Abstract
Background
Modular femoral stems are one option for revision THA surgeons and allow offset restoration, leg length discrepancy correction, and stability independent of distal stem fixation. The complexity of revision THA usually leads surgeons to use multiple revision hip designs to address these issues.
Questions/purposes
We evaluated functional outcomes with a revision modular system and determined whether such a system achieved initial distal fixation, femoral offset restoration, leg length equalization, and hip stability.
Methods
We prospectively followed 118 patients in whom a modular stem system was used for reconstruction of their failed index femoral stem. Sixty-nine hips were classified as Type I (classification of Paprosky et al.), 35 as Type II, 17 as Type III, and one as Type IV. Functional assessment was achieved using patient- and physician-administered outcome evaluations (SF-36, WOMAC, Lower Extremity Activity Scale, Harris hip score). Stem fixation, offset restoration, leg length discrepancy, and hip stability were evaluated radiographically. Complications were also recorded. Minimum followup was 2 years (average, 4 years; range, 2–7 years).
Results
Average values on all functional outcome evaluations showed improvement at latest followup. Distal bone ingrowth fixation was obtained in 100% of the patients, offset was corrected in 66%, leg length discrepancy was corrected in 78%, and stability was achieved in 97%. No failures or fractures at the body to stem junction were seen at latest followup.
Conclusions
Modular femoral components achieved functional outcomes and were useful to address distal fixation, femoral offset restoration, leg length equalization, and hip stability when revising failed femoral components.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Despite high function and survival rates after of primary THA, the burden of revision THA continues to increase [9, 10]. Choices of implants for revision surgery have evolved to deal with the increasing variety of problems seen, especially when severe bone defects may preclude the use of conventional prostheses.
Modular femoral components were developed to address concerns with offset, leg length discrepancy, and instability. Modular femoral components have the potential to make the surgical procedure easier by addressing these issues independently of each other. Solid initial distal fixation is a critical requirement for success of the reconstruction and a modular stem separates this step of the procedure from all other aspects of the revision procedure. Other goals of the revision surgery—offset restoration (important for muscle strength and function), leg length equality, and hip stability—then can be obtained independent of stem fixation [2, 7, 24].
We specifically evaluated the ability of modular stems to achieve (1) high functional scores (patient- and physician-administered); (2) initial distal fixation; (3) component offset restoration; (4) leg length equality; and (5) hip stability in patients who underwent revision hip arthroplasty. We further identified the complications with these devices.
Patients and Methods
We identified all 118 patients who underwent 122 revision hip surgeries (four bilateral) using an uncemented modular femoral component (Restoration Modular Stem®; Stryker Orthopaedics, Mahwah, NJ) between March 2003 and June 2007. Our revision total joint registry collects clinical and radiographic data on all patients undergoing revision arthroplasty prospectively. The indication for surgery in 98 (80%) was pain with radiographic evidence of femoral loosening; other reasons for revision included periprosthetic infection or fracture, fractured stem, and other (Table 1). Four (3.3%) patients had two previous hip arthroplasties, and 105 (89%) of the patients had one previous hip arthroplasty. Finally, 9% of the patients in this series had a history of previous nonarthroplasty hip surgery. We excluded two patients who had other modular stems implanted so all reported patients in this study received the same modular stem system. Gender, age, weight, height, and body mass index (BMI) as well as other demographic variables were collected. There were 64 females (66 hips [54%]) and 54 males (56 hips [46%]) with an average age of 68 years (range, 34–88 years), an average height of 169 cm (range, 147–201 cm), and an average weight of 82 kg (range, 41–217 kg), resulting in an average BMI of 28 kg/m2 (range, 13–58 kg/m2). The underlying diagnosis for the index THA was osteoarthritis in 104 (85%) hips, conversion from a failed treatment for a previous femoral neck fracture in nine (7%) hips, avascular necrosis in five (4%) hips, rheumatoid arthritis in three (2%) hips, and Paget’s disease in one (0.8%) hip. The minimum followup was 2 years (mean, 4 years; range, 2–7 years). Four patients (five hips [3%]) died during the study period, but all four had clinical and radiographic followup at 2 years and all four had bone ingrowth fixation of the femoral component at last followup. Effort to complete followup was attempted for all patients in our cohort; those who were not able to return for physical examination were contacted by telephone. Despite continued efforts, two patients (2%) could not be reached or did not return for the minimum 2-year followup. All other patients were followed clinically for a minimum of 2 years, until failure of the revision arthroplasty, or until death. We had prior Institutional Review Board approval.
Table 1.
Total hip revision (or conversion) surgery: distribution by cause
| Cause of revision | Number of hips | Percentage |
|---|---|---|
| Uncemented loose stem | 49 | 40% |
| Cemented loose stem | 38 | 31% |
| Periprosthetic infection | 11 | 9% |
| Conversion from open reduction and internal fixation | 9 | 7% |
| Fractured stem | 6 | 5% |
| Periprosthetic fracture | 6 | 5% |
| Instability | 2 | 2% |
| Leg length discrepancy | 1 | 0.8% |
The Restoration Modular Stem® system consists of a distal portion, a fluted stem, and a proximal portion or body. The distal portion is a titanium stem with a heavily grit-blasted fluted conical distal segment. The geometry of the conical stem is based on the philosophy of the Wagner design in that the fluted conical stem is believed to provide initial rotational stability [8, 23]. The stems are available in three lengths; a straight 155 mm, a straight or bowed 195 mm, and a bowed 235 mm. Each is available in 15 diameters (range, 14–28 mm) in 1-mm increments. The proximal portion or body is made of a titanium–aluminum-vanadium alloy (Ti-6Al-4 V ELI), it is circumferentially plasma sprayed with commercially pure titanium and sprayed over again with hydroxyapatite (HA) (PureFix™ HA; Stryker Orthopaedics); it has a regular cylindrical form for the “cone” type and a cobalt-chrome (CoCr) flange with perforations to allow proper abductor reattachment added to the cylindrical form in the “calcar” type. Both body types have a 132° neck angle and are available in seven body diameters (range, 19–31 mm) with 2-mm increments. The “cone” type body has four vertical offsets (+0 mm, +10 mm, +20 mm, and +30 mm) providing a vertical size of 70 mm, 80 mm, 90 mm, and 100 mm, respectively; the “calcar” type has only three vertical offsets (+10 mm, +20 mm, and +30 mm) providing a vertical size of 80 mm, 90 mm, and 100 mm, respectively. Both body types have a V40™ (Stryker Orthopaedics) trunion to accept CoCr 22-mm, 26-mm, 28-mm, 32-mm, or 36-mm heads or alumina ceramic 28-mm, 32-mm, or 36-mm heads. Lateral offset is achieved through head-neck increments of −4 mm, +0 mm, +4 mm, +8 mm, or +12 mm.
All procedures were performed by six surgeons through an anterolateral approach. No femoral osteotomy was used in 51 (42%) hips, whereas a standard slide trochanteric osteotomy [14] was performed in 13 (11%) and an extended trochanteric osteotomy [14] was performed in the remaining 58 (48%) hips. The indications for extended trochanteric osteotomy were to achieve faster exposure, easier component removal, and a more satisfactory reconstruction. Cortical strut allografting was undertaken in 12 (10%) cases.
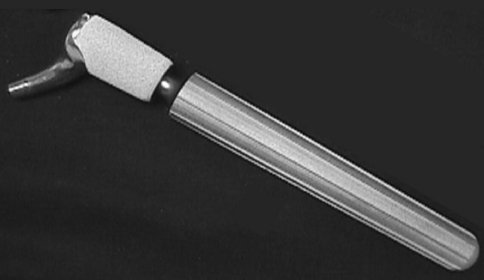
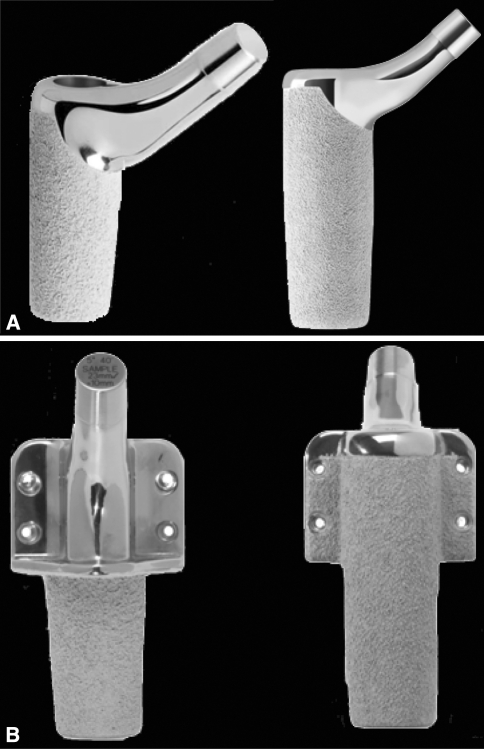
Data regarding need for trochanteric or extended trochanteric osteotomy, use of a structural graft, type of proximal and distal implant components used, and size of femoral heads with neck lengths used were recorded. The 122 revisions (100%) were performed using a conical distal stem (Fig. 1). The distribution between the proximal body types was 121 (99%) hips with the “cone” type (Fig. 2A) and one (0.8%) hip with the “calcar” type (Fig. 2B). Femoral head size was 22 mm in three (2%) hips, 28 mm in 19 (16%) hips, 32 mm in 45 (37%) hips, 36 mm in 49 (40%) hips, and 40 mm in six (5%) hips. The bearing surface was metal (cobalt-chromium) on highly crosslinked polyethylene (Crossfire®; Stryker Orthopaedics) in 105 (86%) hips and alumina ceramic on highly crosslinked polyethylene (Crossfire®) in 17 (14%) hips.
Fig. 1.
A photograph shows the distal “conical” stem from the Restoration Modular Stem® System. Reproduced with permission of Stryker Orthopaedics, Mahwah, NJ.
Fig. 2A–B.
Photographs show the Restoration Modular Stem® with (A) the “cone” proximal body (oblique and AP profiles) and (B) the “calcar” proximal body (medial and lateral profiles). Reproduced with permission of Stryker Orthopaedics, Mahwah, NJ.
The postoperative protocol for all patients was similar: early mobilization on the first day, walking assistance with walker and or crutches for 2 to 4 weeks, and then assistance with a cane for 2 to 4 more weeks. Supervised physical therapy was initiated at 4 weeks in an outpatient facility and lasted 4 weeks.
Patients were followed clinically and radiographically at 6 weeks, 6 months, and every 2 years thereafter. Functional assessment was performed using the SF-36 [22], the WOMAC Osteoarthritis Index [1], the Lower Extremity Activity Scale (LEAS) [21], and the Harris hip score (HHS) [6] on all patients preoperatively and postoperatively at 6 weeks, 6 months, and 2 years and/or at their latest followup. From the followup visits, clinic notes, and registry data, we recorded hip stability and other complications. Special emphasis was placed to determine stem-body junction fractures as seen with other modular stem systems.
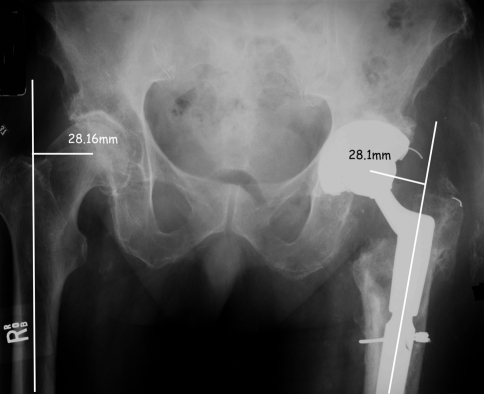
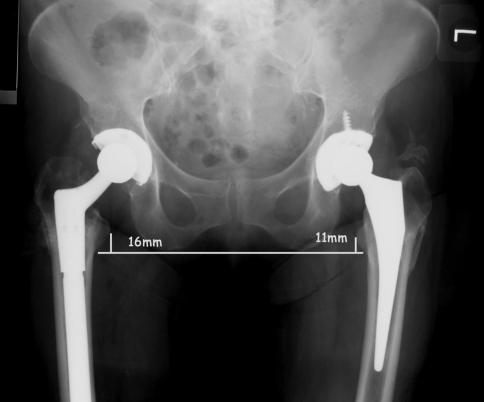
Two of us (WJH, CR) blinded to the clinical findings evaluated all AP and lateral radiographs of the hip and a third orthopaedic surgeon (MSA) ruled in the event of any discrepancies. Femoral bone defects were classified according to the classification of Paprosky et al. [16]. There were 69 (57%) hips classified as Paprosky Type I, 35 (29%) hips as Type II, nine (7%) hips as Type IIIA, eight (7%) hips as Type IIIB, and one (0.8%) hip as Type IV. Postoperative radiographic evaluation included assessment of biologic fixation around the femoral component, degree of subsidence and stability of the femoral component, offset restoration, and leg length equality. Radiographs were analyzed for spot welding along the sleeve and osteolytic lesions (appearance of a focal area of bone resorption evidenced as a cystic lesion not linear and at least 5 mm wide) classified according to Engh et al. [5]. The reference landmarks used to assess subsidence were the distance from the top of the modular body to the most proximal portion of the lesser trochanter. A vertical displacement of 5 mm or greater was considered indicative of subsidence [3]. The orientation of the component was classified as valgus, slight valgus (< 5° with respect to the neutral axis of the femoral canal), neutral, slight varus (< 5° with respect to the neutral axis of the femoral canal), or varus. Postoperative offset was measured on the AP view as the distance from the center of rotation of the femoral head to the axis of the femoral shaft at 90° (Fig. 3) and was considered corrected if it was within 2 mm of the opposite side. Leg length correction was also measured on the AP view (distance from lesser trochanter to a horizontal line based on the teardrop or, if not visible, on the ischial tuberosity) (Fig. 4) and was considered corrected if it was within 5 mm of the other side.
Fig. 3.
An AP radiograph illustrates assessment of offset restoration compared with the contralateral side.
Fig. 4.
An AP radiograph illustrates assessment of leg length equalization compared with the contralateral side.
The changes in SF-36, WOMAC, LEAS, and HHS were evaluated with the Wilcoxon signed-rank test. Offset and leg length were evaluated also with the Wilcoxon signed-rank test. All statistical analysis was performed using SPSS® 15.0 for Windows® (SPSS Inc, Chicago, IL).
Results
SF-36 outcome values improved from a preoperative mean of 68 (range, 60–77) to a mean of 82 (range, 68–92) at the latest followup. WOMAC outcome values improved from 19 (range, 16–21) to 8 (range, 4–12). LEAS outcome values improved from 7 (range, 6–14) to 13 (range, 11–17). HHS also improved from 62 (range, 58–69) to 77 (range, 72–84) with 108 patients (111 hips [91%]) achieving hip scores of more than 80 (no use of walking aid and nonpainful hips), although 10 patients (11 hips [9%]) scored less than 80. Mild hip pain was observed in 68 patients (72 hips [59%]).
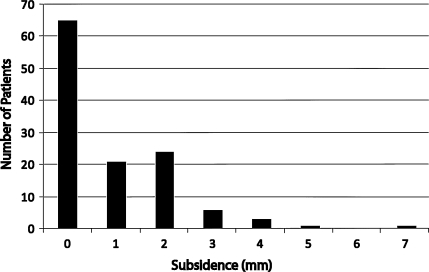
Femoral component position was achieved in 122 (100%) of the hips with only four (3%) of the stems being in slight varus (< 5° with respect to the neutral axis of the femoral canal). There was no evidence of osteolytic lesions around any stems. Subsidence of the femoral component was less than 5 mm in 122 (98%) hips and averaged 1 mm (range, 0–7 mm) (Fig. 5). One stem (0.8%) showed 5 mm of subsidence, and another stem (0.8%) showed 7 mm of subsidence; both had radiographic evidence of bone ingrowth fixation. As such, the mechanical failure rate of the stem was 0%.
Fig. 5.
A graph depicts the degree of subsidence in the entire cohort. Ninety percent of the patients in the cohort had 2 mm or less of subsidence.
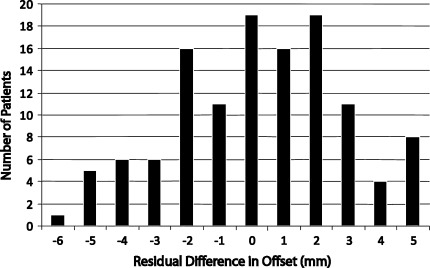
Offset restoration compared with the contralateral side was achieved in 81 (66%) of the hips (Fig. 6). In 19% of the patients, the offset was increased between 3 and 5 mm, and in 16% of the patients, the offset was undercorrected between −3 and −6 mm compared with the contralateral side.
Fig. 6.
A graph depicts the degree of residual difference of offset in the entire cohort. Offset restoration compared with the contralateral side was achieved in 66% of the cohort. The offset was overcorrected in 19% by 3 to 5 mm and undercorrected in 16% by −3 to −6 mm compared with the contralateral side.
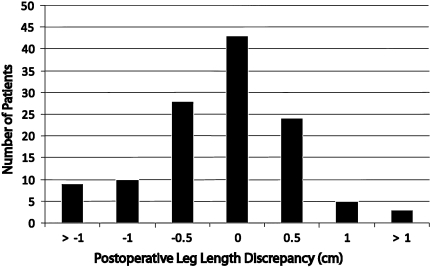
Leg length was corrected to within 5 mm in 95 (78%) hips (Fig. 7). However, when the preoperative leg length discrepancy was less than 2 cm, correction within 5 mm was achieved in 93% of the cases.
Fig. 7.
A graph depicts the degree of postoperative leg length discrepancy in the entire cohort. Leg length was corrected to within 5 mm in 78% of the cohort.
Reoperations of some sort were performed in 10 cases (8%). Dislocation occurred in four (3%) hips at a mean of 11 weeks (range, 6–105 weeks). Two dislocations were treated successfully with temporary bracing; the other two had surgery. Reoperation, with insertion of a constrained acetabular liner, was carried out in two (2%) hips to address recurrent instability as a result of lack of adequate soft tissue tension despite apparent proper component position. No further dislocations occurred in these patients.
Periprosthetic fracture occurred in two (2%) hips. In one case, a greater trochanter avulsion, which occurred 7 months postoperatively, was treated nonoperatively. In the other case, a Vancouver Type B1 [4] periprosthetic fracture, which occurred 6 weeks postoperatively, had open reduction and internal fixation. Other reoperations included hematoma drainage in three (2%) hips and deep infection in two (2%) hips (requiring incision and drainage in two hips); in one of the hips, the infection was controlled, but in the other, resection arthroplasty was required. We identified no component fractures. There were no acetabular failures in this series.
Discussion
Modular femoral stems are one option for the revision THA surgeon. Modularity allows surgeons to achieve offset restoration, leg length discrepancy correction, and stability independent of distal stem fixation. We evaluated functional outcomes (SF-36, WOMAC, LEAS, and HHS) with the use of a specific revision modular system and determined whether such a system achieved initial distal fixation, femoral offset restoration, leg length equalization, and hip stability. Furthermore, we evaluated any complications related to its use.
We acknowledge limitations of our study. First, we had only one cohort and cannot directly compare these findings with those with other devices. It was, however, a relatively large cohort in which all patients with failed femoral THA were treated with only one revision modular stem system. Second, we had only short- to midterm followup; however, our objectives were met because functional outcome, stem fixation, offset and leg length restoration, and stability are evaluated early. Third, although most of the femoral deformities were classified as Paprosky Types I and II (86%) and a modular stem may not be considered an option by some surgeons, the remainder of patients in our cohort was adequately treated with such a system.
Our observations demonstrate a modular femoral revision stem is useful when dealing with a variety of femoral revision situations. The first priority of the revision operation is to secure adequate initial fixation of the femoral component, which hopefully then translates into secure long-term fixation. Subsidence of the femoral component in this series was minimal with only two stems subsiding greater than 5 mm; however, both stems showed evidence of bone ingrowth fixation at the latest followup, and the subsidence degree in these stems did not result in hip instability (Fig. 5). The mechanical failure rate in this series was 0%. Although extensively coated nonmodular femoral stems are known to have a definite role in reconstruction of deficient femurs during revision THA [23], one series reporting the minimum 11-year followup of 170 such stems found aseptic loosening of the stem necessitating reoperation in six cases with an additional 4% of the stems being unstable [23]. Other modular stems [15, 19] have also demonstrated mechanical failure rates in the 4% range. The low mechanical failure rate experienced with the modular stem in this report most likely is a result of the ability of the surgeon to separate fixation from all other aspects of the revision procedure such as stability, offset, leg length, and ROM.
Offset and leg length restoration are important goals of the revision procedure and likely play a large role in the functional outcome of the procedure [12]. Very little information is available in the published literature regarding these two issues in the modular revision situation. Our bias is that the use of a modular stem where fixation is achieved independently of all other parameters allows the surgeon more flexibility in properly establishing the mechanical restoration of the hip mechanics. Both leg length and offset correction are critical parameters that need to be addressed. In this study, leg lengths were restored within 5 mm in 77% of patients and offset was restored within 2 mm in 65% of patients. There are no comparisons available within the recent published literature at this time.
Our data suggest a low dislocation rate (3%) compared with other studies with modular stems such as Park et al. [18] with a 5% dislocation rate, Ovesen et al. [15] with 6%, and Rodriguez et al. [19] with 10%. Dislocation can be minimized with modular stems. The offset changes with the size of the cone body for one thing. However, you can change offset by modifying cone body height in combination with neck length. You can maintain a specific leg length but have two different offsets by modulating cone body height (0, +10, etc) and neck length. The etiology of instability in this group of patients is multifactorial. Probably most importantly, these patients often have undergone multiple previous reconstructive procedures that have led to a compromised soft tissue envelope around the hip preventing optimal soft tissue tensioning. Some additional techniques may need to be implemented to further reduce the incidence of instability, including large femoral heads, selective use of constrained cups, and augmentation of the abductor mechanism repair whenever appropriate.
At a mean followup of 4 years with up to 7 years of followup, there have been no fractures of the modular prosthesis. This is a potential problem related to modularity that has limited the application of modular stems to the revision situation. Two other recent reports on modular revision stems [15, 19] both experienced a 1% stem fracture rate. The authors continue to stress the importance of bony support at the modular junction as a way of minimizing this serious complication.
Comparison of findings in our cohort to other studies in which modular stem systems have been used according to the type of femoral defect present is difficult. For instance, Lakstein et al. [11] used the classification of Saleh et al. [20], whereas Ovesen et al. [15] modified the classification of Saleh et al. [20] for their study, and Rodriguez et al. [19] used instead the Mallory [13] classification. Paprosky et al. [17] used their own classification, but their method of treatment was with extensively porous-coated nonmodular stems. Although our study appears to have had a higher percentage of patients with less severe defects, the initial fixation in the more severely damaged bone situations were equivalent to those achieved in the other studies.
We believe modular femoral components are an important tool in the surgeons’ armamentarium to address most problems encountered when facing a failed femoral component. Another advantage of modular components is the need for a smaller inventory in the operating room, which also decreases overall operating time. Longer-term followup clearly is needed to fully evaluate the ultimate role of these modular revision femoral stems.
Footnotes
One of the authors (JP) is a consultant for Stryker Orthopaedics (Mahwah, NJ) and has intellectual properties on SmarTech (Philadelphia, PA). One of the authors (WJH) is a consultant for and receives royalties from Stryker Orthopaedics.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 2.Berry DJ. Treatment of Vancouver B3 periprosthetic femur fractures with a fluted tapered stem. Clin Orthop Relat Res. 2003;417:224–231. doi: 10.1097/01.blo.0000096821.67494.f6. [DOI] [PubMed] [Google Scholar]
- 3.Callaghan JJ, Salvati EA, Pellicci PM, Wilson PD, Jr, Ranawat CS. Results of revision for mechanical failure after cemented total hip replacement, 1979 to 1982. A two to five-year follow-up. J Bone Joint Surg Am. 1985;67:1074–1085. [PubMed] [Google Scholar]
- 4.Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995;44:293–304. [PubMed] [Google Scholar]
- 5.Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;257:107–128. [PubMed] [Google Scholar]
- 6.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 7.Kolstad K, Adalberth G, Mallmin H, Milbrink J, Sahlstedt B. The Wagner revision stem for severe osteolysis. 31 hips followed for 1.5–5 years. Acta Orthop Scand. 1996;67:541–544. doi: 10.3109/17453679608997752. [DOI] [PubMed] [Google Scholar]
- 8.Kronick JL, Barba ML, Paprosky WG. Extensively coated femoral components in young patients. Clin Orthop Relat Res. 1997;344:263–274. doi: 10.1097/00003086-199711000-00026. [DOI] [PubMed] [Google Scholar]
- 9.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 10.Kurtz SM, Ong KL, Schmier J, Zhao K, Mowat F, Lau E. Primary and revision arthroplasty surgery caseloads in the United States from 1990 to 2004. J Arthroplasty. 2009;24:195–203. doi: 10.1016/j.arth.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 11.Lakstein D, Backstein D, Safir O, Kosashvili Y, Gross AE. Revision total hip arthroplasty with a porous-coated modular stem: 5 to 10 years followup. Clin Orthop Relat Res. 2010;468:1310–1315. doi: 10.1007/s11999-009-0937-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lecerf G, Fessy MH, Philippot R, Massin P, Giraud F, Flecher X, Girard J, Mertl P, Marchetti E, Stindel E. Femoral offset: anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop Traumatol Surg Res. 2009;95:210–219. doi: 10.1016/j.otsr.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 13.Mallory TH. Preparation of the proximal femur in cementless total hip revision. Clin Orthop Relat Res. 1988;235:47–60. [PubMed] [Google Scholar]
- 14.McGrory BJ, Bal BS, Harris WH. Trochanteric osteotomy for total hip arthroplasty: six variations and indications for their use. J Am Acad Orthop Surg. 1996;4:258–267. doi: 10.5435/00124635-199609000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Ovesen O, Emmeluth C, Hofbauer C, Overgaard S. Revision total hip arthroplasty using a modular tapered stem with distal fixation good short-term results in 125 revisions. J Arthroplasty. 2010;25:348–354. doi: 10.1016/j.arth.2008.11.106. [DOI] [PubMed] [Google Scholar]
- 16.Paprosky WG, Bradford MS, Younger TI. Classification of bone defects in failed prostheses. Chir Organi Mov. 1994;79:285–291. [PubMed] [Google Scholar]
- 17.Paprosky WG, Greidanus NV, Antoniou J. Minimum 10-year-results of extensively porous-coated stems in revision hip arthroplasty. Clin Orthop Relat Res. 1999;369:230–242. doi: 10.1097/00003086-199912000-00024. [DOI] [PubMed] [Google Scholar]
- 18.Park YS, Moon YW, Lim SJ. Revision total hip arthroplasty using a fluted and tapered modular distal fixation stem with and without extended trochanteric osteotomy. J Arthroplasty. 2007;22:993–999. doi: 10.1016/j.arth.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 19.Rodriguez JA, Fada R, Murphy SB, Rasquinha VJ, Ranawat CS. Two-year to five-year follow-up of femoral defects in femoral revision treated with the link MP modular stem. J Arthroplasty. 2009;24:751–758. doi: 10.1016/j.arth.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 20.Saleh KJ, Holtzman J, Gafni A, Saleh L, Davis A, Resig S, Gross AE. Reliability and intraoperative validity of preoperative assessment of standardized plain radiographs in predicting bone loss at revision hip surgery. J Bone Joint Surg Am. 2001;83:1040–1046. doi: 10.2106/00004623-200107000-00009. [DOI] [PubMed] [Google Scholar]
- 21.Saleh KJ, Mulhall KJ, Bershadsky B, Ghomrawi HM, White LE, Buyea CM, Krackow KA. Development and validation of a lower-extremity activity scale. Use for patients treated with revision total knee arthroplasty. J Bone Joint Surg Am. 2005;87:1985–1994. doi: 10.2106/JBJS.D.02564. [DOI] [PubMed] [Google Scholar]
- 22.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Weeden SH, Paprosky WG. Minimal 11-year follow-up of extensively porous-coated stems in femoral revision total hip arthroplasty. J Arthroplasty. 2002;17(Suppl 1):134–137. doi: 10.1054/arth.2002.32461. [DOI] [PubMed] [Google Scholar]
- 24.Whiteside LA, McCarthy DS, White SE. Rotational stability of noncemented total hip femoral components. Am J Orthop. 1996;25:276–280. [PubMed] [Google Scholar]