoms. Implications and future directions are discussed for the role of nonclinical panic attacks and distress tolerance in PTSD symptom expression.
Keywords: PTSD, distress tolerance, panic attacks, anxiety
Panic attacks, which reflect a discrete fear response (Barlow, 2002), play an important role in understanding various anxiety and other psychological disorders. For example, in addition to being a defining feature of panic disorder (American Psychiatric Association, 1994), panic attacks are a risk marker for a relatively broad range of psychopathological conditions, such as anxiety disorders (Reed & Wittchen, 1998), major depressive disorder (Bittner et al., 2004), substance use disorders (Baillie & Rapee, 2005), and psychotic disorders (Goodwin, Fergusson, & Horwood, 2004). Furthermore, panic attacks, even those that are “nonclinical” (i.e., experienced out of the context of panic disorder), can be personally distressing and are associated with significant levels of life disruption (Norton, Cox, & Malan, 1992).
One growing line of scientific inquiry has sought to explicate the role of panic attacks in regard to posttraumatic stress disorder (PTSD) sequale (Falsetti & Resnick, 1997). Specifically, numerous scholars have suggested that trauma exposure can result in an increased propensity to experience panic attacks, which in turn, may play a formative role in the maintenance of arousal and development of posttraumatic stress disorder (PTSD; Falsetti & Resnick, 2000; Falsetti, Resnick, Dansky, Lydiard, & Kilpatrick, 1995; Hinton, Hofmann, Pitman, Pollack, & Barlow, 2008; Jones & Barlow, 1990). The empirical literature is consistent with a panic attack-PTSD association. For example, 69% of individuals with PTSD met criteria for panic attacks among a treatment-seeking sample (Falsetti & Resnick, 1997). Similarily, Resnick, Falsetti, Kilpatrick, and Foy (1994) found that 90% of rape victims assessed within 72 hours after the assault met full criteria for panic attacks during that same time frame; a finding consistent in individuals who experienced non-sexual trauma (e.g., Bryant & Panasetis, 2001). Other work has found significant relations between heightened anxious arousal during trauma exposure and increased frequency of panic attacks post-trauma (Nixon, Resick, & Griffin, 2004). Similarly, panic attacks experienced during traumatic events have been found to be associated with an increased risk of more intense PTSD symptoms post-trauma exposure (Galea et al., 2002).
Despite empirical evidence of a panic attack-PTSD association, a number of formative limitations characterizes this corpus of work. First, little is known about the specific PTSD symptoms to which panic attacks may be related. Understanding links between panic attacks and specific PTSD symptom clusters may be important in understanding the potential underlying processes linking these clinical problems. For example, integrative theories regarding panic-PTSD symptom co-occurrence suggest that panic attacks may be linked to specific PTSD symptoms due to a fear conditioning process (e.g., Hinton et al., 2008). For instance, panic attack symptoms (e.g., increased heart rate) may become interoceptive triggers for PTSD symptoms, such as re-experiencing and hyperarousal, due to associations developed during traumatic events (Hinton et al., 2008; Jones & Barlow, 1990). According to this type of perspective, panic attacks may be particularly relevant to the re-experiencing and hyperarousal symptoms among trauma exposed persons; and yet, empirical work documenting this putative association is lacking.
Second, there has been a lack of integration of other relevant risk candidates in the panic-trauma context. In one relevant study, Vujanovic, Zvolensky, and Bernstein (2008) found significant relations between anxiety sensitivity (the fear of anxiety and related sensations) lower order factors and both panic symptoms and PTSD symptoms; however, these factors were not integrated into one overarching model. Distress tolerance, defined as the perceived and/or actual behavioral capacity to withstand exposure to aversive or threatening experiential states (e.g., negative emotions, uncomfortable physical sensations; Brown, Lejuez, Kahler, Strong, & Zvolensky, 2005; Simons & Gaher, 2005), is one promising cognitive-affect factor for better understanding the nature of the panic-PTSD co-occurrence. Lower levels of perceived distress tolerance for negative emotional states are related to greater levels of PTSD symptoms (Vujanovic, Bonn-Miller, Potter, Marshall, & Zvolensky, under review), even when considered in the context of other measures of behavioral and self-reported distress tolerance constructs (Marshall-Berenz, Vujanovic, Bonn-Miller, Bernstein, & Zvolensky, in press). With regard to panic attack-trauma relations, individuals with lower levels of distress tolerance who also have a panic attack history may be more likely to manifest PTSD symptoms. That is, lower levels of perceived tolerance for emotional distress, including trauma-related distress, in conjunction with a higher overall relative risk for anxious hyperarousal (i.e., history of panic attacks), may increase the probability of more severe PTSD symptoms. Individuals experiencing intense episodes of negative emotion (i.e., panic attacks) who perceive that they cannot tolerate such distress may interpret distressing symptoms as more severe, thereby increasing reactivity to such symptoms (e.g., greater hyperarousal) and increasing sensitivity to such symptoms (e.g., greater likelihood of re-experiencing symptoms). Conversely, higher levels of an actual or perceived ability to tolerate negative emotional states may attenuate relative risk for more severe PTSD symptoms.
Together, the current study investigated the main and interactive effects of a recent (past two year) unexpected, nonclinical panic attack history (i.e., panic attacks were experienced as “out of the blue” and did not qualify for panic disorder) and distress tolerance, as assessed by the Distress Tolerance Scale (DTS; Simons & Gaher, 2005), in relation to PTSD symptom severity (total symptoms, as well as 4-factor symptom clusters) among individuals with a history of trauma exposure. This study was predicated on three interrelated sets of hypotheses. First, it was hypothesized that the main effect of DTS - total score would be significantly related to PTSD symptom clusters,a finding that would be consistent with past empirical work (Marshall-Berenz et al., in press; Vujanovic et al., under review). Second, it was hypothesized that the main effect of a nonclinical panic attack history would be significantly related to re-experiencing and hyperarousal PTSD symptom clusters, a finding that would be consistent with existing theory but would provide a novel contribution to the panic-PTSD literature (Hinton et al., 2008). Finally, it was hypothesized that the significant main effects would be qualified by a significant interaction between the DTS - total score and a nonclinical panic attack history in terms of re-experiencing and hyperarousal PTSD symptom clusters, a finding that would provide a novel contribution to the literature. In all instances, the hypothesized significant effects were expected to be evident above and beyond the variance accounted for by the number of experienced traumas.
Method
Participants
Advertisements for a study on emotion were distributed via fliers in commonly visited areas of Burlington, VT (e.g., downtown, college campuses) and local newspaper advertisements. Participants were 91 adults (62.6% women; Mage = 23.45, SD = 9.56) who met the DSM-IV-TR PTSD Criterion A1 (the event “involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others”; APA, 2000, p. 467) and Criterion A2 (the trauma response “involved intense fear, helplessness, or horror”; APA, 2000, p. 467). Consistent with the Vermont state population (State of Vermont, Department of Health, 2007), approximately 96.7% of the sample identified as white/Caucasian, 1.1% as Hispanic/Latino, 1.1% as Asian, and 1.1% as Biracial. With regard to educational status, approximately 63.7% reported completing some college, 19.8% reported completing high school/GED, 8.8% reported completing college, 5.5% reported attaining a graduate degree, and 2.2% reported attaining less than a high school degree.
Measures
Structured Clinical Interview for DSM-IV – Non-patient Version
(SCID-I/NP; First et al., 1995). The SCID-I/NP was administered (1) to assess whether participants met criteria for a recent (past two years) nonclinical history of unexpected panic attacks (i.e., panic attacks outside of the context of panic disorder that are perceived as occurring “out of the blue”), as well as current (past month or past six months for substance dependence) psychopathology, and (2) to assess for current suicidal ideation. The SCID-I/NP has evidenced adequate inter-rater and test-retest reliability for anxiety and mood diagnoses (Zanarini et al., 2000). In the present study, each SCID-I/NP administration was reviewed by the PI to ensure inter-rater agreement on symptom coding and diagnoses.
Clinician-Administered PTSD Scale
(CAPS; Blake et al., 1995). The CAPS was employed to measure the frequency and intensity of current (past month) PTS symptoms as well as to assess current (past month) PTSD diagnostic status. All individuals met the DSM-IV-TR PTSD Criterion A1 (the event “involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others”; APA, 2000, p. 467) and Criterion A2 (the trauma response “involved intense fear, helplessness, or horror”; APA, 2000, p. 467). The CAPS Life Events Checklist was used to index number of traumatic events; all degrees of exposure (i.e., “happened to me,” “witnessed it,” “learned about it”) were included to comprise a comprehensive index of perceived past life traumatic stressors (i.e., number of past traumas variable). All events endorsed on the Life Events Checklist are not assessed for Criterion A status. Past work has found that the Life Events Checklist has good test-retest reliability, good convergent validity with the Traumatic Life Events Checklist (Kubany et al., 2000), and significant relations with PTSD symptom severity (Gray, Litz, Hsu, & Lombardo, 2004). Consistent with prior research (e.g., Monson et al., 2006), symptom severity was defined as the sum of the frequency and intensity items on the CAPS. The CAPS is considered a “gold standard” for indexing PTSD diagnostic status as well as symptom severity and has demonstrated excellent psychometric properties (Weathers, Keane, & Davidson, 2001). In the present study, each CAPS administration was conducted by trained clinical assessors and reviewed by the PI to ensure agreement on PTSD symptom ratings and diagnosis.
Distress Tolerance Scale
(DTS; Simons & Gaher, 2005). The DTS is a 15-item self-report measure, on which respondents indicate, on a 5-point Likert-type scale (1 = “strongly agree” to 5 = “strongly disagree”), the extent to which they believe they can experience and withstand distressing emotional states (Simons & Gaher, 2005). The DTS encompasses four types of emotional distress items including: perceived ability to tolerate emotional distress (e.g., “I can’t handle feeling distressed or upset”), subjective appraisal of distress (e.g., “My feelings of distress or being upset are not acceptable”), attention being absorbed by negative emotions (e.g., “When I feel distressed or upset, I cannot help but concentrate on how bad the distress actually feels”), and regulation efforts to alleviate distress (e.g., “When I feel distressed or upset I must do something about it immediately;” Simons & Gaher, 2005). High levels of distress tolerance are indicated by higher scores on the DTS. The DTS has evidenced convergent validity with measures assessing emotion regulatory processes (Simons & Gaher, 2005). As in past work (e.g., Anestis, Selby, Fink, & Joiner, 2007), the total DTS score (α = .94) was employed as a global index of perceived distress tolerance.
Panic Attack Questionnaire – IV
(PAQ-IV; Norton et al., 2008). The PAQ-IV is a self-report measure, which assesses qualitative and quantitative facets of panic attack symptoms and relevant correlates. Specifically, the PAQ-IV indexes family history of panic attacks; frequency and severity of current panic attacks; severity ratings from 0 (“does not occur”) to 4 (“very severe”) of symptoms of the “typical” panic attack, “most recent” panic attack, and “worst ever” panic attack; likelihood of experiencing panic attacks in various situations; likelihood of avoiding certain situations/places out of fear of having another panic attack; and interference/distress ratings. The PAQ-IV was used in the current study as a descriptive measure of panic attack history (e.g., age of onset, frequency of panic attacks).
Panic Disorder Severity Scale
(PDSS; Shear et al., 1997, 2001). The PDSS is a semi-structured, 7-item clinical interview, designed to assess panic disorder symptom severity, which assesses frequency and severity of panic attacks, anticipatory anxiety, panic-relevant avoidance, and related life impairment. The 7 items are rated on a Likert-type scale from 0 (“none”) to 4 (“extreme;” Shear et al., 1997). The PDSS has evidenced adequate inter-rater and test-retest reliability (r = .71), as well as high internal consistency (α = .88; Shear et al., 2001). Individuals with panic disorder tend to score significantly higher on the PDSS than individuals without PD (Shear et al., 2001). The PDSS total score (α = .80) for past-month symptom severity was utilized as a descriptive measure of current severity within the positive panic attack group.
Procedure
The current study data were collected as part of a larger laboratory investigation examining cognitive risk factors among individuals with and without a recent history of nonclinical, unexpected panic attacks. Interested participants were scheduled for a session in the laboratory to determine eligibility and collect study data. Upon arrival to the laboratory, interested participants first provided informed consent. The SCID-I/NP was then administered to determine eligibility and nonclinical panic attack history status based on the criteria identified above. Eligible participants were administered the CAPS and completed a battery of self-report measures. An initial 154 participants were enrolled in the primary study after a brief phone screen, of which 5 (3.2%) participants were ruled out at the baseline session. Of the 149 eligible participants, 91 (61.1%) met Criterion A for trauma exposure and past-month alcohol use and were thus included in the current study. Participants were compensated $30 for their involvement with the entire study; ineligible participants were compensated $10 for participating in the SCID-I/NP administration.
Data-Analytic Plan
A series of hierarchical multiple regressions was conducted to test the study hypotheses. Following the recommendations of Aiken and West (1991), the number of traumas endorsed on the Life Events Checklist of the CAPS and the main effects of DTS total score (mean-centered) and nonclinical panic attack history (dichotomous variable derived from the SCID-N/P) were entered into step one of the regression, and the DTS - total score by nonclinical panic attack history interaction term was entered into step two of the regression. The five criterion variables included past-month (1) CAPS – Total symptom severity, (2) CAPS – Re-experiencing symptom severity, (3) CAPS – Avoidance symptom severity, (4) CAPS – Emotional Numbing symptom severity, and (5) CAPS – Hyperarousal symptom severity. Based on recommendations of Cohen and Cohen (1983; pp. 323, 419), the forms of significant interactions were examined graphically by inserting specific values for each predictor variable (1/2 SD above and below the mean, in the current study) into the regression equation associated with the described analysis.
Results
Participant Characteristics
48.4% of the sample met criteria for current (past month) axis I psychopathology, not including nonclinical panic attacks. Participants endorsing current psychopathology met criteria for an average of 2.20 (SD = 1.53) diagnoses. Specifically, 18.7% of the total sample met current (past month) criteria for Social Anxiety Disorder, 16.5% met criteria for Generalized Anxiety Disorder, 11.0% met criteria for Specific Phobia, 8.8% met criteria for Dysthymia, 7.7% met criteria for Major Depressive Disorder, 4.4% met criteria for Posttraumatic Stress Disorder, 4.4% met criteria for Obsessive Compulsive Disorder, 2.2% met criteria for Eating Disorder Not Otherwise Specified, and 1.1% met criteria for Bipolar II Disorders. With regard to current (past 6 months) substance use disorders, 6.7% of the sample met criteria for alcohol abuse, 7.8% met criteria for alcohol dependence, 7.7% met criteria for cannabis abuse, 6.6% met criteria for cannabis dependence, and 1.1% met criteria for amphetamine dependence. 53.8% of the sample met criteria for a nonclinical panic attack history on the SCID-I/NP and were categorized as having a “positive” panic attack history. See Table 1 for descriptive statistics relevant to panic attack history within the positive panic attack group.
Table 1.
Positive Panic Attack Group Characteristics
| Variable | Mean or % | SD |
|---|---|---|
| Age of Onset of Panic Attacksa | 18.27 | 7.20 |
| Number of Years Experiencing Panic Attacksa | 4.85 | 5.10 |
| Number of Panic Attacks in Past Yeara | 7.16 | 9.28 |
| Duration of “Typical” Panic Attacka | ||
| Less than 10 minutes | 58.5% | |
| 10-30 minutes | 36.6% | |
| 30-60 minutes | 4.9% | |
| Panic Disorder Severity Scale (PDSS) - Total Scoreb | 5.80 | 4.94 |
Note: Descriptive statistics conducted among participants endorsing a positive panic attack history
Assessed with Panic Attack Questionnaire (Norton et al., 2008)
PDSS total score < 8 indicates sub-clinical panic disorder symptoms (i.e., PDSS score < 8; Shear et al., 2001).
All participants in the current study endorsed at least one traumatic event on the Life Events Checklist of the CAPS (Blake et al., 1995), with participants reporting an average of 7.77 (SD = 5.98) lifetime traumatic events. With regard to participants’ “worst” traumatic event, 21.1% endorsed a sudden, unexpected death; 15.6% endorsed a transportation accident; 13.3% endorsed a sexual assault; 11.1% endorsed a life threatening illness/serious injury; 6.7% endorsed a sudden, violent death; 5.6% endorsed a physical assault; 5.6% endorsed a serious accident at home or work; 4.4% endorsed an unwanted sexual experience; 3.3% endorsed a natural disaster; 1.1% endorsed a fire or explosion; 1.1% endorsed assault with a weapon; 1.1% endorsed severe human suffering; and 10.0% endorsed an “other” traumatic event. Participants scored an average of 14.12 (SD = 17.25; Range = 0-66) on CAPS severity ratings (frequency + intensity), indicating generally low levels of PTSD symptom severity (e.g., minimum score of 45 reliably corresponds to PTSD diagnosis; Weathers, Ruscio, & Keane, 1999), with 4.4% (n = 4) of participants meeting criteria for a current (past month) PTSD diagnosis.
Descriptive Statistics and Zero-Order (Pearson) Correlations
See Table 2 for descriptive statistics and zero-order correlations for the key study variables. The covariate of number of traumas was significantly positively related to CAPS total symptom severity, Re-experiencing symptom severity, and Emotional Numbing symptom severity (rs = .22, .24, and .21, respectively). DTS total score and nonclinical panic attack group (dichotomously coded: 0 = no history, 1 = past two year history) were significantly negatively correlated (r = −.40), with individuals endorsing a nonclinical panic attack history reporting lower levels of distress tolerance. Both nonclinical panic attack history and DTS total score were significantly correlated with CAPS total symptom severity (r’s = .37 and −.40, respectively), Re-experiencing symptom severity (r’s = .31 and −.32, respectively), Emotional Numbing symptom severity (r’s = .29 and −.32, respectively), and Hyperarousal symptom severity (r’s = .40 and −.38, respectively), such that a nonclinical panic attack history and lower levels of distress tolerance were related to greater traumatic stress symptom severity. DTS total score, but not a nonclinical panic attack history, was significantly negatively correlated with CAPS Avoidance symptom severity (r = −.28), such that lower levels of distress tolerance were related to greater Avoidance symptom severity.
Table 2.
Descriptive Statistics and Zero-Order Correlations for Study Variables
| Variable1 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | Mean (SD) or % |
|---|---|---|---|---|---|---|---|---|---|
| 1. Panic Group (% positive) |
1 | −.40** | .09 | .37** | .31** | .17 | .29** | .40** | 53.8% |
| 2. DTS - Total | 1 | −.07 | −.40** | −.32** | −.28** | −.32** | −.38** | 3.29 (.96) |
|
| 3. Number of Traumas |
1 | .22* | .24* | .17 | .21* | .14 | 7.77 (5.98) |
||
| 4. CAPS – Total Symptom Severity |
1 | .88** | .76** | .82** | .86** | 14.12 (17.25) |
|||
| 5. CAPS – Re- experiencing Symptom Severity |
1 | .72** | .60** | .62** | 4.75 (5.81) |
||||
| 6. CAPS – Avoidance Symptom Severity |
1 | .55** | .50** | 1.77 (2.69) |
|||||
| 7. CAPS – Emotional Numbing Symptom Severity |
1 | .58** | 3.07 (5.24) |
||||||
| 8. CAPS – Hyperarousal Symptom Severity |
1 | 4.54 (6.77) |
Note:
p < .05
p < .01
Panic Group (dichotomous variable): Nonclinical Panic Attack History, Past 2 Years (SCID; First et al., 1995); DTS – Total: Distress Tolerance Scale – Total Score (Simons & Gaher, 2005); Number of Traumas: Total Number of Traumas endorsed, CAPS – Life Events Checklist; CAPS – Total Posttraumatic Stress Symptom Severity (frequency + intensity); CAPS – Total Re-Experiencing Symptom Cluster Severity (frequency + intensity); CAPS – Total Avoidance Symptom Cluster Severity (frequency + intensity); CAPS – Emotional Numbing Symptom Cluster Severity (frequency + intensity); CAPS – Hyperarousal Symptom Cluster Severity (frequency + intensity; Blake et al., 1995).
Regression Results
See Table 3 for hierarchical multiple regression results. The proposed model significantly predicted CAPS – total symptom severity (F(4, 90) = 7.78, p < .001). At step 1, number of traumas (t = 1.93, β = .18, sr2 = .03, p = .05), DTS – Total score (t = −2.83, β = −.29, sr2 = .07, p < .01), and nonclinical panic attack history (t = 2.39, β = .24, sr2 = .05, p < .05) were significant predictors. The interactive effect at step 2 was not significant.
Table 3.
Hierarchical Regression Analyses: Distress Tolerance, Panic Group Status, and Posttraumatic Stress
| ΔR2 | t | β | sr2 | p | |
|---|---|---|---|---|---|
| Criterion Variable: CAPS – Total Symptom Severity | |||||
| Step 1 | .25 | < .001 | |||
| Number of Traumas | 1.93 | .18 | .03 | .05 | |
| DTS – Total | −2.83 | −.29 | .07 | < .01 | |
| Panic Group | 2.39 | .24 | .05 | < .05 | |
| Step 2 | .02 | ns | |||
| Number of Traumas | 1.98 | .18 | .03 | .05 | |
| DTS – Total | .56 | .18 | .00 | ns | |
| Panic Group | 2.36 | .24 | .05 | < .05 | |
| DTS – Total x Panic Group | −1.57 | −.49 | .02 | ns | |
| Criterion Variable: CAPS – Re-Experiencing Symptom Severity | |||||
| Step 1 | .18 | .001 | |||
| Number of Traumas | 2.08 | .20 | .04 | < .05 | |
| DTS – Total | −2.10 | −.22 | .04 | < .05 | |
| Panic Group | 1.93 | .21 | .04 | .05 | |
| Step 2 | .03 | ns | |||
| Number of Traumas | 2.14 | .21 | .04 | < .05 | |
| DTS – Total | .89 | .29 | .01 | ns | |
| Panic Group | 1.91 | .20 | .03 | ns | |
| DTS – Total x Panic Group | −1.66 | −.54 | .03 | ns | |
| Criterion Variable: CAPS – Avoidance Symptom Severity | |||||
| Step 1 | .11 | < .05 | |||
| Number of Traumas | 1.35 | .14 | .02 | ns | |
| DTS – Total | −2.37 | −.26 | .06 | < .05 | |
| Panic Group | .55 | .06 | .00 | ns | |
| Step 2 | .00 | ns | |||
| Number of Traumas | 1.36 | .14 | .02 | ns | |
| DTS – Total | −.34 | −.13 | .00 | ns | |
| Panic Group | .53 | .06 | .00 | ns | |
| DTS – Total x Panic Group | −.40 | −.14 | .00 | ns | |
| Criterion Variable: CAPS – Emotional Numbing Symptom Severity | |||||
| Step 1 | .16 | .001 | |||
| Number of Traumas | 1.75 | .17 | .03 | ns | |
| DTS – Total | −2.24 | −.24 | .05 | < .05 | |
| Panic Group | 1.69 | .18 | .03 | ns | |
| Step 2 | .00 | ns | |||
| Number of Traumas | 1.75 | .17 | .03 | ns | |
| DTS – Total | −.54 | −.18 | .00 | ns | |
| Panic Group | 1.68 | .18 | .03 | ns | |
| DTS – Total x Panic Group | −.19 | −.06 | .00 | ns | |
| Criterion Variable: CAPS – Hyperarousal Symptom Severity | |||||
| Step 1 | .23 | < .001 | |||
| Number of Traumas | 1.01 | .10 | .01 | ns | |
| DTS – Total | −2.59 | −.27 | .06 | .01 | |
| Panic Group | 2.73 | .28 | .07 | < .01 | |
| Step 2 | .04 | < .05 | |||
| Number of Traumas | 1.08 | .10 | .01 | ns | |
| DTS – Total | 1.30 | .41 | .01 | ns | |
| Panic Group | 2.73 | .27 | .06 | < .01 | |
| DTS – Total x Panic Group | −2.28 | −.71 | .04 | < .05 | |
Note: β = standardized beta weight; sr2 = Squared semi-partial correlation; CAPS – Total Posttraumatic Stress Symptom Severity (frequency + intensity); CAPS – Total Re-Experiencing Symptom Cluster Severity (frequency + intensity); CAPS – Total Avoidance Symptom Cluster Severity (frequency + intensity); CAPS – Emotional Numbing Symptom Cluster Severity (frequency + intensity); CAPS – Hyperarousal Symptom Cluster Severity (frequency + intensity); Total Number of Traumas endorsed, CAPS – Life Events Checklist (Blake et al., 1995); Distress Tolerance Scale – Total Score (Simons & Gaher, 2005); Panic Group (dichotomous variable): Nonclinical Panic Attack History, Past 2 Years (SCID; First et al., 1995)
The model significantly predicted CAPS – Re-experiencing symptom severity (F(4, 90) = 5.63, p < .001). At step 1, number of traumas (t = 2.08, β = .20, sr2 = .04, p < .05), DTS – Total score (t = −2.10, β = −.22, sr2 = .04, p < .05), and nonclinical panic attack history (t = 1.93, β = .21, sr2 = .04, p = .05) were significant predictors. There was no significant interaction effect at step 2 of the model.
The model significantly predicted CAPS – Avoidance symptom severity (F(4, 90) = 2.70, p < .05). At step 1, DTS – Total score was the only significant predictor (t = −2.37, β = −.26, sr2 = .06, p < .05). There was no significant interactive effect at step 2 in the model.
The model significantly predicted CAPS – Emotional Numbing symptom severity (F(4, 90) = 4.29, p < .01). At step 1, DTS – Total score (t = −2.24, β = −.24, sr2 = .05, p < .05) was the only significant predictor. There was no significant interactive effect at step 2 in the model.
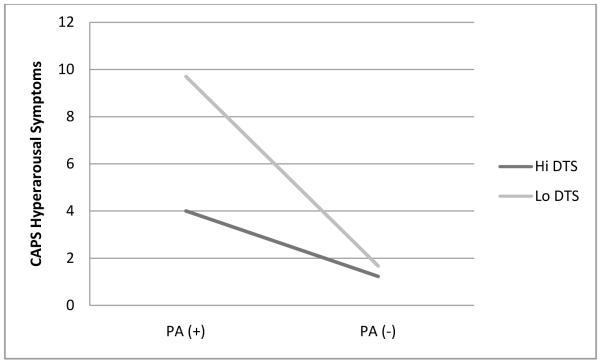
The model significantly predicted CAPS – Hyperarousal symptom severity (F(4, 90) = 7.96, p < .001). At step 1, DTS – Total score (t = −2.59, β = −.27, sr2 = .06, p = .01) and nonclinical panic attack history (t = 2.73, β = .28, sr2 = .07, p < .01) were significant predictors. At step 2, the DTS – Total by nonclinical panic attack history interactive effect was significant (t = −2.28, β = −.71, sr2 = .04, p < .05). Based on recommendations of Cohen and Cohen (1983; pp. 323, 419), the form of the significant interaction was examined graphically by inserting specific values for each predictor variable (1/2 SD above and below the mean, in the current study) into the regression equation associated with the described analysis. It was observed that individuals with a history of nonclinical panic attacks with the lowest levels of distress tolerance reported the greatest Hyperarousal symptom severity. Please see Figure 1 for a graphic representation of the observed interaction.
Figure 1.
Interactive effects of distress tolerance and panic attack status in predicting CAPS hyperarousal symptoms
Note: Based on recommendations of Cohen and Cohen (1983; pp. 323, 419), the form of the significant interaction was examined graphically by inserting specific values for each predictor variable (1/2 SD above and below the mean, in the current study) into the regression equation associated with the described analysis. “PA(+)” – Recent (past two years) history of nonclinical panic attacks; “PA(−)” – No history of panic attacks; “Hi DTS” – 1/2 SD above the sample mean on the Distress Tolerance Scale (Simons & Gaher, 2005); “Lo DTS” – 1/2 SD below the sample mean on the Distress Tolerance Scale; “CAPS Hyperarousal Symptoms” – Hyperarousal traumatic stress symptom severity endorsed on the Clinician Administered PTSD Scale (Blake et al., 1995).
Discussion
There is limited research on the vulnerability processes underlying the co-occurrence of panic attack-PTSD relations. The current study investigated the main and interactive effects of a recent (past two year) nonclinical panic attack history and distress tolerance in relation to PTSD symptom severity among trauma-exposed individuals. It was hypothesized that the main effects of distress tolerance and panic attack history would be related to PTSD total and symptom cluster symptom severity and that the interaction of these variables would be significantly related to PTSD re-experiencing and hyperarousal symptoms.
First, as hypothesized, the main effect of distress tolerance was significantly related to total PTSD symptoms, as well as all PTSD symptom clusters. This effect is consistent with past work documenting distress tolerance-PTSD relations (Marshall-Berenz et al., in press; Vujanovic et al., under review). Generally, it is possible that individuals who perceive a diminished ability to cope with or tolerate negative emotions are more likely to avoid such states, thereby perpetuating and exacerbating their perceived threat. Similarly, individuals with lower levels of distress tolerance may hold perceptions that they are ill-equipped to cope with emotional distress, and such perceptions may impede their abilities to regulate PTSD symptoms following trauma (Ehlers & Clark, 2000; Vujanovic, Bernstein, & Litz, in press). Alternatively, PTSD symptoms may disrupt certain individuals’ abilities to cope with emotional distress and predispose them to develop even higher levels of PTSD symptoms following trauma (Vujanovic et al., in press). Future work may benefit from investigating, longitudinally, temporal order of, and potential interactive effects between, distress tolerance and degree of trauma exposure in relation to PTSD symptoms. These proposed theoretical mechanisms are clinically noteworthy, as lower levels of distress tolerance may interfere with an individual’s willingness to engage in the emotional and cognitive processing of distressing trauma-related memories and emotions, possibly undermining their ability to engage successfully in trauma-focused treatment (e.g., Foa et al., 2005; Resick & Schnicke, 1992). Further work is needed to better understand the mechanisms linking perceived distress tolerance and PTSD symptoms.
Second, as hypothesized, the main effect of a nonclinical panic attack history was significantly related to PTSD symptom severity and evidenced unique relations with the re-experiencing and hyperarousal PTSD symptom clusters. These findings are broadly in line with integrative theoretical models that posit panic symptoms experienced at the time of a traumatic event promote links between panic attacks/symptoms and traumatic memories and further arousal post-trauma exposure (Hinton et al., 2008; Jones & Barlow, 1990). The current study measured panic attack histories, but it did not include a method for explicating whether or not the panic attacks were related to trauma per se. Thus, it is not possible to isolate the precise nature of the panic attack experience and trauma exposure. Nonetheless, present findings suggest that a recent history of nonclinical panic attacks, after adjusting for trauma exposure history, is significantly related to certain aspects of PTSD symptoms. Further work is therefore needed to delineate these relations, particularly investigations utilizing longitudinal designs.
Third, only partially consistent with hypothesis, the interaction of a nonclinical panic attack history and distress tolerance was significantly related to hyperarousal PTSD symptoms, but no other PTSD symptom clusters. The form of the interaction indicated that individuals low in perceived distress tolerance with a recent history of panic attacks evidenced the greatest level of PTSD hyperarousal symptoms. This finding may indicate that a trauma-exposed individual who has lower levels of perceived distress tolerance for negative emotionality – potentially triggered by trauma-related internal or external cues - and who is also at high risk for experiencing anxious hyperarousal (i.e., history of nonclinical panic attacks) may be particularly prone to experiencing certain clusters of PTSD symptoms. Based upon the current cross-sectional findings, it may be advisable to ascertain whether the interactive effects observed in the present study are evident over time among a trauma-exposed sample.
Although not the primary aim of the investigation, another observation warrants brief comment. A nonclinical panic attack history and distress tolerance evidenced a significant negative correlation, underscoring a novel association between panic history and distress tolerance among a trauma-exposed sample. Further, these variables shared only 16% of variance with one another, indicating that these two factors are tapping different, albeit related, types of vulnerability processes for the expression of PTSD symptoms.
Present findings suggest that there is possible merit in focusing scientific attention on the main and interactive effects of nonclinical panic attacks and distress tolerance in regard to understanding the expression of PTSD symptoms. Overall, perhaps the main implication of the present findings is that while both studied factors are theorized to be central explanatory constructs in models of PTSD vulnerability, they appear to be independent, unique contributing factors. From a prevention/early intervention standpoint, it may, therefore, be clinically useful to target both factors in the identification of trauma-exposed individuals at heightened risk for developing PTSD (Zvolensky, Schmidt, Bernstein, & Keough, 2006). Further research is necessary to determine whether perceived distress tolerance and panic attacks are risk factors for versus the result of PTSD symptoms. From an etiological perspective, the findings also suggest that a continued emphasis on understanding the roles of a panic attack history and distress tolerance in the pathogenesis of PTSD following trauma is a worthwhile pursuit. For example, there may be utility in exploring possible mediation processes among the variables studied (e.g., possible mediation effects of nonclinical panic attack history on the relation between trauma exposure and PTSD symptom severity among trauma-exposed persons). With regard to clinical significance of the current findings, it seems to be the case that trauma-exposed individuals who experience panic attacks and report low levels of peceived distress tolerance experience greater severity of hyperarousal PTSD symptoms. It is possible that treatment of panic attack symptoms among individuals experiencing hyperarousal symptoms would lead to improvements in these symptoms. Similarly, it is possible that installation of distress tolerance skills in treatment efforts (e.g., distress tolerance module of DBT; Linehan, 1993) may lead to improvements in PTSD symptoms. Further research is necessary to understand the effects of treating one of these conditions on the others.
There are several limitations to consider regarding the current study. First, the study utilized cross-sectional measurement. As such, causality and chronology of the current findings cannot be determined. Future work would greatly benefit from incorporating longitudinal designs. Second, the current sample, despite having high rates of psychopathology, reported relatively low levels of PTSD symptoms. Replication and extension of the current findings among individuals with a PTSD diagnosis is recommended. Third, the study relied on participants’ verbal or written self-reports of symptoms and distress tolerance. Future work might consider employing multi-dimensional approaches to this area of study to replicate and extend current findings. Fourth, the current study examined self-reported distress tolerance, but no other tolerance or sensitivity factors, in relation to PTSD symptoms. Future work would benefit from using larger samples to integrate distress tolerance with other related factors, such as anxiety sensitivity (e.g., Bernstein, Zvolensky, Vujanovic, & Moos, 2009), in the investigation of panic attack history and PTSD onset and maintenance. Finally, the time frame regarding participants’ trauma exposure and onset of panic attacks was not assessed in the current study. It might be especially important for future work to examine the chronology of these frequently co-occurring clinical problems, as well as how they influence one another over time.
Together, the current investigation examined the main and interactive effects of a nonclinical panic attack history and distress tolerance in relation to PTSD symptoms among trauma-exposed individuals. The current findings indicated that distress tolerance was significantly related to all PTSD symptom clusters, and a nonclinical panic attack history was significantly related to re-experiencing and hyperarousal PTSD symptoms. In addition, the interaction of a nonclinical panic attack history and distress tolerance was significantly related to hyperarousal PTSD symptoms.
Acknowledgments
This research was supported by a National Institute on Mental Health National Research Service Award (1 F31 MH080453-01A1) awarded to Erin C. Marshall. This research also was supported by National Institute on Health grants awarded to Dr. Michael Zvolensky (1 R01 DA027533-01; 1 R01 MH076629-01). The views expressed here are the authors’ and do not necessarily represent those of the Department of Veterans Affairs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Erin C. Marshall-Berenz, Department of Psychology, University of Vermont, Burlington, VT and Department of Psychiatry, University of Mississippi Medical Center/Jackson VA
Anka A. Vujanovic, National Center for PTSD - Behavioral Science Division, VA Boston Healthcare System and Boston University School of Medicine, Boston, MA
Michael J. Zvolensky, Department of Psychology, University of Vermont, Burlington, VT
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; Newbury Park, CA: 1991. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 1994. rev. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 2000. text revision. [Google Scholar]
- Anestis MD, Selby EA, Fink E, Joiner TE. The multifaceted role of distress tolerance in dysregulated eating behaviors. International Journal of Eating Disorders. 2007;40(8):718–726. doi: 10.1002/eat.20471. [DOI] [PubMed] [Google Scholar]
- Baillie AJ, Rapee RM. Panic attacks as risk markers for mental disorders. Social Psychiatry and Psychiatric Epidemiology. 2005;40:240–244. doi: 10.1007/s00127-005-0892-3. [DOI] [PubMed] [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2nd ed. Guilford Press; New York: 2002. [Google Scholar]
- Bittner A, Goodwin RD, Wittchen H, Beesdo K, Hofler M, Lieb R. What characteristics of primary anxiety disorders predict subsequent major depressive disorder? Journal of Clinical Psychiatry. 2004;65:618–626. doi: 10.4088/jcp.v65n0505. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. Journal of Abnormal Psychology. 2002;111:180–185. [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR, Zvolensky MJ. Distress tolerance and early smoking lapse. Clinical Psychology Review. 2005;25:713–733. doi: 10.1016/j.cpr.2005.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant RA, Panasetis P. Panic symptoms during trauma and acute stress disorder. Behaviour Research and Therapy. 2001;39(8):961–966. doi: 10.1016/s0005-7967(00)00086-3. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. 2nd ed. Erlbaum; Hillsdale, NJ: 1983. [Google Scholar]
- Falsetti SA, Resnick HS. Frequency and severity of panic attack symptoms in a treatment seeking sample of trauma victims. Journal of Traumatic Stress. 1997;10(4):683–689. doi: 10.1023/a:1024810206381. [DOI] [PubMed] [Google Scholar]
- Falsetti S, Resnick H. Cognitive behavioral treatment of PTSD with comorbid panic attacks. Journal of Contemporary Psychotherapy. 2000;30:163–179. [Google Scholar]
- Falsetti S, Resnick H, Dansky B, Lydiard R, Kilpatrick D. The relationship of stress to panic disorder: Cause or effect? In: Mazure CM, editor. Does Stress Cause Psychiatric Illness? American Psychiatric Press; Washington, DC: 1995. pp. 111–147. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for Axis I DSM-IV Disorders. Biometrics Research Department; New York: 1994. [Google Scholar]
- Foa EB, Hembree EA, Cahill SP, Rauch SAM, Riggs DS, Feeny NC, et al. Journal of Consulting and Clinical Psychology. Vol. 73. 2005. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics; pp. 953–964. [DOI] [PubMed] [Google Scholar]
- Galea S, Resnick H, Ahern J, Gold J, Bucuvalas M, Kilpatrick D, Stuber J, Vlahov D. Posttraumatic stress disorder in Manhattan, New York City, after the September 11th terrorist attacks. Journal of Urban Health. 2002;79(3):340–353. doi: 10.1093/jurban/79.3.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin RD, Hamilton SP. Panic attack as a marker of core psychopathological processes. Psychopathology. 2001;34:278–288. doi: 10.1159/000049326. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Fergusson DM, Horwood LJ. Panic attacks and psychoticism. American Journal of Psychiatry. 2004;161:88–92. doi: 10.1176/appi.ajp.161.1.88. [DOI] [PubMed] [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11:330–341. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- Hinton DE, Hofmann SG, Pitman RK, Pollack MH, Barlow DH. The panic attack-posttraumatic stress disorder model: Applicability to orthostatic panic among Cambodian refugees. Cognitive Behaviour Therapy. 2008;37(2):101–116. doi: 10.1080/16506070801969062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones JC, Barlow DH. The etiology of PTSD. Clinical Psychology Review. 1990;10:299–328. [Google Scholar]
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, et al. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment. 2000;12:210–224. doi: 10.1037//1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Marshall-Berenz EC, Vujanovic AA, Bonn-Miller MO, Bernstein A, Zvolensky MJ. Multi-method study of distress tolerance and posttraumatic stress symptom severity in a trauma-exposed community sample. Journal of Traumatic Stress. doi: 10.1002/jts.20568. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, Stevens SP. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2006;74:898–907. doi: 10.1037/0022-006X.74.5.898. [DOI] [PubMed] [Google Scholar]
- Nixon RD, Resick PA, Griffin MG. Panic following trauma: The etiology of acute posttraumatic arousal. Journal of Anxiety Disorders. 2004;18(2):193–210. doi: 10.1016/S0887-6185(02)00290-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton GR, Cox BJ, Malan J. Nonclinical panickers: A critical review. Clinical Psychology Review. 1992;12:121–139. [Google Scholar]
- Norton PJ, Zvolensky MJ, Bonn-Miller MO, Cox BJ, Norton GR. Use of the Panic Attack Questionnaire-IV to assess non-clinical panic attacks and limited symptom panic attacks in student and community samples. Journal of Anxiety Disorders. 2008;22(7):1159–1171. doi: 10.1016/j.janxdis.2007.12.002. [DOI] [PubMed] [Google Scholar]
- Reed V, Wittchen H-U. DSM-IV panic attacks and panic disorder in a community sample of adolescents and young adults: How specific are panic attacks? Journal of Psychiatric Research. 1998;32(6):335–345. doi: 10.1016/s0022-3956(98)00014-4. [DOI] [PubMed] [Google Scholar]
- Resick PA, Schnicke MK. Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology. 1992;60:748–756. doi: 10.1037//0022-006x.60.5.748. [DOI] [PubMed] [Google Scholar]
- Resnick HS, Falsetti SA, Kilpatrick DG, Foy DW. Associations between panic attacks during rape assaults and follow-up PTSD or panic attack outcomes; 10th Annual Meeting of the International Society of Traumatic Stress Studies; Chicago, IL. 1994. [Google Scholar]
- Shear MK, Brown TA, Barlow DH, Money R, Sholomskas DE, Woods SW, Gorman JM, Papp LA. Multicenter collaborative panic disorder severity scale. The American Journal of Psychiatry. 1997;154(11):1571–1575. doi: 10.1176/ajp.154.11.1571. [DOI] [PubMed] [Google Scholar]
- Shear MK, Rucci P, Williams J, Frank E, Grochocinski V, Vander Bilt J, Houck P, Wang T. Reliability and validity of the Panic Disorder Severity Scale: Replication and extension. Journal of Psychiatric Research. 2001;35(5):293–296. doi: 10.1016/s0022-3956(01)00028-0. [DOI] [PubMed] [Google Scholar]
- Simons JS, Gaher RM. The distress tolerance scale: Development and validation of a self-report measure. Motivation and Emotion. 2005;29:83–102. [Google Scholar]
- State of Vermont, Department of Health Retrieved June 30, 2007, from http://www.healthyvermonters.info/
- Vujanovic AA, Bonn-Miller MO, Potter C, Marshall EC, Zvolensky MJ. An evaluation of the relation between distress tolerance and posttraumatic stress within a trauma-exposed sample. doi: 10.1007/s10862-010-9209-2. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walser R, Westrup D. Acceptance & Commitment Therapy for the Treatment of Post-Traumatic Stress Disorder & Trauma-Related Problems: A Practitioner’s Guide to Using Mindfulness & Acceptance Strategies. New Harbinger; Oakland, CA: 2007. [Google Scholar]
- Weathers FW, Keane TM, Davidson JR. Clinician-Administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety. 2001;13(3):132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychological Assessment. 1999;11(2):124–133. [Google Scholar]
- Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, et al. The longitudinal personality disorders study: Reliability of axis I and II diagnoses. Journal of Personality Disorders. 2000;14:291–299. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A, Vujanovic AA, editors. Distress Tolerance. Guilford Press; New York, NY: in press. [Google Scholar]
- Zvolensky MJ, Schmidt NB, Bernstein A, Keough ME. Risk-factor research and prevention programs for anxiety disorders: A translational research framework. Behaviour Research and Therapy. 2006;44(9):1219–1239. doi: 10.1016/j.brat.2006.06.001. [DOI] [PubMed] [Google Scholar]