Abstract
Background
Proximal femoral replacement using a segmental modular system is one option for revision THA in the presence of severe bone loss or periprosthetic fracture. While many papers report function in these patients, they do not describe the quality of life.
Questions/purposes
We evaluated the quality of life in patients undergoing proximal femoral replacement using a segmental modular system for severe bone loss.
Patients and Methods
We retrospectively reviewed 63 patients undergoing complex revision THA using a modular replacement system for nonneoplastic conditions between April 1996 and June 2006. Average age was 73 years (range, 23–94 years). Twenty-one patients were lost to followup and six patients died before 2-year minimum followup. The remaining 36 patients were followed for an average of 3.2 years (range, 2–10 years). Study patients were matched by age-decade to a control group of patients undergoing conventional revision THA. At baseline, both groups were comparable with respect to age, comorbidities, and quality-of-life scores.
Results
At last followup, the modular system group showed improvement in WOMAC function, WOMAC pain, Oxford score, and the SF-12 mental component. Compared to the control group, the modular system group scored lower on WOMAC function and Oxford scores, but there were no differences in any other scores.
Conclusions
In patients with severely compromised bone stock, a segmental modular replacement system can improve the quality of life. Special attention should be given to the stability of the hip intraoperatively and a constrained acetabular liner should be used when the risk of postoperative dislocation is high.
Level of Evidence
Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Salvage of the hip with severe proximal femoral bone loss can be challenging [25]. With the ever-increasing number of hip arthroplasties performed worldwide and the advancing age of the target population, the arthroplasty surgeon is faced with more severe instances of this difficult situation. Numerous factors can contribute to the eventual loss of femoral bone stock, including osteolysis, infection, and periprosthetic fracture [16, 24, 26, 29].
When the proximal femur is severely deficient, treatment options become limited. With resection arthroplasty, patients have limited walking ability and function with a short limb [18]. Other surgical options include the use of a cemented or cementless long femoral stem, which intentionally bypasses the deficient proximal femur; impaction grafting with cement [8]; and the use of an allograft-prosthesis composite [10, 12]. The last option is a major undertaking in the elderly, often frail patient and requires a substantial period of protected weightbearing after the operation. Moreover, it may be followed by junctional nonunion, escape of the greater trochanter, and graft resorption [13].
The segmental modular replacement system (MRS), also known as a “megaprosthesis,” was developed for replacing the proximal femur in patients with neoplastic conditions [23]. The implants come in cemented and cementless versions and are modular to allow for replacement of the exact length of femur that is deficient. This implant has inherent advantages over some of the other options typically used to address severe proximal bone loss, such as the allograft-prosthesis system, including the availability of the implant and the avoidance of the risk of disease transmission associated with the use of allograft. Although a number of papers have addressed the functional outcomes of patients undergoing proximal femoral replacement for severe bone loss [15, 18, 23, 24], these do not specifically assess the quality-of-life outcomes of patients receiving the MRS.
Therefore, we (1) evaluated the functional and quality-of-life outcomes of MRS patients at a minimum of 2 years after the index surgery; (2) compared the outcomes to a matched group of patients undergoing conventional revision THA (RTHA); and (3) evaluated serial radiographs of MRS patients.
Patients and Methods
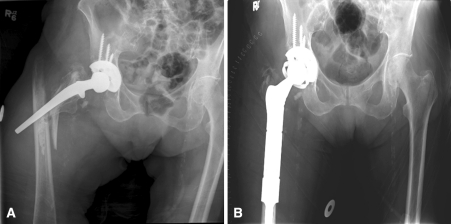
From our database, we identified 63 patients with nonneoplastic conditions who underwent complex RTHA using a segmental modular prosthesis (Modular Replacement System™, Stryker Orthopaedics, Mahwah, NJ) between April 1996 and June 2006. The indications for the use of the MRS were aseptic loosening in 27 patients (Fig. 1), a Vancouver Type B3 periprosthetic fracture [7] in 27 patients (Fig. 2), deep chronic infection in seven patients, and recurrent dislocation associated with severe bone loss in two patients. The study cohort consisted of 38 women and 25 men, with an average age of 73 years (range, 23–94 years) at the time of the index surgery. Medical records and radiographic data for all the patients were retrieved and analyzed retrospectively. Six patients died before the followup period had elapsed and 21 (33%) were lost to followup. While every effort was made to locate those lost to followup, most were elderly (median age of 81 years at time of surgery) and could not be reached. The remaining 36 patients were followed clinically and radiographically for at least 2 years postoperatively (average, 3.2 years; range, 2–10 years). All data were obtained from our divisional research database, medical records, and pre- and postoperative radiographs. Ethics board approval was obtained before the start of the study and validated clinical assessment tools were utilized.
Fig. 1A–B.
(A) A preoperative radiograph shows aseptic loosening of the right hip arthroplasty associated with severe proximal bone loss. (B) A postoperative radiograph shows the patient treated with a MRS femoral reconstruction and a constrained liner cemented into the preexisting well-fixed shell.
Fig. 2A–B.
(A) A preoperative radiograph shows a Vancouver Type B3 fracture with severe proximal femoral bone deficiency. (B) A postoperative radiograph shows the same patient treated with a MRS femoral reconstruction and a constrained liner cemented into the preexisting well-fixed shell.
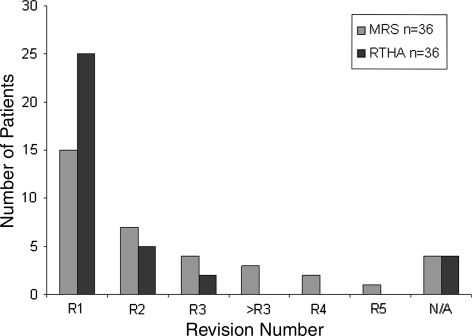
The 36 MRS patients were age-matched to 36 control patients who underwent conventional RTHA during the same time period and the scores for the two groups were compared preoperatively. At baseline, the WOMAC score, Oxford score, UCLA activity score, and the physical component of the SF-12 of the two groups were similar except for the mental component of SF-12, which was higher (p = 0.022) in the control group (Table 1). Patients in the MRS group underwent more prior operations than the control group: 42% of the MRS group had their index segmental replacement surgery as their first revision (Fig. 3). For 89% of the control group, the index RTHA was their first, second, or third revision, while 28% of the MRS patients were having at least their fourth, fifth, or even later revision.
Table 1.
Preoperative intergroup analysis between MRS and control groups
| Score | Mean value | p Value | |
|---|---|---|---|
| MRS | Control | ||
| WOMAC function | 39.9 | 49.8 | 0.170 |
| WOMAC stiffness | 44.9 | 47.6 | 0.699 |
| WOMAC pain | 41.5 | 48.9 | 0.212 |
| WOMAC global | 49.2 | 56.6 | 0.263 |
| Oxford | 34.9 | 43.2 | 0.126 |
| SF-12 physical | 30.8 | 32.3 | 0.558 |
| SF-12 mental | 38.9 | 48.9 | 0.022 |
| UCLA activity | 2.6 | 4.0 | 0.211 |
MRS = modular replacement system.
Fig. 3.
A graph shows the revision number distribution for the MRS group and the RTHA control group. R1, R2, etc = Revision 1, Revision 2, etc; N/A = not available.
The location and extent of bone loss was assessed on preoperative films. Bone loss was categorized using the classification system of Paprosky et al. [21, 22]. All patients had Type III-B defects (metaphyseal and diaphyseal damage with < 4 cm of diaphyseal bone available for femoral fixation).
In the case of a periprosthetic fracture, the type of the fracture was noted. All fractures in our series were of the Vancouver B3 type, where there is a loose stem and severe proximal femoral bone deficiency [7].
The surgical approach was anterolateral in 12 patients and posterolateral in 24. The proximal bone-deficient femur was split longitudinally and “peeled” off the failed implant. This remaining shell of bone was wrapped around the new femoral stem during wound closure. The Modular Replacement System™ was used in 34 patients, and its successor, the Global Modular Replacement System™, in two patients (both implants manufactured by Stryker). This prosthesis is modular in such a way that a variable length of the implant can be used depending on the length of the deficient bone fragment. The prosthesis has a roughened surface on the body segments to promote soft tissue attachment and potential bone ingrowth. The stem segment is of two surface designs to permit the options of cemented or cementless fixation and is of varied diameters for the same purpose. Thirty-three patients had cemented fixation, and three patients had a cementless stem. Simplex-T® cement (Stryker) with tobramycin (1 g/41 g cement powder) was used in 28 cases, and Palacos® (Zimmer, Inc, Warsaw, IN) with gentamicin (0.5 g/40 g cement powder) was used in five. The femoral canal was prepared to permit contemporary cementing techniques, including careful canal preparation and plugging when possible, vacuum cement mixing, retrograde filling, proximal sealing, and pressurization. The choice of acetabular liner was at the surgeon’s discretion. A constrained liner was used in 23 patients initially.
Patients were mobilized with touch weightbearing on the affected limb for 6 weeks (use of a walker). This was followed by a period of 50% partial weightbearing for another 6 weeks. The patients received supervised physical therapy care while in the hospital and after they were discharged home or to a nursing facility.
Patients were seen at 2, 6, and 12 weeks, 6 months, and 1 year postoperatively and annually thereafter. At each clinical visit, patients were examined for ability to ambulate, muscle strength, and stability of the hip with ROM, and standard AP and crosstable lateral radiographs were obtained.
Functional and quality-of-life assessment tools utilized included the WOMAC Osteoarthritis Index [2], SF-12 [27], Oxford-12 [20], and the UCLA activity level [28]. For this study, the WOMAC and Oxford-12 scores were normalized to a score that is out of 100, with lower values indicating a worse outcome. The scores were recorded preoperatively and at the minimum 2-year followup mark. Charnley class [5] and the satisfaction score of Mahomed et al. [17] were recorded at followup as well.
Serial AP and crosstable lateral radiographs of the operated hip were available for 31 patients, and they were evaluated in detail. On postoperative serial radiographs, one of the authors (MMA), who was not a treating surgeon, divided the femur into seven zones as described by Gruen et al. [11] and the acetabulum into three zones as described by DeLee and Charnley [6] and visually evaluated for cavitary or segmental bone loss and the presence or absence of continuous progressive lucent lines (2-mm thickness) on subsequent radiographs.
Descriptive statistics were run for all variables at baseline and at followup. Intragroup comparison was performed (baseline to followup) using one-sample t tests on common portions of the dataset to provide p values. For the intergroup comparison, matching was on patient age-decade. Two-sample t tests were used to compare the two cohorts (MRS and control) for age at surgery, WOMAC (function, stiffness, pain, global), Oxford, SF-12 (physical, mental), and UCLA activity level at baseline and at followup. In addition, for the assessment at followup, comparison of satisfaction (pain, function, recreation, results, overall) was performed using two-sample t tests. Chi square tests were used to test for differences in Charnley class between the cohorts (at followup only). Statistical analysis was performed with SAS® 9.1.3 statistical analysis software (SAS Institute Inc, Cary, NC).
Results
At followup, patients in the MRS group showed improvement on WOMAC pain (p = 0.007), Oxford score (p = 0.003), and the mental component of the SF-12 (p = 0.030) (Table 2). Similarly, patients in the control group showed improvement on WOMAC scores (p = 0.006), Oxford score (p = 0.000), and the physical component of the SF-12 (p = 0.001) (Table 3).
Table 2.
MRS intragroup analysis at latest followup
| Score | Mean value | p Value | |
|---|---|---|---|
| Preoperative | Followup | ||
| WOMAC function | 39.9 | 56.3 | 0.056 |
| WOMAC stiffness | 44.9 | 62.9 | 0.157 |
| WOMAC pain | 41.5 | 71.3 | 0.007 |
| WOMAC global | 49.2 | 62.2 | 0.168 |
| Oxford | 34.9 | 54.9 | 0.003 |
| SF-12 physical | 30.8 | 37.0 | 0.220 |
| SF-12 mental | 38.9 | 50.8 | 0.030 |
| UCLA activity | 2.6 | 3.9 | 0.528 |
MRS = modular replacement system.
Table 3.
Control group intragroup analysis at latest followup
| Score | Mean value | p Value | |
|---|---|---|---|
| Preoperative | Followup | ||
| WOMAC function | 49.8 | 70.0 | 0.000 |
| WOMAC stiffness | 47.6 | 67.0 | 0.002 |
| WOMAC pain | 48.9 | 77.6 | 0.000 |
| WOMAC global | 56.6 | 71.5 | 0.006 |
| Oxford | 43.2 | 70.3 | 0.000 |
| SF-12 physical | 32.3 | 37.8 | 0.001 |
| SF-12 mental | 48.9 | 52.5 | 0.102 |
| UCLA activity | 4.0 | 4.7 | 0.182 |
Patients in the control group scored higher on WOMAC function (p = 0.027) and Oxford scores (p = 0.009) (Table 4) than the MRS group. However, there were no differences in any of the other WOMAC components, the SF-12, satisfaction, or UCLA scores.
Table 4.
Intergroup analysis of MRS and control groups at latest followup
| Score | Mean value | p Value | |
|---|---|---|---|
| MRS | Control | ||
| WOMAC function | 56.3 | 70.0 | 0.027 |
| WOMAC stiffness | 62.9 | 67.0 | 0.530 |
| WOMAC pain | 71.3 | 77.6 | 0.347 |
| WOMAC global | 62.2 | 71.5 | 0.122 |
| Oxford | 54.9 | 70.3 | 0.009 |
| SF-12 physical | 37.0 | 37.8 | 0.811 |
| SF-12 mental | 50.8 | 52.5 | 0.553 |
| Satisfaction pain | 81.3 | 84.8 | 0.628 |
| Satisfaction function | 62.7 | 68.6 | 0.530 |
| Satisfaction recreation | 55.6 | 68.7 | 0.183 |
| Satisfaction results | 68.0 | 83.8 | 0.072 |
| Satisfaction all | 67.0 | 76.5 | 0.217 |
| UCLA activity | 3.9 | 4.7 | 0.070 |
MRS = modular replacement system.
The immediate postoperative radiographs showed the femoral and acetabular components to be well positioned. The alignment of the femoral stems in the coronal plane was within 5° of neutral. The cups were positioned in 40° to 50° of abduction. At latest followup, there was a nonprogressive radiolucent line measuring less than 2 mm at Zone 3 of three acetabular components and at Zones 3, 4, and 5 of the stem of four femoral components. None of the implants were deemed radiographically loose.
Six MRS patients (17%) had a complication related to the index operation. The most common being instability, as three of 36 patients (8%) suffered at least one dislocation. Two of the three patients who had a dislocation had a nonconstrained liner at the time of the index procedure. The third patient had a constrained liner, but the constraining ring failed and the hip subsequently dislocated. The three patients underwent limited rerevision to a constrained variant, with a successful outcome. Further surgery was not required. Cup pullout was seen in one patient (3%), which occurred 3 years after the index surgery. The liner in this case was constrained. The patient underwent reconstruction of the acetabular component. Unfortunately, the patient developed a subsequent infection and eventually ended up with a nonfunctional resection arthroplasty. Infection was seen in one other patient (3%) who was successfully treated with débridement, implantation of an antibiotic depot around the implant, prolonged antibiotic therapy, and retention of the components. Progressive osteolysis and loosening of both the acetabular and femoral components were seen in one patient (3%). The patient was not medically fit to undergo any form of reconstruction and underwent revision to a nonfunctional resection arthroplasty.
Discussion
Proximal femoral bone loss continues to be a challenging condition for the arthroplasty surgeon, which is compounded by the fact that most of these patients have already had multiple hip operations, have severe abductor and possible acetabular bone stock deficiency, and are commonly elderly with preexisting comorbidities. If substitution of the proximal femur is chosen as the preferred treatment, the options include the use of a proximal allograft-prosthetic composite or proximal femoral replacement such as a MRS. The use of a conventional modular revision stem is an option; however, reattachment of the abductor mechanism can be compromised and there are no long-term results reported for this type of reconstruction [3, 4]. We evaluated whether the quality of life improves for patients undergoing proximal femoral replacement using a segmental modular system for severe bone loss.
Our study is subject to certain limitations. First, the number of patients is relatively small because this procedure is uncommon even in a tertiary care center such as the one where the study was conducted. Second, many of the patients in the original sample were eventually lost to followup despite extensive efforts to locate them. We attribute this loss to followup to their already advanced age at the time of surgery (median age, 81 years). Third, there is disparity in the number of hip revisions between patients in the MRS group and patients in the control group. Patients in the MRS group were more likely to have had multiple revisions and were expected to have more deficient bone stock, compromised abductor mechanism, and decreased functional reserve, which makes our control group not the ideal comparison group (Fig. 3).
Our data suggest proximal femoral replacement using the MRS in patients with severe proximal femoral bone deficiency led to functional and quality-of-life improvements as measured by several validated scores. We believe this study is a valuable contribution to the literature, which is lacking in regard to quality-of-life assessment in MRS patients.
The degree of improvement in pain for MRS patients was comparable to that achieved after RTHA using a conventional hip revision system. However, the improvement in function, while present, was less dramatic than that observed in the control group. The control group fared better as measured by WOMAC function and Oxford scores. This might be, at least partially, due to the fact that MRS patients, on average, had undergone a larger number of prior revisions as noted above.
Radiographs were available for 31 MRS patients (86%), none of whom showed evidence of radiographic loosening at the time of latest followup. Our findings are consistent with those of the study of Parvizi et al. [24], which, like our study, had a small sample size (n = 48) and a minimum 2-year followup.
The most common complication reported after proximal femoral replacement was dislocation [14, 15, 18, 30]. In our study, three of the 36 patients (8.3%) had a dislocation. Likewise, dislocation occurred in six of 43 patients (14%) in one study [24], in three of 18 (16.7%) in another [30], and in two of four (50%) in another series [15]. This degree of instability is higher than that encountered after RTHA using a conventional implant [1, 19] but is comparable to that seen after the use of an allograft-prosthesis composite [9].
Our data suggest the MRS is a reasonable option for hip salvage in the setting of severe proximal femoral bone loss. Patients treated with this implant had improvement in function and quality of life. Some authors have conducted studies describing the functional outcome after this kind of reconstruction [15, 23, 24], but none assessed the patients’ postoperative quality of life. Dislocation rates were high and we suggest using a constrained cup in all cases where there is adequate fixation of the acetabular shell.
Acknowledgment
We thank Daphné Savoy for her assistance in the preparation of this manuscript.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent was obtained for participation in the study.
References
- 1.Alberton GM, High WA, Morrey BF. Dislocation after revision total hip arthroplasty: an analysis of risk factors and treatment options. J Bone Joint Surg Am. 2002;84:1788–1792. [PubMed] [Google Scholar]
- 2.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 3.Berry DJ. Treatment of Vancouver B3 periprosthetic femur fractures with a fluted tapered stem. Clin Orthop Relat Res. 2003;417:224–231. doi: 10.1097/01.blo.0000096821.67494.f6. [DOI] [PubMed] [Google Scholar]
- 4.Chandler H, Clark J, Murphy S, McCarthy J, Penenberg B, Danylchuk K, Roehr B. Reconstruction of major segmental loss of the proximal femur in revision total hip arthroplasty. Clin Orthop Relat Res. 1994;298:67–74. [PubMed] [Google Scholar]
- 5.Charnley J. The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg Br. 1972;54:61–76. [PubMed] [Google Scholar]
- 6.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 7.Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995;44:293–304. [PubMed] [Google Scholar]
- 8.Gie GA, Linder L, Ling RS, Simon JP, Slooff TJ, Timperley AJ. Impacted cancellous allografts and cement for revision total hip arthroplasty. J Bone Joint Surg Br. 1993;75:14–21. doi: 10.1302/0301-620X.75B1.8421012. [DOI] [PubMed] [Google Scholar]
- 9.Gross AE. Allograft prosthetic composite. In: Barrack RL, Rosenberg AG, editors. The Hip. 2. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. pp. 385–396. [Google Scholar]
- 10.Gross AE, Hutchison CR. Proximal femoral allografts for reconstruction of bone stock in revision arthroplasty of the hip. Orthop Clin North Am. 1998;29:313–317. doi: 10.1016/S0030-5898(05)70329-1. [DOI] [PubMed] [Google Scholar]
- 11.Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 12.Haddad FS, Garbuz DS, Masri BA, Duncan CP. Structural proximal femoral allografts for failed total hip replacements. J Bone Joint Surg Br. 2000;82:830–836. doi: 10.1302/0301-620X.82B6.10485. [DOI] [PubMed] [Google Scholar]
- 13.Haddad FS, Masri BA, Garbuz DS, Duncan CP. Femoral bone loss in total hip arthroplasty: classification and preoperative planning. Instr Course Lect. 2000;49:83–96. [PubMed] [Google Scholar]
- 14.Haentjens P, Boeck H, Opdecam P. Proximal femoral replacement prosthesis for salvage of failed hip arthroplasty: complications in a 2–11 year follow-up study in 19 elderly patients. Acta Orthop Scand. 1996;67:37–42. doi: 10.3109/17453679608995606. [DOI] [PubMed] [Google Scholar]
- 15.Johnsson R, Carlsson A, Kisch K, Moritz U, Zetterstrom R, Persson BM. Function following mega total hip arthroplasty compared with conventional total hip arthroplasty and healthy matched controls. Clin Orthop Relat Res. 1985;192:159–167. [PubMed] [Google Scholar]
- 16.Klein GR, Parvizi J, Rapuri V, Wolf CF, Hozack WJ, Sharkey PF, Purtill JJ. Proximal femoral replacement for the treatment of periprosthetic fractures. J Bone Joint Surg Am. 2005;87:1777–1781. doi: 10.2106/JBJS.D.02420. [DOI] [PubMed] [Google Scholar]
- 17.Mahomed N, Sledge C, Daltroy L, Fossel A, Katz J. Self-administered satisfaction scale for joint replacement arthroplasty. J Bone Joint Surg Br. 1998;80(Suppl 1):9. [Google Scholar]
- 18.Malkani A, Seti’ecerri J, Sim F, Chao E, Wallrichs S. Long-term results of proximal femoral replacement for non-neoplastic disorders. J Bone Joint Surg Br. 1995;77:351–356. [PubMed] [Google Scholar]
- 19.Morrey BF. Results of reoperation for hip dislocation: the big picture. Clin Orthop Relat Res. 2004;429:94–101. doi: 10.1097/01.blo.0000150318.27723.8c. [DOI] [PubMed] [Google Scholar]
- 20.Murray DW, Fitzpatrick R, Rogers K, Pandit H, Beard DJ, Carr AJ, Dawson J. The use of the Oxford hip and knee scores. J Bone Joint Surg Br. 2007;89:1010–1014. doi: 10.1302/0301-620X.89B8.19424. [DOI] [PubMed] [Google Scholar]
- 21.Paprosky WG, Greidanus NV, Antoniou J. Minimum 10-year-results of extensively porous-coated stems in revision hip arthroplasty. Clin Orthop Relat Res. 1999;369:230–242. doi: 10.1097/00003086-199912000-00024. [DOI] [PubMed] [Google Scholar]
- 22.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty: a 6-year follow-up evaluation. J Arthroplasty. 1994;9:33–44. doi: 10.1016/0883-5403(94)90135-X. [DOI] [PubMed] [Google Scholar]
- 23.Parvizi J, Sim FH. Proximal femoral replacements with megaprostheses. Clin Orthop Relat Res. 2004;420:169–175. doi: 10.1097/00003086-200403000-00023. [DOI] [PubMed] [Google Scholar]
- 24.Parvizi J, Tarity TD, Slenker N, Wade F, Trappler R, Hozack WJ, Sim FH. Proximal femoral replacement in patients with non-neoplastic conditions. J Bone Joint Surg Am. 2007;89:1036–1043. doi: 10.2106/JBJS.F.00241. [DOI] [PubMed] [Google Scholar]
- 25.Sim FH, Chao EY. Hip salvage by proximal femoral replacement. J Bone Joint Surg Am. 1981;63:1228–1239. [PubMed] [Google Scholar]
- 26.Springer BD, Berry DJ, Lewallen DG. Treatment of periprosthetic femoral fractures following total hip arthroplasty with femoral component revision. J Bone Joint Surg Am. 2003;85:2156–2162. doi: 10.2106/00004623-200311000-00015. [DOI] [PubMed] [Google Scholar]
- 27.Ware JE, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Zahiri CA, Schmalzried TP, Szuszczewcz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890–895. doi: 10.1016/S0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]
- 29.Zaki SH, Sadiq S, Purbach B, Wroblewski BM. Periprosthetic femoral fractures treated with a modular distally cemented stem. J Orthop Surg (Hong Kong) 2007;15:163–166. doi: 10.1177/230949900701500207. [DOI] [PubMed] [Google Scholar]
- 30.Zehr RJ, Enneking WF, Scarborough MT. Allograft-prosthesis composite versus megaprosthesis in proximal femoral reconstruction. Clin Orthop Relat Res. 1996;322:207–223. doi: 10.1097/00003086-199601000-00026. [DOI] [PubMed] [Google Scholar]