Abstract
Context:
Although abnormal foot posture long has been associated with lower extremity injury risk, the evidence is equivocal. Poor intertester reliability of traditional foot measures might contribute to the inconsistency.
Objectives:
To investigate the validity and reliability of a digital photographic measurement method (DPMM) technology, the reliability of DPMM-quantified foot measures, and the concurrent validity of the DPMM with clinical-measurement methods (CMMs) and to report descriptive data for DPMM measures with moderate to high intratester and intertester reliability.
Design:
Descriptive laboratory study.
Setting:
Biomechanics research laboratory.
Patients or Other Participants:
A total of 159 people participated in 3 groups. Twenty-eight people (11 men, 17 women; age = 25 ± 5 years, height = 1.71 ± 0.10 m, mass = 77.6 ± 17.3 kg) were recruited for investigation of intratester and intertester reliability of the DPMM technology; 20 (10 men, 10 women; age = 24 ± 2 years, height = 1.71 ± 0.09 m, mass = 76 ± 16 kg) for investigation of DPMM and CMM reliability and concurrent validity; and 111 (42 men, 69 women; age = 22.8 ± 4.7 years, height = 168.5 ± 10.4 cm, mass = 69.8 ± 13.3 kg) for development of a descriptive data set of the DPMM foot measurements with moderate to high intratester and intertester reliabilities.
Intervention(s):
The dimensions of 10 model rectangles and the 28 participants' feet were measured, and DPMM foot posture was measured in the 111 participants. Two clinicians assessed the DPMM and CMM foot measures of the 20 participants.
Main Outcome Measure(s):
Validity and reliability were evaluated using mean absolute and percentage errors and intraclass correlation coefficients. Descriptive data were computed from the DPMM foot posture measures.
Results:
The DPMM technology intratester and intertester reliability intraclass correlation coefficients were 1.0 for each tester and variable. Mean absolute errors were equal to or less than 0.2 mm for the bottom and right-side variables and 0.1° for the calculated angle variable. Mean percentage errors between the DPMM and criterion reference values were equal to or less than 0.4%. Intratester and intertester reliabilities of DPMM-computed structural measures of arch and navicular indices were moderate to high (>0.78), and concurrent validity was moderate to strong.
Conclusions:
The DPMM is a valid and reliable clinical and research tool for quantifying foot structure. The DPMM and the descriptive data might be used to define groups in future studies in which the relationship between foot posture and function or injury risk is investigated.
Keywords: foot structure, reliability, pronation, pes planus, pes cavus
Key Points.
The digital photographic measurement method is a valid and reliable clinical and research tool for quantifying foot structure using the arch and navicular indices.
When used to quantify foot structure, the digital photographic measurement method might offer several advantages over traditional clinical-measurement methods.
The digital photographic measurement method is reliable for relatively inexperienced clinicians.
The digital photographic measurement method and the descriptive data might be used to define typical and abnormal foot-posture groups in future studies in which the relationship between foot posture and function or injury risk is investigated.
Researchers have conducted a plethora of studies of the relationship between foot posture and lower extremity injuries. Although many investigators have reported relationships between abnormal foot posture and lower extremity injury,1–4 others have not.5–8 An obvious source of inconsistency might be the different methods used to compute foot posture. A factor that is not obvious might be the low intertester reliability associated with many of the commonly used methods.9–15 Low intertester reliability could result in 2 researchers classifying the same foot differently. Furthermore, the clinical relevance of such studies might be limited because clinicians using the same measurement methods also could classify the same foot differently. Hence, the prerequisite step that must be accomplished before determining the relationship between static measures of foot posture and injury is development of measurement methods that have moderate to high intratester and intertester reliabilities.
A measurement method with moderate to high intratester and intertester reliabilities that also correlates strongly with radiographic measures is the arch index (AI).16 The AI is the ratio of the dorsum height of the foot at 50% of the total foot length to the truncated foot length computed during 10% or 90% weight-bearing (WB) conditions. Although the reliability of the AI is acceptable, there may be sources of error or variability associated with the currently used clinical-measurement method (CMM) that could be improved. When computing the AI in 90% WB, the positions of the most posterior point of the calcaneus, the end of the longest toe, the first metatarsophalangeal joint, and the dorsum height must be read as the participant maintains 90% WB on the limb. In addition, after measuring total foot length and before measuring dorsum height, 50% of the total foot length must be calculated and located. Attempting to rapidly take the various foot measurements as the participant maintains 90% WB might increase the likelihood of reading or recording errors. Furthermore, participants might shift their weight and alter foot posture during the measurement or recording process. Finally, dorsum-height measurements might be influenced by the degree to which the clinician compresses the soft tissue on the dorsal surface of the participant's foot.
To address some of these potential sources of error, several methods that quantify foot posture17,18 or mobility19 from digital images have been developed. Although all the methods are similar because they involve capturing a digital image of the foot, the postprocessing procedures differ. Postprocessing procedures include (1) printing the digital images followed by hand measuring of the anatomic landmarks,19 (2) printing the digital images followed by identifying anatomic landmarks with a digitizing tablet,17 and (3) uploading the digital images to software in which select anatomic landmarks are digitized.18 Although all have been reported to have moderate to high intratester and intertester reliabilities for at least some of the calculated foot measures, none appear to correct for perspective errors due to out-of-plane (in front of or behind the calibration frame) anatomic landmarks (ie, the most posterior portion of the calcaneus, the dorsum of the foot at 50% foot length, the tip of the hallux or longest toe). Furthermore, some require the use of custom hardware, such as a mirrored photo box18 or digitizing tablet,17 that might limit the clinical relevance of the methods.
To address the potential limitations of currently available digital foot-measurement methods, a new digital photographic measurement method (DPMM) was developed. The DPMM uses commercially available digital photography technology and a custom computer-software data acquisition and analysis algorithm. Advantages of the DPMM over traditional CMMs include elimination of soft tissue deformation, simultaneous computation of several anthropometric measures for the clinician, and quantification of several measures of foot posture from 1 digital image. The latter 2 advantages are also advantages of the DPMM over 2 of the 3 current digital methods, and the correction of perspective error is an advantage over all of the digital methods. In addition to the AI, the navicular index (NI)16 and longitudinal arch angle17,20 also might be calculated from 1 digital image. The NI and longitudinal arch angle both have been reported to have moderate to high intratester reliabilities but low intertester reliability.16,17 The advantages of the DPMM that we identified also might improve upon the intertester reliability of these measures. Furthermore, the ability to compute several different measures of foot posture from 1 image might be beneficial if subsequent studies reveal that a combination of static measures better predict injury risk (or dynamic function) than 1 measure. In addition to quantifying foot structure, measures of foot mobility, such as the relative arch deformity ratio (RAD),16 relative navicular mobility ratio (RNM) (calculated using the same algorithm as the RAD but with navicular height substituted for dorsum height), dorsum-height displacement, and navicular displacement, might be computed using data from the 10% and 90% WB conditions. However, the intratester and intertester reliabilities of the mobility measures using purely digital photographic measurement techniques have not been investigated.
Finally, because the data-acquisition and data-reduction procedures can be performed separately, the DPMM might be advantageous to the corresponding CMMs when large groups of individuals are examined (eg, preparticipation examinations). Data acquisition using the DPMM only requires identification of a select number of anatomic landmarks followed by the capture of a digital image of the individual's foot. Data reduction can be performed later when a participant's time is not a factor. When data reduction is performed, the ability to calculate all of the foot measures from 1 digital image using the DPMM allows the clinician or researcher to reduce the data more rapidly than when each measure is taken separately using the CMMs. Therefore, the purposes of our study were (1) to investigate the reliability and validity of the DPMM technology; (2) to investigate the intratester and intertester reliability of DPMM-quantified foot posture; (3) to investigate concurrent validity of the DPMM and CMM measures of AI, NI, longitudinal arch angle, RAD, RNM, dorsum-height displacement, and navicular-height displacement; and (4) to report descriptive data for the DPMM foot measures with moderate to high intratester and intertester reliabilities.
METHODS
DPMM Technology Validity
We evaluated the validity of the DPMM technology relative to the known dimensions of 10 rectangles (size range, 5.1 × 5.1 mm to 254.0 × 177.8 mm) constructed on the grid of 1 sheet of commercially available engineering graph paper. Two investigators (S.C.C., C.R.J.) measured the bottom and right sides of the constructed rectangles 3 times each to the nearest 0.1 mm using a standard ruler. The mean values of the manually measured lengths and the calculated angles between diagonal lines connecting the lower left and upper right corners and the bottom sides of the rectangles were defined as criterion reference values. We then obtained digital images of 2-dimensional rectangles mounted to a flat vertical surface using a 6.3-megapixel camera (FinePix S700; Fujifilm Corp, Tokyo, Japan). Before capturing the digital image of the objects, we positioned the camera 1 m from the data-analysis plane, leveled and squared it in 3 dimensions, and manually focused it. We placed a standard 30-cm ruler, which was oriented parallel to the horizontal edge of the graph paper, against the graph paper to allow calibration of the 2-dimensional plane. The digital camera conformed to the exchangeable image file format (Exif version 2.2 standard), which requires a 1-to-1 vertical-to-horizontal pixel aspect ratio. Therefore, calibration of the 2-dimensional plane was required only for 1 direction within the plane. After capture of the digital image, we used the DPMM software program (MATLAB version R2006b; The MathWorks, Inc, Natick, MA) to digitize 2 points on a reference object of known length captured in the photograph and the 4 corners of each rectangle. The software program used the digitized points on the reference object to scale the measurements of the rectangles. The algorithm also calculated the angle formed between the diagonal and the bottom side.
DPMM Technology Reliability
Participants
We evaluated intratester and intertester reliabilities of the DPMM technology via same-day test-retest measurements of the rectangles and of the feet of 28 participants (11 men, 17 women; age = 25 ± 5 years, height = 1.71 ± 0.10 m, mass = 77.6 ± 17.3 kg). We recruited participants from a sample of convenience with no restrictions on foot size or posture. Before the study began, all participants provided written informed consent, and the study was approved by the Protection of Human Subjects Committee of the Texas Tech University Health Sciences Center.
Procedures
We obtained the dimensions of each rectangle using the procedures that we outlined. For the foot measures, we identified 3 anatomic landmarks on each participant's foot using a ballpoint pen (Figure 1). The positions of anatomic landmarks that were not in the calibrated plane were marked on graph paper to allow for correction of the perspective error (Figure 1). We then positioned the medial border of the participant's foot along the front edge of a custom-built measuring platform placed on the measurement scale with the leg aligned vertically in the frontal and sagittal planes, and we obtained digital images during an equal to or greater than 90% WB condition (Figure 1).
Figure 1.
To ensure equal to or more than 90% weight was placed on the foot being measured, participants stood with the involved foot on a mechanical scale set at 90% of body weight and the uninvolved foot placed on a platform of the same height located adjacent to the scale. Participants were instructed to push or pull lightly on the upright portion of the scale to maintain balance. Next, participants were instructed to unload the uninvolved limb until the movable arm on the scale was at or above the horizontal. Anatomic landmarks that the tester identified were the first metatarsophalangeal joint, the most prominent point of the navicular tuberosity, and the midpoint of the medial malleolus. To correct out-of-plane perspective error, the tester also identified the distance from the calibrated plane (depth) of the tip of the longest toe, the dorsum of the first metatarsophalangeal joint, the most prominent point on the dorsum of the foot, and the most prominent point of the calcaneus on graph paper (not shown). The position of each out-of-plane landmark was projected onto graph paper, measured, and saved as a text file that was uploaded later to the MATLAB (version R2006b; The MathWorks, Inc, Natick, MA) program and used as the input variables in the perspective error correction algorithm.
We uploaded the digital images to the software program and digitized the scaling factor points, 7 anatomic landmarks, and 2 reference points from each image (Figure 2). We corrected perspective errors of out-of-plane anatomic landmarks by linearly adjusting the scaling factor by the percentage distance out of plane using the following formula:
where L1 is the plane-to-camera distance and L2 is the landmark-to-camera distance (Figure 1). Unique scaling factors were calculated for each out-of-plane landmark. The perspective error correction was verified empirically before incorporating the algorithm into the DPMM. Total foot length, truncated foot length, dorsum height, AI, and longitudinal arch angle measures were computed from the scaled coordinate data (Figure 2). Each investigator (S.C.C., C.R.J.) digitized 1 digital image of the rectangles and each foot 3 times.
Figure 2.
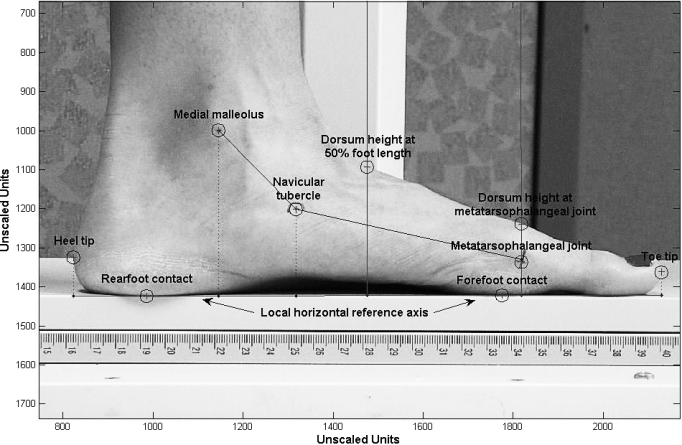
Landmarks that the tester digitized included 2 points on the ruler to compute the scale factor (not pictured), rearfoot and forefoot contact points (defined by digitizing the supporting surface under the regions of the rearfoot and forefoot) with the supporting surface, heel tip, navicular tubercle, first metatarsophalangeal joint, toe tip, dorsum metatarsophalangeal joint, dorsum at 50% foot length, and medial malleolus. To facilitate identification of the dorsal landmarks, the software program plotted reference lines at the appropriate locations (50% of total foot length, metatarsophalangeal joint) that were perpendicular to the local horizontal reference axis (the line connecting the rearfoot and forefoot contact points). The anthropometric variables quantified with the digital photographic measurement method were total foot length (toe tip to heel tip), truncated foot length (metatarsophalangeal joint to heel tip), navicular height (navicular tubercle to local horizontal reference axis), dorsum height (dorsum 50% foot length to local horizontal reference axis), and midpoint of the metatarsophalangeal joint (midpoint between local horizontal reference axis and metatarsophalangeal dorsum points). Computed foot posture variables were arch index (dorsum height/truncated foot length), navicular index (navicular height/truncated foot length), and longitudinal arch index (the angle measured counterclockwise between a line connecting the midpoint of the metatarsophalangeal joint and navicular tubercle and a line connecting the medial malleolus and navicular tubercle).
DPMM and CMM Reliability and Concurrent Validity
Participants
Twenty healthy individuals (10 men and 10 women; age = 24 ± 2 years, height = 1.71 ± 0.09 m, mass = 76 ± 16 kg) volunteered to participate. We excluded participants if they had a history of lower extremity surgery, had sustained a lower extremity injury within the 6 months before the study, had a diagnosed pathologic condition of the foot, or were currently pregnant. We chose the criteria to allow inclusion of a wide range of “normal” foot postures and exclusion of conditions that might adversely affect the reliability of the procedures due to gross deformity or pain during WB. Before the study began, all participants provided written informed consent, and the study was approved by the Protection of Human Subjects Committee of the Texas Tech University Health Sciences Center.
Instrumentation
In addition to the DPMM, we used a sliding caliper (GPM 101; Seritex, Inc, East Rutherford, NJ) and standard goniometer to quantify foot posture using the CMMs. Sliding caliper and goniometric measurements were recorded to the nearest 0.5 mm and degree, respectively.
Procedures
We recorded each participant's height and mass and then the DPMM and CMM foot measurements during 10% and 90% WB conditions. The procedures used for the CMMs were those previously reported for the AI,16 NI,16 RAD,16 and longitudinal arch angle.17 All DPMM and CMM measurements were obtained 3 times by the same 2 testers (M.H., J.K.), who were designated clinician 1 (CL1) and clinician 2 (CL2). For each “trial,” the appropriate anatomic landmarks were identified and used to compute foot structure with the CMM and then the DPMM. Alcohol wipes were used to completely remove all anatomic landmark pen marks before performing the next trial. The clinicians were instructed to clean a relatively large area when removing the marks so that any skin irritation would not affect landmark re-identification. Additionally, the clinicians alternated taking the measurements on each participant and were blinded to their previously recorded measurements and to each other's measurements.
Descriptive Foot Posture Data Set
Participants
To develop a descriptive data set of the DPMM foot measurements with moderate to high intratester and intertester reliabilities, 111 participants (42 men, 69 women; age = 22.8 ± 4.7 years, height = 168.5 ± 10.4 cm, mass = 69.8 ± 13.3 kg) with no medically diagnosed foot pathologic conditions or history of lower extremity surgery or injury within the 6 months before the study were recruited from a sample of convenience. Before the study began, all participants provided written informed consent, and the study was approved by the Institutional Review Board of the University of Wisconsin-Milwaukee.
Procedures
We quantified the foot posture of each participant's right and left feet during 10% WB and 90% WB single-limb stance positions using the DPMM procedures that we outlined (Figure 1). Equal to or less than 10% WB was ensured in a similar manner as described for the 90% WB condition except that the participant was instructed to unload the involved foot located on the mechanical scale until the movable arm on the scale was at or below the horizontal. The same investigator (S.C.C.) performed all foot measurements.
Statistical Analysis
DPMM Technology Reliability and Validity
The intratester reliability of the measurements obtained from the DPMM analysis of the rectangles were investigated by calculating the intraclass correlation coefficient (ICC) (3,1) across the 3 repeated measurements for 3 dependent variables (length of the bottom side, length of the right side, and angle between the bottom side and the diagonal). The intertester reliability of the measurements obtained from the DPMM analysis of the rectangles was determined by calculating the ICC (2,3) using the mean of the 3 trials. The validity of the DPMM technology was evaluated using the absolute and percentage differences (error) between the mean of the 6 DPMM measurements (2 testers, 3 measurements each) and the criterion reference values of the rectangles. The ICC (2,3) was used to quantify absolute agreement between the measured and known dimensions of the rectangles. Finally, the intratester and intertester reliabilities of the DPMM measurements obtained from the feet was calculated using the same procedures as described for the rectangles. All ICC values were determined using SPSS (version 15; SPSS Inc, Chicago, IL). The ICC threshold for moderate reliability was defined21 as equal to or greater than 0.70.
DPMM and CMM Reliability and Concurrent Validity
The intratester reliability of the measurements obtained from the DPMM and CMM were investigated by calculating the ICC (3,1) across the 3 repeated measurements for the anthropometric (truncated foot length in 10% WB, truncated foot length in 90% WB, dorsum height in 10% WB, dorsum height in 90% WB, navicular height in 10% WB, navicular height in 90% WB), structural (AI in 10% WB, AI in 90% WB, NI in 10% WB, NI in 90% WB, longitudinal arch angle in 10% WB, longitudinal arch angle in 90% WB), and mobility (RAD, RNM, dorsum-height displacement, navicular displacement) variables of interest for each clinician. The intertester reliability of the measurement methods was determined by calculating the ICC (2,3). Finally, ICC (2,3) of the anthropometric variables and the AI and NI structural measures during both WB conditions for each clinician were performed to investigate concurrent validity (agreement) between the DPMM and CMM. We used SPSS for statistical analysis.
Descriptive Data Set
Means and SDs of the 111 participants (222 feet) were calculated to represent descriptive data for the DPMM-quantified foot measurement with moderate to high intratester and intertester reliabilities.
RESULTS
DPMM Technology Reliability and Validity
The DPMM intratester and intertester reliability ICCs for the 10 rectangles and the anthropometric and structural variables for the 28 feet were 1.00 (95% confidence intervals [CIs] = 0.90, 1.00) for each tester and variable, respectively. The mean absolute error between the DPMM and criterion reference values were 0.2 ± 0.2 mm, 0.1 ± 0.1 mm, and 0.1° ± 0.1° for the bottom-side, right-side, and calculated angle variables, respectively. The corresponding mean percentage error values were 0.3% ± 0.3%, 0.3% ± 0.3%, and 0.4% ± 0.4% for the bottom-side, right-side, and calculated angle variables, respectively. All ICC (2,3) values for agreement between the measured and known dimensions were 1.00 (95% CI = 1.00, 1.00).
DPMM and CMM Reliability and Concurrent Validity
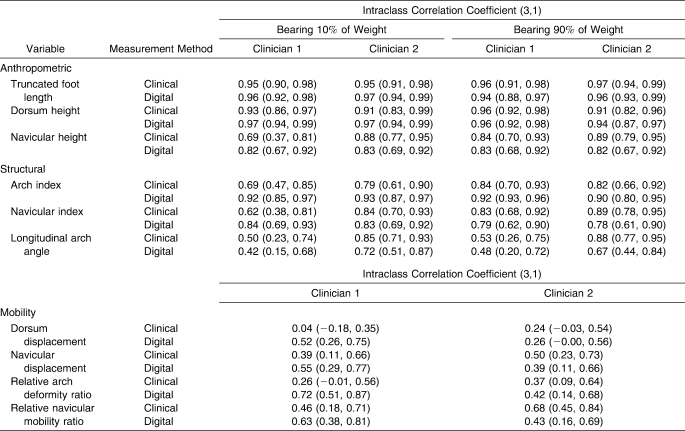
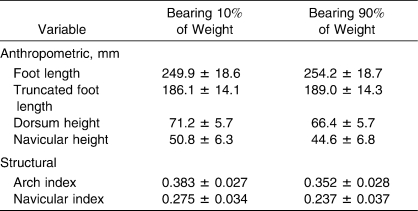
Clinical Measurement Reliability
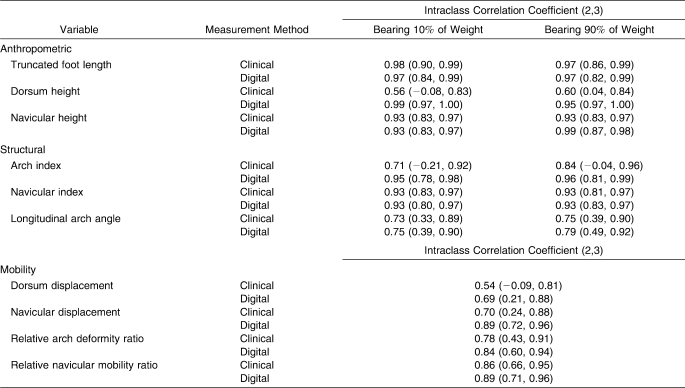
The DPMM intratester and intertester reliabilities during both WB conditions were moderate to high for the anthropometric (ICCs > 0.81) and the AI and NI structural measures (ICCs > 0.78) (Tables 1 and 2). Intratester and intertester reliability results of the longitudinal arch angle and mobility measures were less consistent. Intratester reliability values for the longitudinal arch angle in 10% WB were moderate to high for CL2 but were low for CL1, and values for the longitudinal arch angle in 90% WB did not meet the moderate reliability criteria for either clinician (Table 1). However, intertester reliability for longitudinal arch angle was moderate to high (ICCs > 0.75) in both WB conditions (Table 2). Of the mobility measures, only the RAD for CL1 achieved moderate intratester reliability (ICC [3, 1] = 0.72) (Table 1). Conversely, intertester reliability was moderate to high for all mobility measures, with the exception of dorsum-height displacement (ICC [2, 3] = 0.69) (Table 2).
Table 1.
Intratester Reliability (95% Confidence Interval) of Clinical and Digital Photographic Measurement Methods
Table 2.
Intertester Reliability (95% Confidence Interval) of Clinical and Digital Photographic Measurement Methods
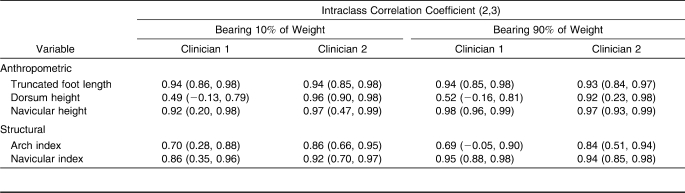
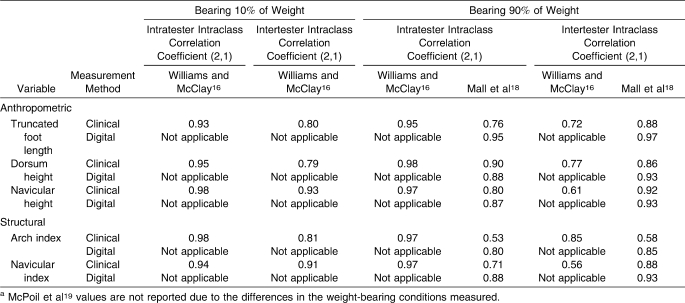
Concurrent Validity
Concurrent validity between the DPMM and CMM was moderate to strong. The ICC (2,3) values were moderate to high for all of the anthropometric and structural values for CL2 (ICCs > 0.84) (Table 3). For CL1, values were moderate to high for all variables with the exception of dorsum height in 10% WB, dorsum height in 90% WB, and AI in 90% WB (Table 3). The mean differences of 10% WB, 90% WB, and mobility CMM and DPMM measures for each clinician are presented in Table 4.
Table 3.
Concurrent Validity (95% Confidence Interval) Between the Clinical and Digital Photographic Measurement Methods
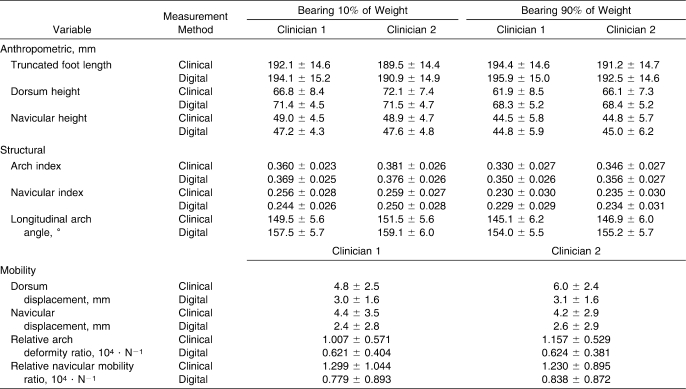
Table 4.
10% Weight-Bearing, 90% Weight-Bearing, and Mobility Clinical Measurement Method and Digital Photographic Measurement Method Measures (Mean ± SD)
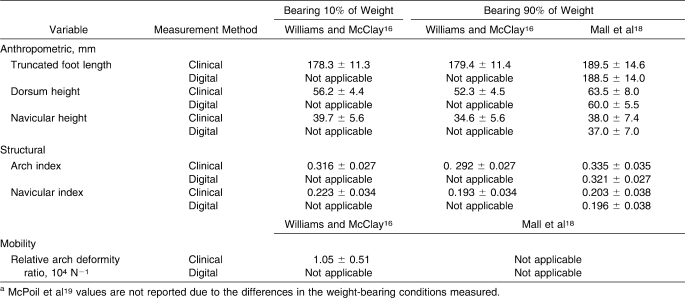
Descriptive Data Set
Descriptive data for the DPMM measures with moderate to high intratester and intertester reliabilities are presented in Table 5.
Table 5.
Descriptive Data for the Digital Photographic Measurement Method–Computed Foot Measures With Moderate to High Intratester and Intertester Reliability (N = 111) (Mean ± SD)
DISCUSSION
The purposes of our study were (1) to investigate the validity and reliability of the DPMM technology, (2) to investigate intratester and intertester reliabilities of DPMM-quantified foot posture, (3) to investigate concurrent validity of the DPMM and CMM measures and (4) to report descriptive data for the DPMM-quantified foot measures with moderate to high intratester and intertester reliabilities.
DPMM Technology Reliability and Validity
The intratester and intertester reliability and validity of the DPMM technology results suggested that the DPMM is a valid and reliable method for quantifying foot posture. The moderate to high ICC values between the CMM and DPMM for most anthropometric and structural variables also suggested that the 2 methods measure the same foot characteristics. The only variables not moderately correlated were dorsum height in 10% WB, dorsum height in 90% WB, and AI in 90% WB for CL1 (Table 3). Average differences in dorsum height in 10% WB and dorsum height in 90% WB between the DPMM and CMM for CL1 were 4.6 mm and 6.4 mm, respectively, and the difference in AI in 90% WB was 0.02 (Table 4). Although the primary sources for the lack of agreement between the DPMM and CMM measures of dorsum height for CL1 cannot be determined definitively, lack of agreement might have been due to variability: (1) reading the sliding caliper (when measuring the dorsum height or locating the 50% of total foot-length position) or soft tissue deformation during dorsum-height measurement associated with the CMM or (2) measuring the depth of the dorsum-height position from the calibrated plane associated with the DPMM. With respect to the lack of agreement for AI in 90% WB between the DPMM and CMM for CL1, the strong agreement for truncated foot length in 90% WB between the DPMM and CMM suggested that the dorsum height in 90% WB measure was likely the cause (Table 1).
DPMM and CMM Reliability and Concurrent Validity
The moderate to high intratester and intertester reliabilities and relatively narrow 95% CIs for all of the DPMM anthropometric measures suggested that the DPMM was a reliable method of measuring foot anthropometrics (Tables 1 and 2). For the CMM, intratester and intertester reliabilities were also moderate to high and the 95% CIs were relatively narrow for most, but not all, of the anthropometric measures (Tables 1 and 2). The intratester reliability and 95% CI of CL1's measure of navicular height in 10% WB were poor and wide, respectively. The same was true of the intertester reliability and 95% CIs for dorsum height in 10% and 90% WB. The sources of error for measuring navicular height in 10% WB for CL1 might have been the result of variability in reading the sliding caliper or in identifying the navicular between trials. However, the moderate to high intratester reliability of the clinician's measures of navicular height in 90% WB, which was the same mark identified in the 10% WB condition, suggests that navicular identification was not likely the error source.
The poor intratester reliability for CL1's measure of navicular height in 10% WB, the poor intertester reliability for the measures of dorsum height in 10% and 90% WB, and the moderate to high intertester reliability for the CMM measure of navicular height in 90% WB in our study were inconsistent with the findings of Williams and McClay16 (Table 6). The lower reliability in our study than in the study by Williams and McClay16 for the CMM measures of navicular height in 10% WB and dorsum height in 10% and 90% WB anthropometric variables might be explained, in part, by the difference in the experience of the clinicians taking the foot measurements. The clinicians in our study were second-year students in an entry-level master's of athletic training program with relatively limited experience taking foot measurements, whereas those in the Williams and McClay16 study were licensed physical therapists with 3 and 20 years of experience taking foot measurements on a daily basis.
Table 6.
Intratester Reliability of Previously Reported Clinical and Digital Photographic Measurement Methodsa
The inconsistency in the intertester reliability for the measure of the navicular height in 90% WB, on the other hand, might be due to a methodologic difference between the studies. Williams and McClay16 reidentified the navicular during the 90% WB condition, whereas we used the same mark identified in the 10% WB condition. The methodologic difference as the likely factor might be further supported by the moderate to high intertester reliability for the measure of navicular height in 90% WB reported by Mall et al18 for both a mirrored-foot photobox method and the CMM in which the navicular was identified before the 90% WB condition. Although the poor intertester reliability for the measure of dorsum height is also inconsistent with the results reported by McPoil et al,19 the reason for the difference is unclear because McPoil et al19 assessed dorsum height in non–WB and 50% WB conditions, whereas we assessed it in 10% and 90% WB conditions (Table 6).
The average DPMM anthropometric values were also consistent with the CMM values reported by us, Williams and McClay,16 and Mall et al18 and with the mirrored-foot photobox measures reported by Mall et al.18 The greatest differences were 15.2 and 16.1 mm for dorsum height in 10% WB and dorsum height in 90% WB, respectively, between the DPMM in our study and the CMM in the Williams and McClay16 study (Tables 4 and 7). Aside from the different populations in the 3 studies, soft tissue deformation associated with the CMM of dorsum height might have contributed to the difference between the measurement methods. Soft tissue deformation as an influencing factor also was supported by lower average dorsum-height values for the CMM than for the DPMM in our study (Table 4). The only other difference between the DPMM in our study and the measurement methods in previous studies in which anthropometric values were greater than 10 mm were with Williams and McClay16 for truncated foot length in 10% WB, truncated foot length in 90% WB, and navicular height in 90% WB. Different participant populations were the most likely source of variability in the truncated foot-length measurements between the studies, whereas the method of navicular identification might have contributed to the differences in navicular height. We identified the most prominent point of the navicular, whereas Williams and McClay16 and Mall et al18 identified the most plantar aspect of the navicular.
Table 7.
Previously Reported Clinical and Digital Photographic Measurement Method Foot Measuresa
With respect to the structural measures, the moderate to high intratester and intertester reliabilities for the DPMM and CMM measure of AI in our study were consistent with the reliability for the CMM reported by Williams and McClay16 and for the mirrored-foot photobox method reported by Mall et al18 (Tables 1, 2, and 6). The moderate to high intertester reliability for the DPMM measure of NI in 90% WB in our study was an improvement over the reliability for the CMM reported by Williams and McClay16 and was consistent with the reliability for the mirrored-foot photobox method reported by Mall et al18 (Tables 2 and 6). However, the differences in reliability between the 2 digital methods and the CMM reported by Williams and McClay16 likely were associated with the differences in navicular identification rather than the measurement technology. The AI and NI structural measures in our study also were consistent with those reported by others, with the variability likely explained by the different populations and the anthropometric measures discussed previously (Tables 4 and 7). Finally, although the intratester and intertester reliabilities for the CMM and DPMM measures of AI in our study were both moderate to high, the tighter 95% CI intervals for the DPMM might suggest an improvement over the CMM (Tables 1 and 2).
The low intratester reliability for the DPMM measure of longitudinal arch angle, with the exception of CL2's measure of longitudinal arch angle in 10% WB, and the moderate to high intertester reliability were inconsistent with the results reported by McPoil and Cornwall,17 which also were computed using digital images (Tables 1, 2, and 4). The lower intratester reliability of the longitudinal arch angle versus the other structural measures may not be unexpected because more potential sources of between-measurements variability (identification of the midpoint of the first metatarsophalangeal joint, the most prominent point of the navicular, and the midpoint of the medial malleolus) might be associated with the longitudinal arch angle. The inconsistency between the intratester reliability results of our study and of McPoil and Cornwall17 might be explained, in part, by the experience of the clinicians taking the measurements in the 2 studies. As noted, the clinicians in our study were second-year students in an entry-level master's of athletic training program, whereas those in the McPoil and Cornwall17 study were described as “experienced raters.” Greater experience palpating the landmarks might have improved the intratester reliability.
Despite the moderate to high intratester reliability for the DPMM-calculated dorsum height and navicular height in both WB conditions, the intratester reliability for the mobility measures computed using the measurements was overwhelmingly low (Table 1). However, the intertester reliabilities for the same mobility measures were moderate to high. The intertester reliability results of dorsum height displacement were consistent with McPoil et al19; however, the poor intratester reliability was not. Again, the reason for the disagreement, as well as for the agreement, between the 2 studies was unclear due to differences in the WB conditions assessed. Options to improve the DPMM mobility measurement might include averaging of multiple measurements using our methods, improvement in our methods, or investigation of additional mobility measures. With respect to our methods, intratester reliability of the algorithms that use navicular height to quantify foot mobility might be improved by identifying the most plantar aspect versus the most prominent point of the navicular. Furthermore, the moderate to high intertester reliability might suggest that, when computing the mobility measurements, taking the average of multiple measurements is warranted.
Finally, the differences in the reliability of CMM AI values reported by Williams and McClay16 and those in both our study and the study by Mall et al18 might be clinically relevant. Although the intratester and intertester reliability of computing AI with the CMM was acceptable in our study, this reliability was somewhat lower than that reported by Williams and McClay16 (Tables 1, 2, and 6). Furthermore, Mall et al18 reported low intratester and intertester reliabilities associated with the CMM (Table 6). The lower reliability in our study than in the study by Williams and McClay16 might be explained, in part, by the difference in the experience of the clinicians taking the foot measurements. The clinicians in the Williams and McClay16 study were licensed physical therapists with 3 and 20 years of experience taking foot measurements on a daily basis. However, clinical experience as a potential factor in the Mall et al18 study was unclear because the level of clinician experience was not reported.
Differences between the descriptive data in our study and those reported by Williams and McClay16 are likely due to the factors identified previously. Because the descriptive data sets differed, researchers should continue to use the normative data reported by Williams and McClay16 to define foot-posture groups in future studies in which AI is computed with the CMM. In future studies in which foot-posture groups are quantified using the DPMM, investigators should use the descriptive values reported in our study.
Limitations
The descriptive data set was computed from a relatively young population, which might limit the generalizability to older populations. In addition, the DPMM algorithm program currently requires a MATLAB software license and the custom algorithm, which is not publically available. However, the custom algorithm is available upon request from the corresponding author to interested clinicians or researchers with a MATLAB software license. Furthermore, the goal of developing the DPMM was to develop a method using commercially available and relatively inexpensive equipment (eg, digital camera, standard analog weight scale) that ultimately can be used by clinicians and researchers. Although MATLAB is a commercially available program, it is not inexpensive, so plans to compile the program into a form independent of MATLAB that might be used by clinicians and researchers also are being developed. A final limitation of the DPMM in its current stage of development is the ability to only quantify sagittal plane foot-posture and mobility measurements. Although not reported in our study, we are investigating measurement of first metatarsal position and mobility, rearfoot position and mobility, and forefoot splay using the DPMM.
CONCLUSIONS
The DPMM is a valid and reliable clinical and research tool for quantifying foot structure using the AI and NI. Furthermore, quantifying foot structure using the DPMM might offer several advantages over the CMM, including the following: (1) All anthropometric measurements are calculated at the same instant in time; (2) variability in identifying 50% of total foot length might be decreased; (3) variability due to reading an analog measurement scale is eliminated; (4) variability due to soft tissue deformation is eliminated; (5) multiple measurements of foot posture might be quantified from 1 digital image; (6) the DPMM algorithm assists in the identification of landmarks by drawing reference lines on the photograph during the analysis; and (7) the DPMM is reliable for relatively inexperienced clinicians, which might not be the case with the CMM. The primary remaining source of variability among repeated measures and testers, which cannot be accounted for by either the DPMM or CMM, is consistent manual identification of anatomic landmarks. With respect to foot mobility, the measures used in our study did not result in moderate intratester reliability using the DPMM and, therefore, are not recommended for use in clinical or research settings. Additional research aimed at either improving the current mobility methods or identification of additional measures of foot mobility that have both moderate to high intratester and intertester reliabilities is warranted. Finally, the DPMM and the descriptive data also might be used to define typical and abnormal foot-posture groups in future studies in which the relationship between foot posture and function or injury risk is investigated.
Acknowledgments
We thank David Bazett-Jones and Mukta Joshi of the University of Wisconsin-Milwaukee Neuromechanics Laboratory for their assistance with descriptive data collection.
REFERENCES
- 1.Burns J., Keenan A. M., Redmond A. Foot type and overuse injury in triathletes. J Am Podiatr Med Assoc. 2005;95(3):235–241. doi: 10.7547/0950235. [DOI] [PubMed] [Google Scholar]
- 2.Giladi M., Milgrom C., Stein M., et al. The low arch, a protective factor in stress fractures: a prospective study of 295 military recruits. Orthop Rev. 1985;14(11):709–712. [Google Scholar]
- 3.Kaufman K. R., Brodine S. K., Shaffer R. A., Johnson C. W., Cullison T. R. The effect of foot structure and range of motion on musculoskeletal overuse injuries. Am J Sports Med. 1999;27(5):585–593. doi: 10.1177/03635465990270050701. [DOI] [PubMed] [Google Scholar]
- 4.Williams D. S., 3rd, McClay I. S., Hamill J. Arch structure and injury pattern in runners. Clin Biomech (Bristol, Avon) 2001;16(4):341–347. doi: 10.1016/s0268-0033(01)00005-5. [DOI] [PubMed] [Google Scholar]
- 5.Baumhauer J. F., Alosa D. M., Renstrom A. F., Trevino S., Beynnon B. A prospective study of ankle injury risk factors. Am J Sports Med. 1995;23(5):564–570. doi: 10.1177/036354659502300508. [DOI] [PubMed] [Google Scholar]
- 6.Cowan D. N., Jones B. H., Robinson J. R. Foot morphologic characteristics and risk of exercise-related injury. Arch Fam Med. 1993;2(7):773–777. doi: 10.1001/archfami.2.7.773. [DOI] [PubMed] [Google Scholar]
- 7.Michelson J. D., Durant D. M., McFarland E. The injury risk associated with pes planus in athletes. Foot Ankle Int. 2002;23(7):629–633. doi: 10.1177/107110070202300708. [DOI] [PubMed] [Google Scholar]
- 8.Wen D. Y., Puffer J. C., Schmalzried T. P. Lower extremity alignment and risk of overuse injuries in runners. Med Sci Sports Exerc. 1997;29(10):1291–1298. doi: 10.1097/00005768-199710000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Cowan D. N., Robinson J. R., Jones B. H., Polly D. W., Jr, Berrey B. H. Consistency of visual assessments of arch height among clinicians. Foot Ankle Int. 1994;15(4):213–217. doi: 10.1177/107110079401500411. [DOI] [PubMed] [Google Scholar]
- 10.Evans A. M., Copper A. W., Scharfbillig R. W., Scutter S. D., Williams M. T. Reliability of the foot posture index and traditional measures of foot position. J Am Podiatr Med Assoc. 2003;93(3):203–213. doi: 10.7547/87507315-93-3-203. [DOI] [PubMed] [Google Scholar]
- 11.Keenan A. M., Bach T. M. Video assessment of rearfoot movements during walking: a reliability study. Arch Phys Med Rehabil. 1996;77(7):651–655. doi: 10.1016/s0003-9993(96)90003-9. [DOI] [PubMed] [Google Scholar]
- 12.Menz H. B., Keenan A. M. Reliability of two instruments in the measurement of closed chain subtalar joint positions. Foot. 1997;7(4):194–201. [Google Scholar]
- 13.Sell K. E., Verity T. M., Worrell T. W., Pease B. J., Wigglesworth J. Two measurement techniques for assessing subtalar joint position: a reliability study. J Orthop Sports Phys Ther. 1994;19(3):162–167. doi: 10.2519/jospt.1994.19.3.162. [DOI] [PubMed] [Google Scholar]
- 14.Smith-Oricchio K., Harris B. A. Interrater reliability of subtalar neutral, calcaneal inversion and eversion. J Orthop Sports Phys Ther. 1990;12(1):10–15. doi: 10.2519/jospt.1990.12.1.10. [DOI] [PubMed] [Google Scholar]
- 15.Vinicombe A., Raspovic A., Menz H. B. Reliability of navicular displacement measurement as a clinical indicator of foot posture. J Am Podiatr Med Assoc. 2001;91(5):262–268. doi: 10.7547/87507315-91-5-262. [DOI] [PubMed] [Google Scholar]
- 16.Williams D. S., McClay I. S. Measurements used to characterize the foot and the medial longitudinal arch: reliability and validity. Phys Ther. 2000;80(9):864–871. [PubMed] [Google Scholar]
- 17.McPoil T. G., Cornwall M. W. Use of the longitudinal arch angle to predict dynamic foot posture in walking. J Am Podiatr Med Assoc. 2005;95(2):114–120. doi: 10.7547/0950114. [DOI] [PubMed] [Google Scholar]
- 18.Mall N. A., Hardaker W. M., Nunley J. A., Queen R. M. The reliability and reproducibility of foot type measurements using a mirrored foot photo box and digital photography compared to caliper measurements. J Biomech. 2007;40(5):1171–1176. doi: 10.1016/j.jbiomech.2006.04.021. [DOI] [PubMed] [Google Scholar]
- 19.McPoil T. G., Cornwall M. W., Medoff L., Vicenzino B., Forsberg K., Hilz D. Arch height change during sit-to-stand: an alternative for the navicular drop test. J Foot Ankle Res. 2008;1(1):3. doi: 10.1186/1757-1146-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dahle L. K., Mueller M. J., Delitto A., Diamond J. E. Visual assessment of foot type and relationship of foot type to lower extremity injury. J Orthop Sports Phys Ther. 1991;14(2):70–74. doi: 10.2519/jospt.1991.14.2.70. [DOI] [PubMed] [Google Scholar]
- 21.Landis J. R., Koch G. G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]