Abstract
Objectives
To examine whether clinical severity is greater among children receiving ADHD care in primary care compared to those in specialty mental health clinics, and to examine how care processes and clinical outcomes vary by sector across three 6-month time intervals.
Method
Longitudinal cohort study of 530 children ages 5–11 years receiving ADHD care in primary care or specialty mental health clinics from November 2004 through September 2006 in a large, county-wide managed care Medicaid program.
Results
Clinical severity at study entry did not differ between children who received ADHD care in solely primary or specialty mental health care clinics. At three 6-month intervals, receipt of no care ranged from 34%–44% and unmet need for mental health services ranged from 13%–20%. In primary care, 80%–85% of children had at least one stimulant prescription filled and averaged 1–2 follow-up visits a year. Less than one-third of children in specialty mental health clinics received any stimulant medication, but all received psychosocial interventions averaging more than 5 visits per month. In both sectors, stimulant medication refill prescription persistence was poor (31%–49%). With few exceptions, ADHD diagnosis, impairment, academic achievement, parent distress, and parent-reported treatment satisfaction, perceived benefit, and improved family functioning did not differ between children who remained in care and those that received no care.
Conclusion
Areas for quality improvement are alignment of clinical severity with provider type, follow-up visits, stimulant use in specialty mental health, agency data infrastructure to document delivery of evidence-based psychosocial treatment, and stimulant medication refill prescription persistence.
Keywords: ADHD, quality of care, primary care, managed care, Medicaid
INTRODUCTION
Improving the quality of mental health care for publicly-insured children has been identified as a national priority in multiple reports 1–4 and health care reform legislation.5 The landmark Patient Protection and Affordable Care Act expands Medicaid eligibility to all who earn less than 133% of the federal poverty level and mandates that mental health services be included as basic services in Medicaid plans.6 The Children s Health Insurance Program Reauthorization Act of 2009 also adds $33 billion in federal funds to provide health insurance coverage to an estimated 4.1 million children in Medicaid and State Children s Health Insurance Program by 2013.7 Yet, if access to mental health services for children is increased under these new health policies, what is the quality of mental health care that children are anticipated to receive?
Within this context, the quality of care for Attention Deficit/Hyperactivity Disorder (ADHD) among children enrolled in Medicaid is significant because it is the most common childhood psychiatric disorder affecting 3–7% of U.S. children8–10 and more than one-third of the national healthcare expenditures for child mental disorders are paid for by Medicaid.11 During the past decade, ADHD medication prescriptions have doubled12, 13 and stimulant medication may be over-used.14 In California s Medicaid outpatient specialty mental health clinics, based on medical record data, medication treatment was found to be poorly monitored and slightly less than one-half of children received acceptable care for ADHD, depression and conduct disorder;15 rates similar to national estimates of quality of health care for children and adults.16, 17
In addition, care for ADHD is anticipated to increasingly occur in primary care settings as child mental health care is forecast to “constitute a significant part of general pediatric practice by 2020.”18 An estimated 6–42% of children are identified as having a mental health problem during a primary care visit,19–22 more than 70% of general pediatricians report being responsible for treating ADHD,23 and primary care clinician receptivity to adhering to evidence-based practices has improved.24 Nevertheless, studies based on provider survey data suggest that target areas for quality improvement include use of diagnostic criteria and rating scales, evidence-based behavior therapy, and more frequent follow-up care.25–27 For children enrolled in Medicaid, administrative barriers to the integration of mental health care in primary care settings include lack of diagnostic and procedural parity for Medicaid reimbursement and limitations on payments for same-day billing for physical and mental health services.28, 29
Within Medicaid, the quality of care in managed care is of relevance because enrollment of Medicaid beneficiaries has increased from 56% to 71% between 2000 to 2008,1 and unmet need for mental health services has been found to be higher among children enrolled in managed care compared to those in fee for service.30 In California, similar to several states, specialty mental health services are “carved-out” and Medicaid reimbursement requires that a child meet medical necessity criteria.31, 32 Evidence that use of specialty mental health services is reserved for the care of children with greater clinical severity however is mixed,25, 33, 34 but earlier studies did not hold insurance status constant. In managed care Medicaid programs with behavioral health carve-outs, comparison of clinical severity across care sectors is also problematic because Medicaid data is fragmented between primary care and specialty mental health agencies.35 Differences in clinical severity of ADHD across sectors have not been examined to explore whether the policy s intention to reserve specialty mental health services for children of greater clinical need is met. Further, little is known about the quality of ADHD care delivered in primary care clinics, how it compares to that provided in specialty mental health programs, and whether clinical outcomes differ by sector.
To address these questions, this study merges Medicaid data from primary care and specialty mental health care clinics and integrates child-level data from parent and child interviews as well as school records to describe ADHD care in one of the nation s largest managed care Medicaid programs.1 Clinical severity and unmet need for mental health services are described using standardized measures of symptoms and impairment. Across three 6-month time intervals, data on ADHD care processes and clinical outcomes by sector are aligned with the interview dates of the baseline, 6- and 12-month follow-up parent surveys. The study objectives are: 1) to examine whether clinical severity is greater among children receiving outpatient ADHD care in primary care compared to those in specialty mental health clinics; 2) to examine how broadly defined care processes (i.e., no care, unmet need, cross-sector contact, treatment type, stimulant medication refill prescription persistence, service use intensity) vary by sector; and 3) to explore how clinical outcomes compare between children who receive care in primary or specialty mental health clinics and those that receive no care, adjusting for potential selection effects. We hypothesize that children receiving ADHD care in outpatient specialty mental health settings will have greater clinical severity and thus will be more likely to receive combined treatment (i.e., psychosocial and medication) and more intensive services than children in primary care. The analysis examining how clinical outcomes vary by care sector is exploratory as there is little empirical data on ADHD care within a managed care Medicaid program.
METHOD
Study population
The study population was children aged 5–11 years who were identified by the agency as receiving any ADHD care in a large managed care Medicaid program in primary or specialty mental health care outpatient settings between January 1, 2003 and June 30, 2004. The health plan serves nearly 750,000 County of Los Angeles residents of all ages enrolled in managed care Medicaid, and specialty mental health services are carved-out to the County of Los Angeles Department of Mental Health (DMH).36
Sample
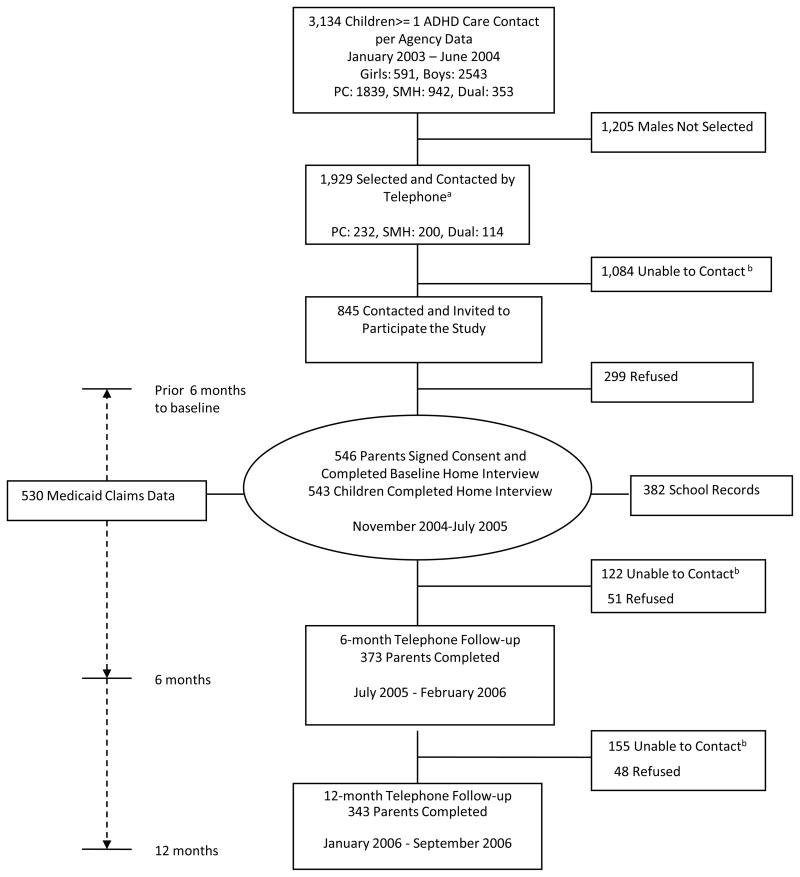
Medicaid service encounter and pharmacy claims data from the primary care and specialty mental health care agencies were used to construct the sampling frame and define the study time intervals (Figure 1). A child was identified as receiving ADHD care if he or she had at least one visit with a primary diagnosis of ADHD (ICD9: 314.00, 314.01 or 314.9) or at least one claim for a stimulant prescription during the sampling time period. The other eligibility criteria were age 5–11 years, primary language was Spanish or English, and Los Angeles County residence. For children identified from DMH, membership in the managed care Medicaid health plan was verified prior to entry into the sampling frame. We identified 3,134 children who were eligible for the study. We included all girls (n=591) and randomly selected boys (1338/2543; 53%), yielding 1,929 children who were eligible for enrollment. Of these children, 56% were not reachable and the most common reason was incorrect contact information (84%; 910/1084). Of the 845 parents or primary care givers contacted (here after referred to as parents), 546 (65%) participated in the home interviews and of these, almost all children (n=542, 99%) completed depression and anxiety screenings. Of the 546 parents enrolled, 530 children had Medicaid claims data available between January 2003 to December 2006. This analysis is based on these 530 children. Selection of boys, reachable status and participation varied by sector, therefore enrollment weights were created to adjust for the probability of selection, reachability, and non-response bias. Description of sampling procedure and enrollment weights is included in the supplemental materials (see Table S1, available online).
Figure 1.
Flowchart of Participants in the Partners in Care for Children Study
Note: Agency data available for constructing sampling frame: January 2003 – June 2004 in specialty mental health care (SMH); January 2003 – February 2004 in primary care (PC). Dual = one or more contact for ADHD or stimulant medication filled in both sectors.
aIncluded all females (n=591) and randomly selected males (n=1,338) stratified by care sector.
bParents could not be reached either due to problems with locator information (moved, disconnected telephones), or they never responded to telephone messages with 10 attempts during three different time periods of the day (i.e., morning, midday, early evening).
Parent and child home interviews were completed between November 2004 and July 2005, and follow-up parent telephone surveys were administered at approximately 6 and 12 months. The 6-month survey was conducted between July 2005 and February 2006 with a response rate of 68% (n=373), and the 12-month survey was conducted between January through September 2006 with a response rate of 63% (n=343). Seventy-seven percent (n=421) of children had parent-reported data from at least one follow-up survey, and 54% (n=295) of children had parent survey data at all three time points. On average, 6-month follow-up interviews were completed 7.2 months (SD, 1.4) and 12-month interviews were completed 13.4 months (SD, 1.3) from date of first parent interview. For each child, agency data were abstracted for three 6-month study time intervals. School record data were obtained for 70% of the children (N=382).
Procedures
Study and consent procedures were approved by the State of California Department of Health Care Services and UCLA Institutional Review Boards. Interviews were conducted in English or Spanish at home or convenient meeting place. Following the interview, parents were asked to authorize the release of school records. Parents received $50 and children were given a $5 gift certificate for their participation. The interview team included bilingual, bicultural interviewers with on average 7 years survey experience, including interviewing low-income children and their families. All interviewers received three days of training and were certified for data collection if they had at least 90% agreement on three standardized videotaped parent/child interviews. Survey responses were reviewed for accuracy within two weeks of the interview, and subjects were re-contacted by phone to correct any errors. School record data were abstracted using a computerized record abstraction tool developed for this study using FileMaker® database software.
Study Variables
Construction of the study variables to describe the clinical characteristics and care processes is summarized in the supplemental tables (see Table S2A and S2B, available online). To align the time frames for describing care processes and clinical outcomes over time, school record data and Medicaid claims data were aligned with the interview dates of the baseline, 6- and 12-month follow-up parent surveys. Agency data were used to construct three 6-month time intervals; namely, the time between the 6 months prior to the parent baseline interview to baseline interview, between the baseline and 6-month interview, and between 6-month and 12-month interview. For children whose parent did not complete a follow-up survey, an interview date was extrapolated based on the distribution of the interview dates.
Data Analysis
The sociodemographic and clinical characteristics assessed at baseline were described using means and standard deviations for continuous variables, and percentages for categorical variables. Each variable was cross-tabulated with the three care sector contact groups at sampling (i.e., the sector from which the child received ADHD care when determined to be eligible for the study), namely primary care, specialty mental health, and dual. Weighted estimates applicable to the population of eligible children were calculated using SUDAAN 10.0 software (http://www.rti.org/SUDAAN/) to account for sampling procedures and unit non-response. Distribution of sample characteristics by the follow-up survey response status at 6 and 12 months is included in the supplemental materials (see Table S3, available online). We performed non-response analyses for the 6- and 12-month surveys and developed weights that account for non-response bias. The products of the enrollment weights and non-response weights were used for follow-up analyses.
To compare the rates of no care and unmet need across initial care sectors (primary care, specialty mental health, dual) over 18 months, we estimated multiple logistic regression models. To account for confounding and the multi-level data structure with repeated measurements nested within children, we used a generalized estimating equations (GEE) method incorporated in SUDAAN to fit a longitudinal repeated measure logistic regression model using data at baseline, 6 months, and 12 months.37 In these models, we included main effects of care sector, wave, and their interaction, as well as main effects of child age, gender, race/ethnicity, primary language, type of ADHD care when selected (visit only, stimulant prescription filled, both). Significance of comparisons by care sector at each wave was based on regression coefficients. F-test is used to designate statistical significance of 0.05 or stronger for the overall test of the difference among the three care groups and t test is used for a comparison between two groups. To facilitate interpretation of the estimates, we present the predicted probabilities for each care group along with 95% confidence intervals.
Descriptive summaries are provided for service use patterns. Among children who received ADHD care at three 6-month intervals (T1: 6 months prior to the baseline interval, T2: baseline–6 month, T3: 6–12 months) the service use patterns were compared between primary and specialty mental health care. A small group of children who received ADHD care from both care sectors (18 from T1, 16 from T2, 9 from T3) were excluded to improve the homogeneity of the care sector groups. The chi-square test was used to test for differences among categorical variables, and t-test was used for continuous variables.
For clinical outcomes at three 6-month intervals (i.e., ADHD diagnosis, functional impairment, ≥ C average academic grade, parent poor mental health, positive parent treatment perception), the GEE method described above was used. To examine differences in clinical outcomes by care sector contact status (i.e., no care, primary care, specialty mental health), we fit longitudinal repeated measure logistic regression models with the covariates of child age, gender, race/ethnicity, parent marital status, and education.
For all logistic regression models, we assessed the sensitivity of the findings to adjustment for additional covariates (biologic parent) as well as in unweighted analyses. Findings using unweighted data that are adjusted for selected covariates were qualitatively similar to those based on weighted data.
RESULTS
Sociodemographic Characteristics
The average child age was 9.9 years (SD, 1.9), 68% were male (n=370), and most (n=474, 87%) were from minority racial or ethnic backgrounds. Nearly one quarter (n=125, 23%) were African-American, 54% (n=293) were Latino, 13% (n=72) were Caucasian, and 10% (n=56) were reported by their parents as being from two or more ethnic backgrounds or from other ethnic groups. Of the Latino children, 75% (208/277, 16 missing data) were in the family s first U.S. born generation. Forty percent (n=218) of the parents had less than 12 years of education, 34% (n=182) had graduated from high school, and 27% (n=144) had 13 or more years of education. Forty percent (n=216) were married, 26% (n=139) were widowed, separated or divorced, and 35% (n=191) had never been married. Only 11% of children (n=61) were living with a non-biologic parent and 4% (n=21) had a foster parent. One-quarter of the parents (n=141; 26%) screened positive for high psychological distress. Demographic characteristics did not vary by care sector in pair-wise comparisons, with few exceptions. Children living with a non-biologic or foster parent were more likely to be receiving care in specialty mental health clinics than in primary care (p<.017).
Clinical Characteristics
Slightly more than three-fourths of the children (n=411; 76%) met diagnostic criteria for ADHD in the past year, and the combined subtype was most common (n=264; 48%) followed by inattention type (n=97; 18%) and hyperactive/impulsivity type (n=50; 9%). Of those with ADHD, 63% (n=258) also met diagnostic criteria for a disruptive behavior disorder (ODD: n=254, 62%, CD: n=57, 14%) and 26% (n=106) screened positive for depression or anxiety. Overall, 82% (n=446) of the children had symptoms of at least one common childhood psychiatric disorder and of these, 45% (n=243) had high functional impairment. To conservatively estimate need for mental health services, 41% (n=220) met diagnostic criteria for ADHD and had high functional impairment, and 43% (n=234) had at least one common disorder and were impaired. One-half of the children received a grade of C or better in English (n=153; 50%) and 41% (n=128) received an average grade or higher in math during the most recently completed grading period. Almost 40% of children (n=214) had a history of being suspended (n=207; 38%) or expelled (n=42; 8%) from school.
Clinical severity and academic variables did not differ significantly between children who received ADHD care in solely primary and specialty mental health care at study entry. Children who had contacted both sectors for ADHD care at study entry had higher functional impairment than children who had initial contact in only one sector (p<.017), and compared to children served in only primary care, had a higher rate of being suspended (p<.017) (See Table S4, available online).
No Care, Unmet Need and Cross-Sector Contact over Time
Adjusted percentages of no care and unmet need for each 6-month study time interval by the initial care sector from which the child was sampled are summarized in Table 1. Slightly more than one-third of the children (34%) were receiving no care during the 6 months prior to the baseline home interview and 44% were receiving no care between the 6-and 12-month follow-up. For children that had contact for ADHD care in only primary care at sampling, 52% received no care at the 6–12 month time interval. Among the total sample, 13%–20% of children met criteria for past year ADHD diagnosis and high functional impairment and were receiving no care during the 6-month study time intervals. Applying a stricter definition of unmet need for mental health services, among children with ADHD and high functional impairment, 32%–37% were receiving no care during the 6-month study time intervals. At each 6-month interval, children who had contact for ADHD care in only primary care clinics at sampling were more likely to receive no care and have unmet need for mental health services than children who had contact in only specialty mental health care clinics or both care sectors at study entry.
TABLE 1.
Adjusted Percentage of Children who Receive No Care and Have Unmet Need during 18-Month Study Time Period by the Care Sector Contact at Sampling
| Analytic | Overall | PC | SMH | Dual | Difference across care sectors | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PC vs SMH | PC vs Dual | SMH vs Dual | Group test | ||||||||||
| N | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | t | p | t | p | t | p | χ2 | p | |
| No Care | |||||||||||||
| 6 months prior to baseline | 530 | 33.6 (28.9–38.2) | 41.3 (33.8–48.7) | 25.7 (20.0–31.5) | 15.7 (8.7–22.8) | 3.2 | <0.01 | 4.3 | <.001 | 1.9 | 0.06 | 22.6 | <.001 |
| Baseline – 6 months | 530 | 38.6 (33.8–43.4) | 48.0 (40.4–55.5) | 29.5 (23.4–35.5) | 15.2 (8.2–22.3) | 3.6 | <.001 | 5.3 | <.001 | 2.6 | <0.01 | 32.5 | <.001 |
| 6–12 months | 530 | 43.8 (38.9–48.7) | 51.9 (44.5–59.4) | 34.4 (28.0–40.8) | 27.2 (18.6–35.8) | 3.4 | <.001 | 4.0 | <.001 | 1.2 | 0.23 | 20.3 | <.001 |
| Unmet Need | |||||||||||||
| Any ADHD + Impairment + No Carea | |||||||||||||
| 6 months prior to baseline | 529 | 12.7 (9.3–16.1) | 16.1 (10.5–21.8) | 8.5 (4.9–12.0) | 8.1 (2.8–13.3) | 2.4 | 0.01 | 1.8 | 0.08 | 0.1 | 0.90 | 7.1 | 0.03 |
| Baseline – 6 months | 360 | 18.7 (12.8–24.5) | 25.9 (16.0–35.8) | 11.6 (6.9–16.3) | 5.7 (0.6–10.8) | 2.8 | 0.01 | 3.2 | <0.01 | 1.4 | 0.16 | 13.5 | <0.01 |
| 6–12 months | 334 | 20.3 (14.8–25.7) | 25.0 (16.2–33.9) | 14.3 (8.6–20.0) | 9.7 (0.7–18.8) | 2.1 | 0.03 | 1.9 | 0.06 | 0.8 | 0.45 | 6.2 | 0.04 |
| No Care among any ADHD + Impairmentb | |||||||||||||
| 6 months prior to baseline | 216 | 31.8 (24.5–39.1) | 43.9 (32.1–55.8) | 18.8 (11.0–26.6) | 16.0 (6.1–25.9) | 3.4 | <.001 | 3.3 | <0.01 | 0.4 | 0.68 | 16.7 | <.001 |
| Baseline – 6 months | 186 | 35.1 (25.7–44.4) | 50.6 (37.7–63.5) | 17.6 (10.3–25.0) | 12.9 (2.0–23.7) | 4.3 | <.001 | 3.7 | <.001 | 0.7 | 0.49 | 23.8 | <.001 |
| 6–12 months | 179 | 37.4 (28.7–46.2) | 50.1 (36.7–63.5) | 23.4 (13.6–33.2) | 18.3 (2.6–33.9) | 3.1 | <0.01 | 2.6 | 0.01 | 0.5 | 0.60 | 12.0 | <0.01 |
Note: Data are adjusted for child age, gender, race/ethnicity, primary language, type of Attention-Deficit/Hyperactivity Disorder (ADHD) care when selected (visit only, stimulant prescription filled, both), and sampling weights. For Unmet Need, nonresponse weighting was also used to extrapolate from the observed 6-month and 12-month sample to the enrolled sample. CI = confidence interval; Dual = one or more contact for ADHD or stimulant medication filled in both sectors; PC=primary care; SMH=specialty mental health care.
Any ADHD: 6 or more inattentive or hyperactive symptoms in past year; Impairment: Columbia Impairment Scale (CIS)>=15.
Analytic sample limited to those who had 6 or more inattentive or hyperactive symptoms in past year and CIS>=15.
Of the children that had initial contact in one care sector, none crossed over to the other at each 6-month time interval (see Table S5, available online). Of the 21% of children (110/530) that had contact with both care sectors at study entry, 65% transitioned to only specialty mental health care 6 months prior to baseline interview, and very few (6%) went back to receiving mental health services in only primary care. A very similar pattern persisted during the two follow-up time intervals.
ADHD Care in Primary and Specialty Mental Health Settings
Treatment type, stimulant medication refill prescription persistence, and service use intensity among children who remained in only primary care or specialty mental health clinics by 6-month time intervals are summarized in Table 2. Treatment type and service use intensity differed strikingly by sector. Only 39% of children receiving mental health services in primary care clinics had a visit for any psychiatric diagnosis during the 6 months prior to the baseline home interview, and mental health visits declined to 28% at the 6–12 month time interval. For each time interval, the majority of children receiving mental health services in primary care had at least one psychotropic medication prescription filled (95%, 98%, 96% at 3 time intervals respectively) and about two-thirds of children (61%, 68%, 72% at 3 time intervals respectively) received only medication treatment. The rates of stimulant medication treatment in primary care clinics was consistently at least 2.8 times greater than that found in specialty mental health programs over three time intervals. During each time interval, most children in primary care clinics (85%, 85%, 80% at 3 time intervals respectively) were significantly more likely to have at least one stimulant medication prescription filled compared to less than one third (30%, 29%, 28% at 3 time intervals respectively) of children in specialty mental health programs. However, stimulant medication refill prescription persistence was poor in both sectors, ranging from 33%–44% in primary care and 31%–49% in specialty mental health care.
TABLE 2.
Treatment Type, Stimulant Medication Refill Persistence, and Service Use Intensity among Children who Receive Care from Only Primary Care (PC) or Specialty Mental Health (SMH)
| 6 months prior to baseline | Baseline – 6 months | 6 – 12 months | ||||
|---|---|---|---|---|---|---|
| PC (N=139) | SMH (N=206) | PC (N=127) | SMH (N=197) | PC (N=124) | SMH (N=178) | |
| Any Psychosocial | ||||||
| Any mental health visit, % | 39.1 | 100 | 31.8 | 100 | 28.0 | 100 |
| Any Medication | ||||||
| Any psychotropic medication, % | 95.2 | 40.1*** | 97.6 | 39.9*** | 95.5 | 35.0*** |
| Only psychotropic medication, % | 60.9 | 0.0*** | 68.2 | 0.0*** | 72.0 | 0.0*** |
| Any stimulant medication, % | 85.1 | 30.3*** | 85.2 | 29.3*** | 79.8 | 28.2*** |
| Only stimulant medication, % | 61.1 | 21.3*** | 63.4 | 18.1*** | 54.0 | 17.3*** |
| Stimulant medication + other psychotropic medication, % | 24.0 | 9.1** | 21.8 | 11.2* | 25.9 | 11.0** |
| Only other psychotropic medication, % | 10.1 | 9.8 | 12.4 | 10.6 | 15.7 | 6.8* |
| Stimulant medication refill persistencea, % | 35.9 | 31.3 | 40.8 | 39.9 | 48.6 | 49.2 |
| Combined | ||||||
| Mental health visit + psychotropic medication, % | 34.3 | 40.1 | 29.4 | 39.9 | 23.5 | 35.0* |
| Service Use Intensity | ||||||
| Average no. of visits per month, mean (SD) | 0.2±0.7 | 5.3±5.9*** | 0.2±0.4 | 5.6±6.0*** | 0.1±0.5 | 5.2±5.7*** |
Note: Data are presented as n (%) unless otherwise indicated. Data are limited to children who had service contact from primary care or specialty mental health care. Chi-square tests were used for the comparisons of PC vs. SMH (see p values below).
Stimulant medication available for more than 67% of total day supply. Sample sizes for PC at 3 time intervals are 113, 105, 96 and 67, 62, 51 for SMH respectively.
p<.05,
p<.01,
p<.001.
In addition, about one quarter of the children receiving mental health services in primary care clinics had at least one prescription filled for a stimulant medication and another class of psychotropic medication. Combined psychotropic medication treatment was more likely among children receiving mental health services in primary care than specialty mental health clinics during each time interval. Rates of combined psychotropic medication prescriptions among children with ADHD and comorbid ODD or CD were also similar to those among the larger sample of children receiving any care in primary care or specialty mental health clinics (see Table S6, available on line).
Between 26%–43% of children received medication and psychosocial treatment at each time interval, and receipt of combined treatment did not vary by care sector. In contrast, service use intensity varied widely between primary care and specialty mental health clinics. On average, children in primary care had only 1–2 mental health visits per year compared to an average of 5 visits per month among children receiving care in specialty mental health clinics. Among children receiving care in specialty mental health, over 90% received supportive services and more than three-quarters received psychotherapy at each 6-month time interval (See Table S7, available online). Only 29%–34% of children had at least one visit for psychotherapy and at least one psychotropic medication prescription filled for each time interval. The average number of contacts per month for supportive services ranged from 1.8–2.3, and average number of visits per month for psychotherapy ranged from 2.3–2.7.
Clinical Outcomes
Clinical outcomes among children who received no care and those who remained in care are summarized in Table 3. With a few exceptions at specific time intervals, clinical outcomes did not vary between children receiving and not receiving ADHD care or between those in primary care or specialty mental health clinics. Compared to children receiving no care, children in specialty mental health clinics were more likely to have high functional impairment at 6- and 12-month follow-up. Twenty-four percent of parents had high psychological distress at baseline, and the proportion of parents with high distress did not vary by whether their child was receiving care or not. Despite little evidence of clinical improvement, most parents had very positive perceptions of treatment that remained stable over time regardless of treatment status. At baseline, 75% of parents were satisfied or very satisfied with treatment, 86% reported tremendous or some treatment benefit and 83% reported improved family relationships.
TABLE 3.
Clinical Outcomes among Children who Receive No Care or Remain in Care during 18-Month Study Time Perioda
| Analytic | Overall | No Care | PC | SMH | Difference across care sectors | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No Care vs PC | No Care vs SMH | PC vs SMH | Group test | ||||||||||
| N | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | t | p | t | p | t | p | χ2 | p | |
| Child | |||||||||||||
| Any ADHD | |||||||||||||
| Baseline | 512 | 76.8 (72.7–80.9) | 77.8 (70.7–84.9) | 75.1 (66.7–83.5) | 77.4 (72.3–82.6) | 0.5 | 0.63 | 0.1 | 0.93 | −0.5 | 0.64 | 0.3 | 0.87 |
| 6-month follow-up | 349 | 72.6 (67.6–77.7) | 75.6 (67.1–84.1) | 68.7 (57.5–79.8) | 70.8 (63.4–78.2) | 1.0 | 0.33 | 0.8 | 0.41 | −0.3 | 0.75 | 1.1 | 0.58 |
| 12-month follow-up | 328 | 69.5 (63.7–75.3) | 65.1 (55.6–74.6) | 70.0 (57.9–82.2) | 78.7 (71.5–85.8) | −0.6 | 0.54 | −2.3 | 0.02 | −1.3 | 0.21 | 5.3 | 0.07 |
| Impairment | |||||||||||||
| Baseline | 511 | 43.5 (38.7–48.2) | 41.3 (32.2–50.4) | 41.4 (32.1–50.7) | 48.0 (41.7–54.3) | −0.0 | 0.99 | −1.2 | 0.24 | −1.1 | 0.25 | 2.0 | 0.36 |
| 6-month follow-up | 348 | 61.6 (55.9–67.3) | 50.6 (39.4–61.9) | 66.5 (55.5–77.5) | 67.5 (60.0–75.1) | −2.0 | 0.05 | −2.4 | 0.01 | −0.2 | 0.88 | 6.6 | 0.04 |
| 12-month follow-up | 328 | 59.8 (53.7–66.0) | 51.5 (41.2–61.8) | 61.8 (49.0–74.6) | 72.7 (64.5–80.9) | −1.2 | 0.22 | −3.0 | <0.01 | −1.4 | 0.15 | 9.3 | 0.01 |
| Any ADHD + Impairment | |||||||||||||
| Baseline | 511 | 40.0 (35.3–44.8) | 38.6 (29.6–47.6) | 37.8 (28.7–46.9) | 43.8 (37.4–50.1) | 0.1 | 0.91 | −0.9 | 0.36 | −1.0 | 0.30 | 1.5 | 0.48 |
| 6-month follow-up | 348 | 53.9 (47.9–59.8) | 48.9 (37.6–60.2) | 54.1 (41.9–66.4) | 56.9 (48.9–64.9) | −0.6 | 0.54 | −1.1 | 0.26 | −0.4 | 0.71 | 1.3 | 0.52 |
| 12-month follow-up | 328 | 54.4 (48.1–60.6) | 47.7 (37.3–58.2) | 54.3 (40.6–67.9) | 66.9 (58.3–75.5) | −0.7 | 0.46 | −2.7 | 0.01 | −1.5 | 0.12 | 7.4 | 0.02 |
| English C equivalent grade or better | |||||||||||||
| Baseline | 293 | 51.1 (44.6–57.6) | 54.0 (43.3–64.8) | 49.8 (36.8–62.8) | 48.5 (39.7–57.3) | 0.5 | 0.61 | 0.8 | 0.43 | 0.2 | 0.87 | 0.7 | 0.72 |
| 6-month follow-up | 262 | 49.0 (40.6–57.4) | 47.9 (34.5–61.2) | 53.7 (35.5–71.9) | 44.2 (31.0–57.3) | −0.5 | 0.60 | 0.4 | 0.70 | 0.8 | 0.40 | 0.7 | 0.70 |
| 12-month follow-up | 211 | 46.6 (36.9–56.3) | 42.2 (27.5–56.9) | 51.7 (31.2–72.3) | 55.0 (39.8–70.1) | −0.8 | 0.44 | −1.2 | 0.24 | −0.2 | 0.80 | 1.5 | 0.47 |
| Math C equivalent grade or better | |||||||||||||
| Baseline | 298 | 44.1 (37.7–50.6) | 38.7 (27.4–49.9) | 56.2 (43.6–68.8) | 36.8 (28.3–45.3) | −2.0 | 0.04 | 0.3 | 0.79 | 2.5 | 0.01 | 6.7 | 0.04 |
| 6-month follow-up | 265 | 42.7 (34.5–50.9) | 40.7 (27.3–54.2) | 52.8 (36.1–69.5) | 40.2 (27.7–52.7) | −1.1 | 0.26 | 0.1 | 0.95 | 1.2 | 0.23 | 1.7 | 0.43 |
| 12-month follow-up | 216 | 51.1 (41.5–60.7) | 41.1 (26.3–55.9) | 62.1 (44.1–80.0) | 55.5 (40.4–70.6) | −1.7 | 0.08 | −1.4 | 0.18 | 0.6 | 0.58 | 3.4 | 0.18 |
| Parent/Care giver | |||||||||||||
| Parent distress (MHI-5<56) | |||||||||||||
| Baseline | 512 | 23.7 (19.8–27.5) | 25.5 (17.7–33.2) | 19.1 (12.2–25.9) | 28.6 (22.9–34.3) | 1.3 | 0.21 | −0.6 | 0.53 | −2.1 | 0.04 | 4.2 | 0.12 |
| 6-month follow-up | 347 | 18.1 (13.8–22.4) | 14.1 (7.6–20.6) | 19.7 (10.8–28.7) | 21.4 (14.5–28.4) | −1.0 | 0.30 | −1.5 | 0.14 | −0.3 | 0.76 | 2.3 | 0.32 |
| 12-month follow-up | 325 | 19.2 (14.1–24.3) | 17.3 (9.1–25.5) | 20.4 (10.3–30.4) | 18.8 (11.2–26.3) | −0.5 | 0.64 | −0.3 | 0.79 | 0.3 | 0.80 | 0.2 | 0.89 |
| Treatment perceptionb | |||||||||||||
| Satisfaction (very satisfied/satisfied) | |||||||||||||
| Baseline | 223 | 74.3 (67.6–81.0) | 72.7 (62.2–83.2) | 77.3 (70.2–84.5) | −0.7 | 0.46 | |||||||
| 6-month follow-up | 167 | 76.0 (68.9–83.2) | 66.4 (50.8–81.9) | 82.7 (75.4–89.9) | −2.0 | 0.05 | |||||||
| 12-month follow-up | 138 | 76.6 (68.3–84.9) | 76.1 (62.9–89.4) | 78.0 (68.8–87.2) | −0.2 | 0.81 | |||||||
| Perceived benefit of treatment | |||||||||||||
| Baseline | 222 | 85.7 (80.3–91.0) | 84.9 (76.6–93.2) | 87.9 (82.2–93.6) | −0.6 | 0.55 | |||||||
| 6-month follow-up | 164 | 72.9 (65.5–80.3) | 66.2 (50.6–81.8) | 77.5 (69.4–85.5) | −1.4 | 0.17 | |||||||
| 12-month follow-up | 139 | 75.3 (67.1–83.6) | 73.2 (60.3–86.0) | 79.2 (69.0–89.5) | −0.7 | 0.46 | |||||||
| Family relationships improved | |||||||||||||
| Baseline | 210 | 82.4 (76.3–88.5) | 80.1 (70.4–89.9) | 85.8 (80.1–91.4) | −1.0 | 0.30 | |||||||
| 6-month follow-up | 162 | 79.6 (72.8–86.4) | 79.2 (65.5–92.8) | 82.2 (74.3–90.0) | −0.4 | 0.70 | |||||||
| 12-month follow-up | 137 | 78.9 (70.8–86.9) | 79.2 (66.5–91.8) | 77.1 (67.0–87.1) | 0.3 | 0.79 | |||||||
Note: Data are limited to children whose administrative data showed “no care”, “PC only” (primary care), “SMH” (specialty mental health care) from the 6 months prior to the baseline parent interview date to the 12 months follow-up. Any Attention-Deficit/Hyperactivity Disorder (ADHD): 6 or more inattentive or hyperactive symptoms in past year; Impairment: Columbia Impairment Scale (CIS)>=15. MHI = Mental Health Inventory
Data are adjusted for child age, gender, race/ethnicity, parent marital status, education level, and sampling weights. Non-response weighting was also used to extrapolate from the observed 6-month and 12-month sample to the enrolled sample.
Data are limited to children who had service contact from PC or SMH.
DISCUSSION
Care for childhood ADHD in the managed care Medicaid program studied failed to meet the Institute of Medicine s definition of quality that requires “consistency with current professional knowledge” and “improved likelihood of desired health outcomes”.2 More than one-third of children were receiving no care when interviewed at baseline, a rate double the national rate for adults.38 Despite similar clinical severity, treatment approaches for children were strikingly different in primary care and specialty mental health clinics. Children in primary care received predominantly medication treatment, as recommended by treatment guidelines,8, 39, 40 at rates that exceed earlier estimates in community-based primary care.27 Follow-up visits however were on average roughly once per year, a rate similar to that found in other primary care settings.25 The low follow-up visit rate falls short of the National Quality Forum-endorsed standards41 and substantially below nationally recommended psychotropic medication treatment and monitoring.42 In contrast, almost all children in specialty mental health clinics received psychosocial interventions, averaging about five visits per month, and less than one-third of children had at least one stimulant medication prescription filled, a rate consistent with other community-based samples.43, 44 In both sectors, documentation of evidence-based psychosocial treatment for ADHD (i.e., behavior therapy) was missing in the agency databases, and stimulant medication refill prescription persistence was poor but also at rates similar to other community-based populations.43, 45 Despite substantial differences in treatment and service use intensity, children remained symptomatic over time whether or not they were in care, with few exceptions.
Contrary to our hypothesis, children with greater clinical severity were not more likely to access specialty mental health care. There was also little evidence of cross-care sector contact over time. In this large county-wide program, prior authorization from the primary care provider (i.e., “gatekeeper”) is not required to access Medicaid-funded specialty mental health services. Parents may also directly access specialty mental health services which are supported by a patchwork of Medicaid-funded and state legislated programs. Further, there is little infrastructure or incentives to support the transfer of children stabilized in mental health clinics back to primary care or more clinically complex children from primary care to specialty mental health clinics. Together, these findings raise questions about whether the policy that requires medical necessity for Medicaid reimbursement is sufficient to reserve specialty mental health resources for those with greater need. In addition, these findings support future research to develop quality improvement interventions, which are ideally compatible with health information technologies, which promote alignment of the child s clinical severity with provider type as well as improved coordination of care across primary and specialty mental health care providers.
The striking differences in treatment approaches may reflect variation in provider training or clinic workflow. In community-based specialty mental health programs, clinic workflow does not usually follow the medical model found in primary care clinics. Children in specialty mental health clinics may be more likely to have a trial of psychosocial treatment because access to therapists is greater.2 During this study s time period, at the county agency level there was no implementation of treatment protocols that specify a trial of behavior therapy prior to medication evaluation (personal communication, W. Arroyo, June, 14, 2010). Low stimulant medication treatment rates in specialty mental health clinics may occur because access to the physician is often restricted to children identified by non-medically trained professionals as meriting a medication evaluation.28 Nevertheless, differences in provider training do not explain the greater use of combined psychotropic medication in primary care, and is consistent with pediatrician opinion that psychopharmacology is a priority area for continued medical education.22 In future research, comparisons of ADHD care across providers in primary care and specialty mental health care settings should consider adding a study arm for children served in specialty mental health clinics in which the intake evaluation is conducted by a child psychiatrist followed by referral to a therapist to examine whether detection of ADHD, adherence to evidence-based practices, clinical outcomes, and cost-savings over time is improved compared to usual care in specialty mental health programs.
Although linking of child-level data with Medicaid data is a “powerful and under-used resource for health services research,”35 this study s findings also underscore the need for improved Medicaid data infrastructure to assess and monitor even broad indices of quality of care for children with ADHD.5 A substantial proportion of children had poor contact information in their Medicaid data, suggesting that these data have limited capacity to be used by agencies for quality improvement interventions, such as parent education or prevention programs. The use of recommended behavior therapy, like parent training, may be underestimated in both sectors because procedure codes for Medicaid service encounter data do not specify use of evidence-based psychosocial treatments. Mental health visits in primary care may be under-reported because of lack of procedural parity in Medicaid reimbursement for mental health services delivered in primary care.28, 29 Additionally, within specialty mental health clinics, similar procedure codes for psychosocial interventions may be billed for by therapists from a variety of disciplines, making it problematic to examine how quality of care varies by provider type. Further, there is no single standard for measuring prescription refill persistence using Medicaid pharmacy claims data.35 The cut-point for acceptable stimulant medication availability, which accounts for possible drug holidays on weekends, was developed for this study. This approach may overestimate medication refill persistence because some children may receive treatment with two stimulant medications daily or underestimate it because the gap between prescriptions filled for each specific type of stimulant medication was not measured.46 Future data analyses will examine the agreement between parent-reported care processes and medication adherence with Medicaid data, and explore predictors of agreement in service use and medication treatment.
Of note, conclusions about the effectiveness of treatment cannot be made because children were not randomized to treatment groups. Unlike the Multimodal Treatment Study of Children with ADHD that included a community care arm,47 this is an observational study for which a natural comparison group emerged over time. High functional impairment among children who remained in specialty mental health clinics compared to children receiving no care is consistent with prior studies that suggest clinical need drives service use.15 Some clinical outcomes may also have been missed because it was beyond the scope of this study s design and budget to conduct follow-up home interviews for this relatively large community-based population of children and administer a more comprehensive battery of clinical measures. Further, the consistently high rate of positive treatment perceptions by parents may not necessarily be incongruent with poor clinical outcomes, as these are not indicators of good technical care48 and have been found only minimally associated with youth-reported improvement in functioning.49
This study has several additional limitations. More than one-half (56%) of the children eligible for enrollment into the study could not be contacted by telephone, and weighting adjustment for selection and non-response does not include unmeasured variables that could also contribute to selection bias. Thus, even weighted data may not be representative of children that met eligibility criteria within the managed care Medicaid program for the study time period. Unmet need for mental health services may be underestimated because impairment due to ADHD symptoms was required for the diagnosis50 as well as global impairment,51 and duration of symptoms was not included in the operational definition of clinical severity. Using only past year ADHD diagnosis as the indicator of mental health service need, 26–28% of children had unmet need during the three 6 month-time intervals. Unmet need also may be overestimated if asymptomatic patients included those that were successfully treated, but this is less likely because stimulant medication refill prescription persistence was poor. Conclusions about medication treatment appropriateness cannot be made because some disorders for which psychotropic medication treatment may be clinically indicated was not assessed. Initial and maintenance phases of treatment also cannot be defined to assess adherence to most national quality indicators for ADHD because children did not enter the study when starting a new episode of care. Further, findings are not generalizable to children in other managed care Medicaid programs or other states because administrative approaches of mental health services by state Medicaid agencies widely varies.32, 52
Nevertheless, this is the first quality of care study for childhood ADHD in a large managed care Medicaid program that combines four data sources and examines how care processes and clinical outcomes compare across primary care and specialty mental health clinics over time. Findings from this study identify several areas for quality improvement for ADHD care within the managed care Medicaid program studied. These areas are alignment of the child s clinical severity with provider type, frequency of follow-up visits, stimulant medication use in specialty mental health, agency data infrastructure to document delivery of evidence-based psychosocial treatments, and stimulant medication refill prescription persistence. The enduring symptoms, impairment, and poor academic achievement of the children who remain in care and those untreated underscores the public health significance of improving the quality of care for publicly-insured children with ADHD. As advocacy for diagnostic and procedural parity in Medicaid reimbursement for mental health services across primary and specialty mental health care sectors continues, may there also be public investment in improving the quality of care delivered in both care sectors.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Medicare and Medicaid Services. Managed Care Trends. [Accessed 12/17/09];Medicaid Managed Care Enrollment Report. http://www.cms.hhs.gov/MedicaidDataSourcesGenInfo/downloads/08Trends508.pdf.
- 2.Institute of Medicine, Committee on Quality of Health Care in America. Crossing the Quality Chasm: a New Health System for the 21st Century. Washington D.C: The National Academies Press; 2001. [Google Scholar]
- 3.U.S. Department of Health and Human Services. New Freedom Commission on Mental Health: Achieving the Promise: Transforming Mental Health Care in America. Final Report. Rockville, MD: Department of Health and Human Services; 2003. SMA-03-3832. [Google Scholar]
- 4.U.S. Public Health Service. Mental Health: A Report of the Surgeon General. Rockville, MD: Department of Health and Human Services; 1999. [Google Scholar]
- 5.PL 111–113 Children’s Health Insurance Program Reauthorization Act,.
- 6.PL 111–148 [HR 3590] Patient Protection and Affordable Care Act,. ( ).
- 7.Kaiser Commission of Medicaid and the Uninsured. Children’s Health Insurance Program Reauthorization Act of 2009 (CHIPRA) [Accessed 6/10/10]; www.kff.org.
- 8.American Academy of Child and Adolescent Psychiatry Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(7):894–921. doi: 10.1097/chi.0b013e318054e724. [DOI] [PubMed] [Google Scholar]
- 9.Goldman LS, Genel M, Bezman RJ, Slanetz PJ. Diagnosis and treatment of attention-deficit/hyperactivity disorder in children and adolescents. JAMA. 1998;279:1100–1107. doi: 10.1001/jama.279.14.1100. [DOI] [PubMed] [Google Scholar]
- 10.Wolraich ML, Hannah JN, Pinnock TY, Baumgaertel A, Brown JD. Comparison of diagnostic criteria for attention-deficit hyperactivity disorder in a county-wide sample. J Am Acad Child Adolesc Psychiatry. 1996;35(3):319–333. doi: 10.1097/00004583-199603000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Soni A. The Five Most Costly Children’s Conditions 2006: Estimates for the U.S. Civilian Noninstitutionalized Children Ages 0-17. Rockville, MD: DHHS; 2009. Statistical Brief #242. [Google Scholar]
- 12.Guevara J, Lozano P, Wickizer T, Mell L, Gephart H. Psychotropic medication use in a population of children who have Attention-Deficit/Hyperactivity Disorder. Pediatrics. 2002;109:733–739. doi: 10.1542/peds.109.5.733. [DOI] [PubMed] [Google Scholar]
- 13.Winterstein A, Gerhard T, Shuster J, et al. Utilization of pharmacologic treatment in youths with attention deficit/hyperactivity disorder in Medicaid database. Ann Pharmacother. 2008;42(1):24–31. doi: 10.1345/aph.1K143. [DOI] [PubMed] [Google Scholar]
- 14.Olfson M, Gameroff MJ, Marcus SC, Jensen PS. National trends in the treatment of attention deficit hyperactivity disorder. Am J Psychiatry. 2003;160(6):1071–1077. doi: 10.1176/appi.ajp.160.6.1071. [DOI] [PubMed] [Google Scholar]
- 15.Zima BT, Hurlburt MS, Knapp P, et al. Quality of publicly-funded outpatient specialty mental health care for common childhood psychiatric disorders in California. J Am Acad Child Adolesc Psychiatry. 2005;44(2):130–144. doi: 10.1097/00004583-200502000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Mangione-Smith R, DeCristofaro AH, Setodji CM, et al. The quality of ambulatory care delivered to children in the United States. N Engl J Med. 2007;357(15):1515–1523. doi: 10.1056/NEJMsa064637. [DOI] [PubMed] [Google Scholar]
- 17.McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 18.Foy JM American Academy of Pediatrics Task Force on Mental Health. Introduction: Enhancing Pediatric Mental Health Care. Pediatrics. 2010;125:S69–S74. doi: 10.1542/peds.2010-0788C. [DOI] [PubMed] [Google Scholar]
- 19.Briggs-Gowan MJ, Owens PL, Schwab-Stone ME, Leventhal JM, Leaf PJ, Horwitz SM. Persistence of psychiatric disorder in pediatric settings. J Am Acad Child Adolesc Psychiatry. 2003;42(11):1360–1369. doi: 10.1097/01.CHI.0000084834.67701.8a. [DOI] [PubMed] [Google Scholar]
- 20.Brown JD, Riley AW, Wissow LS. Identification of youth psychosocial problems during pediatric primary care visits. Adm Policy Ment Health. 2007;34(3):269–281. doi: 10.1007/s10488-006-0106-7. [DOI] [PubMed] [Google Scholar]
- 21.Cooper S, Valleley RJ, Polaha J, Begeny JH, Evans JH. Running out of time: physician management of behavioral health concerns in rural pediatric primary care. Pediatrics. 2006;118(1):132–138. doi: 10.1542/peds.2005-2612. [DOI] [PubMed] [Google Scholar]
- 22.Williams J, Klinepeter K, Palmes G, Pulley A, Foy JM. Diagnosis and treatment of behavioral health disorders in pediatric practice. Pediatrics. 2004;114(3):601–606. doi: 10.1542/peds.2004-0090. [DOI] [PubMed] [Google Scholar]
- 23.Stein RE, Horwitz SM, Storfer-Isser A, et al. Attention-deficit/hyperactivity disorder: how much responsibility are pediatricians taking? Pediatrics. 2009;123(1):248–255. doi: 10.1542/peds.2007-3198. [DOI] [PubMed] [Google Scholar]
- 24.Wolraich M, Bard D, Stein M, Rushton J, O’Connor K. Pediatricians attitudes and practices on ADHD before and after the development of ADHD pediatric practice guidelines. J Atten Disord. 2009 August 25; doi: 10.1177/1087054709344194. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 25.Gardner WP, Kelleher KJ, Pajer KA, Campo JV. Follow-up care of children identified with ADHD by primary care clinicians: A prospective cohort study. J Pediatr. 2004;145(6):767–771. doi: 10.1016/j.jpeds.2004.08.028. [DOI] [PubMed] [Google Scholar]
- 26.Hoagwood K, Jensen PS, Feil M, Vitiello B, Bhatara VS. Medication management of stimulants in pediatric practice settings: a national perspective. J Dev Behav Pediatr. 2000;21(5):322–331. doi: 10.1097/00004703-200010000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Rushton JL, Fant KE, Clark SJ. Use of practice guidelines in the primary care of children with attention-deficit/hyperactivity disorder. Pediatrics. 2004;114(1):23–28. doi: 10.1542/peds.114.1.e23. [DOI] [PubMed] [Google Scholar]
- 28.American Academy of Child and Adolescent Psychiatry Committee on Health Care Access and Economics and the American Academy of Pediatrics Task Force on Mental Health. Improving mental health services in primary care: reducing administrative and financial barriers to access and collaboration. Pediatrics. 2009;123(4):1248–1251. doi: 10.1542/peds.2009-0048. [DOI] [PubMed] [Google Scholar]
- 29.Kautz C, Mauch D, Smith SA. Reimbursement of Mental Health Services in Primary Care Settings. Rockville, MD: DHHS, Center for Mental Health Services, Substance Abuse adn Mental Health Services Administration; 2008. SMA-08-4324. [Google Scholar]
- 30.Tang M, Hill K, Boudreau A, Yucel R, Perrin J, Kuhlthau K. Medicaid managed care and the unmet need for mental health care among children with special health care needs. Health Serv Res. 2008;43(3):882–900. doi: 10.1111/j.1475-6773.2007.00811.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.California Administration Code title 9 §1830.205.
- 32.US Department of Health and Human Services, Health Resources and Services Administration. Behavioral Health-2001 HSRA Partial Update to State by State Profiles: Medicaid Funded, Public Sector. Managed Behavioral Health Care Payers; [Google Scholar]
- 33.Busch B, Biederman J, Cohen LG, et al. Correlates of ADHD among children in pediatric and psychiatric clinics. Psychiatr Serv. 2002;53(9):1103–1111. doi: 10.1176/appi.ps.53.9.1103. [DOI] [PubMed] [Google Scholar]
- 34.Guevara JP, Rothbard A, Shera D, et al. Correlates of behavioral care management strategies used by primary care pediatric providers. Ambul Pediatrics. 2007;7(2):160–166. doi: 10.1016/j.ambp.2006.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Crystal S, Akincigil A, Biler S, Walkup JT. Studying prescription drug use and outcomes wtih Medicaid claims data: strengths, limitations, and strategies. Med Care. 2007;45:S58–S65. doi: 10.1097/MLR.0b013e31805371bf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.LA Health Care Plan. [Accessed August 24, 2009];Mission, vision & values. http://www.lacare.org/aboutlascare.
- 37.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometric. 1986;42:121–130. [PubMed] [Google Scholar]
- 38.Olfson M, Mojtabai R, Sampson NA, et al. Dropout from outpatient mental health care in the United States. Psychiatr Serv. 2009;60:898–907. doi: 10.1176/appi.ps.60.7.898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.American Academy of Pediatrics Subcommittee on Attention Deficit/Hyperactivity Disorder and Committee on Quality Improvement. Clinical practice guideline: diagnosis and evaluation of the child with attention-deficit/hyperactivity disorder. Pediatrics. 2000;105(5):1158–1170. doi: 10.1542/peds.105.5.1158. [DOI] [PubMed] [Google Scholar]
- 40.American Academy of Pediatrics Subcommittee on Attention Deficit/Hyperactivity Disorder and Committee on Quality Improvement. Clinical practice guideline: treatment of the school-age child with attention-deficit/hyperactivity disorder. Pediatrics. 2001;108(4):1033–1044. doi: 10.1542/peds.108.4.1033. [DOI] [PubMed] [Google Scholar]
- 41.National Quality Forum. National Quality Forum issue brief: strengthening pediatric quality measurement and reporting. J Healthc Qual. 2008;30(3):51–55. doi: 10.1111/j.1945-1474.2008.tb01143.x. [DOI] [PubMed] [Google Scholar]
- 42.Walkup J Work Group on Quality Issues. Practice parameters on the use of psychotropic medication in children and adolesecents. J Am Acad Child Adolesc Psychiatry. 2009;48:961–973. doi: 10.1097/CHI.0b013e3181ae0a08. [DOI] [PubMed] [Google Scholar]
- 43.Bussing R, Zima B, Mason D, Hou W, Garvan CW, Forness S. Use and persistence of pharmacotherapy for elementary school children with attention-deficit hyperactivity disorder. J Child Adolesc Psychopharmacol. 2005;15(1):78–87. doi: 10.1089/cap.2005.15.78. [DOI] [PubMed] [Google Scholar]
- 44.Leslie LK, Canino G, Landsverk J, et al. ADHD Treatment patterns of youth served in public sectors in San Diego and Puerto Rico. J Emot Behav Disord. 2005;13(4):224–236. [Google Scholar]
- 45.Charach A, Ickowicz A, Schachar R. Stimulant treatment over five years: adherence, effectiveness, and adverse effects. J Am Acad Child Adolesc Psychiatry. 2004;43(5):559–567. doi: 10.1097/00004583-200405000-00009. [DOI] [PubMed] [Google Scholar]
- 46.Rizzo JA, Simons WR. Variations in compliance among hypertensive patients by drug class: implications for health care costs. Clin Ther. 1997;19(6):1446–1457. doi: 10.1016/s0149-2918(97)80018-5. [DOI] [PubMed] [Google Scholar]
- 47.The MTA Cooperative Group. A 14-month randomized clinical trial of treatment strategies for attention deficit/hyperactivity disorder. Arch Gen Psychiatry. 1999;56:1073–1086. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- 48.Donabedian A. The Definition of Quality and Approaches to Its Assessment. Vol. 1. Ann Harbor, MI: Health Administration Press; 1980. [Google Scholar]
- 49.Garland AF, Aarons GA, Hawley KM, Hough RL. Relationship of youth satisfaction with mental health services and changes in symptoms and functioning. Psychiatr Serv. 2003;54(11):1544–1546. doi: 10.1176/appi.ps.54.11.1544. [DOI] [PubMed] [Google Scholar]
- 50.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39(1):28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 51.Bird HR, Shaffer D, Fisher P, et al. The Columbia Impairment Scale (CIS): pilot findings on a measure of global impairment for children and adolescents. Int J Methods Psychiatr Res. 1993;3(3):167–176. [Google Scholar]
- 52.Verdier J, Barrett A, Davis S. Administration of Mental Health Services by Medicaid Agencies. Rockville, MD: DHHS, Center for Mental Health Services, Substance Abuse and Mental Health Services Administration; 2007. (SMA) 07-4301. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.