Abstract
Background
Cam-type femoroacetabular impingement is secondary to lack of concavity at the anterosuperior femoral head-neck junction, resulting in reduced femoral head-neck offset and femoral head asphericity. This morphologic deformity can be detected by MRI and plain radiographs and quantified using the alpha angle.
Questions/purposes
We evaluated the accuracy and reproducibility of plain radiography in the diagnosis of cam-type deformity.
Methods
Sixty-eight patients (37 females, 31 males) with a mean age of 38 years (range, 17–60 years) were treated for intraarticular hip pathology with 43 hips having cam-type femoroacetabular impingement and 25 having isolated labral tears. All patients had alpha angle measurements made on plain radiographs (AP pelvis, crosstable lateral, Dunn view) and multiplanar MRI using an alpha angle of more than 50.5° as the gold standard.
Results
The Dunn view had a sensitivity of 91%, specificity of 88%, positive predictive value of 93%, negative predictive value of 84%, and accuracy of 90% for diagnosing the cam deformity associated with femoroacetabular impingement. The Pearson correlation coefficients between the MRI and plain radiography values were 0.702, 0.552, and 0.349 for the Dunn, crosstable lateral, and AP views, respectively.
Conclusions
Our observations validate the clinical use of the Dunn view in the evaluation of the femoral head-neck contour in cam-type femoroacetabular impingement.
Level of Evidence
Level I, diagnostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Femoroacetabular impingement (FAI) is a recognized cause of hip pain in the young adult and is postulated to be a major cause of early osteoarthritis [12, 15, 26]. Ganz et al. [12] described two main forms of FAI. Cam-type impingement is the result of a deformity of the femur where there is a lack of concavity at the femoral head-neck junction resulting in insufficient femoral head-neck offset with subsequently reduced clearance for the femur during adduction, internal rotation, and flexion. This lack of clearance leads to impingement and shearing injury to the chondrolabral junction, resulting in labral tears and acetabular hyaline cartilage damage. Pincer-type impingement results from overcoverage of the femoral head by the acetabulum. This can be due to acetabular retroversion, coxa profunda, or acetabular protrusio.
In the majority of cases of hip dysplasia and pincer impingement [8], plain radiographs are sufficient to detect the osseous deformities, and magnetic resonance imaging (MRI) is not necessary to confirm the diagnosis. However, in cam-type FAI, Dudda et al. [10] have recently shown a normal, spherical-appearing femoral head on plain radiographs does not necessarily exclude the presence of a cam deformity, emphasizing the need for cross-sectional, multiplanar imaging. One reason for this is that the epicenter of the cam deformity is not always isolated to the anterosuperior femoral head-neck junction [16, 21, 22]. Thus, in theory, a cam deformity may be missed or underestimated if only a single radiographic image is evaluated [4, 17]. Consequently, this raises some questions about the accuracy of plain radiographs in the detection of a cam deformity. The accuracy of the alpha angle measured on the AP pelvis projection [13] or on lateral projections of the hip (the crosstable lateral [11] or Dunn views [17]) compared to the alpha angle measured using a multiplanar imaging modality such as MRI and computed tomography (CT) has never been investigated.
Therefore, we determined (1) the inter- and intraobserver reliability of the three different radiographic views, (2) the sensitivity and specificity of the plain radiograph alpha angle measurements as compared to MRI and (3) the degree of agreement between the alpha angle measurements obtained from the Dunn view and MR arthrogram (MRA).
Patients and Methods
In January 2006, a prospective database of all patients undergoing joint-preserving surgery of the hip was established and approved by the institutional review board. As of February 2009, 286 patients had been entered, with 169 undergoing hip arthroscopy, 68 surgical dislocation, and 48 periacetabular osteotomy. As part of the clinical protocol, all patients underwent a preoperative complete set of plain radiographic views and a MRA of the symptomatic hip. From this database, we identified 83 patients younger than 61 years presenting with unilateral hip pain, a positive impingement sign, positive labral pathology on MRA, no radiographic signs of dysplasia, and no prior hip surgery. Fifteen of these 83 patients (18%) had inadequate plain radiographs (i.e., not well centered or the patient’s pelvis was rotated), leaving 68 patients for the study group. The study group had a mean age of 38 years (range, 17–60 years), with 37 females and 31 males and with 29 left and 39 right hips.
Plain radiographs were taken by radiology technologists using standardized techniques as described by Clohisy et al. [8]. The AP pelvis radiograph was taken with the patient supine on the radiographic table with both lower extremities oriented in 15° of internal rotation. The tube was oriented perpendicular to the table. The crosstable lateral was taken with the patient supine on the radiographic table with the contralateral hip and knee flexed beyond 80° and the symptomatic limb internally rotated 15° to expose the anterolateral surface of the femoral head-neck junction. The Dunn view was taken with the patient supine with the symptomatic hip flexed at 90° and abducted 20° in neutral rotation
MRA is the standard test at our institution for the investigation of FAI and internal hip derangement. In addition to evaluation of the femoral head-neck contour, MRA also allows for detection of associated labral and chondral injury. As per the routine MRA protocol, each hip was injected with 10 to 15 mL of a dilute (2 mmol) gadolinium-saline solution (Omniscan®; GE Healthcare, Princeton, NJ) under fluoroscopic guidance by a musculoskeletal radiologist. The MRI scan was initiated within 30 minutes of the injection. The examinations were carried out on a 1.5-T scanner (Symphony Quantum; Siemens, Erlangen, Germany) with a flexible surface coil. The protocol included a three-dimensional isotropic, T1-weighted spoiled gradient echo (MPRAGE/Turbo-FLASH) sequence with water excitation (25-cm field of view, 1-mm slice thickness, 256 × 256 matrix, TR/TE/flip angle = 1970 ms/7 ms/15º, 1 average). Multiplanar reformation (MPR) was carried out to generate 2-mm-thick oblique axial and oblique sagittal plane images, parallel and perpendicular to, respectively, the long axis of the femoral neck. The latter plane was used to prescribe the radial MPR, using the center of the femoral neck as the axis of rotation, with 2-mm-thick images generated at 15° intervals. As such, all radial MPR images were oriented orthogonal to the femoral head-neck junction.
All radiographs and MRI images were sent to PACS (McKesson Horizon Rad Station 3.3, San Francisco, CA) for review. Using the method of Nötzli et al. [19], the alpha angle was measured on each of the plain radiographs: AP pelvis, crosstable lateral, and Dunn view, by two blinded readers. The first arm (1) of the angle was the long axis of the femoral neck, defined as the line drawn between the center of the femoral neck at its narrowest point to the center of the best fit circle. The second arm (2) of the angle was drawn from the center of the best fit circle anteriorly to the point where the head extended beyond the margin of the circle. The alpha angle formed provides a quantitative measurement of the degree of femoral head asphericity and/or lack of head-neck junction offset and/or concavity. All measurements were repeated 4 weeks later to determine the inter- and intraobserver agreement. In addition, femoral head sphericity was assessed on the AP view as described by Dudda et al. [10] Alpha angle measurements were also performed on the axial oblique MR image through the midfemoral neck and on a radial image through the anterosuperior femoral neck at the 1:30 clock face position by an experienced musculoskeletal radiologist. The mean alpha angle measurement on MRI using the standard oblique axial image was 59° (range, 37°–88°) (Table 1). Forty-three of 68 hips had an alpha angle of more than 50.5° as measured on MRI axial oblique view (cam positive) with impingement confirmed intraoperatively by direct visualization of the cam lesion (Fig. 1). The remaining 25 hips had an alpha angle of 50.5° or less (cam negative) and were treated for isolated labral pathology by means of hip arthroscopy. In six patients, the plain radiograph was positive for a cam deformity while the oblique axial MRI was negative. However, using the alpha angle value measured at the 1:30 position on the radial MRI series as described by Rakhra et al. [22], all of the hips had alpha angles of more than 50.5° on MRI (Table 2). The intra- and interclass reliability measurements for the two observers for each of the plain radiographic projections ranged from .85 to .98 (Table 3).
Table 1.
Mean alpha angle (and range) obtained for each view and Pearson correlation coefficients for each view as compared to the axial oblique MRI
| Imaging | AP view | Cross table | Dunn view | MRI |
|---|---|---|---|---|
| Alpha angle | 65 (34–118) | 63 (32–101) | 61 (35–94) | 59 (37–88) |
| Pearson correlation coefficient | 0.349 p < 0.05 | 0.552 p < 0.001 | 0.702 p < 0.001 | 1 |
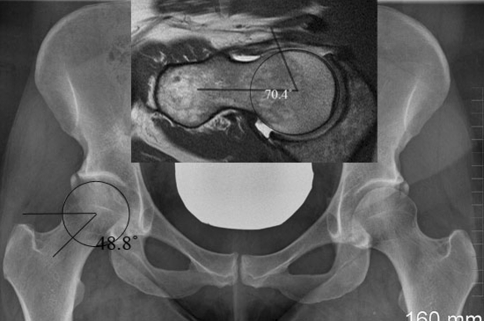
Fig. 1.
An AP radiograph of a 33-year-old woman with right hip pain is shown. The alpha angle is measured. The femoral head appears spherical with an alpha angle of 48.8°. The inset shows an axial oblique MR image with an alpha angle measuring 70.4°.
Table 2.
Cases where at least one plain film view is diagnostic for cam and the axial oblique MRI is not. These are compared to the radial reformat values which were positive in all but one case
| AP value | Cross table | Dunn | Axial | Radial | |
|---|---|---|---|---|---|
| 1 | 43 | 72 | 68 | 48 | 63 |
| 2 | 45 | 53 | 42 | 48 | 54 |
| 3 | 42 | 50 | 62 | 44 | 43 |
| 4 | 87 | 63 | 66 | 45 | 53 |
| 5 | 83 | 76 | 69 | 50 | 68 |
| 6 | 80 | 53 | 47 | 50 | 55 |
Table 3.
The intra- and interobserver reliability (with confidence intervals) of plain radiography for measuring the alpha angle
| AP view | Cross table view | Dunn view | |
|---|---|---|---|
| Intraobserver | 0.884 (0.746–0.949) | 0.947 (0.88–0.977) | 0.979 (0.952–0.991) |
| Interobserver | 0.947 (0.909–0.969) | 0.85 (0.751–0.911) | 0.90 (0.832–0.942) |
The sensitivity and specificity of the plain radiograph alpha angle measurements were calculated using a threshold alpha angle value of 50.5° as measured on the axial oblique MRI view. To determine the degree of agreement between the alpha angle measurements obtained from MRA and plain radiography, Pearson correlation coefficients were used. Bland and Altman plots were further used to provide a visual assessment of alpha angle measurement agreement between the Dunn view and MRA. This plot included horizontal lines depicting the level of bias and the limits of agreement [7]. The results were analyzed using SPSS® software (Version 15.0; SPSS Inc, Chicago, IL).
Results
The Dunn view had the highest sensitivity and specificity of 0.91 and 0.88, respectively, whereas the AP pelvis projection alone had a sensitivity and specificity of 0.60 and 0.81, respectively (Table 4). On plain radiographs of the 43 subjects with an alpha angle of more than 50.5° on MRI (cam positive), a cam deformity was present in 30 on the AP pelvis, 39 on the crosstable lateral, and 42 on the Dunn view. Evaluation of the shape of the femoral head on the AP radiograph found 38 hips had normal, spherical femoral heads, although 19 (50%) of these 38 patients had an alpha angle of more than 50.5° (cam positive) as determined on the oblique axial MRI (Fig. 1).
Table 4.
Comparison of sensitivity, specificity, positive predictive value, negative predictive value and accuracy (with confidence intervals) of the three views in comparison to the axial oblique MRI values
| View | AP | Cross table | Dunn |
|---|---|---|---|
| Sensitivity | 0.60 (0.44–0.75) | 0.74 (0.59–0.86) | 0.91 (0.78–0.97) |
| Specificity | 0.81 (0.58–0.95) | 0.63 (0.38–0.84) | 0.88 (0.68–0.97) |
| PPV | 0.60 (0.69–0.96) | 0.82 (0.66–0.92) | 0.93 (0.80–0.98) |
| NPV | 0.50 (0.32–0.68) | 0.52 (0.31–0.73) | 0.84 (0.64–0.95) |
| Accuracy | 0.67 (0.54–0.78) | 0.71 (0.58–0.82) | 0.90 (0.80–0.96) |
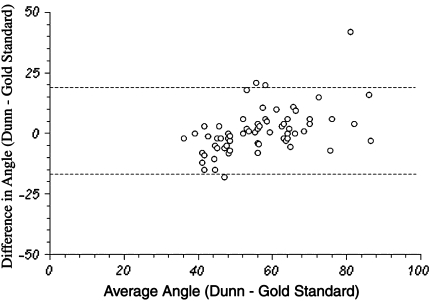
The Pearson correlation coefficients between the MRI and plain radiography values were 0.702 (p < 0.001), 0.552 (p < 0.001), and 0.349 (p < 0.05) for the Dunn, crosstable lateral, and AP views, respectively (Fig. 2). The Bland-Altman plot (Fig. 3) plots the average value of the alpha angle between the Dunn and MRI reading for each patient, ie, the theoretical true value (x axis) against the difference between them, ie, how far apart the two values are (y axis). The dotted lines represent two SDs from the norm and the majority of the results in our study lie within these lines.
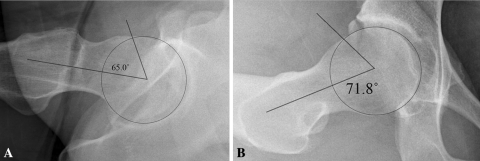
Fig. 2A–B.
The alpha angle is measured on both the (A) crosstable and (B) Dunn views with respective values of 65.0° and 71.8°.
Fig. 3.
A Bland-Altman plot showing a high level of agreement between alpha angle values on the Dunn view compared to the axial oblique MRI (gold standard [Std]).
Discussion
With respect to cam-type FAI, although the deformity was long recognized as a tilt or pistol grip deformity [18, 23, 24], there was no real way to quantify the deformity as one would do using the center edge angle for dysplasia. The introduction of the alpha angle by Nötzli et al. [19] measured on MRI has provided clinicians and researchers a way to quantify the contour deformity of the femoral head-neck junction and permit the development of treatment guidelines [1, 2, 25]. Having said that, because of the three-dimensional nature of the cam deformity, it is unclear how the alpha angle measured on plain radiographs correlates with MRI measurements. This is critical as numerous authors have solely used alpha angle measurements on plain radiographs to determine the natural history of the cam deformity [2, 14] and evaluate its severity [1]. However, the quantification of the cam deformity using the alpha angle on plain radiographs has yet to be validated. Therefore, we determined (1) the sensitivity and specificity of the plain radiograph alpha angle measurements as compared to MRI and (2) the degree of agreement between the alpha angle measurements obtained from the Dunn view and MRA.
We acknowledge limitations of our study. First, data on what alpha angle values represent a normal femoral head-neck junction are still lacking. We used the current standard of 50.5° as the cutoff value for an alpha angle to diagnose cam impingement [5, 25]. However, some patients may not have had true cam impingement and others may have had impingement but not diagnosed as such. Consequently, the diagnosis of cam FAI cannot be based solely on the alpha angle value but rather on the overall clinical presentation. Further research is required to better define what represents a normal femoral head-neck contour. Second, although we know that the measurement and subsequent interpretation of the alpha angle value on MRI is a function of the imaging plane, we cannot definitely state the exact location on the femoral head-neck junction that is represented by the Dunn view. However, because of the strong correlation (0.702) between alpha angle values on the Dunn view and the axial oblique MRI, we can state with some certainty that the Dunn view is highly representative of the MRI in terms of alpha angle measurements.
We found plain radiographic evaluation with measurement of the alpha angle had a relatively high positive predictive value (> 0.8) with both the crosstable and Dunn views using the axial oblique MRI alpha angle value as the gold standard [19]. In contrast, the use of a single AP radiograph has a sensitivity of only 60% compared to 74% and 90% for the crosstable and Dunn views, respectively. The accurate assessment of the cam deformity is especially critical as Nouh et al. [20] recently showed a simple visual estimation of the presence or absence of a cam deformity was a poor predictor of an abnormal measured alpha angle. This also corroborates the study of Clohisy et al. [9], which reported a poor inter- and intraobserver reliability in diagnosing cam-type FAI on plain radiographs when using a simple qualification of presence or absence of sphericity. The greater sensitivity and specificity of the Dunn view over the crosstable lateral and AP radiograph projections in quantifying the alpha angle is consistent with the findings of Meyer et al. [17]. More specifically, our study confirms the findings of Dudda et al. [10] that the appearance of a spherical femoral head on the AP radiograph cannot exclude the presence of a cam deformity, as 19 of 38 (50%) patients with a spherical head had a cam deformity detected by MRI. The limitations of plain radiography in accurately quantifying the maximal alpha angle is consistent with the MRI studies of Pfirrmann et al. [21] and Rakhra et al. [22], which showed the epicenter or peak of the cam deformity can vary between the 1:30 and 3:00 positions. These findings are consistent with the six false-positive cases on the Dunn view where the alpha angle was normal on the axial oblique MR image but abnormal on the 1:30 radial image. It follows from this that the radial series images may be required in borderline cases and may be more sensitive than the oblique axial MRI plane view in detecting a cam deformity.
However, the strong correlation between the alpha values measured on MRI and the Dunn view as shown on the Bland-Altman plot suggests radiographs alone may be adequate for evaluation of the femoral head-neck junction in the investigation and management of cam FAI. More importantly, this emphasizes the importance of a proper and detailed clinical evaluation in determining the underlying pathology of patients complaining of hip pain where diagnostic imaging is complementary to the overall patient evaluation but not the sole tool for diagnosing cam FAI [3]. In addition, the cam deformity is not necessarily focal and can be diffuse along a portion of the femoral head-neck junction [6, 21, 22]. Thus, imaging with MRI and/or CT should be the gold standard in the identification of a cam deformity due to their multiplanar capability.
Traditionally, plain radiographs have been, and still are, the standard for evaluating the severity of bony abnormality and deficiency. In specific relation to the hip, plain radiographs are the mainstay in the evaluation of hip dysplasia and arthritis. This can be said also of FAI, and although previous studies have demonstrated the important role of proper lateral radiographs in the evaluation of the femoral head-neck contour for a cam deformity, this study demonstrates and confirms the accuracy of the alpha angle measurement on plain radiographs in quantifying the cam deformity when compared to the gold standard, multiplanar MRI. However, given the secondary derangement a cam deformity can cause to the labrum and cartilage, MRI will remain a powerful tool in the investigation of FAI as it will give further information to the clinician for prognostication and patient counseling.
Acknowledgment
We thank Steve Doucette, MSc from the Ottawa Hospital Methods Center for his assistance with data analysis.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Allen DJ, Beaule PE, Ramadan O, Doucette S. Prevalence of associated deformities and hip pain in patients with cam type femoroacetabular impingement. J Bone Joint Surg Br. 2009;91:589–594. doi: 10.1302/0301-620X.91B5.22028. [DOI] [PubMed] [Google Scholar]
- 2.Bardakos NV, Villar RN. Predictors of progression of osteoarthritis in femoroacetabular impingement. A radiological study with a minimum of ten years follow-up. J Bone Joint Surg Br. 2009;91:162–169. doi: 10.1302/0301-620X.91B2.21137. [DOI] [PubMed] [Google Scholar]
- 3.Beaule PE, Allen DJ, Clohisy JC, Schoenecker PE, Leunig M. The young adult with hip impingement: deciding on the optimal intervention. J Bone Joint Surg Am. 2009;91:210–221. doi: 10.2106/JBJS.H.00802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beaule PE, Harvey N, Zaragoza EJ, LeDuff M, Dorey FJ. The femoral head/neck offset and hip resurfacing. J Bone Joint Surg Br. 2007;89:9–15. doi: 10.2106/JBJS.F.00681. [DOI] [PubMed] [Google Scholar]
- 5.Beaule PE, LeDuff M, Zaragoza EJ. Quality of life following femoral head-neck osteochondroplasty for femoroacetabular impingement. J Bone Joint Surg Am. 2007;89:773–779. doi: 10.2106/JBJS.F.00681. [DOI] [PubMed] [Google Scholar]
- 6.Beaule PE, Zaragoza EJ, Motamedic K, Copelan N, Dorey J. Three-dimensional computed tomography of the hip in the assessment of femoro-acetabular impingement. J Orthop Res. 2005;23:1286–1292. doi: 10.1016/j.orthres.2005.03.011.1100230608. [DOI] [PubMed] [Google Scholar]
- 7.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 8.Clohisy JC, Carlisle JC, Beaule PE, Kim Y-J, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PE, Millis M. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90:47–66. doi: 10.2106/JBJS.H.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clohisy JC, Carlisle JC, Trousdale RT, Kim Y-J, Beaule PE, Morgan P, Steger-May K, Schoenecker PE, Millis M. Radiographic evaluation of the hip has limited reliability. Clin Orthop Relat Res. 2009;467:666–675. doi: 10.1007/s11999-008-0626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dudda M, Albers C, Mamisch T, Werlen S, Beck M. Do normal radiographs exclude asphericity of the femoral head-neck junction? Clin Orthop Relat Res. 2009;467:651–659. doi: 10.1007/s11999-008-0617-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eijer H, Leunig M, Mahomed N, Ganz R. Cross-table lateral radiographs for screening of anterior femoral head-neck offset in patients with femoro-acetabular impingement. Hip Int. 2001;11:37–41. [Google Scholar]
- 12.Ganz R, Parvizi J, Leunig M, Siebenrock KA. Femoroacetabular Impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 13.Gosvig KK, Jacobsen S, Palm H, Sonne-Holm S, Magnusson E. A new radiological index for assessing asphericity of the femoral head in cam impingement. J Bone Joint Surg Br. 2007;89:1309–1316. doi: 10.1302/0301-620X.89B10.19405. [DOI] [PubMed] [Google Scholar]
- 14.Gosvig KK, Jacobsen S, Sonne-Holm S, Gebuhr P. The prevalence of cam-type deformity of the hip joint: a survey of 4151 subjects of the Copenhagen Osteoarthritis Study. Acta Radiol. 2008;49:436–441. doi: 10.1080/02841850801935567. [DOI] [PubMed] [Google Scholar]
- 15.Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20–33. [PubMed] [Google Scholar]
- 16.Ito K, Minka-II MA, Leunig S, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. J Bone Joint Surg Br. 2001;83:171–176. doi: 10.1302/0301-620X.83B2.11092. [DOI] [PubMed] [Google Scholar]
- 17.Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparision of six radiographic projections to assess femoral head/asphericity. Clin Orthop Relat Res. 2006;445:181–185. doi: 10.1097/01.blo.0000201168.72388.24. [DOI] [PubMed] [Google Scholar]
- 18.Murray RO. The aetiology of primary osteoarthritis of the hip. Br J Radiol. 1965;38:810–824. doi: 10.1259/0007-1285-38-455-810. [DOI] [PubMed] [Google Scholar]
- 19.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour fo the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 20.Nouh MR, Schweitzer ME, Rybak L, Cohen J. Femoroacetabular impingement: can the alpha angle be estimated? AJR Am J Roentgenol. 2008;190:1260–1262. doi: 10.2214/AJR.07.3258. [DOI] [PubMed] [Google Scholar]
- 21.Pfirrmann CW, Mengiardi B, Dora C, Kalverer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characterstic MR arthrographic findings in 50 patients. Radiology. 2006;240:778–785. doi: 10.1148/radiol.2403050767. [DOI] [PubMed] [Google Scholar]
- 22.Rakhra K, Sheikh AM, Allen DJ, Beaule PE. Comparison of MRI alpha angle measurement planes in femoroacetabular impingement. Clin Orthop Relat Res. 2009;467:660–665. doi: 10.1007/s11999-008-0627-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Solomon L. Patterns of osteoarthritis of the hip. J Bone Joint Surg Br. 1976;58:176–183. doi: 10.1302/0301-620X.58B2.932079. [DOI] [PubMed] [Google Scholar]
- 24.Stulberg SD, Cordell LD, Harris WH, Ramsey PL, MacEwen GD. Unrecognized childhood hip disease: a major cause of idiopathic osteoarthritis of the hip. In: Amstutz HC, ed. The Hip, Proceedings of the Third Open Scientific Meeting of the Hip Society. St. Louis, MO: C.V. Mosby; 1975:212–228.
- 25.Tannast M, Siebenrock KA, Anderson S. Femoroacetabular impingement: radiographic diagnosis - what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 26.Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004;429:170–177. doi: 10.1097/01.blo.0000150119.49983.ef. [DOI] [PubMed] [Google Scholar]