Abstract
Background
TKA is commonly performed to treat advanced inflammatory and degenerative knee arthritis. With increasing use in younger patients, it is important to define the best practices to enhance clinical performance and implant longevity.
Questions/purposes
We systematically reviewed the literature to assess: (1) how TKAs perform in young patients; (2) whether the TKA is a durable procedure for young patients, and (3) what guidance the literature outlines for TKA in young patients.
Methods
We searched the literature between 1950 and 2009 for all studies reporting on TKAs for patients younger than 55 years that documented clinical and radiographic assessments with a minimum 2-year followup. Thirteen studies, reporting on 908 TKAs performed for 671 patients, met these criteria.
Results
Mean Knee Society clinical and functional scores increased by 47 and 37 points, respectively. Implant survivorship was reported between 90.6% and 99% during the first decade and between 85% and 96.5% during the second decade of followup. The literature does not direct specific techniques for TKA for young patients.
Conclusions
TKA provides surgeon-measured clinical and functional improvements with a moderate increase in second-decade implant failures. Improvements in study design and reporting will be beneficial to guide decisions regarding implant selection and surgical technique.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
TKAs commonly are performed to treat advanced inflammatory and degenerative knee arthritis. Long-term followup studies have suggested implant survivorship of as much as 96% between 15 and 20 years after surgery [20, 23, 31]. Although the majority of TKAs performed in the United States have been for patients older than 65 years, a substantial number of TKAs are being performed on younger patients [17]. Kurtz et al. reviewed the National Inpatient Sample from 2006 and reported approximately 70,000 TKAs performed annually for patients younger than 55 years [18]. Extrapolating trends of arthroplasties performed during the past decade, Kurtz et al. projected that patients younger than 65 years will become the majority treated with TKAs during the next two decades and that up to one million TKAs may be performed for patients younger than 55 years by 2030 [18]. W-Dahl et al. reported that the trend toward TKA use is not confined to the United States, with similar increases noted in the Swedish Knee Arthroplasty and Australian Joint Replacement registries [36].
The increase in TKAs performed on younger patients suggests that surgeons and patients either expect durability for the reconstructed knee or improvement in patient employability or quality of life that offset the potential for early revision surgery. However, recent studies reporting data from community, academic, and national registries have suggested higher TKA revision rates occur in this patient group [13, 15, 29, 36].
Therefore, this systematic review was performed to assess (1) how TKAs perform in young patients, (2) whether the TKA is a durable procedure for young patients, and (3) what guidance the literature provides for implant selection or surgical technique specifically for TKAs performed in patients younger than 55 years.
Materials and Methods
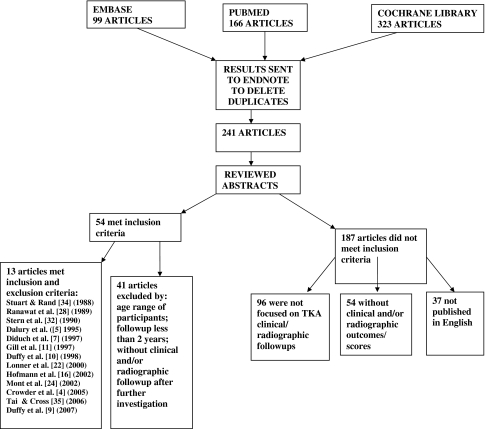
We searched PubMed, Cumulative Index to Nursing & Allied Health (CINAHL), OVID, Medline, and the Cochrane Library for articles published between January 1950 and May 2008. We also searched EMBASE for articles published between January 1980 and May 2008. The databases initially were queried on May 8, 2008. All of the databases were searched again on November 9, 2009, to identify articles that had been missed during the initial review. Database search terms included: “total knee arthroplasty,” “knee replacement,” “young patient,” and “55 years.” We also hand-searched the following journals for articles published between February 2009 and November 2009: Clinical Orthopaedics and Related Research, The Journal of Bone and Joint Surgery (American and British editions), and The Journal of Arthroplasty. Bibliographies of identified studies also were searched. A total of 241 articles were identified and each abstract underwent review by two of the authors. (SE, GP). We included only studies that were peer-reviewed; published in English; reported clinical and radiographic results of TKAs; and consisted exclusively of patients younger than 55 years with a minimum of 2 years followup. Articles were excluded if they were surgical technique descriptions; did not adequately describe clinical and radiographic results; treated conditions other than osteoarthritis, rheumatoid arthritis, or posttraumatic arthritis; or reported less than 2-year minimum followup data. Of the 241 articles, 54 met first-pass review and underwent a detailed, full-text review. After the detailed, full-text review, 13 articles remained that met all inclusion criteria (Fig. 1).
Fig. 1.
A flow diagram outlines the process and results of our literature search for TKA in patients younger than 55 years.
Two authors (SE, JK) independently performed quality appraisal of the included studies. This included assessment for selection and reporting biases that may have affected the quality of conclusions made by the study authors. Examples of selection bias included the use of fixation methods or implant design on the basis of intraoperative bone quality assessment, patient age, or anticipated activity level. Reporting biases included favorable documentation of clinical performance while minimizing the impact of revision surgeries other than total component revision (Table 1). Patient characteristics and study demographic information were noted (Table 2). Study design and levels of evidence, clinical and functional scoring, radiographic assessments, definitions of clinical failure, revision rates, and reported component survivorship also were identified (Table 3). We assessed for the use of statistical tools, including power analysis and confidence intervals; however, only basic statistical reporting of group mean, range, and standard deviation was performed for the majority of studies. Differences noted between the reviewers were discussed and consensus was reached regarding the item in question. Criteria developed by the STROBE statement (Strengthening the Reporting of Observational Studies in Epidemiology) were used to assess the quality of reporting for the included studies (Table 4). Although the STROBE criteria do not assess the quality of research, they provide a perspective on the quality of reporting that may be useful in the process of critically appraising published studies [33].
Table 1.
Study biases and limitations identified during systematic review
| Study | Knees/patients | Selection bias/reporting bias/limitations |
|---|---|---|
| Stuart and Rand [34] | 44/26 | 13/26 patients had significant involvement in other joints; authors were unable to determine functional score improvement |
| Ranawat et al. [28] | 90/60 | Revisions performed for 8% of patients with RA; 9% of OA patients documented to have radiographic or clinical failure; authors noted 97.7% with good or excellent clinical results |
| Stern et al. [32] | 68/50 | 4 knees revised for patellar component failures (5.9%); all results reported as good or excellent |
| Dalury et al. [6] | 103/67 | 16/103 (16%) unavailable for followup; predominantly rheumatoid arthritis/juvenile rheumatoid arthritis |
| Diduch et al. [7] | 103/80 | 9% of patients not available for followup; 8% revised; 97% good or excellent clinical results reported |
| Gill et al. [11] | 72/60 | Diverse diagnoses; 12 patients (16%) not available; Knee Society scores reported as increased to 97 points; 78% of patients reported to have good or excellent results |
| Duffy et al. [10] | 74/54 | 7 revision procedures (9.5%); mean followup 13 years; authors report survival of 95% at 15 years |
| Lonner et al. [22] | 32/32 | Authors excluded 12 patients who had knee replacements with an implant that failed in 9/12; 6 different component designs were used; mixture of techniques (cemented, cementless, hybrid); 4 radiographically loose (12.5%) at 8 years; authors reported 90.6% survivorship at 8 years |
| Hofmann et al. [15] | 75/57 | Diverse surgical technique; 57% posterior stabilized design/43% cruciate retaining design; decision for cementless fixation based on surgeon assessment of bone quality; 69% patellar resurfacing; clinical score 97 (range, 85–100); 14 patients had revision surgery (18.6%) without adversely impacting Knee Society clinical score |
| Mont et al. [24] | 30/30 | Diverse fixation technique; hybrid > cemented > cementless; no reporting bias identified |
| Crowder et al. [4] | 47/32 | 6 revisions performed between 17–23 years postoperative (12.8%); 20-year survivorship reported as 93.7% |
| Tai and Cross [35] | 118/81 | Followup reported for 118/119 enrolled patients No selection or reporting biases identified |
| Duffy et al. [9] | 52/42 | No selection or reporting biases identified |
Table 2.
Participant demographics for studies of TKA in patients 55 years or younger
| Study | Years of investigation | Mean followup | Percent followup | Mean age (years) (range) | Male:female | Unique features of cohort | Number of knees with a specific diagnosis | Previous surgery (%) |
|---|---|---|---|---|---|---|---|---|
| Stuart and Rand [34] | 1978–1986 | 5 years | 100% | 29 (19–39) | 20:6 | RA and JRA | 13 JRA 13 RA |
8 (18%) |
| Ranawat et al. [28] | 1974–1982 | 6.1 years | 97% | 48.7 (42.4–55) | 48:14 | RA > OA | 17 OA 73 RA |
NA |
| Stern et al. [32] | 1979–1987 | 6.2 years | 86% | 51 (36–55) | 36:14 | OA/PT only | 68 OA | 25 (37%) |
| Dalury et al. [5] | 1978–1984 | 7.2 years | 83% | 36 (20–45) | 38:18 | JRA included | 50 RA 25 JRA 11 other diagnosis |
NA |
| Diduch et al. [7] | 1977–1992 | 8 years | 95% | 51 (22–55) | 29:55 | OA only | 103 OA | 63 (58%) |
| Gill et al. [11] | 1977–1989 | 9.9 years | 96% | 50.7 (30–55) | 30:20 | OA > RA | 37 OA 29 RA 2 ankylosing spondylosis |
NA |
| Duffy et al. [10] | 1977–1983 | 13 years | 91% | 43 (22–55) | 35:19 | Primarily RA | 47 RA 12 OA 6 PT 3 osteonecrosis 2 hemophilia 5 other |
9 (16)% |
| Lonner et al. [22] | 1982–1984 | 7.9 years | 73% | 35 (22–40) | 13:19 | Workers’ compensation included | 21 OA 11 posttraumatic |
26 (82%) |
| Hofmann et al. [16] | 1986–1998 | 9.3 years | 100% | 42 (31–50) | 33:24 | Posttraumatic > OA/RA | 27 posttraumatic 17 OA 19 RA |
NA |
| Mont et al. [24] | 1991–1995 | 7.2 years | 88% | 43 (31–50) | 17:13 | OA | 29 OA 1 PVNS |
NA |
| Crowder et al. [4] | 1977–1983 | 20 years | 91% | 43 (24–55) | 24:8 | RA | 32 RA | NA |
| Tai and Cross [35] | 1992–2000 | 7.9 years | 99% | 50.7 (32–55) | 38:43 | OA/PT only | 92 OA 26 posttraumatic |
9 (11.1%) |
| Duffy et al. [9] | 1987–1994 | 12 years | 100% | 53 (29–55) | 24:18 | OA/PT only | 52 OA/posttraumatic | 28 (54%) |
* NA = data not available; OA = osteoarthritis; RA = rheumatoid arthritis; JRA = juvenile rheumatoid arthritis; PT = posttraumatic arthritis; PVNS = pigmented villonodular synovitis
Table 3.
Surgical techniques and outcomes in studies of TKAs in patients 55 years and younger
| Study | Level of evidence | Change in clinical score | Change in KS functional score | Radiographic lucency | Reported failure mechanisms | Revision surgeries | Component survival rate |
|---|---|---|---|---|---|---|---|
| Stuart and Rand [34] | IV Retrospective case series | 32 points* | Not reported | 18% | Patellar revision | 2 | 100%—5 years |
| Ranawat et al. [28] | IV Retrospective case series | 41.3 points† | Not reported | 30% | Global radiolucency | 2 | 96%—10 years |
| Stern et al. [32] | IV Retrospective case series | 37 points† | Not reported | 22% | Patellar revision | 4 | 94%—6.2 years |
| Dalury et al. [6] | IV Retrospective case series (prospectively collected) | 56 points† | 41 points | 30% | Patellar fracture or loosening | 3 | Not reported |
| Diduch et al. [7] | IV Retrospective case series (prospectively collected) | 37 points† | Not reported | 9% | Patellar revision | 7 | 87%—18 years |
| Gill et al. [11] | IV Mixed prospective/retrospective case series | 37.4 points† | Not reported | 22% | Infection/aseptic loosening | 2 | 96.5%—18 years |
| Duffy et al. [10] | IV Retrospective case series | 48 points† | 15 points | None | Instability/patellar fracture | 7 | 99%—10 years |
| Lonner et al. [22] | IV Retrospective case series | 41 points† | 35 points | None | Wear/loosening | 3 | 90.6%—8 years |
| Hofmann et al. [16] | IV Retrospective case series | 31 points† | 39 points | None | None reported | 0 | Not reported |
| Mont et al. [24] | IV Retrospective case series | 40 points† | Not reported | 20% | Pain | 1 | Not reported |
| Crowder et al. [4] | IV Retrospective case series | 48 points† | Not reported | None | Wear/osteolysis | 6 | 100%—15 years |
| Tai and Cross [35] | IV Retrospective case series | 47 points† | 26 points | None | None reported | 2 | 97.5%—12 years |
| Duffy et al. [9] | IV Retrospective case series | 56 points† | 26 points | 3.8% | Instability/wear/osteolysis | 11 | 85%—15 years |
* Hospital for Special Surgery; †Knee Society clinical score.
Table 4.
Analysis of studies of TKAs in patients younger than 55 years using STROBE criteria
| Category | Number | Item summary | Number of studies | Percentage of studies |
|---|---|---|---|---|
| Title | 1a | Indicate the study’s design with a commonly used term in the title or the abstract | 7 | 54% |
| Abstract | 1b | Provide in the abstract an informative and balanced summary of what was done and what was found | 12 | 92% |
| Introduction | 2 | Explain the scientific background and rationale for the investigation being reported | 12 | 92% |
| Background | 3 | State specific objectives, including any prespecified hypotheses | 1 | 8% |
| Methods | 4 | Present key elements of study design early in the paper | 10 | 77% |
| 5 | Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, followup, and data collection | 11 | 85% | |
| 6a | Give the eligibility criteria and the sources and methods of selection of participants; describe methods of followup | 12 | 92% | |
| 6b | Give matching criteria and numbers of [patients] treated and untreated | 3 | 23% | |
| 7 | Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers; give diagnostic criteria, if applicable | 9 | 69% | |
| 8 | For each variable of interest, give sources of data and details of methods of assessment (measurement); describe comparability of assessment methods if there is more than one group | 0 | 0% | |
| 9 | Describe any efforts to address potential sources of bias | 0 | 0% | |
| 10 | Explain how the study size was arrived at | 6 | 46% | |
| 11 | Explain how quantitative variables were handled in the analyses; if applicable, describe which groupings were chosen, and why | 4 | 31% | |
| 12a | Describe all statistical methods, including those used to control for confounding | 2 | 15% | |
| 12b | Describe any methods used to examine subgroups and interactions | 1 | 8% | |
| 12c | Explain how missing data were addressed | 1 | 8% | |
| 12d | If applicable, explain how loss to followup was addressed | 1 | 8% | |
| 12e | Describe any sensitivity analyses | 0 | 0% | |
| Results | 13a | Report the numbers of individuals at each stage of the study (eg, the numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing followup, and analyzed) | 3 | 23% |
| 13b | Give reasons for nonparticipation at each stage | 0 | 0% | |
| 13c | Consider use of a flow diagram | 0 | 0% | |
| 14a | Give characteristics of study participants and information regarding exposures and potential confounders | 13 | 100% | |
| 14b | Indicate the number of participants with missing data for each variable of interest | 0 | 0% | |
| Descriptive data | 14c | Summarize followup time (eg, average and total amount) | 11 | 85% |
| Outcome data | 15 | Report number of outcome events or summary measures with time | 8 | 62% |
| Main results | 16a | Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision | 3 | 23% |
| 16b | Report category boundaries when continuous variables were categorized | 2 | 15% | |
| 16c | If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time | 1 | 8% | |
| Other analyses | 17 | Report other analyses done (eg, analyses of subgroups and interactions, and sensitivity analyses) | 5 | 38% |
| Discussion | 18 | Summarize key results with reference to study objectives | 11 | 85% |
| 19 | Discuss limitations of the study, taking into account sources of potential bias or imprecision; discuss direction and magnitude of any potential bias | 1 | 8% | |
| 20 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence | 3 | 23% | |
| 21 | Discuss the generalizability (external validity) of the study results | 10 | 77% | |
| Funding | 22 | Give the source of funding and the role of the funders for the current study and, if applicable, for the original study on which the current article is based | 0 | 0% |
Nine hundred eight TKAs were performed for 671 patients, with individual study mean followups between 5 and 18 years, and individual patient followups between 2 and 25.7 years. Cochran Q-test statistics were calculated to assess for study heterogeneity with respect to the most common variables reported: pain, Knee Society (KS) clinical score, and KS functional score. Although study heterogeneity limited the ability to perform meta-analysis of pooled data, postoperative KS clinical and functional scores were available for all studies for determination of mean postoperative scores and average improvement.
Results
The mean postoperative KS clinical score from these 13 studies was 90.9 points (95% confidence interval [CI], 88.3–95 points), which improved by an average of 47 points (range, 31–56 points). The postoperative mean KS functional score was 81.6 points (95% CI, 70.2–89.8 points) with an average improvement of 37 points (range, 15–41). Four studies documented preoperative and postoperative ROM with mean improvements from 102° to 109° flexion [9, 11, 22, 35]. Radiographic assessments reported in the studies noted nonprogressive radiolucencies observed in between 3.8% and 30% of cases (mean, 14.5%) with the patella and tibia being the most common locations (Table 3). Progressive radiolucencies were not commonly reported.
Component survivorship was either directly reported or estimated by Kaplan-Meier analysis in 10 of the studies with survivorship between 90.6% and 99% during the initial 6 to 10 years and between 85% and 96.5% for studies that projected at or beyond 15 years. Revisions for patellar component failure, instability, or infection were the most commonly reported complications, with component revisions uncommon. Fifty revision procedures were documented among the 908 TKAs (5.5%), with a range of revisions reported in individual studies from 3.4% to 18.6% at 2 to 25.7 years (mean, 5–20 years).
Study heterogeneity and limited data reporting attenuate the literature’s impact on guidance for surgical technique and implant selection in younger patients. Cochran’s Q-testing indicated significant heterogeneity among the 13 studies, with p values of 0 calculated for pain, clinical score, incomplete, and functional score. Five studies reported results for 414 TKAs without differentiating between lower demand patients with inflammatory arthropathy and potentially higher-demand patients with osteoarthritis or posttraumatic arthritis [5, 10, 11, 16, 28]. The mean improvement in KS clinical score was 43.6 points in these studies. Two studies (91 TKAs) reporting exclusively on patients with inflammatory arthritis, [4, 34] noted a mean improvement in KS clinical score of 40.8 points (range, 32–48 points). Six studies (402 TKAs) reported specifically on patients with a diagnosis of either osteoarthritis or posttraumatic arthritis [7, 9, 22, 24, 32, 35], and noted a mean improvement in clinical scores for this group of 42.9 points (range, 37–56 points). Cementless fixation was used in only one study in this group (118 TKAs) [35] with a KS clinical score improvement of 47 points. Cemented fixation was used for all patients in three studies [7, 9, 32], with a mean improvement in KS or HSS clinical score of 41.4 points (range, 37–56 points). A posterior cruciate retaining design was used exclusively in three studies [9, 24, 35], with a mean improvement in KS clinical score of 48.3 points (range, 40–56 points). A posterior cruciate substituting design was used exclusively in only two studies [7, 32], both reporting a mean HSS score improvement of 37 points.
Discussion
TKA is being performed with increasing frequency in younger and more active adults, yet the published data on the clinical scores and long-term durability for TKA for these patients are limited. The purposes of this study were to assess the performance and durability of the TKA when performed in young patients and to determine whether the literature provides specific guidance with respect to implant selection or fixation technique for TKA in young patients.
We acknowledge substantial limitations of our review largely reflecting limitations in the existing body of literature. First, the majority of studies are small, retrospective, single-surgeon case series reporting on a heterogeneous group of patients with respect to diagnosis, activity levels, and surgical technique. Only six of the 13 articles that met our inclusion criteria focused specifically on patients with posttraumatic arthritis or osteoarthritis [7, 9, 22, 24, 32, 35]. Five studies included patients with a predominance of rheumatoid arthritis without distinguishing clinical outcomes on the basis of diagnosis or other potential considerations [5, 10, 11, 16, 28], and two studies exclusively reported on patients with rheumatoid arthritis [4, 34]. Second, although variations in surgical technique occurred in most studies, clinical scores were not reported specific to the techniques used, including posterior cruciate ligament management [4, 16, 32], fixation choice [22, 24], tibial component modularity [5, 10], and patellar management [11, 16]. Third, defining TKA performance may not be determined accurately from measurement tools traditionally reported in the literature. Although the KS clinical score consistently assesses knee status after TKA [21], its focus on pain and knee examination may not necessarily reflect physical function, return to desired level of activity, or patient satisfaction. Although the KS function score incorporates elements of activity, walking, and stair climbing, it was not assessed before and after surgery for the majority of available studies on TKAs in younger patients. Fourth, estimates for component survivorship (eg, Kaplan-Meier survivorship curves) often were reported, whereas actual long-term followup with patients enrolled in the studies did not occur for a majority of patients. Stern et al. [32] and Diduch et al. [7] presented the longest followup for studies focused on patients with osteoarthritis or posttraumatic arthritis, noting 87% survivorship at 18 years. However, the mean followup was 8 years (range, 3–18 years) and only 36 patients (31.5%) had documented followups beyond 10 years postoperatively. The authors calculated an annual implant failure rate up to the latest followup and made a linear determination of implant survivorship based on revisions that had occurred. Duffy et al., reporting predominantly on patients with inflammatory arthritis, noted 96% implant survival at 10 years but an increase in polyethylene wear-related failures at 15 years (85% survival), indicating the importance of followup through the end of the second decade [10]. Because younger patients likely will live long enough to require revision surgery, more complete long-term followup is essential to provide an adequate assessment of durability. Continuing and reporting followup through the second decade are important to confirm whether implant survivorship follows a linear or exponential curve beyond the first decade. Finally, we excluded 37 articles published in languages other than English. As we were unable to perform an adequate review of these publications, we cannot exclude positive or negative impacts that these studies might have on the total body of literature. However, with the low percentage of articles that met our strict inclusion criteria with publication in English (13 of 206 studies), we anticipate similar weakness in reporting in the international literature.
Our review showed improvement in mean Knee Society clinical and functional scores that parallel the results reported in studies that have not separated patients on the basis of patient age [1, 2, 6, 8, 12, 19, 27, 30]. Although physician-generated scores suggest improvement, reporting biases that appear to overlook negative patient experiences were identified during this review, including minimizing the impact of revision procedures for patellar resurfacing, polyethylene wear, instability, and stiffness (Table 1). Bourne et al. recently reported patient satisfaction with TKA is achieved by only 81% of patients [3]. Eight of the 13 studies in our review reported between 94% and 98% of patients having a good or excellent result as defined by the authors and generally attributed to a postoperative KS clinical score greater than 80. Notably, four of the six studies reporting on this patient group since 2000 noted good or excellent clinical scores for only 81% to 87% [4, 9, 16, 22], more consistent with the report by Bourne et al. [3]. The inclusion of patient-derived assessment tools, (eg, SF-36, WOMAC, KOOS, satisfaction surveys) [37], assessment of activity level (eg, UCLA activity score) [25, 38], and functional performance testing (eg, stair climbing, timed ambulation) [14], could limit the potential for surgeon bias in reporting clinical and functional scores.
TKA component revisions were relatively uncommon in these series. A few studies noted failures that may have been related to design-specific considerations. Lonner et al. excluded 12 patients (27%) from their study group because an implant design was used that had a 75% rate of polyethylene wear and failure in these younger patients [22]. Although component retention is a major factor in the complexity of revision surgery, implant-related failures may be underemphasized in the literature when only component survivorship is considered. Hofmann et al. noted five revisions (6.6%) performed for polyethylene wear and seven liner revisions (9.3%) for instability but did not present these as clinical failures [16].
Although guidelines may be extrapolated from research that did not meet the criteria of this systematic review, substantiation of specific techniques for TKA in young patients has not been documented in the literature. The two most recent studies most clearly stated their inclusion criteria, and used a single implant and standardized surgical technique, suggesting improvement in reporting quality [9, 35]. However, the authors did not define whether their studies included all young patients who underwent surgery or simply those treated with the specified protocol.
Because our systematic review was performed to consider TKA performance and durability, we excluded some studies [13, 15, 29, 36] that nonetheless provide valuable information in our efforts to understand the results of TKA performed for young patients. National, academic institutional, and community registries have reported on revision surgery rates among young patients. Himanen et al. reported lower 10-year survival rates among patients younger than 60 years, male gender, and a diagnosis of osteoarthritis [15]. W-Dahl et al. noted increased cumulative rates of revision for patients younger than 55 years compared with older patients, but lower revision rates for TKA than for other surgical procedures performed in this patient group, including unicompartmental arthroplasty and proximal tibial osteotomy [36]. Rand et al. reported survivorship analysis for 11,606 TKAs performed in one institution during a 22-year period and noted a lower estimated component survivorship at 10 years for patients younger than 55 years and for patients with a primary diagnosis of osteoarthritis [29]. Gioe et al. reported on implant survival from a community registry for more than 1000 TKAs in patients younger than 55 years and noted higher failure rates for male patients and for patients undergoing either unicompartmental knee arthroplasty or cementless TKA [13]. Although the registry data are valuable in identifying potential implant- or technique-related implant survivorship data, important clinical questions including durability of implants under sustained high activity levels, fixation techniques, implant design selection, surgical techniques, and the influence of perioperative protocols and rehabilitation on functional recovery would be answered with greater certainty from retrospective or prospective studies conducted at a higher level of evidence. The existing body of literature regarding TKA in patients younger than 55 years consists of studies with Level IV evidence. Although the levels of evidence for a specific study indicate the potential for bias and not the validity of results, the strength of conclusions may be less certain when a collective body of evidence contains studies with only the lowest levels of evidence [26]. Although prospective data collection might be inferred from the majority of the articles, only one study specified prospective entry or analysis [11]. Although Diduch et al. [7] likely included patients initially enrolled in the study reported by Stern et al. [32] from the same institution, they did not specify whether the additional patients added to the study were added in a retrospective or prospective fashion.
General reporting quality weaknesses were noted across the studies when using the STROBE criteria (Table 4). Although all studies gave appropriate introduction to the reasons for assessing this patient group, only two studies specifically identified a study purpose or hypothesis [22, 35]. None of the studies discussed or explained missing data or defined how they accounted for patients lost to followup. Although clinical outcomes were reported in a similar fashion by all of the studies, survivorship data rarely were reported with confidence intervals [11, 35], and only the most recently published study [9] specifically acknowledged both statistical methods for evaluating data and the presence of either bias or limitations. These improvements in the most recently published studies may reflect a change in research quality reporting or an elevation in standards for publication.
The use of TKA is increasing among patients younger than 55 years. This collection of data provides important and more generalized information regarding the results of TKA in young patients and may be useful as baseline or comparative data for future studies with this patient population. The existing literature suggests surgeon-reported improvements in pain occur in a similar fashion as in other patients undergoing TKA. However, many of these younger patients are likely to outlive the period of reporting in the current literature. With a relatively low volume of young patients in most individual surgeon practices, multicenter collaboration and improving the details of data submitted to registries will be important to provide more reliable information to guide surgical decisions. Future research should be directed to answer questions regarding TKA implant design considerations, fixation methods, and the effect of activity levels on the durability of TKA among the most young and active patients, who may become a large subpopulation undergoing TKAs during the next 20 years. Improvements in data reporting, emphasized since release of the STROBE statement, will be beneficial in improving the quality of systematic reviews and meta-analyses to help guide clinical decisions.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
This study was performed at the Department of Orthopaedic Surgery, Washington University School of Medicine, and Wilford Hall Medical Center.
References
- 1.Barrington JW, Sah A, Malchau H, Burke DW. Contemporary cruciate-retaining toal knee arthroplasty with a pegged tibial baseplate: results at a minimum of ten years. J Bone Joint Surg Am. 2009;91:874–878. doi: 10.2106/JBJS.G.01609. [DOI] [PubMed] [Google Scholar]
- 2.Bonutti PM, Zywiel MG, Ulrich SD, Stroh DA, Seyler TM, Mont MA. A comparison of subvastus and midvastus approaches in minimally invasive total knee arthroplasty. J Bone Joint Surg Am. 2010;92:575–582. doi: 10.2106/JBJS.I.00268. [DOI] [PubMed] [Google Scholar]
- 3.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468:57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crowder AR, Duffy GP, Trousdale RT. Long-term results of total knee arthroplasty in young patients with rheumatoid arthritis. J Arthroplasty. 2005;20(7 suppl 3):12–16. [DOI] [PubMed]
- 5.Dalury DF, Ewald FC, Christie MJ, Scott RD. Total knee arthroplasty in a group of patients less than 45 years of age. J Arthroplasty. 1995;10:598–602. doi: 10.1016/S0883-5403(05)80202-5. [DOI] [PubMed] [Google Scholar]
- 6.Dalury DF, Gonzales RA, Adams MJ, Gruen TA, Trier K. Midterm results with the PFC Sigma total knee arthroplasty system. J Arthroplasty. 2008;23:175–181. doi: 10.1016/j.arth.2007.03.039. [DOI] [PubMed] [Google Scholar]
- 7.Diduch DR, Insall JN, Scott WN, Scuderi GR, Font-Rodriquez D. Total knee replacement in young, active patients: long-term follow-up and functional outcome. J Bone Joint Surg Am. 1997;79:575–582. doi: 10.2106/00004623-199704000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Dixon MC, Brown RR, Parsch D, Scott RD. Modular fixed-bearing total knee arthroplasty with retention of the posterior cruciate ligament: a study of patients followed for a minimum of fifteen years. J Bone Joint Surg Am. 2005;87:598–603. doi: 10.2106/JBJS.C.00591. [DOI] [PubMed] [Google Scholar]
- 9.Duffy GP, Crowder AR, Trousdale RT, Berry DJ. Cemented total knee arthroplasty using a modern prosthesis in young patients with osteoarthritis. J Arthroplasty. 2007;22(6 suppl 2):67–70. [DOI] [PubMed]
- 10.Duffy GP, Trousdale RT, Stuart MJ. Total knee arthroplasty in patients 55 years old or younger: 10–17 year results. Clin Orthop Relat Res. 1998;356:22–27. doi: 10.1097/00003086-199811000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Gill GS, Chan KC, Mills DM. 5- to 18-year follow-up study of cemented total knee arthroplasty for patients 55 years old or younger. J Arthroplasty. 1997;12:49–54. doi: 10.1016/S0883-5403(97)90046-2. [DOI] [PubMed] [Google Scholar]
- 12.Gioe TJ, Glynn J, Sembrano J, Suthers K, Santos ER, Singh J. Mobile and fixed-bearing (all-polyethylene tibial component) total knee arthroplasty designs: a prospective randomized trial. J Bone Joint Surg Am. 2009;91:2104–2112. doi: 10.2106/JBJS.H.01442. [DOI] [PubMed] [Google Scholar]
- 13.Gioe TJ, Novak C, Sinner P, Ma W, Mehle S. Knee arthroplasty in the young patient: survival in a community registry. Clin Orthop Relat Res. 2007;464:83–87. doi: 10.1097/BLO.0b013e31812f79a9. [DOI] [PubMed] [Google Scholar]
- 14.Heiberg KE, Bruun-Olsen V, Mengshoel AM. Pain and recovery of physical functioning nine months after total knee arthroplasty. J Rehabil Med. 2010;42:614–619. doi: 10.2340/16501977-0568. [DOI] [PubMed] [Google Scholar]
- 15.Himanen AK, Belt E, Nevalainen J, Hämäläinen M, Lehto MU. Survival of the AGC total knee arthroplasty is similar for arthrosis and rheumatoid arthritis: Finnish Arthroplasty Register report on 8, 467 operations carried out between 1985 and 1999. Acta Orthop. 2005;76:85–88. doi: 10.1080/00016470510030373. [DOI] [PubMed] [Google Scholar]
- 16.Hofmann AA, Heithoff SM, Camargo M. Cementless total knee arthroplasty in patients 50 years or younger. Clin Orthop Relat Res. 2002;404:102–107. doi: 10.1097/00003086-200211000-00018. [DOI] [PubMed] [Google Scholar]
- 17.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 18.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606–2612. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lachiewicz PF, Soileau ES. Ten-year survival and clinical results of constrained components in primary total knee arthroplasty. J Arthroplasty. 2006;21:803–808. doi: 10.1016/j.arth.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 20.Lachiewicz PF, Soileau ES. Fifteen-year survival and osteolysis associated with a modular posterior stabilized knee replacement: a concise follow-up of a previous report. J Bone Joint Surg Am. 2009;91:1419–1423. doi: 10.2106/JBJS.H.01351. [DOI] [PubMed] [Google Scholar]
- 21.Lingard EA, Katz JN, Wright RJ, Wright EA, Sledge CB, Kinemax Outcomes Group Validity and responsiveness of the Knee Society Clinical Rating System in comparison with the SF-36 and WOMAC. J Bone Joint Surg Am. 2001;83:1856–1864. doi: 10.2106/00004623-200112000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Lonner JH, Hershman S, Mont M, Lotke PA. Total knee arthroplasty in patients 40 years of age and younger with osteoarthritis. Clin Orthop Relat Res. 2000;380:85–90. doi: 10.1097/00003086-200011000-00012. [DOI] [PubMed] [Google Scholar]
- 23.Ma HM, Lu YC, Ho FY, Huang CH. Long-term results of total condylar knee arthroplasty. J Arthroplasty. 2005;20:580–584. doi: 10.1016/j.arth.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 24.Mont MA, Lee CW, Sheldon M, Lennon WC, Hungerford DS. Total knee arthroplasty in patients </= 50 years old. J Arthroplasty. 2002;17:538–543. doi: 10.1054/arth.2002.32174. [DOI] [PubMed] [Google Scholar]
- 25.Naal FD, Impellizzeri FM, Leunig M. Which is the best activity rating scale for patients undergoing total joint arthroplasty? Clin Orthop Relat Res. 2009;467:958–965. doi: 10.1007/s11999-008-0358-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oxford Centre for Evidenced Based Medicine. Levels of Evidence. Available at: http://www.cebm.net/?o=1025. Accessed July 15, 2010.
- 27.Parsch D, Kruger M, Moser MT, Geiger F. Follow-up of 11–16 years after modular fixed-bearing TKA. Int Orthop. 2009;33:431–435. doi: 10.1007/s00264-008-0543-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ranawat CS, Padgett DE, Ohashi Y. Total knee arthroplasty for patients younger than 55 years. Clin Orthop Relat Res. 1989;248:27–33. [PubMed] [Google Scholar]
- 29.Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg Am. 2003;85:259–265. doi: 10.2106/00004623-200302000-00012. [DOI] [PubMed] [Google Scholar]
- 30.Rasquinha VJ, Ranawat CS, Cervieri CL, Rodriguez JA. The press-fit condylar modular total knee system with a posterior cruciate-substituting design: a concise follow-up of a previous report. J Bone Joint Surg Am. 2006;88:1006–1010. doi: 10.2106/JBJS.C.01104. [DOI] [PubMed] [Google Scholar]
- 31.Ritter MA. The Anatomical Graduated Component total knee replacement: a long-term evaluation with 20-year survival analysis. J Bone Joint Surg Br. 2009;91:745–749. doi: 10.1302/0301-620X.91B6.21854. [DOI] [PubMed] [Google Scholar]
- 32.Stern SH, Bowen MK, Insall JN, Scuderi GR. Cemented total knee arthroplasty for gonoarthrosis in patients 55 years old or younger. Clin Orthop Relat Res. 1990;260:124–129. [PubMed] [Google Scholar]
- 33.Strengthening the Reporting of Observational Studies. Available at: http://www.strobe-statement.org/index.php?id=available-checklists. Accessed July 15, 2010.
- 34.Stuart MJ, Rand JA. Total knee arthroplasty in young adults who have rheumatoid arthritis. J Bone Joint Surg Am. 1988;70:84–87. [PubMed] [Google Scholar]
- 35.Tai CC, Cross MJ. Five- to 12-year follow-up of hydroxapatite-coated, cementless total knee replacement in young, active patients. J Bone Joint Surg Br. 2006;88:1158–1163. doi: 10.1302/0301-620X.88B9.17789. [DOI] [PubMed] [Google Scholar]
- 36.W-Dahl A, Robertsson O, Lidgren L. Surgery for knee osteoarthritis in younger patients: a Swedish Register Study. Acta Orthop. 2010;81:161–164. doi: 10.3109/17453670903413186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wright RJ, Sledge CB, Poss R, Ewald FC, Walsh ME, Lingard EA. Patient-reported outcome and survivorship after Kinemax total knee arthroplasty. J Bone Joint Surg Am. 2004;86:2464–2470. doi: 10.2106/00004623-200411000-00016. [DOI] [PubMed] [Google Scholar]
- 38.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890–895. doi: 10.1016/S0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]