Abstract
Context:
More than 1.6 million sport-related concussions occur every year in the United States, affecting greater than 5% of all high school athletes who participate in contact sports. As more females participate in sports, understanding possible differences in concussion symptoms between sexes becomes more important.
Objective:
To compare symptoms, symptom resolution time, and time to return to sport between males and females with sport-related concussions.
Design:
Descriptive epidemiology study.
Setting:
Data were collected from 100 high schools via High School RIO (Reporting Information Online).
Patients or Other Participants:
Athletes from participating schools who sustained concussions while involved in interscholastic sports practice or competition in 9 sports (boys' football, soccer, basketball, wrestling, and baseball and girls' soccer, volleyball, basketball, and softball) during the 2005–2006 and 2006–2007 school years. A total of 812 sport concussions were reported (610 males, 202 females).
Main Outcome Measure(s):
Reported symptoms, symptom resolution time, and return-to-play time.
Results:
No difference was found between the number of symptoms reported (P = .30). However, a difference was seen in the types of symptoms reported. In year 1, males reported amnesia (exact P = .03) and confusion/disorientation (exact P = .04) more frequently than did females. In year 2, males reported more amnesia (exact P = .002) and confusion/disorientation (exact P = .002) than did females, whereas females reported more drowsiness (exact P = .02) and sensitivity to noise (exact P = .002) than did males. No differences were observed for symptom resolution time (P = .40) or return-to-play time (P = .43) between sexes.
Conclusions:
The types of symptoms reported differed between sexes after sport-related concussion, but symptom resolution time and return-to-play timelines were similar.
Keywords: epidemiology, mild traumatic brain injuries, symptom resolution, return to play
Key Points.
After a sport-related concussion, male and female high school athletes presented with different types of symptoms.
Males reported more cognitive symptoms, whereas females reported more neurobehavioral and somatic symptoms.
Symptom resolution time and time to return to play did not differ between sexes.
There are an estimated 7.3 million high school students participating in organized interscholastic athletics in the United States each year.1 An estimated 1.6 to 3.8 million sport-related concussions are sustained every year,2 with an average of 21% occurring in high school athletes.3,4 More than 5% of all high school athletes who participate in contact sports such as football, lacrosse, and hockey sustain a concussion each year.5–8 Although males continue to participate in sports at a higher rate than females, in 2008, 3.01 million (or 41%)1 of high school athletes were female, up from 2.4 million 10 years earlier.9 Injury incidence among females has increased with increased female sport participation, and now females have a higher incidence rate of sport-related concussions than do males.3,10,11 However, the female response to concussion has not been well described, and similarities in male and female sport-related concussion symptoms remain largely anecdotal.
Diagnosing sport-related concussions is one of the most elusive tasks of sports medicine clinicians. No biological markers exist to detect this relatively mild injury, and diagnosis largely depends on a patient's report.12 Assessment is further complicated by the tendency of many athletes to underreport or hide symptoms from clinicians, coaches, and parents.13
Research14–16 on more severe closed head injuries and traumatic brain injuries (TBIs) indicates that females may respond to concussions differently than males. Authors14 of a meta-analysis of postconcussion outcome sex differences identified 8 studies that provided data by sex, citing worse overall outcomes in females. Twenty outcomes were compared, including variables such as postconcussive symptoms at 6 weeks, days of posttraumatic amnesia, length of hospitalization, inability to return to work, and presence of headache, dizziness, and insomnia. Retrospective studies16,17 comparing males and females with TBI showed that females tended to fare worse than their male counterparts, with longer hospitalizations, longer residual disabilities, and higher mortality rates. In one pharmacologic trial,15 female patients younger than 51 years had greater frequency of brain swelling and intracranial hypertension than did male patients of the same age. These findings were not associated with increased injury severity on the Glasgow Coma Scale; in fact, females with higher scores had more pronounced swelling.15 Thus, females with TBI may require greater monitoring and more aggressive treatment than males.
In an attempt to elucidate the mechanisms explaining sex differences in TBI, animal models have been developed.18,19 When rats were supplemented with estrogen before a fluid-percussion brain injury was induced, a protective effect was seen among male rats, but female rates showed exacerbated effects and higher mortality rates.19 Bramlett and Dietrich,18 however, noted that estrogen had a neuroprotective effect on cerebral hematoma size in rats. Both estrogen and progesterone are associated with the inflammatory reaction and extent of tissue damage in the brain.20 Therefore, different outcomes among females after TBI may reflect a biochemical basis, with hormonal factors playing a role in the response to head trauma. This relationship remains unclear, especially in adolescents, whose hormone levels vary; also unknown is whether similar effects occur in cases involving mild head injury and sport-related concussion.
Neuropsychological data have been examined to identify sex differences in sport-related concussions. However, most investigators have studied collegiate athletes, and whether high school athletes will behave similarly is uncertain. Covassin et al21 reported differences in visual memory composite scores in collegiate athletes and suggested a relationship between postconcussive symptoms and sex. In a mixed sample of collegiate and high school athletes, Broshek et al22 found that females tended to be more cognitively impaired after a sport-related concussion. Lovell et al23 noted that high school athletes with concussions had memory and processing deficits, but they did not compare sex differences in symptoms. Sport-related concussions in male and female high school athletes have been the focus of limited research; specifically, sex differences in symptoms, symptom resolution time (SRT), and return-to-play (RTP) timelines in high school athletes have not been studied.
The purpose of our study was to investigate concussion symptoms in male and female athletes using a national sample of high schools. We compared the total number of symptoms reported by sex and the prevalence of each reported symptom among males and females, SRT, and RTP timelines. Based on the previous literature dealing with sport-related concussion and TBI, we hypothesized that females would report a greater number of symptoms, longer symptom duration, and later RTP.
METHODS
During the 2005–2006 (year 1) and 2006–2007 (year 2) school years, injury and exposure data were prospectively collected from athletes via the High School Sport-Related Injury Surveillance System, RIO (Reporting Information Online, Columbus, OH).3,24–26 An Internet-based injury surveillance system, RIO records injury data in US high school sports. Sports studied during years 1 and 2 were boys' football, soccer, basketball, wrestling, and baseball and girls' soccer, basketball, volleyball, and softball.
All US high schools with at least one Board of Certification–certified athletic trainer (AT) on staff with a valid e-mail address (N = 4120 in 2005–2006 and N = 3378 in 2006–2007) were eligible to participate. A total of 425 and 316 (in years 1 and 2, respectively) of the ATs agreed to participate. Schools were then categorized into 8 sampling strata based on US census geographic regions (northeast, midwest, south, and west)27 and school size (enrollment of <1000 or ≥1000 students). Schools were randomly selected from each of the sampling strata (n = 100). If a school dropped out of the study, another school from the same stratum was randomly selected to replace it.4
During each school year, ATs from participating high schools were required to log on to the High School RIO Web site weekly, using an individualized study identification number, to report athlete-exposures (AEs) and injury data. An AE was defined as 1 athlete participating in 1 practice or competition. Injury was defined by 3 factors: (1) it occurred during an organized high school practice or competition; (2) it required attention by a team AT or physician; and (3) it resulted in restriction of participation of the student-athlete for at least 1 day. The data-collection software used sequential drop-down menus to administer a questionnaire asking for detailed information regarding each injury, including student-athlete demographics. The ATs were able to view, edit, and update previously entered information throughout the study period. The data analysis for this study had institutional review board approval.
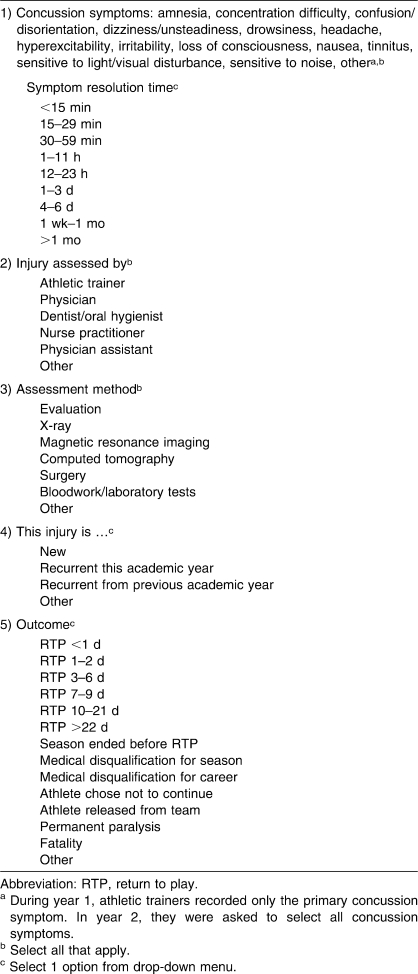
During year 1 (2005–2006), ATs were asked to record only the primary symptom experienced by the injured athletes. For year 2 (2006–2007), the data-collection procedures were changed such that the clinician was prompted to record all symptoms reported by the concussed athlete using a computerized drop-down menu. Subsequently, the AT recorded the time period during which symptoms resolved as well as the time period after which the athlete returned to play. The AT was also asked to indicate all clinicians who assessed the injury, all methods of injury assessment, and, via drop-down menu, whether the injury was new or recurrent (Table 1).
Table 1.
Possible Responses for Select Questions Pertaining to Concussions in the Reporting Information Online (RIO) System
For the purpose of this study, we included only those injuries classified as concussions in the analysis. The main exposure (sex) was determined by the sport in which the student-athlete participated. Outcome variables of interest were (1) symptoms, including frequency of reported symptoms and total number of symptoms (year 2 only), (2) SRT, and (3) RTP time.
We assessed the following as potential confounders: regional strata, age, height, mass, by whom the concussion was assessed, whether the concussion took place during practice or competition, whether the concussion was a new or recurrent injury, and whether the athlete was wearing personal protective equipment (eg, helmet, mouthguard, shin guards).
Statistical Analysis
Because the data-collection methods differed between years 1 and 2, symptom data for each year were analyzed separately. As expected, cell counts for some symptoms were less than or equal to 5, so the Fisher exact test was performed to assess differences in the proportions of athletes reporting each symptom by sex. Differences between the mean numbers of reported symptoms by sex were also evaluated via t test for year 2. Logistic regression was used to assess for the confounding variables listed above.
To evaluate the relationships between sex and both SRT and the RTP, we fit complementary log-log models. These models were used for discrete time-to-event data for which it cannot be assumed that the exact time of the occurrence of the event is known within the interval (eg, less than 15 minutes). Because the reported time intervals in the data set were not of equal length, this model is appropriate: it assumes a continuous time process with events not occurring at discrete time points but rather occurring at any time point during the interval. Multivariable analysis was used to assess for potential confounding by the variables listed above. All analyses were performed using SAS (version 9.1.3; SAS Institute Inc, Cary, NC), with α = .05 set a priori. The α level was not adjusted for these preplanned comparisons.28
RESULTS
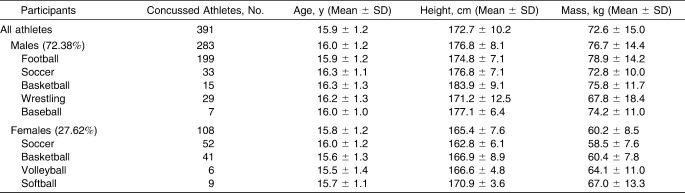
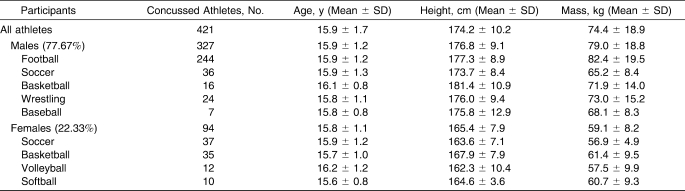
A total of 391 concussions (283 males, 108 females) were reported in year 1 (Table 2), and 421 concussions (327 males, 94 females) were reported in year 2 (Table 3).
Table 2.
Concussed Athletes and Height, Mass, and Age by Sport: Year 1
Table 3.
Concussed Athletes and Height, Mass, and Age by Sport: Year 2
Symptoms
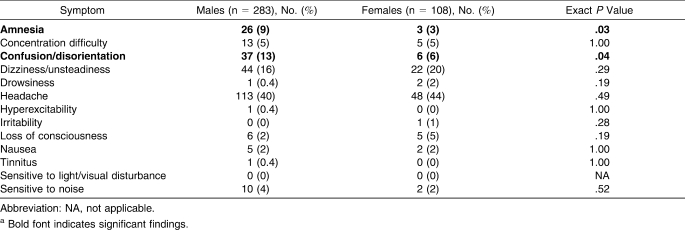
Only the primary symptom was reported in year 1. Headache was the most commonly reported primary symptom (40% [n = 113] among males, 44% [n = 48] among females), although no difference was noted between sexes (exact P = .49) (Table 4). When we compared symptoms by sex, males reported amnesia and confusion/disorientation as their primary symptom more frequently than did females (exact P values = .03 and .04, respectively). No additional symptoms were reported by one sex more often than by the other sex.
Table 4.
Primary Concussion Symptom Reported: Year 1a
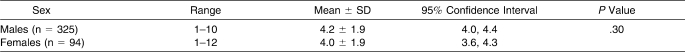
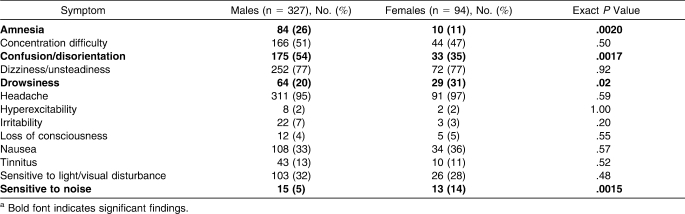
In year 2, all reported symptoms were recorded. No difference (P = .30) was evident between the mean number of symptoms reported by males (4.2 ± 1.9) and females (4.0 ± 1.9) (Table 5). Headache was the most commonly reported symptom for both sexes (95% among males [n = 311] and 97% [n = 91] among females), although no difference was found between sexes (exact P = .59). Males reported amnesia (exact P = .002) and confusion/disorientation (exact P = .002) more often than did females (Table 6). However, females reported drowsiness (exact P = .02) and sensitivity to noise (exact P = .002) more often than did males.
Table 5.
Number of Symptoms Reported by Sex: Year 2 Only
Table 6.
All Concussion Symptoms Reported: Year 2a
Time to Symptom Resolution
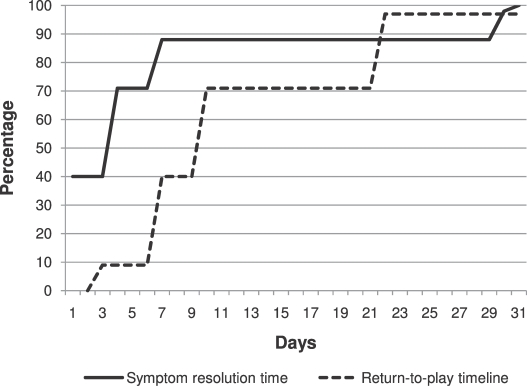
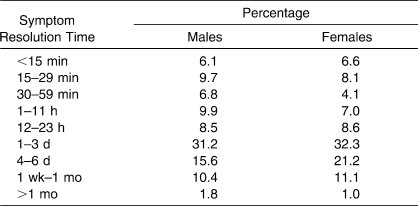
Most (n = 556, 70.8%) of the student-athletes reported resolution of their symptoms within 3 days of injury (Figure; n = 424 [72.2%] among males and n = 135 [66.7%] among females) (Table 7). Data were missing for 23 males and 4 females. The SRT was not different between the sexes (hazard ratio = 1.07; 95% confidence interval = 0.91, 1.27). The relationship between sex and SRT did not appear to be appreciably affected by any of the variables assessed as potential confounders.
Figure.
Time to symptom resolution and return to play.
Table 7.
Time to Concussion Symptom Resolution by Sex
Time to RTP
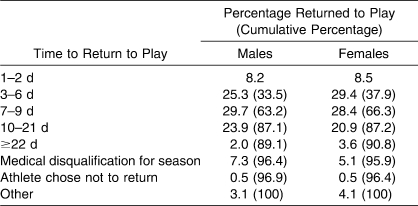
Among all student-athletes, 64% (n = 503) returned to play by 9 days postinjury (63% [n = 133] of males and 66% [n = 370]) of females. The greatest percentage of males returned to play between 7 and 9 days after concussion (n = 174, 29.7%), whereas the greatest percentage of females returned between 3 and 6 days after concussion (n = 59, 29.4%) (Table 8). Data were missing for 24 males and 1 female. No difference was noted between male and female athletes with regard to RTP timelines (hazard ratio = 0.93; 95% confidence interval = 0.78, 1.11). The effect between sex and time to RTP also did not appear to be appreciably confounded by the previously mentioned variables.
Table 8.
Time to Return to Play by Sex
DISCUSSION
Historically, authors29–31 of sport-related concussion studies have examined symptoms in males and focused on football because of the increased risk of concussion in that sport. However, both the risk of injury and the incidence rate of sport-related concussions are higher among female athletes.3,11 There is little information currently available that compares concussion symptoms between sexes, especially among adolescent athletes. The large database we used allowed us to examine the spectrum of sport-related concussions experienced by high school student-athletes over a 2-year period and allowed symptom comparison between males and females. These surveillance data represent what is actually happening in high school sports rather than what might happen in the atmosphere of a controlled study. Thus, our findings represent the injuries that are being diagnosed as concussions and how these injuries are being managed, given the reality of the wide variations in level of education, experience, and resources.
Symptom Prevalence
Symptoms are used as a criterion for concussion evaluation and for making RTP decisions. In a 2005 survey,12 clinical examination and a symptom checklist were the concussion-evaluation tools used most often by clinicians. Headache was the primary symptom most commonly reported by both sexes in year 1 and the most consistently reported symptom in year 2 (95% among males and 97% among females). Headache is considered a hallmark symptom of concussion and was reported in similar frequencies by other researchers.32–34 However, symptom type has not been conclusively associated with the severity of sport-related concussion. Guskiewicz et al33 associated the persistence of headache with more severe injury because a greater percentage of football players with grade II concussions had complaints of headache lasting longer than 7 days when compared with players with grade I concussions. In the same study, headache symptoms among 28% of participants resolved within 24 hours, and only 10% of those with grade I injuries had headaches lasting longer than 5 days.
Loss of consciousness (LOC) is also used to rate the severity of a sport-related concussion, but it was 1 of the 3 least-reported symptoms (<5%) in our study, consistent with the findings of Erlanger et al35 and Barnes et al.36 Some grading systems (eg, Torg,37 Colorado Medical Society [Kelly and Rosenberg38], and American Academy of Neurology [Kelly39]) rely heavily on LOC to rate the severity of a concussion, whereas the more recent Evidence-Based Cantu Grading Scale40 focuses on postconcussion signs and symptoms. In our study, the reports of LOC between sexes did not differ, nor was there a difference in SRT. Thus, both males and females sustained a high number of mild concussion injuries with no apparent difference in severity based on LOC data.
Number of Reported Symptoms
The database we used relied on a system by which clinicians chose symptoms from a drop-down menu. In most cases, clinicians selected from the symptoms provided, but they were also provided a choice of other to capture injury symptoms not included on the list. Many used the other option to list symptoms that were already on the list, particularly in year 1, when only the primary symptom was captured. Listing several symptoms in this manner would not prioritize a specific symptom. For example, of the 35 clinicians who used other, 23 included headache among the symptoms listed rather than using the drop-down menu. The majority of symptoms listed using the text field were also on the drop-down menu. In year 2, it appeared that clinicians used the other category to list specific characteristics, such as “loss of peripheral vision in the right eye” or “difficulty using left hand.” In year 2, the other category was often used in conjunction with the list of multiple symptoms to provide more descriptive characteristics.
With respect to the number of symptoms reported, only the data from year 2 could be evaluated because a single, primary symptom was recorded in year 1. We found no difference in the number of symptoms reported between males and females, consistent with reports from other studies.38,41,42 Some researchers,22,43 however, have shown that females reported more postconcussion symptoms than did males. This result may reflect differences in the populations studied, severity of injury, and mechanism of reporting, given that Lovell et al43 and Broshek et al22 studied smaller samples of collegiate athletes. Those authors examined participants who had been referred by physicians for neuropsychological testing or had symptoms lasting at least 5 days. Our study included more than 800 concussions sustained by high school student-athletes that were identified by an AT and most symptoms resolved in fewer than 3 days. All concussion injuries that required disqualification from athletic participation for at least 1 day were included. Mechanisms of reporting symptoms varied from those used in our study. Lovell et al43 and Broshek et al22 used computerized neurocognitive evaluation tools that relied on self-recorded symptoms rather than reports of symptoms to a health care professional. Self-recorded symptoms are subjective and many are not reported.13,44 One group13 suggested that just over 50% of concussions go unreported, and others13,31,45,46 suggest that underreporting may occur when an athlete is unaware of the signs and symptoms of a sport-related concussion. Thus far, studies13 investigating the denial of symptoms associated with concussion have only included males.
Symptom Classification
Previous researchers have attempted to categorize concussion symptoms based on factorial analysis. A 3-factor measurement model has been proposed by Piland et al47 to evaluate the validity of the Graded Symptom Checklist. They were able to categorize self-reported symptoms into the following factors: (1) cognitive (feeling “slowed down,” feeling like they were “in a fog,” difficulty concentrating, and difficulty remembering), (2) neurobehavioral (sleeping more than usual, drowsiness, fatigue, and nervousness), and (3) somatic (headache, nausea, sensitivity to light and noise, and balance problems).47 The Post Concussion Symptom Scale (another self-reported symptom inventory) has traditionally been used to capture concussion symptoms in an uncategorized manner48 and, more recently, the Acute Concussion Evaluation categorized concussion symptoms as physical, cognitive, emotional, and sleep associated.49 The RIO used a pull-down menu to describe symptoms that were reported to the AT (Table 4) and incorporated a symptom list similar to the lists of the Graded Symptom Checklist, Acute Concussion Evaluation, and Post Concussion Symptom Scale.48 Each symptom category was represented by RIO, although sadness, trouble falling asleep, feeling like one is “in a fog,” and feeling “slowed down” were not listed options. However, RIO did include irritability, dizziness/unsteadiness, and tinnitus. Because RIO used recorded data by a health care professional, these data were perhaps of better quality than those collected by self-report. We do not know if ATs used the symptom checklist provided by the drop-down menus of the RIO or if they relied on the injured student-athletes for symptom reporting. Again, the potential for underreporting symptoms may be minimized by using checklists rather than relying on injured student-athletes to report their concussion symptoms.13
Our data indicate that the type of symptoms recorded for high school athletes who sustained concussions differed between males and females. In year 1, when only the primary symptom was recorded, males were more likely to report amnesia and confusion/disorientation—both cognitive symptoms—than were females. Females did not report any single primary symptom more often than males. In year 2, when all symptoms were listed, males again were more likely to report amnesia and confusion/disorientation (cognitive symptoms) than were females. Females reported drowsiness (neurobehavioral symptom) and sensitivity to noise (somatic symptom) more than did males. These data indicate that male and female high school students who suffer concussions may have different types of symptoms and, thus, may present differently to health care professionals. Without adequate symptom assessment, the neurobehavioral or somatic symptoms more commonly described by females may be more easily missed or attributed to other conditions, such as stress, depression, or anxiety.50 Clearly, more information is needed to interpret subtle differences in postconcussive symptoms, but ATs need to be aware that after a concussion, the symptoms reported by females should be linked to the concussion until conflicting neuropsychological conditions can be ruled out.
From a clinical perspective, it is important to evaluate each concussion individually and to record all symptoms reported by the injured athlete. Some symptoms, especially in the neurobehavioral category, are often overlooked on a sideline or initial assessment. Because high school girls are more likely to display these symptoms, ATs should initially associate those types of symptoms with a potential concussion and should withhold an athlete from contact activity until the symptoms subside. Although no investigators have been able to accurately assess severity of the sport-related concussion based on the symptoms presented, the scales used, either self-reported or recorded, are valid assessment tools.43,47 The differentiation of concussion symptoms and categorization into cognitive, neurobehavioral, and somatic groups may help to predict outcomes, RTP criteria, or likelihood of experiencing postconcussion syndrome in the future.
Symptom Resolution Time
Research examining the SRT for high school athletes is sparse. In our study, most symptoms associated with sport-related concussion resolved in 3 days or fewer, and the SRT did not differ between males and females. This rapid resolution of symptoms is consistent with other findings in collegiate athletes. In a study of more than 1600 collegiate football players,29 nearly 90% of all concussed athletes' symptoms resolved within 7 days of the initial injury. Collie et al41 reported that participants' SRTs ranged between 2 and 10 days. Maddocks and Saling51 noted that although certain concussion symptoms (such as headache and nausea) resolved within 5 days, persistent neuropsychological changes were still apparent at 5 days postinjury. Furthermore, concussions are often accompanied by cognitive problems, such as increased processing time and short-term memory loss, which can easily be overlooked if they are not carefully assessed. Lovell et al52 demonstrated that it takes 1 week or longer to resolve the neurocognitive deficits seen with “ding” or grade I concussions in high school athletes. Thus, symptom resolution is required before returning to play, but the evaluation of symptoms cannot be the only determining factor in making these decisions.
Time to RTP
The median time to RTP for all participants was 3 to 6 days and was not different between males and females. These findings agree with those of another large observational cohort investigation23 involving high school athletes, in which a median time to RTP of 3 days was reported. Both groups studied athletes participating in similar high school sports and used the same operational definition of concussion. Powell and Barber-Foss,10 however, captured the RTP data with greater precision than RIO permitted. We were able to report only the median category of RTP, but the median time to RTP for all concussions reported by Powell and Barber-Foss10 falls within our reported category. Powell and Barber-Foss,10 however, did not report or conduct data analysis comparing time to RTP between sexes. Comparison of their reported data for each category indicates findings similar to ours because no difference was noted in the RTP time between sexes after concussion (Table 8).
Strengths
We are the first to examine concussion symptoms, SRT, and RTP time in a national high school population. This study provides insight into concussion presentation, evaluation, and management at the high school level. The methods used in RIO have undergone internal validity checks with high sensitivity, specificity, and positive predictive values.53 These values, combined with the very low failure-to-report and incomplete-variable rates, indicate that this is the highest-quality data available for a national sample of US high school athletes. Furthermore, no confounding variables, such as protective equipment or initial or recurrent injury, affected the results.
Limitations
Our study had several limitations. First, no uniform definition of concussion was used by ATs reporting to RIO. As a result, disparities in the data may reflect disparities in the interpretations of concussion by the reporting ATs. Additionally, injuries were only included in the data set if the participating AT was aware of the injury and if the injury had a time-loss factor of one or more days. The software was also changed within our study period, ultimately improving the instrument. However, we were unable to combine the data for both years to analyze the number of symptoms reported. Finally, there was no operational definition for grading the severity of the concussion, and the clinicians' grading was arbitrary. Therefore, we were not able to analyze concussion severity as a potential confounding factor.
Conclusions
Many authors3,11,22,36 have suggested that differences between sexes exist in sport-related concussion. Based on SRT and RTP time, little difference is evident in the severity or outcome of concussions sustained between sexes in high school athletes. However, male and female high school athletes appeared to present with different types of symptoms after a sport-related concussion. Males reported more cognitive symptoms, whereas females reported more symptoms in the neurobehavioral and somatic categories. Symptom evaluation is only one component of a concussion evaluation, and each symptom should be evaluated and monitored to resolution before RTP. Neurocognitive assessments, balance measurements, symptoms, and the physical examination should be used collectively to evaluate concussions.
Acknowledgments
This research was funded by the Centers for Disease Control and Prevention (CDC), grant no. R49/CEOOO674-01.
REFERENCES
- 1.National Federation of State High School Associations. 2005–2006 High School Athletics Participation Survey. http://www.nfhs.org/sports.aspx. Accessed July 17, 2007.
- 2.Langlois J. A., Rutland-Brown W., Wald M. M. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375–378. doi: 10.1097/00001199-200609000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Gessel L. M., Fields S. K., Collins C. L., Dick R. W., Comstock R. D. Concussions among United States high school and collegiate athletes. J Athl Train. 2007;42(4):495–503. [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Sports-related injuries among high school athletes—United States, 2005–06 school year. MMWR Morb Mortal Wkly Rep. 2006;55(38):1037–1040. [PubMed] [Google Scholar]
- 5.Leblanc K. E. Concussion in sport: diagnosis, management, return to competition. Compr Ther. 1999;25(1):39–45. doi: 10.1007/BF02889833. [DOI] [PubMed] [Google Scholar]
- 6.Georgia Institute of Technology. Cumulative effects of concussions. Georgia Tech Sports Med Perform Newsl. 2002;11(3):3. [Google Scholar]
- 7.McKeever C. K., Schatz P. Current issues in the identification, assessment, and management of concussions in sports-related injuries. Appl Neuropsychol. 2003;10(1):4–11. doi: 10.1207/S15324826AN1001_2. [DOI] [PubMed] [Google Scholar]
- 8.Ruchinskas R. A., Francis J. P., Barth J. T. Mild head injury in sports. Appl Neuropsychol. 1997;4(1):43–49. doi: 10.1207/s15324826an0401_5. [DOI] [PubMed] [Google Scholar]
- 9.US Department of Education. Title IX: 25 years of progress, 1997. http://www2.ed.gov/pubs/TitleIX/index.html. Accessed February 5, 2008.
- 10.Powell J. W., Barber-Foss K. Traumatic brain injury in high school athletes. JAMA. 1999;282(10):958–963. doi: 10.1001/jama.282.10.958. [DOI] [PubMed] [Google Scholar]
- 11.Covassin T., Swanik C. B., Sachs M. L. Sex differences and the incidence of concussions among collegiate athletes. J Athl Train. 2003;38(3):238–244. [PMC free article] [PubMed] [Google Scholar]
- 12.Notebaert A. J., Guskiewicz K. M. Current trends in athletic training practice for concussion assessment and management. J Athl Train. 2005;40(4):320–325. [PMC free article] [PubMed] [Google Scholar]
- 13.McCrea M., Hammeke T., Olsen G., Leo P., Guskiewicz K. Unreported concussion in high school football players: implications for prevention. Clin J Sport Med. 2004;14(1):13–17. doi: 10.1097/00042752-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Farace E., Alves W. M. Do women fare worse? A meta-analysis of gender differences in traumatic brain injury outcome. J Neurosurg. 2000;93(4):539–545. doi: 10.3171/jns.2000.93.4.0539. [DOI] [PubMed] [Google Scholar]
- 15.Farin A., Deutsch R., Biegon A., Marshall L. F. Sex-related differences in patients with severe head injury: greater susceptibility to brain swelling in female patients 50 years of age and younger. J Neurosurg. 2003;98(1):32–36. doi: 10.3171/jns.2003.98.1.0032. [DOI] [PubMed] [Google Scholar]
- 16.Kraus J. F., Peek-Asa C., McArthur D. The independent effect of gender on outcomes following traumatic brain injury: a preliminary investigation. Neurosurg Focus. 2000;8(1):5. doi: 10.3171/foc.2000.8.1.156. [DOI] [PubMed] [Google Scholar]
- 17.Morrison W. E., Arbelaez J. J., Fackler J. C., De Maio A., Paidas C. N. Gender and age effects on outcome after pediatric traumatic brain injury. Pediatr Crit Care Med. 2004;5(2):145–151. doi: 10.1097/01.pcc.0000112373.71645.2a. [DOI] [PubMed] [Google Scholar]
- 18.Bramlett H. M., Dietrich W. D. Neuropathological protection after traumatic brain injury in intact female rats versus males or ovariectomized females. J Neurotrauma. 2001;18(9):891–900. doi: 10.1089/089771501750451811. [DOI] [PubMed] [Google Scholar]
- 19.Emerson C. S., Headrick J. P., Vink R. Estrogen improves biochemical and neurologic outcome following traumatic brain injury in male rats, but not in females. Brain Res. 1993;608(1):95–100. doi: 10.1016/0006-8993(93)90778-l. [DOI] [PubMed] [Google Scholar]
- 20.Stein D. G., Hoffman S. W. Estrogen and progesterone as neuroprotective agents in the treatment of acute brain injuries. Pediatr Rehabil. 2003;6(1):13–22. doi: 10.1080/1363849031000095279. [DOI] [PubMed] [Google Scholar]
- 21.Covassin T., Schatz P., Swanik C. B. Sex differences in neuropsychological function and post-concussion symptoms of concussed collegiate athletes. Neurosurgery. 2007;61(2):345–350. doi: 10.1227/01.NEU.0000279972.95060.CB. [DOI] [PubMed] [Google Scholar]
- 22.Broshek D. K., Kaushik T., Freeman J. R., Erlanger D., Webbe F., Barth J. T. Sex differences in outcome following sports-related concussion. J Neurosurg. 2005;102(5):856–863. doi: 10.3171/jns.2005.102.5.0856. [DOI] [PubMed] [Google Scholar]
- 23.Lovell M. R., Collins M. W., Iverson G. L., et al. Recovery from mild concussion in high school athletes. J Neurosurg. 2003;98(2):296–301. doi: 10.3171/jns.2003.98.2.0296. [DOI] [PubMed] [Google Scholar]
- 24.Rechel J. A., Yard E. E., Comstock R. D. An epidemiologic comparison of high school sports injuries sustained in practice and competition. J Athl Train. 2008;43(2):197–204. doi: 10.4085/1062-6050-43.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shankar P. R., Fields S. K., Collins C. L., Dick R. W., Comstock R. D. Epidemiology of high school and collegiate football injuries in the United States, 2005–2006. Am J Sports Med. 2007;35(8):1295–1303. doi: 10.1177/0363546507299745. [DOI] [PubMed] [Google Scholar]
- 26.Yard E. E., Collins C. L., Dick R. W., Comstock R. D. An epidemiologic comparison of high school and college wrestling injuries. Am J Sports Med. 2008;36(1):57–64. doi: 10.1177/0363546507307507. [DOI] [PubMed] [Google Scholar]
- 27.US Census Bureau. Census regions of the United States. http://www.census.gov/const/regionmap.pdf. Accessed July 9, 2010.
- 28.Hopkins W. G., Marshall S. W., Batterham A. M., Hanin J. Progressive statistics for studies in sports medicine and exercise science. Med Sci Sports Exerc. 2009;41(1):3–13. doi: 10.1249/MSS.0b013e31818cb278. [DOI] [PubMed] [Google Scholar]
- 29.McCrea M., Guskiewicz K. M., Marshall S. W., et al. Acute effects and recovery time following concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290(19):2556–2563. doi: 10.1001/jama.290.19.2556. [DOI] [PubMed] [Google Scholar]
- 30.Pellman E. J., Lovell M. R., Viano D. C., Casson I. R., Tucker A. M. Concussion in professional football: neuropsychological testing, part 6. Neurosurgery. 2004;55(6):1290–1305. doi: 10.1227/01.neu.0000149244.97560.91. [DOI] [PubMed] [Google Scholar]
- 31.Delaney J. S., Lacroix V. J., Leclerc S., Johnston K. M. Concussions among university football and soccer players. Clin J Sport Med. 2002;12(6):331–338. doi: 10.1097/00042752-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 32.Thurman D. J., Branche C. M., Sneizek J. E. The epidemiology of sports-related traumatic brain injuries in the United States: recent developments. J Head Trauma Rehabil. 1998;13(2):1–8. doi: 10.1097/00001199-199804000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Guskiewicz K. M., Weaver N. L., Padua D. A., Garrett W. E., Jr Epidemiology of concussion in collegiate and high school football players. Am J Sports Med. 2000;28(5):643–650. doi: 10.1177/03635465000280050401. [DOI] [PubMed] [Google Scholar]
- 34.Collins M. W., Iverson G. L., Lovell M. R., McKeag D. B., Norwig J., Maroon J. On-field predictors of neuropsychological and symptom deficit following sports-related concussion. Clin J Sport Med. 2003;13(4):222–229. doi: 10.1097/00042752-200307000-00005. [DOI] [PubMed] [Google Scholar]
- 35.Erlanger D., Feldman D., Kutner K., et al. Development and validation of a web-based neuropsychological test protocol for sports-related return-to-play decision-making. Arch Clin Neuropsychol. 2003;18(3):293–316. [PubMed] [Google Scholar]
- 36.Barnes B. C., Cooper L., Kirkendall D. T., McDermott T. P., Jordan B. D., Garrett W. E., Jr Concussion history in elite male and female soccer players. Am J Sports Med. 1998;26(3):433–438. doi: 10.1177/03635465980260031601. [DOI] [PubMed] [Google Scholar]
- 37.Torg J. Athletic Injuries to the Head, Neck, and Face. St Louis, MO: Mosby; 1991. [Google Scholar]
- 38.Kelly J. P., Rosenberg J. H. The development of guidelines for the management of concussion in sports. J Head Trauma Rehabil. 1998;13(2):53–65. doi: 10.1097/00001199-199804000-00008. [DOI] [PubMed] [Google Scholar]
- 39.Kelly J. P. Loss of consciousness: pathophysiology and implications in grading and safe return to play. J Athl Train. 2001;36(3):249–252. [PMC free article] [PubMed] [Google Scholar]
- 40.Cantu R. C. Posttraumatic retrograde and anterograde amnesia: pathophysiology and implications in grading and safe return to play. J Athl Train. 2001;36(3):244–248. [PMC free article] [PubMed] [Google Scholar]
- 41.Collie A., Makdissi M., Maruff P., Bennell K., McCrory P. Cognition in the days following concussion: comparison of symptomatic versus asymptomatic athletes. J Neurol Neurosurg Psychiatry. 2006;77(2):241–245. doi: 10.1136/jnnp.2005.073155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Asplund C. A., McKeag D. B., Olsen C. H. Sport-related concussion: factors associated with prolonged return to play. Clin J Sport Med. 2004;14(6):339–343. doi: 10.1097/00042752-200411000-00003. [DOI] [PubMed] [Google Scholar]
- 43.Lovell M. R., Iverson G. L., Collins C. W., et al. Measurement of symptoms following sports-related concussion: reliability and normative data for the post-concussion scale. Appl Neuropsychol. 2006;13(3):166–174. doi: 10.1207/s15324826an1303_4. [DOI] [PubMed] [Google Scholar]
- 44.Broglio S. P., Puetz T. W. The effect of sport concussion on neurocognitive function, self-report symptoms and postural control: a meta-analysis. Sports Med. 2008;38(1):53–67. doi: 10.2165/00007256-200838010-00005. [DOI] [PubMed] [Google Scholar]
- 45.Theye F., Mueller K. A. “Heads up”: concussions in high school sports. Clin Med Res. 2004;2(3):165–171. doi: 10.3121/cmr.2.3.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Delaney J. S., Lacroix V. J., Gagne C., Antoniou J. Concussions among university football and soccer players: a pilot study. Clin J Sport Med. 2001;11(4):234–240. doi: 10.1097/00042752-200110000-00005. [DOI] [PubMed] [Google Scholar]
- 47.Piland S. G., Motl R. W., Ferrara M. S., Peterson C. L. Evidence for the factorial and construct validity of a self-report concussion symptoms scale. J Athl Train. 2003;38(2):104–112. [PMC free article] [PubMed] [Google Scholar]
- 48.Lovell M. R., Collins M. W. Neuropsychological assessment of the college football player. J Head Trauma Rehabil. 1998;13(2):9–26. doi: 10.1097/00001199-199804000-00004. [DOI] [PubMed] [Google Scholar]
- 49.Gioia G. A., Collins M., Isquith P. K. Improving identification and diagnosis of mild traumatic brain injury with evidence: psychometric support for the acute concussion evaluation. J Head Trauma Rehabil. 2008;23(4):230–242. doi: 10.1097/01.HTR.0000327255.38881.ca. [DOI] [PubMed] [Google Scholar]
- 50.Santa Maria M. P., Pinkston J. B., Miller S. R., Gouvier W. D. Stability of postconcussion symptomatology differs between high and low responders and by gender but not by mild head injury status. Arch Clin Neuropsychol. 2001;16(2):133–140. doi: 10.1016/s0887-6177(99)00059-1. [DOI] [PubMed] [Google Scholar]
- 51.Maddocks D., Saling M. Neuropsychological deficits following concussion. Brain Inj. 1996;10(2):99–103. doi: 10.1080/026990596124584. [DOI] [PubMed] [Google Scholar]
- 52.Lovell M. R., Collins M. W., Iverson G. L., Johnston K. M., Bradley J. P. Grade 1 or “ding” concussions in high school athletes. Am J Sports Med. 2004;32(1):47–54. doi: 10.1177/0363546503260723. [DOI] [PubMed] [Google Scholar]
- 53.Comstock D., Yard E., Collins C. Summary report, High School Sports-Related Injury Surveillance Study, 2006–2007. Center for Injury Research and Policy, The Research Institute at Nationwide Children's Hospital. http://injuryresearch.net/resources/1/rio/2006-07HighSchoolRIOSummaryReport.pdf. Accessed July 13, 2010.