Abstract
Purpose
This study was aimed to determine the status and related factors of age-appropriate immunization among urban-rural children aged 24-35 months in a 2005 population-based survey in Nonsan, Korea.
Materials and Methods
We conducted household survey and provider check using questionnaire and checklist to obtain data on immunization status for children, aged 24-35 months. Age-appropriate immunization was defined as status of receiving the fourth diphtheria-tetanus-pertussis (4 DTP), 3 Polio, the first measles-mumps-rubella (1 MMR) doses, and the 4 : 3 : 1 series.
Results
Age-appropriate immunization rates were 51.7% for 4 DPT, 88.0% for 3 Polio, 87.9% for 1 MMR, and 50.3% for the 4 : 3 : 1 series. First-born children, lower perceived barrier scores, and higher perception of immunization data were significantly related to age-appropriate immunization.
Conclusion
The findings indicated that age-appropriate immunization rate could be improved by implementing reminder/recall service and providing the knowledge about immunization. Identification and consideration related factors would improve immunization rate and age-appropriate immunization.
Keywords: Related factors, age-appropriate immunization, DPT, Polio, MMR
INTRODUCTION
Childhood immunization is recognized as the most effective medical means to control infectious diseases; it is cost-effective, reduces morbidity, and prevents further outbreaks of infectious disease.1 Although immunization is remarkably effective, children are still becoming infected with preventable diseases, resulting in debilitating disorders and even death. Support for immunization over other public health issues has been signaled as a social priority.2
An outbreak of a measles epidemic among U.S. children focused attention on the adequacy of and barriers to immunization. The primary cause of measles epidemic was a failure to provide vaccines on schedule. When compliance with a vaccination schedule occurs that results in a high national level of vaccination, the risk of periodic epidemics decreases. In the USA, the proportion of children who are immunized against measles has increased dramatically over the past few decades. To avoid future outbreaks, it is crucial to attain high coverage levels by ensuring timely vaccinations. Even with an expected outbreak of measles and pertussis in the future, age-appropriate immunization will prevent another resurgence and epidemic of measles.3
To achieve maximal protection against vaccine-preventable disease, age-appropriate immunization means that children receive all immunization within recommended age intervals fully "on-time". Maximum immunity is not achieved if children have too early or delayed vaccination.4 Age-appropriate immunization indicators more accurately reflect adequacy of protection for childhood than up-to-date indicators at both individual and population levels. Therefore, age-appropriate immunization can be an indicator for problems of accessibility of immunization services.5-7
Age-appropriate immunization has been defined as being on schedules by a number of public healthcare agencies such as: CDC,8 Immunization Guidelines of Advisory Committee on Immunization Practice (ACIP), American Academy of Pediatricians, and American Academy of Family Physicians (AAFP). Age-appropriate immunization is generally defined as being not more than 1 month between minimum age and the final time of immunization schedule. When an interval to next dose by each vaccine meets the minimum interval to next dose, it is classified as an age-appropriate immunization. For example, it is reported that DPT and Polio vaccines are not effective when they are conducted at too early an age,9 and the vaccine of measles and Hepatitis B, and Haemophilus influenza vaccine can't take maximum effect if not provided at the optimum age-appropriate time.3,10,11 As a result, some countries changed their targets for immunization to enhance immunization rates by ensuring age-appropriate immunizations.12,13
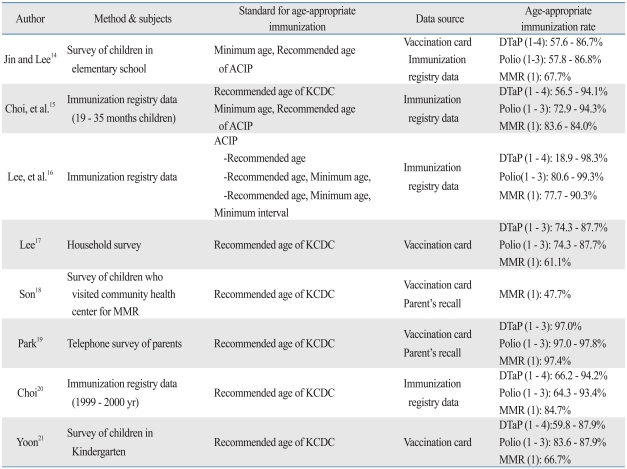
In Korea, age-appropriate immunization rate was highly variable due to application of different standard for age-appropriate immunization (recommended age, minimum age, minimum interval and grace period), survey methods (household survey, registry data, provider check, questionnaire, interview, telephone survey), and subjects (different age), and data source (vaccination card, parent's recall, registry data) (Table 1).14-21 The immunization rate for the vaccine of the National Immunization Program was variable, and this may be due to different study design, time, subject, geographical area and other factors. We carefully considered such factors to ensure more valid and reliable results.
Table 1.
A Studies That have Examined Age-Appropriate Immunization in Korea
ACIP, Advisory committee on Immunization Practice; KCDC, Korea Centers for Disease Control and Prevention.
As infants have no capacity to make decisions for themselves, their immunization or non-immunization is decided by their mothers and primary caregiver. In recent years, beliefs and attitudes about preventive activities have been emphasized as an important disease prevention. Understanding these beliefs and attitude can help explain why caregivers make decisions regarding age-appropriate immunization. Once an understanding of attitudes has been established, effective strategies to educate and change behaviors can be implemented. Most studies of childhood immunization have been focused on the socio-demographic characteristics, and belief and attitude of primary caregiver or mother. Findings suggest that mother's age is an important factor, the older she is, the more likely her infants will be immunized in a timely manner; that is, mothers under 30 have low age-appropriate immunization rates for their children.3
The purpose of this study was to investigate the prevalence and related factors of age-appropriate immunization as it occurs for 4 : 3 : 1 series (4 DPT, 3 Polio, 1 MMR), suggesting integrative and comprehensive information of immunization for defining specific intervention strategies and increasing immunization compliance in a urban-rural children of Korea. The risk of vaccine-preventable disease epidemics increases in spite of high national level of vaccination (e.g., measles). Inappropriate vaccination (e.g., early and/or late) is an important issue, since any inappropriate period represents inadequate protection against vaccine-preventable disease (e.g., DTP, Polio). Vaccination of BCG and Hepatitis B was excluded in this study because it could be determined by provider immediately after birth, and vaccination of varicella was also excluded because it was included in Korean National Immunization Program in 2005.
This study attempted to find immunization rates with a belief that the rates would increase attention to and resolutions for barriers to immunization.
MATERIALS AND METHODS
Subjects of research and methods of survey
Nonsan city has both urban and rural population and a low rate of migration. The subjects of this study were children, aged 24-35 months, in Nonsan city, Korea. Local residence registry data indicated that there were 1,038 children available. We excluded children whose caregivers lived outside of the city (n = 163), refused to answer (n = 111), or did not complete the survey (n = 47). There was no significant difference in gender, age and residential area between children who were included for the analysis and those who were not.
The children's caregivers were contacted and permission was given for 717 children to participate in the study. The group of 717 was divided into rural and urban, based on residence.
A household survey was conducted between February and April, 2005. Interviewers were students from medical schools or schools of public health, who were trained on the study objectives and interviewing methods. We sent a letter to the study subjects before the survey and visited their house. When we could not meet the subjects after three visits, we ascertained the subjects' whereabouts by neighbours or representatives of the town. Many of them did not reside in the town or were living in facilities for orphans or the poor. The primary caregivers of all the children were interviewed and gave written informed consent.
The questionnaire was composed of socio-demographic characteristics and mother's beliefs about childhood immunization. The questionnaire measured mother's beliefs regarding immunization and included perceived barriers to immunization, perceived benefit of immunization, perceived susceptibility to disease, perceived severity of disease being vaccinated against, cues to action, self-efficacy, and knowing when the next shot will be. Each dimension of the questionnaire consisted of 1 or 2 items with 5 point score scale. Immunization history was identified according to a child's vaccination card with additional immunization data collected from medical records of private clinics and immunization registry data of public health center.
Age-appropriate immunization
In this study, age-appropriate immunization was defined as having occurred when a child receives all doses in 4 : 3 : 1 series within 30 days of the recommended age considering minimum recommended age and intervals between doses according to Guideline of Immunization of Korea Centers for Disease Control and Prevention. Age-appropriate immunization was counted from minimum age to recommended age for routine administration according to birth date. For example, the time of age-appropriate immunization for the first dose of DTaP/DTP can be counted from 43 days to 92 days according to the minimum age for the first dose of DTaP/DTP "6 weeks" and recommended age for routine administration "2 months" after birth. And when immunization was administered within a 4 day-grace period, it was regarded as the age-appropriate immunization. The 4-day grace period was defined as 4 days before the specified minimum age, and 4 days before or after minimum interval to next dose.
Statistical analysis
For analysis, respondents were classified into two groups according to age-appropriate immunization status in the 4 : 3 : 1 series. The difference in the age-appropriate immunization according to the socio-demographic characteristics of household was analyzed by χ2 test. The difference in beliefs about childhood immunization was analyzed using a t-test. Finally, logistic regression analysis was used to determine related factors with age-appropriate immunization status by inputting the variables significantly deduced in the univariate analysis and mother's beliefs. All statistical analyses were done with SPSS win software, version 13.0 (SPSS Inc., Chicago, USA). In implementing the analysis, non-responses were treated as missing values.
RESULTS
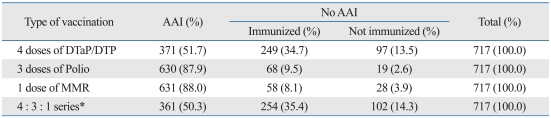
Age-appropriate immunization rate by vaccination type
Age-appropriate immunization rates varied; 51.7%, 88.0%, and 87.9% for each 4 DPT, 3 Polio, and 1 MMR, respectively. Only 50.3% had received all vaccinations in 4 : 3 : 1 series (Table 2).
Table 2.
Age-Appropriate Immunization at 4 : 3 : 1 Series* Unit: n (%)
AAI, age-appropriate immunization.
*4 doses of DTaP/DTP, 3 doses of Polio, and 1 dose of MMR.
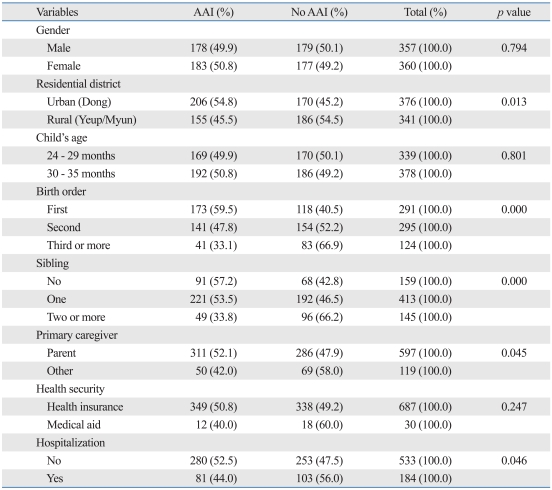
Age-appropriate immunization by general characteristics of children
The age-appropriate immunization was higher for those living in the urban area (54.8%), compared with those living in the rural area (45.5%, p < 0.05). Birth order was an indicator for age-appropriate immunization; the later the birth order, the lower the age-appropriate immunization rate (p < 0.01). Number of siblings in the family was also an indicator for age-appropriate immunization; the more siblings in the family, the lower the rate of age-appropriate immunization (p < 0.01). However, age-appropriate immunization was not statistically significant by the variables such as gender, age, and health security (Table 3).
Table 3.
Age-Appropriate Immunization by General Characteristics of Children Unit: n (%)
AAI, age-appropriate immunization.
Total may not sum to 717 owing to missing values.
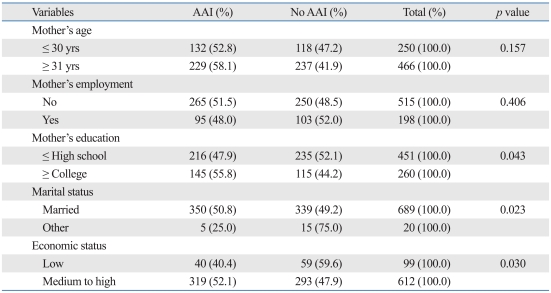
Age-appropriate immunization by characteristics of mothers and a household
The educational attainment of mother/caregiver had an affect on age-appropriate immunization rates of their children; mothers who did not graduate from college had children with age-appropriate immunization rates of 47.9%, while college graduates had children with age-appropriate immunization rates of 55.8% (p < 0.05).
Marital status affected age-appropriate immunization rates, with 50.8% compliance with mothers who had a spouse, and 25.0% compliance in a single parent family (p < 0.05).
Economic status of a household also affected compliance rates, with poor households reporting 40.4% of age-appropriate immunization rates, while average to above households reported 52.1% of age-appropriate immunization rates (Table 4).
Table 4.
Age-Appropriate Immunization by General Characteristics of Mother and Household
AAI, age-appropriate immunization.
Total may not sum to 717 owing to missing values.
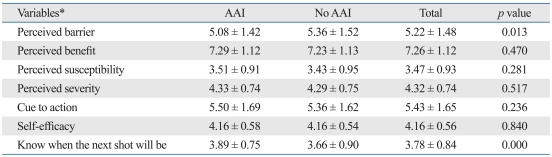
Mother's belief scores about child immunization
The perceived barrier to childhood immunization was a measure of accessibility as distance and time. In the failure-to-comply age-appropriate immunization group the perceived barrier score was 5.36, while the perceived barrier to immunization was 5.08 for the compliance to age-appropriate immunization group.
The perceived benefit of childhood immunization was similar between the failure-to-comply age-appropriate immunization group and compliance to age-appropriate immunization group. There was also no significant difference between the two groups in regard to the susceptibility to diseases that are preventable if vaccinated.
However, the perception of when the next shot would be immunization date was higher in the age-appropriate immunization group (Table 5).
Table 5.
Mother's Belief Scores about Childhood Immunization
AAI, age-appropriate immunization.
*Each dimension of questionnaire consist of 1 or 2 items with 5 point score scale.
Values are presented as mean ± SD.
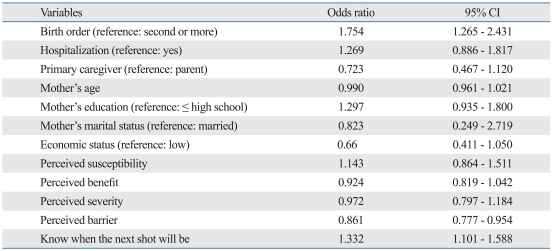
Multivariate logistic regression model on the related factors of age-appropriate immunization
Using logistic regression, the input variables were birth order, primary care-giver, experience of hospitalization, educational level, marital status of mother, the economic status of a household, mothers' beliefs, perceived barrier, perceived susceptibility, perceived severity, perceived benefit, cue to action, and knowing when the next shot would be. Results of the logistic regression model showed birth order, perceived barrier, and the perception of an immunization date predicted age-appropriate immunization status (p < 0.01). Compared with second or more late-born children, those who were first born children were 1.75 times more likely to have their age-appropriate immunization [95% confidence interval (CI): 1.27-2.43]. Also, the higher the perceived barrier scores, the lower the age-appropriate immunization (95% CI: 0.78-0.95), and the higher the perception of immunization date (95% CI: 1.10-1.59), the more the age-appropriate immunization (Table 6).
Table 6.
Related Factors of Age-Appropriate Immunization for 4 : 3 : 1 Series*
CI, confidence interval.
*4 doses of DTaP/DTP, 3 doses of Polio, and 1 dose of MMR, analyzed by multivariate logistic regression analysis.
DISCUSSION
One of the questions which this research set out to answer was at what rate was Korean children having age-appropriate immunizations. Results from this research showed that indicate 50.3% of the children in Nosan city of Korea received all doses in their 4 : 3 : 1 series on time. Age-appropriate immunization was higher for antigen-specific series that required fewer doses than series requiring more doses. Single dose MMR compliance rates were high, while 4 dose DTaP compliance was low. DTaP vaccine compliance was low in achieving age-appropriate immunization levels because non or delayed immunization was high in the 4th dose.3,22-24 Since the period between the 3rd and the 4th dose of DTaP is long and most national mandatory vaccination is completed within 12 months after birth, non and delayed immunization for DTaP and Polio are high, compared with other immunizations. An intervention focusing on the 4th dose of DTaP vaccination enhances the age-appropriate immunization rates of 4 : 3 : 1 series, and has been shown to result in a 10% increase in completed series.25,26
As the importance of the age-appropriate immunization is well established, why are the rates not higher? Perhaps, it is difficult for caregivers to know whether their children have received/completed all mandatory immunizations as there are so many. This is further complicated by poor record keeping. A review of research reveals that very little is known about the risk factors for age-appropriate immunization in childhood immunization.
According to our present study, the related factors for age-appropriate immunizations were residential district, birth order, the number of siblings, primary care-giver, mother's educational level, marital status, and economic status. In regards to residential district, the age-appropriate immunization rate was higher in the urban area than in the rural area. This can in part be interpreted by easy accessibility to a medical institution, because there are more facilities in the urban areas, and shorter traveling times make them more accessible to the facilities. The results from this study are consistent with those which showed that age-appropriate immunizations are low when people residing in a region have difficulty to access to a medical institution because of long distance.13,27 In Korea, residential districts can be a barrier for accessibility to medical institutions as they can limit the date and time when immunizations are provided. If a working caregiver is denied time-off from her work place and the local health district is also inflexible with providing available times for immunization, there is clearly a conflict. Given the fact that more than 60% of national mandatory immunization were implemented by public health centers in the survey area, this may alone explain the difference in the age-appropriate immunization; the degree of the perception of barriers in terms of distance and time. Until now, the strategies to reduce barriers to immunization have carried out by emphasizing the economic aspects (free immunization). However, it is necessary in the future to consider the accessibility, in terms of distance and time, to the institution providing immunization.
In the present study, birth order and the number of siblings were related with the implementation of the age-appropriate immunization. These findings are consistent with what has often been reported; i.e., later birth order and more siblings result in less compliance to age-appropriate immunization.6,7,25,28-37 The present study showed that being born first lowered the perceived barrier scores, and raised the knowledge of the next immunization dates, resulting in higher compliance to age-appropriate immunization. There might be a number of factors contributing to the failure of late order siblings to complete immunization series. Lack of time and resources with larger families can result in attention dispersal. Also, growing confidence in the role of being a mother, as their children grow, may result in perceptions of children as less threatened or better protected by a mother's perceived competency.
The economic level and income conditions are important factors for compliance of immunization and age-appropriate immunization.34 Nevertheless, attempts to relieve economic impacts on immunization rates by providing free immunization12 have not resulted in increased immunization rates among those in lower economic categories.38,39 In Korea, free immunization is also provided when people use public health centers, and the present study also indicates that barriers-including economic factors affect age-appropriate immunization.
There was no difference in the scores of benefit of immunization and the susceptibility and severity of a disease between two groups. Surveys were conducted after immunization, not before it. Therefore, if the side effect of vaccine didn't happen and an infant didn't suffer from an infectious disease, we can conclude that the immunization of the past was good. Since it is perceived that there is little possibility to be sick because of the previous immunization, it is thought that the relationship between the susceptibility and severity of a disease and the fulfillment of behavior wasn't discovered.
There was no statistically significant difference in the scores of benefit of immunization. In addition, the susceptibility and severity of a disease, cue to action, and self-efficacy were higher in the age-appropriate immunization group than in the no age-appropriate immunization group.
However, perceptions of immunization dates were high in the age-appropriate immunization group. Knowing when immunization is scheduled enhances the possibility of carrying out the behavior.29 Especially, if the caregiver thinks that it is important to be immunized timely, the caregiver is Universilikely to act in a timely way.2,9,28,30,40 These results imply that it is necessary to make a policy to reduce the barrier to time and distance.
To our best knowledge, this study is the first report on the factors associated with age-appropriate immunization for 4 : 3 : 1 series (4 DPT, 3 Polio, 1 MMR) in Korea. However, our data were obtained from one limited area, and therefore, are not representatives of entire Korea. We conducted household survey and provider check using the questionnaire and checklist to obtain data. But, immunization history was identified according to a child's vaccination card with additional immunization data collected from medical records of private clinics and immunization registry data of public health center. Therefore, children without a vaccination card and/or medical data, and registry data were excluded. As a result, we might have overestimated the immunization rate. This study was cross-sectional design, therefore, it was not possible to clearly state that exposure or outcome was the cause and which effect. Our study was focused primarily on socio-demographic characteristics and mother's beliefs about childhood immunization, therefore, did not include many other factors, especially clinical condition of children and more objective measurement about the geographic distance between house and hospital or clinic. Children with clinical conditions (e.g., URI) that were contraindication of vaccination were 22.2-60.0%, which ranged widely, depending on the type and dose of vaccination. Prevalence of clinical condition was 60% in 1 dose of DTaP/DTP, 25% in 2 doses of DTaP/DTP, 35.3% in 3 doses of DTaP/DTP, 25.6% in 4 dose of DTaP/DTP, 40.0% in 1 dose of polio, 22.2% in 2 doses of polio, 35.3% in 3 doses of polio, and 40.0% in 1 dose of MMR. These were not categorized according to age-appropriate immunization; therefore, we might have underestimated the immunization rate.
ACKNOWLEDGEMENTS
This work was supported by a grant from the Korea Centers for Disease Control and Prevention.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Ross A, Kennedy AB, Holt E, Guyer B, Hou W, Hughart N. Initiating the first DTP vaccination age-appropriately: a model for understanding vaccination coverage. Pediatrics. 1998;101:970–974. doi: 10.1542/peds.101.6.970. [DOI] [PubMed] [Google Scholar]
- 2.Wood DL American Academy of Pediatrics Committee on Community Health Services; American Academy of Pediatrics Committee on Practice and Ambulatory Medicine. Increasing immunization coverage. American Academy of Pediatrics Committee on Community Health Services. American Academy of Pediatrics Committee on Practice and Ambulatory Medicine. Pediatrics. 2003;112:993–996. doi: 10.1542/peds.112.4.993. [DOI] [PubMed] [Google Scholar]
- 3.Luman ET, McCauley MM, Stokley S, Chu SY, Pickering LK. Timeliness of childhood immunizations. Pediatrics. 2002;110:935–939. doi: 10.1542/peds.110.5.935. [DOI] [PubMed] [Google Scholar]
- 4.Freeman VA, DeFriese GH. The challenge and potential of childhood immunization registries. Annu Rev Public Health. 2003;24:227–246. doi: 10.1146/annurev.publhealth.24.100901.140831. [DOI] [PubMed] [Google Scholar]
- 5.Bolton P, Hussain A, Hadpawat A, Holt E, Hughart N, Guyer B. Deficiencies in current childhood immunization indicators. Public Health Rep. 1998;113:527–532. [PMC free article] [PubMed] [Google Scholar]
- 6.Dombkowski KJ, Lantz PM, Freed GL. Role of health insurance and a usual source of medical care in age-appropriate vaccination. Am J Public Health. 2004;94:960–966. doi: 10.2105/ajph.94.6.960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dombkowski KJ, Lantz PM, Freed GL. Risk factors for delay in age-appropriate vaccination. Public Health Rep. 2004;119:144–155. doi: 10.1177/003335490411900207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC) National, state, and urban area vaccination coverage among children aged 19-35 months--United States, 2004. MMWR Morb Mortal Wkly Rep. 2005;54:717–721. [PubMed] [Google Scholar]
- 9.The national vaccine advisory committee. The measles epidemic. The problems, barriers and recommendations. JAMA. 1991;266:1547–1552. [PubMed] [Google Scholar]
- 10.Steiner RP, Hughes JA, Richardson TL, Looney SW, Clover RD, Rowe MG. Minimum time interval adjustment for 4-3-1 immunization rates among two-year-old children. Am J Prev Med. 1999;16:189–194. doi: 10.1016/s0749-3797(98)00095-6. [DOI] [PubMed] [Google Scholar]
- 11.Atkinson WL, Pickering LK, Schwartz B, Weniger BG, Iskander JK, Watson JC. General recommendations on immunization. Recommendations of the Advisory Committee on Immunization Practices (ACIP) and the American Academy of Family Physicians (AAFP) MMWR Recomm Rep. 2002;51:1–35. [PubMed] [Google Scholar]
- 12.Santoli JM, Setia S, Rodewald LE, O'Mara D, Gallo B, Brink E. Immunization pockets of need: science and practice. Am J Prev Med. 2000;19:89–98. doi: 10.1016/s0749-3797(00)00209-9. [DOI] [PubMed] [Google Scholar]
- 13.Hull BP, McIntyre PB. Timeliness of childhood immunisation in Australia. Vaccine. 2006;24:4403–4408. doi: 10.1016/j.vaccine.2006.02.049. [DOI] [PubMed] [Google Scholar]
- 14.Jin SM, Lee SG. Vaccination status in school entry aged-children and associated factors on timeliness of vaccinations. J Korean Soc Matern Child Health. 2007;11:44–53. [Google Scholar]
- 15.Choi YK, Kim KY, Lee MS, Na BJ, Kim EY, Shim YB, et al. Timeliness of infant immunization rate at public health centers. J Korean Soc Matern Child Health. 2008;12:181–198. [Google Scholar]
- 16.Lee SK, Lee KS, Lee MS, J SY, Kwon SS, Ryu SY, et al. Evaluation of expanded programme of immunization. Gunpo City Public Health Center; 2006. [Google Scholar]
- 17.Lee HS. Immunization rates of children receiving medical Assistance and An analysis of related factors for Immunization. Seoul: Yonsei University; 2004. MPH thesis. [Google Scholar]
- 18.Son YJ. Cognition and behaviors for the optimal MMR vaccination among the parents of 4-6 aged children. Busan: Inje University; 2004. MPH thesis. [Google Scholar]
- 19.Park JH. A survey on the vaccination status of young children in one area of Seoul. Seoul: Seoul National University; 2003. MPH thesis. [Google Scholar]
- 20.Choi SA. The use of immunization registry in public health center and its applications. Seoul: Seoul National University, Graduate School of Public Health; 2003. MPH thesis. [Google Scholar]
- 21.Yoon SJ. Research on the current status and need for vaccination in one area of Seoul. Seoul: Yonsei University; 1998. MPH thesis. [Google Scholar]
- 22.Dombkowski KJ, Lantz PM, Freed GL. The need for surveillance of delay in age-appropriate immunization. Am J Prev Med. 2002;23:36–42. doi: 10.1016/s0749-3797(02)00442-7. [DOI] [PubMed] [Google Scholar]
- 23.Strine TW, Luman ET, Okoro CA, McCauley MM, Barker LE. Predictors of age-appropriate receipt of DTaP dose 4. Am J Prev Med. 2003;25:45–49. doi: 10.1016/s0749-3797(03)00093-x. [DOI] [PubMed] [Google Scholar]
- 24.Mell LK, Ogren DS, Davis RL, Mullooly JP, Black SB, Shinefield HR, et al. Compliance with national immunization guidelines for children younger than 2 years, 1996-1999. Pediatrics. 2005;115:461–467. doi: 10.1542/peds.2004-1891. [DOI] [PubMed] [Google Scholar]
- 25.Bobo JK, Gale JL, Thapa PB, Wassilak SG. Risk factors for delayed immunization in a random sample of 1163 children from Oregon and Washington. Pediatrics. 1993;91:308–314. [PubMed] [Google Scholar]
- 26.Rodewald L, Maes E, Stevenson J, Lyons B, Stokley S, Szilagyi P. Immunization performance measurement in a changing immunization environment. Pediatrics. 1999;103:889–897. [PubMed] [Google Scholar]
- 27.Cotter JJ, Bramble JD, Bovbjerg VE, Pugh GB, McClish DK, Tipton G, et al. Timeliness of immunization of children in a Medicaid primary care case management managed care program. J Natl Med Assoc. 2002;94:833–840. [PMC free article] [PubMed] [Google Scholar]
- 28.Miller LA, Hoffman RE, Barón AE, Marine WM, Melinkovich P. Risk factors for delayed immunization against measles, mumps, and rubella in Colorado two-year-olds. Pediatrics. 1994;94:213–219. [PubMed] [Google Scholar]
- 29.Lieu TA, Black SB, Ray P, Chellino M, Shinefield HR, Adler NE. Risk factors for delayed immunization among children in an HMO. Am J Public Health. 1994;84:1621–1625. doi: 10.2105/ajph.84.10.1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Strobino D, Keane V, Holt E, Hughart N, Guyer B. Parental attitudes do not explain underimmunization. Pediatrics. 1996;98:1076–1083. [PubMed] [Google Scholar]
- 31.Marshall S, Swerissen H. A qualitative analysis of parental decision making for childhood immunization. Aust N Z J Public Health. 1999;23:543–545. doi: 10.1111/j.1467-842x.1999.tb01316.x. [DOI] [PubMed] [Google Scholar]
- 32.Angelillo IF, Ricciardi G, Rossi P, Pantisano P, Langiano E, Pavia M. Mothers and vaccination: knowledge, attitudes, and behaviour in Italy. Bull World Health Organ. 1999;77:224–229. [PMC free article] [PubMed] [Google Scholar]
- 33.Hughart N, Strobino D, Holt E, Guyer B, Hou W, Huq A, et al. The relation of parent and provider characteristics to vaccination status of children in private practices and managed care organizations in Maryland. Med Care. 1999;37:44–55. doi: 10.1097/00005650-199901000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Brenner RA, Simons-Morton BG, Bhaskar B, Das A, Clemens JD NIH-D.C. Initiative Immunization Working Group. Prevalence and predictors of immunization among inner-city infants: a birth cohort study. Pediatrics. 2001;108:661–670. doi: 10.1542/peds.108.3.661. [DOI] [PubMed] [Google Scholar]
- 35.Trauth JM, Zimmerman RK, Musa D, Mainzer H, Nutini JF. Do beliefs of inner-city parents about disease and vaccine risks affect immunization? J Natl Med Assoc. 2002;94:820–832. [PMC free article] [PubMed] [Google Scholar]
- 36.Heininger U, Zuberbühler M. Immunization rates and timely administration in pre-school and school-aged children. Eur J Pediatr. 2006;165:124–129. doi: 10.1007/s00431-005-0014-y. [DOI] [PubMed] [Google Scholar]
- 37.Dayan GH, Shaw KM, Baughman AL, Orellana LC, Forlenza Rl, Ellis A, et al. Assessment of delay in age-appropriate vaccination using survival analysis. Am J Epidemiol. 2006;163:561–570. doi: 10.1093/aje/kwj074. [DOI] [PubMed] [Google Scholar]
- 38.Bates AS, Fitzgerald JF, Dittus RS, Wolinsky FD. Risk factors for under immunization in poor urban infants. JAMA. 1994;272:1105–1110. [PubMed] [Google Scholar]
- 39.Szilagyi PG, Humiston SG, Shone LP, Barth R, Kolasa MS, Rodewald LE. Impact of vaccine financing on vaccinations delivered by health department clinics. Am J Public Health. 2000;90:739–745. doi: 10.2105/ajph.90.5.739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Richards A, Sheridan J. Reasons for delayed compliance with the childhood vaccination schedule and some failings of computerised vaccination registers. Aust N Z J Public Health. 1999;23:315–317. doi: 10.1111/j.1467-842x.1999.tb01263.x. [DOI] [PubMed] [Google Scholar]