Abstract
Background
Recent attention in THA has focused on minimally invasive techniques and their short-term outcomes. Despite much debate over the outcomes and complications of the two-incision and the mini-lateral and mini-posterior approaches, complications arising from use of the anterior THA on a fracture table are not well documented.
Questions/purposes
We determined the intraoperative and postoperative complications with the anterior approach to THA through an extended single-surgeon patient series.
Methods
We reviewed 800 primary THAs performed anteriorly with the aid of a fracture table over 5 years and recorded all intraoperative and postoperative complications up to latest followup (average, 1.8 years; range, 0–5 years). Patients with severe acetabular deformity or severe flexion contractures were excluded and those surgeries were performed with a lateral approach during the time period of this study.
Results
Intraoperative complications included 19 trochanteric fractures, three femoral perforations, one femoral fracture, one acetabular fracture, one bleeding complication, and one case of cardiovascular collapse. There were no ankle fractures. Postoperative complications included seven patients with dislocations; seven with deep infections; one with delayed femur fracture; 37 with wound complications, among which 13 had reoperation for local débridement; 14 with deep venous thrombosis; and two with pulmonary embolism; and 31 other nonfatal medical complications.
Conclusions
The main intraoperative complications of trochanteric fractures and perforations occurred mostly early in the series, while the main postoperative complications related to wound healing were prevalent throughout the entire series. Despite potential advantages of use of a fracture table, surgeons should be aware of the potential complications of trochanteric fractures, perforations, and wound-healing problems associated with this technique.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
In recent years, debate over minimally invasive surgical (MIS) approaches for THA has focused on the two-incision, the mini-lateral, the mini-posterior technique, and more recently, the single-incision anterior THA. Early reports on patient outcome seemed to favor MIS techniques [4, 5, 8, 9, 11, 16], while later reports cautioned against the wide utilization of these techniques due to increased complications related to femur fractures, implant failures, and muscle trauma [2, 13, 14, 18] and the lack of demonstrable clinical benefit [12, 14, 18].
The rationale suggested by proponents of the anterior approach is that by sparing the lateral and posterior muscles during surgical dissection, patients should be afforded a quicker recovery with fewer functional limitations and less risk of dislocation [5, 10, 16, 17]. The technique uses a specialized fracture table to assist in exposure and fluoroscopy for aiding in implant position and insertion [10]. After the initial reports that described the successful use of this technique [5, 10, 16], some authors have reported high complication rates with the procedure [3, 19]. Woolson et al. [19] reported longer operative times, increased blood loss, and increased revision rates when they reviewed the early experience of four surgeons utilizing the anterior technique. However, the complications are not well documented in the literature from other series.
We determined (1) the complication rates associated with this technique; (2) how these complications changed over time related to surgeon experience; and (3) how the complications with this technique compared to complications reported for standard THA and other MIS techniques.
Patients and Methods
We retrospectively reviewed all 800 primary THAs performed with an anterior approach from January 2004 to April 2009. During that time period, THAs were performed with a lateral approach in 187 patients with severe obesity (body mass index > 40), or a flexion contracture greater than 30°, or with severe acetabular bone loss deformity that could not be solved with a cementless hemispherical cup. There were 374 men (47%) and 426 women (53%) in the study group, with an average age of 62.5 years (range, 23–91 years). The average body mass index of the group was 28 (range, 19–43). Clinical followup averaged 1.8 years (range, 0–5 years). No patients were lost to followup.
All operations were performed by a single surgeon (BAJ) using the anterior approach with fracture table assistance, as described by Matta et al. [10]. The anterior (modified Heuter [15]) approach was used for exposure, and fluoroscopy was used to aid in implant position and anatomic referencing, as described by Matta et al. [10]. All THAs were performed with cementless acetabular components (Trilogy® or Trabecular Metal®; Zimmer, Inc, Warsaw, IN) and cementless femoral components (Alloclassic®; Zimmer). The average blood loss was 417 mL (range, 200–1200 mL).
Our standard protocol for prophylaxis during the time of study was low-molecular-weight heparin (Fragmin®; Pfizer, New York, NY) for 14 days postoperatively. We obtained ultrasounds only in patients with symptoms of deep vein thrombosis.
Patients were seen preoperatively and postoperatively at 6 weeks, 3 months, and 1 year and biannually thereafter with clinical examinations that included gait, ROM, and strength assessment. Standard radiographs of the operative hip were taken at 6 weeks postoperatively and at the annual visit. Our independent research institute, the Slocum Foundation, maintains a prospective THA database (Axis, Portland, OR). Patient-generated data are collected preoperatively and annually from patient questionnaires, while surgeon-generated data are collected preoperatively, at the time of surgery, at each patient visit, and with the occurrence of any complication. All known complications are entered into the database in real time and also retrospectively collected and reviewed at each patient visit.
To assure complete capture of all complications, we crossreferenced those 800 cases to the hospital-based discharge charts and discharge database, which captures complication codes, and finally crossreferenced the 800 cases to the clinical charts held at Slocum Orthopedics. All known complications were captured and compiled for descriptive study.
Complications were broken down into two categories: intraoperative complications and postoperative complications. Postoperative complications were described as medical or surgical. Reoperations were tabulated for report.
Results
There were 26 total (3.2%) intraoperative complications (Table 1). There were 19 (2.3%) trochanteric fractures. Sixteen small (< 1 cm) superoposterior capsular avulsions occurred during femoral elevation using the table. These avulsions had no specific intraoperative treatment or postoperative modifications and had no negative impact on recovery, gait, strength, or pain at latest followup. Three larger trochanteric fractures occurred during broaching of the femoral canal. These fractures were not specifically treated intraoperatively, and all three led to a mild painless Trendelenburg limp at latest followup. All but four trochanteric injuries occurred within the first 200 cases in the series. There were three (0.37%) femoral canal perforations while broaching. Each perforation was recognized intraoperatively and was treated by redirection of the primary stem broach, with eventually implantation of the primary cementless stem with no postoperative restrictions. Each of these patients had an uncomplicated recovery with a good clinical outcome. All of the perforations occurred within the first 150 cases of the series. One patient sustained an intraoperative femoral shaft fracture. This patient had a prior DHS plate removed concomitantly, and a spiral fracture propagated from a screw hole during broaching. The anterior approach was aborted and closed, and the patient underwent an immediate posterior approach with the use of a long cementless stem and open cerclage cabling of the femur. One patient sustained a posterior wall acetabular fracture on implant impaction and was treated with exchange to Trabecular Metal® cup without further problems. One patient suffered complete cardiac collapse intraoperatively that required cardiopulmonary resuscitation and immediate wound closure with trials in place and a 3-day intensive care unit resuscitation before completing the surgery with real implants. There were no ankle fractures in this series.
Table 1.
Intraoperative complications
| Complication | Number |
|---|---|
| Trochanteric fracture | 19 (2.3%) |
| Femoral perforation | 3 (0.37%) |
| Femur fracture | 1 (0.12%) |
| Acetabular fracture | 1 (0.12%) |
| Bleeding | 1 (0.12%) |
| Cardiovascular | 1 (0.12%) |
| Ankle fracture | 0 |
| Total | 26 |
There were 91 (11.3%) postoperative complications (Table 2). Seven total patients (0.88%) suffered dislocations. Of the seven patients, three sustained a single posterior dislocation, two sustained a single anterior dislocation, and one patient has dislocated three times posteriorly. One dislocation was diagnosed in the recovery room requiring immediate cup revision. The other patients have not been revised. There were seven deep infections (0.88%). Five cases were diagnosed acutely and treated with irrigation and débridement and component retention. All five occurred greater than 4 months postoperatively. There were two cases of delayed chronic deep infection treated with two-stage reimplantation.
Table 2.
Postoperative complications
| Complication | Number |
|---|---|
| Infection | 7 (0.88%) |
| Dislocation | 7 (0.88%) |
| Wound healing | 37 (4.6%) |
| Femur fracture | 1 (0.12%) |
| Superficial nerve injury | 1 (0.12%) |
| DVT/PE | 14 (1.75%)/2 (0.25%) |
| Other medical | 24 (3.1%) |
| UTI | 4 |
| A-Fib | 2 |
| Delirium | 10 |
| Ileus | 2 |
| Pneumonia | 2 |
| MI | 1 |
| CVA | 1 |
| Other CV | 2 |
| Total | 91 |
DVT = deep venous thrombosis; PE = pulmonary embolism; UTI = urinary tract infection; A-Fib = atrial fibrillation; MI = myocardial infarction; CVA = cerebrovascular accident; CV = cerebrovascular.
There were 37 wound complications (4.6%). Twenty-four patients (3%) developed a noninfectious ulcerative dehiscence typically in the groin crease and were treated as outpatients with local wound care without further incident. Thirteen (1.6%) patients required readmission and irrigation and débridement for larger wound necrosis or superficial infection débridement. No patient with a wound complication ever developed deep infection, and none of the infections had postoperative wound problems.
One patient sustained a postoperative fracture at 6 weeks and was successfully revised to cables and a long revision cementless stem. There was only one confirmed case of painful superficial femoral neuralgia. There were no cases of femoral nerve palsy. Fourteen patients were diagnosed with deep venous thrombosis and two patients with pulmonary embolism. There were 24 other nonfatal medical complications (Table 2).
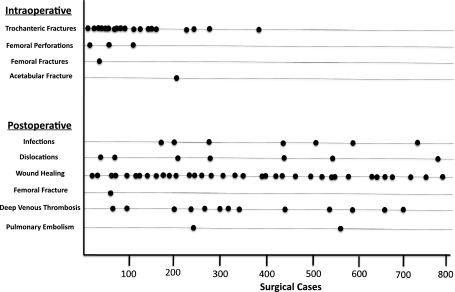
There were 26 total reoperations. There were two femoral fractures (one intraoperative and one postoperative) requiring revision. One patient was revised immediately for dislocation. Thirteen patients underwent wound débridement. Seven patients were revised for infection. One patient returned to the operating room for bleeding from a drain that punctured a superficial varicose vein (blood loss of 1200 mL). One patient underwent revision for head-ball exchange 2 years postoperatively for leg length discrepancy. There were no revisions for loose implants outside the cases of infection. The chronological timeline of complications is presented (Fig. 1).
Fig. 1.
A timeline shows the complications in chronological case order. DVT = deep venous thrombosis.
Discussion
Many early reports of MIS THA related to two-incision technique [4, 8] and both the mini-posterior [5, 16] and mini-lateral approaches [9, 11] demonstrated rapid early return to function for selected patients; however, later investigations showed increased complications, especially with the two–incision technique [2, 13], and no clear benefit of these MIS techniques when compared to standard THA [12, 14]. Early reports regarding anterior THA with fracture table assistance showed safe and early return to function for patients [1, 10], but later reports attempted to show higher rates of complications [19], but these reports were limited to the early experience of a few surgeons. We therefore determined (1) the complication rates associated with this technique, (2) how these complications changed over time related to surgeon experience, and (3) how the complications with this technique compared to complications reported for standard THA and other MIS techniques.
Our study is subject to several limitations. First, we had no control group of alternate approaches for comparison; however, we intended this as a descriptive and not a comparative study. Second, we excluded patients with extreme obesity, hip contractures, and severe acetabular deformity not amenable to hemispherical cup reconstruction. Thus, the findings are not generalizable to a wider population. Their inclusion could have led to higher complications. Third, all operations were performed by a single surgeon familiar with the technique and the complication rates might not be generalizable, particularly for a surgeon doing small numbers of cases.
The intraoperative complications of trochanteric fractures and femoral perforations were higher in our series than in other series of THA, while the individual complications of one femoral fracture, one acetabular fracture, one cardiovascular collapse, and one case of excessive bleeding were not unique and are typical of many series of THAs [4, 6–8]. The majority of trochanteric fractures seen in our series were small posterior capsular avulsions. These typically occurred during femoral exposure where the specialized hook that lifts the femur anteriorly from the wound produces tension on the posterior superior hip capsule attached to the lateral greater trochanter. None of these avulsions were treated intraoperatively, no restrictions were placed on patients postoperatively, and none of these patients demonstrated any loss of strength, disturbance of gait, or pain associated with these trochanteric injuries at latest followup. The three larger trochanteric fractures resulted from femoral broaching. The complication timeline (Fig. 1) shows all of these fractures occurred relatively early in the series, and none were seen in the second half of the series. Trochanteric injuries were avoided by using the second-generation fracture table with an electronic hook elevation system that is surgeon controlled, which allows for a more gradual and gentle elevation of the femur. This system, combined with a better understanding of the tension applied on the femur and necessary superior capsular and occasional periformis tendon release during exposure, led to the resolution of trochanteric injuries. The Alloclassic® stem system has a lateral proximal hump that requires a deeper intrusion into the trochanter and possibly places the trochanter at greater risk of fracture. Implant selection might have an effect on the rate of trochanteric injuries. The three femoral perforations all occurred early in the series in patients with severe flexion contractures and have since been avoided by understanding the effect of flexion contractures on the appropriate insertion angle of the starting broach, where a more horizontal angle is required to follow the angle of the femur that remains in the contracted position during femoral exposure.
The postoperative wound complication rate was higher in our series than in most other series, while the dislocation, deep infection, revision, and medical complications encountered were similar to other large series of THAs [4, 6–8]. Our series demonstrated a 4.6% rate of serious wound-healing complications with a 1.6% reoperation rate for wound infections and wound necrosis. This most likely represents the different properties of the skin anteriorly, being noticeably thinner in the proximal thigh as compared to the lateral thigh, as well as increased skin tension across the flexion crease that could cause increased shear stress that may affect skin healing. Despite attempts to change the location and pattern of the skin incision, the problem persisted throughout the entire length of the series (Fig. 1). Despite the high number of wound-healing complications, no patient with wound problems had a deep infection, and the deep infection rate of 0.8% is comparable to other series [4, 6–8]. The dislocation rate of 0.8% is comparable to other series of THA [4, 6–8], demonstrating, despite fluoroscopic assistance with this approach, the technique does not eliminate the risk of postoperative dislocation.
Woolson et al. [19] reported increased complication rates related to trochanteric injuries, femur fractures, and femoral revisions with the anterior approach when they studied the outcomes associated with the early experience of four community surgeons. The series, however, reported only the early cases of these surgeons. In our series, the problem of trochanteric injuries and femoral perforations occurred only early in the series and resolved with surgeon experience. Our single-surgeon series did not show a high femoral fracture rate or femoral loosening or revision rate like that reported by Woolson et al. [19].
Although the single-incision anterior approach for THA reportedly confers rapid functional recovery [1, 10], our data suggest the technique has a high persistent wound-healing complication rate and a high early rate of trochanteric injuries and femoral perforations. Teaching and education of surgeons learning the approach, as well as implant selection, should focus on how to prevent trochanteric injuries and perforations that were seen early in our series.
Acknowledgment
We thank Crystal Mills, Coordinator for Slocum Research & Education Foundation, for her efforts in support of the project and manuscript.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Anterior Total Hip Arthroplasty Collaborative Investigators. Bhandari M, Matta JM, Dodgin D, Clark C, Kregor P, Bradley G, Little L. Outcomes following the single incision anterior approach to total hip arthroplasty: a multicenter observational study. Orthop Clin North Am. 2009;40:329–342. doi: 10.1016/j.ocl.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 2.Bal BS, Haltom D, Aleto T, Barrett M. Early complications of primary total hip replacement performed with a two incision minimally invasive technique. J Bone Joint Surg Am. 2005;87:2432–2438. doi: 10.2106/JBJS.D.02847. [DOI] [PubMed] [Google Scholar]
- 3.Barton C, Kim PR. Complications of the direct anterior approach for total hip arthroplasty. Orthop Clin North Am. 2009;40:371–375. doi: 10.1016/j.ocl.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Berger RA, Duwelius PJ. The two-incision minimally invasive total hip arthroplasty: technique and results. Orthop Clin North Am. 2004;35:163–172. doi: 10.1016/S0030-5898(03)00110-X. [DOI] [PubMed] [Google Scholar]
- 5.Chimento GF, Pavone V, Sharrock N, Kahn B, Cahill J, Sculco TP. Minimally invasive total hip arthroplasty: a prospective randomized study. J Arthroplasty. 2005;20:139–144. doi: 10.1016/j.arth.2004.09.061. [DOI] [PubMed] [Google Scholar]
- 6.Christie MJ, DeBoer DK, Trick LW, Brothers JC, Jones RE, Vise GT, Gruen TA. Primary total hip arthroplasty with use of the modular S-ROM prosthesis: four to seven year clinical and radiographic results. J Bone Joint Surg Am. 1999;81:1707–1716. doi: 10.2106/00004623-199912000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Clohisy JC, Harris WH. The Harris-Galante porous coated acetabular component with screw fixation: an average ten-year follow-up study. J Bone Joint Surg Am. 1999;81:66–73. doi: 10.2106/00004623-199901000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Duwelius PJ, Burkhart RL, Hayhurst JO, Moller H, Butler JB. Comparison of the 2-incision and mini-incision posterior total hip arthroplasty technique: a retrospective match-pair controlled study. J Arthroplasty. 2007;22:48–56. doi: 10.1016/j.arth.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Howell JR, Masri BA, Duncan CP. Minimally invasive versus standard incision anterolateral hip replacement: a comparative study. Orthop Clin North Am. 2004;35:153–162. doi: 10.1016/S0030-5898(03)00137-8. [DOI] [PubMed] [Google Scholar]
- 10.Matta JM, Shahrdar C, Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopedic fracture table. Clin Orthop Relat Res. 2005;441:115–124. doi: 10.1097/01.blo.0000194309.70518.cb. [DOI] [PubMed] [Google Scholar]
- 11.O’Brien DA, Rorabeck CH. The mini-incision direct lateral approach in primary total hip arthroplasty. Clin Orthop Relat Res. 2005;441:99–103. doi: 10.1097/01.blo.0000193812.31329.3a. [DOI] [PubMed] [Google Scholar]
- 12.Ogonda L, Wilson R, Archbold P, Lawlor M, Humphreys P, O’Brien S, Beverland D. A minimal-incision technique in total hip arthroplasty does not improve early postoperative outcomes: a prospective, randomized, controlled trial. J Bone Joint Surg Am. 2005;87:701–710. doi: 10.2106/JBJS.D.02645. [DOI] [PubMed] [Google Scholar]
- 13.Pagnano MW, Leone J, Lewallen DG, Hanssen AD. Two-incision THA had modest outcomes and some substantial complications. Clin Orthop Relat Res. 2005;441:86–90. doi: 10.1097/01.blo.0000191275.80527.d6. [DOI] [PubMed] [Google Scholar]
- 14.Pagnano MW, Trousdale RT, Meneghini RM, Hanssen AD. Slower recovery after two-incision than mini-posterior-incision total hip arthroplasty: surgical technique. J Bone Joint Surg Am. 2009;91(Suppl 2, Pt 1):50–73. doi: 10.2106/JBJS.H.01531. [DOI] [PubMed] [Google Scholar]
- 15.Rachbauer F, Kain MSH, Leunig M. The history of the anterior approach to the hip. Orthop Clin N Am. 2009;40:311–320. doi: 10.1016/j.ocl.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 16.Sculco TP, Boettner F. Minimally invasive total hip arthroplasty: the posterior approach. Instr Course Lect. 2006;55:205–214. [PubMed] [Google Scholar]
- 17.Siguier T, Siguier M, Brumpt B. Mini-incision anterior approach does not increase dislocation rate. Clin Orthop Relat Res. 2004;426:164–173. doi: 10.1097/01.blo.0000136651.21191.9f. [DOI] [PubMed] [Google Scholar]
- 18.Woolson ST, Mow CS, Syquia JF, Lannin JV, Schurman DJ. Comparison of primary total hip replacements with a standard incision or a mini-incision. J Bone Joint Surg Am. 2004;86:1353–1358. doi: 10.2106/00004623-200407000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Woolson ST, Pouliot MA, Huddleston JI. Primary total hip arthroplasty using an anterior approach and a fracture table: short term results from a community hospital. J Arthroplasty. 2009;24:999–1005. doi: 10.1016/j.arth.2009.04.001. [DOI] [PubMed] [Google Scholar]