Abstract
The aim of the present study was to determine the economic and social burden of compulsive hoarding in a large sample of individuals with self-identified hoarding, as well as a separate sample of family members of individuals who hoard. Self-identified hoarding participants (N = 864, 94% female, 65% met research criteria for clinically relevant compulsive hoarding) and family informants (N = 655, 58% described a relative who appeared to meet research criteria for compulsive hoarding), completed an internet survey. Questions were derived in part from those used in the National Comorbidity Survey (NCS), and when possible, hoarding participants were compared to NCS participants. Compulsive hoarding was associated with an average 7.0 work impairment days in the past month, equivalent to that reported by individuals with psychotic disorders and significantly greater than that reported by female NCS participants with all other anxiety, mood, and substance use disorders. Severity of hoarding predicted the degree of work impairment after controlling for age, sex, and nonpsychiatric medical conditions. Hoarding participants were nearly three times as likely to be overweight or obese as were family members. Compared to female NCS participants, hoarding participants were significantly more likely to report a broad range of chronic and severe medical concerns and had a fivefold higher rate of mental health service utilization. Eight to 12 percent had been evicted or threatened with eviction due to hoarding, and 0.1–3.0% had a child or elder removed from the home. These results suggest that compulsive hoarding represents a profound public health burden in terms of occupational impairment, poor physical health, and social service involvement.
Keywords: hoarding, obsessive-compulsive disorder, economic burden, saving
1. Introduction
Compulsive hoarding is characterized by (a) the acquisition of, and failure to discard, a large number of possessions; (b) clutter that precludes activities for which living spaces were designed; and (c) significant distress or impairment in functioning caused by the hoarding (Frost and Hartl, 1996). Currently, hoarding is mentioned in DSM-IV-TR (American Psychiatric Association, 2000) only in the context of obsessive-compulsive personality disorder, although many consider it a subtype or dimension of obsessive-compulsive disorder (OCD). However, hoarding behavior has been reported in the context of a wide variety of Axis I disorders including schizophrenia, social phobia, organic mental disorders, eating disorders, depression, and dementia (Steketee and Frost, 2003). A large percentage of people with hoarding problems experience no other OCD symptoms (Frost et al., 2006), and hoarding may be as prevalent in patients with other anxiety disorders as it is in patients with OCD (Meunier, Tolin, Frost, Steketee, and Brady, 2006). Furthermore, the fact that many patients with compulsive hoarding report little distress or recognition of the problem (Fitch et al., 2007; Steketee and Frost, 2003) contrasts with the typical clinical presentation of OCD (therefore, hoarding diagnoses are frequently based on obvious impairment, rather than self-reported distress). Factor and cluster analyses indicate that hoarding consistently emerges as a distinct symptom type, although in two studies hoarding combined with symmetry/ordering to form a separate subgroup (Calamari et al., 2004). Although various OCD symptoms appear closely related to one another, hoarding has not been particularly closely associated with OCD and is just as closely linked to depression as it is with OCD (K. D. Wu and Watson, 2005). In addition, studies of treatment outcome by symptom subtype have largely shown hoarding symptoms to predict poor outcome for standard OCD treatments using medication and exposure with response prevention (Abramowitz et al., 2003; Mataix-Cols et al., 2002; Steketee and Frost, 2003), suggesting that compulsive hoarding and OCD may involve different biological, cognitive, or behavioral mechanisms. Neuroimaging studies (Mataix-Cols et al., 2004; Saxena et al., 2004; Tolin, Kiehl et al., 2007) have also revealed patterns of neural activity that differ from those seen in OCD.
Evidence for the burden of compulsive hoarding has largely been anecdotal, based on small samples, or limited to assessment of psychiatric comorbidity. Clutter has been reported to increase risk of fire, falling, poor sanitation and health risks (Steketee et al., 2001). A survey of health department officials indicated that hoarding was judged to pose a substantial health risk and in 6% of reported cases, hoarding was thought to contribute directly to the individual’s death in a house fire. One small town health department spent most of their budget ($16,000) clearing out one house, only to face the same problem 18 months later. The median number of repeat visits by the health department was 3, and ranged from 0 to 12 (Frost, Steketee, and Williams, 2000). In addition to health departments, housing officials struggle with hoarding cases as well (Frost et al., 1999). Several cities in North America have developed inter-agency task forces to help them deal with individuals who hoard (Frost and Steketee, 2003). Compulsive hoarding may also overlap with severe domestic squalor, creating additional public health concerns (Snowdon et al., 2007). Hoarding is also associated with high rates of psychiatric comorbidity; in a study of 104 compulsive hoarding participants, 57% met diagnostic criteria for major depressive disorder, 29% for social phobia, and 28% for generalized anxiety disorder (Frost et al., 2006). Among patients diagnosed with OCD, rates of depressive and anxious comorbidity are higher for individuals with primary hoarding symptoms than for those with other forms of OCD (Samuels et al., 2007; Samuels et al., 2002).
To date, no studies have examined the economic and social burden of compulsive hoarding in a large sample. The aim of the present study was to survey a large sample of individuals who hoard, as well as a sample of family members of those who hoard, to determine the degree of occupational and role impairment and risks for increased health care utilization. It was predicted that people who hoard would report high levels of impairment and health problems, and that these problems would equal or exceed those reported for several psychiatric conditions assessed in the National Comorbidity Survey (NCS) (Kessler et al., 1994). To obtain a large sample, data were collected over the internet. The internet is increasingly being used for mental health research (Skitka and Sargis, 2006), and several studies indicate that web-based data collection results in greater sample diversity, generalizes across presentation formats, and findings are consistent with data collected using more traditional means (Gosling et al., 2004). Equivalence of internet and paper-and-pencil measurement has been established in clinical disorders, including anxiety (Carlbring et al., 2007), OCD (Coles et al., 2007), and OCD spectrum disorders (Woods et al., 2006).
2. Method
2.1. Participants
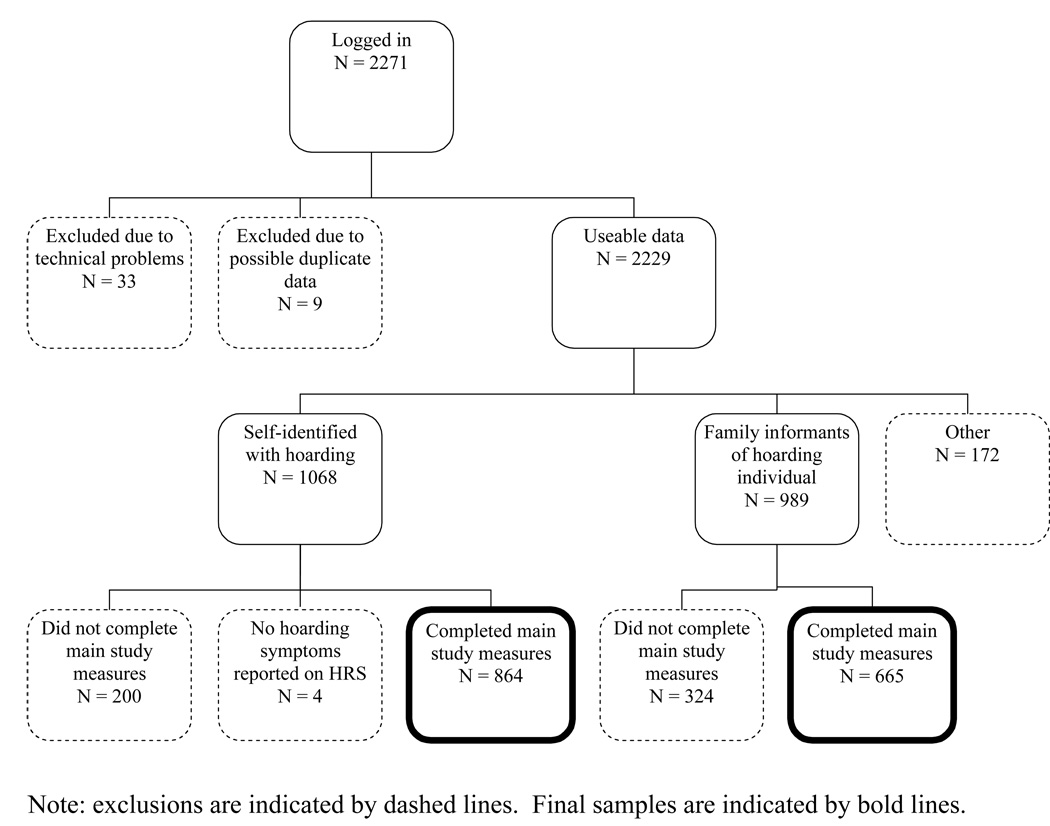
The present sample was recruited from a database of over 8,000 individuals who have contacted the researchers over the past 3 years for information about compulsive hoarding after several national media appearances. Potential participants were sent an e-mail invitation to participate in the study, and were also allowed to forward the invitation to others with similar concerns. Data collection occurred from November 14, 2006 to January 15, 2007. Consistent with current recommendations (Kraut et al., 2004), prior to analysis the data were checked for apparent duplicates (i.e., a participant completing the survey more than once). A flowchart of participation is shown in Figure 1. Of 2271 respondents, we had usable data from 864 people who self-identified with hoarding problems (hoarding participants), and from 665 family informants who answered questions about themselves and their family member who hoarded (hoarding family members). To clarify, hoarding family members were not assessed directly in the present study (i.e., the hoarding family members and the hoarding participants were not the same people); rather, information about these individuals was obtained from the family informants.
Figure 1.
Flow Chart of Participation
For comparison purposes, data were analyzed from the NCS, a stratified, multistage area probability sample of mental disorders in persons aged 15 to 54 years in the United States from 1990–1992. The NCS was selected because of its detailed questions about economic burden of illness, detailed diagnostic assessment, and public availability for analysis. For additional description of the NCS methods see Kessler et al. (1994).
2.2. Materials
Diagnosis and severity of compulsive hoarding was determined using a self-report version of the Hoarding Rating Scale-Interview (HRS-I) (Tolin, Frost et al., 2007a), termed the Hoarding Rating Scale-Self-Report (HRS-SR). Like the interview, the HRS-SR consists of 5 Likert-type ratings from 0 (none) to 8 (extreme) of clutter, difficulty discarding, excessive acquisition, distress, and impairment. The HRS-I has shown high internal consistency and inter-rater reliability, correlated strongly with other measures of hoarding, and reliably discriminated hoarding from non-hoarding participants (Tolin, Frost et al., 2007a).
It is not clear whether compulsive hoarding represents a dimensional phenomenon continuous with normal variations in saving behavior, or a categorical taxon. Preliminary evidence from a nonclinical sample suggests that unlike most OCD symptoms, hoarding shows some evidence of taxonicity (Olatunji et al., 2007). The present analyses, therefore, address hoarding both dimensionally (i.e., as a continuous score) and categorically (i.e., using diagnostic thresholds). Severity of hoarding on the HRS-SR was determined by calculating the mean of all 5 items, with 0 = no hoarding symptoms, 2 = mild hoarding, 4 = moderate, 6 = severe, and 8 = extreme hoarding. Diagnostically, participants were considered to meet diagnostic hoarding criteria if they described moderate (4) or greater clutter and difficulty discarding, as well as either moderate (4) or greater distress or impairment caused by hoarding. The cutoff of 4 is arbitrary, although this is consistent with diagnostic strategies used for other disorders on similar rating scales (Brown et al., 1994). Hoarding participants completed the HRS-SR for their own symptoms and family informants completed the HRS-SR for the identified hoarding family member. We tested the reliability of HRS-SR on a separate sample of 31 participants for whom an HRS-I was also available. The HRS-I and HRS-SR correlated strongly (r = .92, p < .001), with individual item correlations ranging from .74–.91. Hoarding diagnostic status (see above) showed 73% agreement between self- and interviewer-report.
An Economic Impact Questionnaire (EIQ) was developed by the present authors to examine the economic and social burden of hoarding. Many questions on the EIQ were taken verbatim from the NCS interview (Kessler et al., 1994). Specifically, hoarding participants were asked about psychiatric work loss days (number of days in the past month that the respondent was unable to work or carry out usual activities due to mental health issues) and psychiatric work cutback days (number of days in the past month that the respondent was less effective at work or in activities due to mental health issues) (Kessler and Frank, 1997). Consistent with previous research (Kessler et al., 2001), total psychiatric work impairment was calculated as the number of psychiatric work loss days plus 50% of the number of psychiatric work cutback days. Although studies have differed in how psychiatric work impairment was calculated, this method is now preferred and is being used in analyses from the NCS replication study (R.C. Kessler, personal communication, February 10, 2007). NCS-adapted questions also included information about work status, income, and current or most recent job; occupations were entered as text and then recoded into occupational clusters used in prior NCS research (Kessler and Frank, 1997). All participants (hoarding participants and family informants) responded to questions about whether a child, elder, or pet had even been removed from the home by an outside agency due to hoarding; and whether the person had ever been evicted or threatened with eviction because of clutter (all yes/no questions). Both hoarding participants and family informants also responded to queries about whether the person with hoarding had ever been fired due to hoarding (yes/no) or had difficulty finding items at work (never, rarely, sometimes, often), how much workspace was taken up by clutter (none, some, much, a lot), how many of the past 5 years they had filed an income tax return, and how difficult it was to pay bills (not at all difficult, not very difficult, somewhat difficult, very difficult), and family and personal income in 2005. Body mass index (BMI) was calculated as weight (kg) / height (m)2, with a BMI of 25–29.9 considered overweight, and 30 or greater considered obese (Centers for Disease Control and Prevention, 2006). Severe and chronic health conditions (yes/no) were queried among hoarding participants using NCS language. We added questions about fibromyalgia, chronic fatigue syndrome, frequency of mental health service utilization, and likelihood of seeking treatment for hoarding (definitely would go, probably would go, probably would not go, definitely would not go).
2.3. Procedure
The present study was approved by the Institutional Review Boards at Hartford Hospital, Smith College, and Boston University. Human subjects protection was consistent with current recommendations for web-based studies (Kraut et al., 2004). Prior to data collection, participants read an informed consent page and indicated consent by clicking an icon on the page. No protected health information was collected and it was not possible to link study data to an individual or computer. As incentive, participants were given an email address to enroll in a raffle to receive one of 10 copies of a self-help book on compulsive hoarding. Participants responded to the survey by computer. They were allowed to skip any questions they wished, or to complete only portions of the survey. Data were stored on a password-protected server. A summary of aggregate research results was emailed to all individuals in the original database.
2.4. Data Analysis
Comparisons of employment status between hoarding participants meeting vs. not meeting full diagnostic criteria were obtained using Fisher's Exact Test (FET) and DerSimonian-Laird Odds Ratio (OR) with 95% confidence interval (CI). CIs not including 1.00 are considered statistically significant. Comparisons of number of psychiatric work loss, work cutback, and work impairment days were conducted using oneway Analyses of Variance (ANOVAs) with follow-up pairwise comparisons. Because of the strong preponderance of women in the present hoarding sample, our data were compared to female NCS participants who responded to questions about work impairment (N = 3078). Frequencies of specific disorders in the NCS are reported elsewhere (Kessler et al., 1994). The relationship between hoarding severity and psychiatric work impairment days was examined for the total self-identified hoarding group (regardless of diagnostic status, as long as at least some hoarding symptoms were reported on the HRS-SR) using multiple regression analysis in which medical status (the number of chronic medical conditions) was entered in the first block, and the HRS-SR was then entered in a second block. Comparison of rates of medical conditions between the present sample and the NCS was conducted using OR and 95% CI.
3. Results
3.1. Sample Description
Descriptive information for participants is depicted in Table 1. All samples were primarily White and female. Hoarding participants who completed the survey were somewhat younger than were the hoarding family member group described by family informants. In both samples, HRS scores of hoarding participants and hoarding family members meeting full diagnostic criteria were consistent with severe hoarding, whereas scores of those who did not meet full criteria were consistent with moderate hoarding. HRS-SR scores did not correlate significantly with age (r = 0.049) or gender (r = 0.008). Hoarding participants who were married or cohabitating (n = 480; M = 5.43, SD = 1.58) had significantly lower scores on the HRS-SR than did participants who were single, divorced, or widowed (n = 444; M = 5.89, SD = 1.51), t922 = 4.53, p < .001.
Table 1.
Sample Description
| Self-Identified Hoarding Participants | ||||
|---|---|---|---|---|
| Meeting Full Criteria for Compulsive Hoarding | Not Meeting Full Criteria for Compulsive Hoarding | FET | t | |
| N | 645 | 216 | ||
| Female (%) | 93.5% | 94.0% | .873 | |
| White (%) | 89.9% | 92.9% | .219 | |
| Age [M (SD), (range)] | 49.18 (10.40), (21–83) | 48.71 (10.88), (18–85) | .56 | |
| HRS-SR [M (SD)] | 6.32 (1.00) | 3.85 (1.33) | 28.78** | |
| Family Informants reporting on Hoarding Family Members | ||||
| Hoarding Family Member Meeting Full Criteria for Compulsive Hoarding | Hoarding Family Member Not Meeting Full Criteria for Compulsive Hoarding | FET | t | |
| N | 571 | 94 | ||
| Family Informant Female (%) | 83.8% | 80.6% | .453 | |
| Family Informant White (%) | 94.0% | 95.3% | .805 | |
| Family Informant Age [M (SD), (range)] | 45.18 (12.66), (17–86) | 53.23 (12.76), (28–94) | 5.61** | |
| Hoarding Family Member Age [M (SD), (range)] | 60.97 (12.37), (19–94) | 61.53 (13.82), (18–89) | 0.38 | |
| Hoarding Family Member HRS-SR [M (SD)] | 6.72 (0.96) | 4.18 (1.15) | 23.04** | |
Note: HRS-SR = Hoarding Rating Scale-Self-Report. FET = Fisher's Exact Test.
p < .001.
3.2. Work Status
Among hoarding participants, 59.0% (n = 509) indicated that they were currently working. Of those not working, 13.7% (n = 118) were homemakers, 10.1% (n = 87) were retired, 6.5% (n = 56) were unemployed, 5.8% (n = 50) were disabled, 1.7% (n = 15) were temporarily laid off or on maternity or sick leave, 1.7% (n = 15) were students, and 1.4% (n = 12) had other or mixed occupational status. Nearly all (96.0%) of non-working participants had been employed in the past. Disability was reported in 6.7% (n = 43) of hoarding participants meeting diagnostic criteria and 3.2% (n = 7) of hoarding participants not meeting full criteria, FET = .065, OR = 2.13 (0.95–4.81).
3.3. Work Impairment
Thirty-five (5.5%) of hoarding participants meeting diagnostic criteria vs. 8 (3.7%) of hoarding participants not meeting diagnostic criteria indicated that they had been fired because of hoarding, FET = .370, OR = 1.53 (0.70–3.35). Of currently employed hoarding participants, 417 (75.1%) who met diagnostic criteria, vs. 117 (62.9%) who did not, indicated that they sometimes or often had difficulty finding items at work, FET = .002, OR = 1.78 (1.25–2.54). Much or a lot of their workspace was taken up by clutter for 333 (59.8%) hoarding participants meeting diagnostic criteria, vs. 79 (41.6%) not meeting diagnostic criteria, FET < .001, OR = 2.09 (1.49–2.92).
With regard to psychiatric work impairment, 64.5% of hoarding participants meeting full diagnostic criteria reported at least one psychiatric work impairment day [work loss days plus 50% of work cutback days (Kessler et al., 2001)], with 51.6% reporting at least one psychiatric work loss day and 58.8% reporting at least one work cutback day. Of those reporting hoarding symptoms but not meeting full diagnostic criteria, 51.3% met criteria for at least one psychiatric work impairment day, with 28.1% reporting at least one psychiatric work loss day and 48.8% reporting at least one work cutback day. Those meeting full diagnostic criteria (M = 7.01, SD = 8.50) reported significantly more psychiatric impairment days in the past month than did participants not meeting full criteria (M = 3.59, SD = 5.92), t503 = 6.30, p < .001, d = 0.47. Significant differences were also evident comparing full versus not full diagnostic criteria for psychiatric work loss days (M = 4.24, SD = 7.08 versus M = 1.57, SD = 3.97), t625 = 6.66, p < .001, d = 0.47, and also for psychiatric cutback days (M = 6.64, SD = 8.60 versus M = 4.01, SD = 6.66), t474 = 4.57, p < .001, d = 0.34.
For hoarding participants meeting and not meeting full diagnostic criteria, number of psychiatric work impairment days was compared to those reported by female NCS participants meeting DSM III-R (American Psychiatric Association, 1987) diagnostic criteria for several current (1 month) psychiatric disorders. As shown in Table 2, hoarding participants meeting full diagnostic criteria reported significantly more psychiatric work impairment days than did women with the DSM III-R diagnoses of major depressive disorder, dysthymic disorder, panic disorder, agoraphobia, social phobia, simple phobia, posttraumatic stress disorder, alcohol abuse, alcohol dependence, drug abuse, and drug dependence. The number of psychiatric work impairment days for hoarding participants meeting full criteria did not differ significantly from those reported by NCS participants with bipolar disorder or non-affective psychosis. Even those hoarding participants not meeting full diagnostic criteria still reported more psychiatric work impairment than did NCS participants meeting criteria for social phobia, simple phobia, alcohol abuse, alcohol dependence, drug abuse, and drug dependence.
Table 2.
Psychiatric Work Impairment Days in the past 30 days for Hoarding Participants vs. Women in the National Comorbidity Survey Meeting Criteria for DSM III-R Psychiatric Disorders
| Hoarding Participants | NCS Comparison Group | N | M (SD) | F | |
|---|---|---|---|---|---|
| Meeting full diagnostic criteria (M = 7.01, SD = 8.50, n = 591) | Not meeting full diagnostic criteria (M = 3.59, SD = 5.92, n = 199)a | Major Depressive Disorder | 195 | 2.55 (5.43)a | 33.40** |
| Dysthymic Disorder | 31 | 2.15 (3.72)a | 18.15** | ||
| Panic Disorder | 66 | 3.98 (7.17)a | 16.35** | ||
| Agoraphobia | 92 | 3.12 (7.14)a | 20.25** | ||
| Social Phobia | 212 | 1.59 (4.93)a,b | 47.62** | ||
| Simple Phobia | 320 | 1.16 (4.41)a,b | 73.53** | ||
| Generalized Anxiety Disorder | 67 | 4.57 (8.31) | 14.95** | ||
| Posttraumatic Stress Disorder | 131 | 2.55 (5.32)a | 27.55** | ||
| Alcohol Abuse | 296 | 0.62 (3.07)a, b | 86.09** | ||
| Alcohol Dependence | 375 | 1.36 (4.32)a, b | 77.80** | ||
| Drug Abuse | 148 | 0.98 (3.19)a, b | 46.43** | ||
| Drug Dependence | 252 | 1.41 (4.56)a, b | 57.18** | ||
| Bipolar Disorder | 29 | 5.19 (9.24) | 13.88** | ||
| Non-Affective Psychosis | 15 | 11.07 (13.16)b | 16.18** | ||
p < .001.
Significantly different from hoarding participants meeting full diagnostic criteria (p < .05).
Significantly different from hoarding participants not meeting full diagnostic criteria (p < .05).
Within the total hoarding participants group (all hoarding participants who reported at least some hoarding symptoms on the HRS), multiple regression was used to predict the number of psychiatric work impairment days. Bivariate Pearson's correlations indicated that age (r = 0.027) and gender (r = −0.038) did not correlate significantly with the number of psychiatric work impairment days; however, number of chronic medical conditions (r = 0.198) did correlate with psychiatric work impairment days. Therefore, in the regression analysis, the number of chronic medical conditions (range = 0–10) was entered first. This variable was a significant predictor of work impairment (R2= 0.39, β = .198, t = 5.70, p < .001). Next the HRS-SR score was entered, which significantly increased the predictive value of the model (R2 = .121, R2 change = .082, p < .001). Controlling for medical status, the severity of hoarding significantly predicted the number of psychiatric work impairment days, with greater hoarding severity associated with greater impairment (β = .295, t = 8.57, p < .001).
3.4. Taxes
Of hoarding participants who were currently working, 22.0% indicated that in at least 1 of the past 5 years, they had not filed an income tax return. Those meeting full diagnostic criteria (M = 4.41, SD = 1.28) did not differ from those not meeting criteria (M = 4.59, SD = 1.18) in the number of years in which an income tax return was filed in the past 5 years, t253 = 1.48, p = .018.
3.5. Income
Hoarding participants meeting diagnostic criteria were more likely (54.4%) to indicate that it was somewhat or very difficult to pay bills than were those who did not meet diagnostic criteria (38.8%), FET < .001, OR = 1.94 (1.42–2.66). Across all hoarding participants, 37.9% reported personally receiving less than $9,973 in 2005, that year's poverty threshold for a single individual set by the US Census Bureau (U.S. Census Bureau, 2006). Those meeting (37.5%) and those not meeting diagnostic criteria (38.9%) did not differ on this measure, FET = .746, OR = 0.94 (0.69–1.30).
3.6. Health Status
3.6.1. Obesity
BMI was compared among hoarding participants meeting diagnostic criteria (M = 31.59, SD = 8.22), hoarding participants not meeting diagnostic criteria (M = 29.19, SD = 7.11), and family informants (M = 27.32, SD = 6.84). These three groups had BMIs in the overweight or obese range for 78.3%, 71.9%, and 59.1%, respectively, differing significantly on this variable [χ2 (2) = 59.22, p < .001]. Both hoarding participants meeting diagnostic criteria [OR = 2.50 (1.96–3.17)] and those not meeting criteria [OR = 1.77 (1.25–2.51)] were significantly more likely to be overweight or obese than were family informants. Hoarding participants meeting and not meeting criteria did not differ significantly from each other [OR = 1.41 (0.97–2.05)].
3.6.2. Medical Conditions
In response to queries about chronic and severe medical conditions, 63.6% of hoarding participants meeting diagnostic criteria endorsed at least one such condition, compared to 49.8% of hoarding participants not meeting diagnostic criteria [FET < .001, OR = 1.76 (1.31–2.38)]. The rate of specific disorders among hoarding participants is shown in Table 3. Compared to women in the NCS, hoarding participants meeting full diagnostic criteria were significantly more likely to report all of the assessed medical conditions, with increased risk ranging from a twofold risk of ulcer to an 11-fold risk of stroke1. The most commonly-reported medical conditions among hoarding participants were arthritis, hypertension, chronic stomach/gallbladder trouble, lupus/thyroid disorder/autoimmune disease, chronic fatigue syndrome, fibromyalgia, and diabetes/high blood sugar. Hoarding participants who did not meet full criteria showed fewer significant differences with the NCS sample, although increased rates of hypertension, diabetes, and cancer were noted.
Table 3.
Rates of Self-Reported Chronic and Severe Medical Condition among Self-Identified Hoarding Participants who Meet Full Diagnostic Criteria vs. Women in the National Comorbidity Survey (NCS)
| NCS Women | Hoarding (Full Criteria) |
OR vs. NCS |
Hoarding (Not Full Criteria) |
OR vs. NCS |
|
|---|---|---|---|---|---|
| Severe arthritis, rheumatism, other bone or joint diseases | 269 (6.3%) | 147 (22.8%) | 4.38* | 28 (13.0%) | 2.22 |
| Severe asthma, bronchitis, emphysema, tuberculosis, other lung problems | 225 (5.3%) | 118 (18.3%) | 4.02* | 25 (11.6%) | 2.34 |
| HIV/AIDS | 1 (0.0%) | 3 (0.5%) | 19.92* | 0 (0.0%) | -- |
| Blindness, deafness, severe visual/hearing impairment | 49 (1.1%) | 26 (4.0%) | 3.61* | 3 (1.4%) | 1.28 |
| High blood pressure/hypertension | 245 (5.7%) | 189 (29.3%) | 6.80* | 47 (21.8%) | 4.61* |
| Diabetes/high blood sugar | 71 (1.7%) | 71 (11.0%) | 7.30* | 19 (8.8%) | 5.58* |
| Heart attack, other serious heart trouble | 19 (0.4%) | 18 (2.8%) | 6.41* | 3 (1.4%) | 3.54 |
| Severe hernia/rupture | 21 (0.5%) | 19 (2.9%) | 6.13* | 4 (1.9%) | 3.85 |
| Severe kidney/liver disease | 20 (0.5%) | 15 (2.3%) | 5.05* | 4 (1.9%) | 3.85 |
| Lupus, thyroid disease, other autoimmune disorders | 82 (1.9%) | 95 (14.7%) | 8.81* | 18 (8.3%) | 4.67 |
| Multiple sclerosis, epilepsy, other neurological disorders | 46 (1.1%) | 21 (3.3%) | 3.09* | 5 (2.3%) | 2.12 |
| Chronic stomach/gall bladder trouble | 133 (3.1%) | 101 (15.7%) | 5.77* | 19 (8.8%) | 3.02 |
| Stroke | 6 (0.1%) | 10 (1.6%) | 11.17* | 1 (0.5%) | 5.02 |
| Ulcer | 99 (2.3%) | 30 (4.7%) | 2.05* | 3 (1.4%) | 0.60 |
| Cancer, malignant tumor | 33 (0.8%) | 50 (7.8%) | 10.77* | 17 (7.9%) | 10.64* |
| Fibromyalgia | Not assessed | 73 (11.3%) | -- | 16 (7.4%) | -- |
| Chronic fatigue syndrome | Not assessed | 79 (12.2%) | -- | 11 (5.1%) | -- |
p < .05.
OR = Odds ratio.
3.6.3. Medical Expenses
Regarding payment of medical expenses, 13.8% of hoarding participants meeting full criteria and 9.6% of hoarding participants not meeting full criteria reported that their expenses were paid by public aid programs (Medicare, Medicaid, or welfare), FET = .121, OR = 1.51 (0.90–2.52). Private health insurance was reported by similar percentages of hoarding participants meeting full criteria (71.1%) and hoarding participants not meeting full criteria (73.1%), FET = .658, OR = 0.91 (0.64–1.29).
3.6.4. Mental Health Treatment
In the past 12 months, 44.9% of hoarding participants meeting full diagnostic criteria reported that they had seen a mental health specialist, compared to 33.5% of hoarding participants not meeting full criteria, FET = .005, OR = 1.62 (1.17–2.24). Hoarding participants meeting hoarding criteria [OR = 5.29 (4.42–6.33)] and those not meeting criteria [OR = 3.28 (1.61–6.69)] were significantly more likely to have received mental health services than were women in the NCS (13.3%). Of hoarding participants meeting criteria who reported use of mental health services in the past 12 months, 62.1% received medications (number of visits M = 7.71 SD = 8.57), 73.3% had received outpatient therapy (number of visits M = 18.89 SD = 18.85), 2.8% had received inpatient treatment (number of days M = 12.86 SD = 26.31), and 9.8% had received other services (number of visits M = 33.09 SD = 45.38). Of the 853 hoarding participants who reported attitudes toward mental health treatment, 720 (84.4%) reported that they probably or definitely would go for treatment for hoarding problems; 133 (15.6%) reported that they probably or definitely would not go. Participants indicating a willingness to attend treatment showed higher severity of hoarding on the HRS-SR [5.86 (1.43) vs. 4.83 (1.75)] and a higher number of psychiatric work impairment days in the past month [6.66 (8.32) vs. 3.65 (6.08)] than did participants indicating an unwillingness to attend treatment.
3.7. Social Service Intervention
Table 4 depicts external intervention reported by hoarding participants meeting hoarding diagnostic criteria, as well as by family informants describing hoarding family members (note that the family informant and hoarding participants were not paired; thus, the hoarding family members described by the family informants are unlikely to have been the hoarding participants in the present study). In general, the family informant participants reported a greater amount of external intervention, including the removal of a child, elder, or pet from the home (0.5% for hoarders vs. 4.2% for family members) and eviction or threat of eviction (7.8% for hoarders vs. 12.5% for family members).
Table 4.
External Intervention Reported by Hoarding Participants Meeting Diagnostic Criteria and by Family Informants of Family Members Meeting Diagnostic Criteria
| Hoarding Participants | Hoarding Family Members (As Reported by Family Informants) | |
|---|---|---|
| Child removed from home | 1 (0.1%) | 10 (1.8%) |
| Elder removed from home | 0 (0%) | 6 (1.1%) |
| Pet removed from home | 3 (0.4%) | 7 (1.3%) |
| Evicted | 10 (1.5%) | 18 (3.3%) |
| Threatened with eviction | 43 (6.2%) | 52 (9.4%) |
4. Discussion
The prevalence of compulsive hoarding is not known, due to an absence of epidemiologic research. However, some preliminary estimates are possible. The lifetime prevalence of OCD in the U.S. population has been estimated at 1.6% (Kessler et al., 2005). Within samples of OCD patients, 38% report at least some clinically relevant symptoms of hoarding (Samuels et al., 2002). These data alone would suggest a prevalence of 0.6%, or approximately 1.8 million people in the United States. However, research from hoarding (as opposed to OCD) samples suggests that as many as 83% of people with significant hoarding problems do not have OCD (Frost et al., 2006), and therefore would have been unlikely to have presented to the OCD clinics in the aforementioned studies. Thus, 1.8 million is likely a serious underestimate. Although definitive estimates are not possible, it seems clear that compulsive hoarding is highly prevalent in the population.
The present data suggest that hoarding is associated with marked occupational and other role impairment. Prior research with smaller samples suggests that hoarding is associated with greater self-reported work, social, and family impairment than are OCD and other anxiety disorders (Frost, Steketee, Williams et al., 2000). The present study extends these findings in a much larger sample (the largest to date on this topic) by showing that, among people who meet relatively strict diagnostic criteria for hoarding, 7% are on disability and 6% report having been fired from jobs due to hoarding. Even hoarding participants who did not meet full diagnostic criteria reported an elevated rate of job loss due to hoarding, suggesting that even less severe hoarding symptoms might be associated with substantial impairment. Among currently employed hoarding participants, the majority reported that they had difficulty finding items at work, and that their workspace was taken up by clutter. Over one-fifth failed to file income tax in at least 1 of the past 5 years, and 38% brought in personal income below the current poverty threshold for a single individual.
Perhaps most striking are the psychiatric work impairment days, likely a more precise estimate of impairment than self-reported disability used in prior research. Hoarding participants reported significantly more psychiatric work impairment days than did NCS participants with all anxiety and depressive disorders; only NCS patients with bipolar disorder and non-affective psychosis (e.g., schizophrenia) reported work and role impairment to the same extent as did hoarding participants in the present sample. However, differences in sampling methods between the NCS and the present study must be taken into account. The NCS was a stratified random survey of U.S. households, whereas the present study used a convenience sample of individuals who had learned about the research via the media (e.g., television, internet). It is certainly possible that the present sampling method was biased toward more severe cases, and that milder cases might not have self-identified as having hoarding problems or would not have been motivated to seek more information or to participate in the study (alternatively, due to poor insight, very severe cases also might not have self-identified as having hoarding problems). Nevertheless, the magnitude of the differences suggests that hoarding is associated with profound role impairment.
It is also worth noting that the mean age of women in the NCS was approximately 34 years, about 15 years younger than the hoarding participants in the present sample. The maximum age of NCS women was 61, not a match to the older hoarding participants in the present sample. Age-related medical factors likely play some role in occupational and role impairment, although this concern is alleviated somewhat by the facts that: (1) participants specifically identified the number of impairment days due to psychiatric rather than medical factors; (2) the prevalence of psychiatric disorders appears to decline with age across the population (Kessler et al., 1994); (3) in the present sample, age was unrelated to hoarding severity or role impairment days; and (4) in the present sample, hoarding severity was significantly related to impairment even when controlling for non-psychiatric medical conditions. Therefore, it seems unlikely that age accounts for the differences in impairment between the present sample and women in the NCS.
Another potential limitation of the present study is the exclusive reliance on self-report for the hoarding participants. Although several studies now show that data collection over the internet yields results comparable to those using a paper-and-pencil format (Carlbring et al., 2007; Coles et al., 2007; Gosling et al., 2004), a clinical interview might be more reliable and valid than are self-report measures of hoarding, particularly given the poor insight evident in many hoarding participants (e.g., Fitch et al., 2007).
In the absence of epidemiologic research, the gender and race/ethnicity distribution of compulsive hoarding is not known, although participants in clinical trials for hoarding have been primarily female (e.g., Tolin, Frost et al., 2007b). It is not clear whether the mainly White and female sample in the present study accurately reflects the demographics of the hoarding population. Similarly, although the large number of older adults in the present study is consistent with anecdotal estimates suggesting that hoarding severity may increase with age (Steketee et al., 2001), it remains unclear how the present sample compares to the hoarding population in terms of age. Additional research is needed to define the demographic characteristics of individuals who hoard.
It is also unclear the extent to which the reported impairments are caused by hoarding vs. other comorbid conditions. The present study did not include a thorough evaluation of comorbid psychiatric disorders, and research suggests that comorbidity in hoarding is the rule, rather than the exception (Frost et al., 2006). Therefore, it is entirely possible that some of the impairment among individuals who hoard is associated with other conditions such as major depressive disorder, social phobia, generalized anxiety disorder, or attention deficit-hyperactivity disorder, conditions that appear strongly related to hoarding (Frost et al., 2006; Hartl et al., 2005; Meunier, Tolin, Frost, Steketee, Brady et al., 2006) and to role impairment (Adler et al., 2006; Biederman and Faraone, 2006; Kessler, 2003; Wittchen, 2002). The fact that much of the variance in role impairment remains unexplained after accounting for age, gender, medical conditions, and hoarding severity is consistent with the presence of other, unknown contributors.
Although medical service utilization was not formally measured in the present study, non-psychiatric medical expenses among individuals who hoard are likely high. A large majority (78%) was either overweight or obese according to current standards, and a majority (64%) reported at least one chronic and severe medical condition—markedly greater than the rates reported by women in the general population (as reflected by the NCS sample). Patients meeting full diagnostic criteria for hoarding showed higher rates than did NCS women of all assessed medical conditions. Fibromyalgia and chronic fatigue syndrome were among the more commonly-reported conditions, and although these conditions were not assessed in the NCS, the rates in the present hoarding participants (11% and 12%, respectively) seem to exceed women's rates of these conditions in other epidemiologic research (4.9% and 0.2%, respectively) (Jason et al., 1999; White et al., 1999). Forty-five percent had received mental health services in the past year, a fivefold increase over women in the general population. Among those receiving such services, the amount of utilization was high (8 psychopharmacology visits, 19 outpatient therapy visits, and a remarkable 13 inpatient hospitalization days). It is noteworthy that 14% of hoarding participants report that their medical expenses were paid by public aid programs, suggesting that the cost to society is high.
Reports of external interventions differed between self-identified hoarding participants and family informants. It is possible that the family members who participated in the present study were reporting on more severe cases. That is, family members of milder cases of hoarding may have less interest or motivation to participate in such a study. According to the family informants, as many in 1 of 25 of their hoarding relatives had a child, elder, or pet removed from the home due to hoarding, and as many as 1 in 8 had been evicted or threatened with eviction. The rates of such interventions reported by the hoarding participants themselves were lower, but nevertheless striking in underscoring the severity of hoarding. Such data are consistent with the high rate of community agency involvement in cases of hoarding (Frost, Steketee, and Williams, 2000) and the associated high cost of such involvement.
The present data do not permit estimation of the dollar amount of the economic burden of hoarding, as has been reported for other disorders (Greenberg et al., 2003; Greenberg et al., 1999; E. Q. Wu et al., 2005). However, the available data suggest that the impact of compulsive hoarding on a per-person basis exceeds those of many psychiatric disorders. High costs appear likely to affect not only individuals, but also society as a whole in terms of lost work productivity, mental health service utilization, non-psychiatric medical costs, and community agency involvement. Evaluation of the overall cost and impact of compulsive hoarding in the population awaits epidemiologic research.
Acknowledgements
This study was funded by National Institute of Mental Health grants R01 MH074934 (Tolin), R01 MH068008 and MH068007 (Frost & Steketee), and R21 MH068539 (Steketee). Results of this study have been submitted for presentation at the Annual Meeting of the Association of Behavioral and Cognitive Therapies, November 2007, Philadelphia. The authors thank Dr. Nicholas Maltby for his technical assistance and Dr. Ronald Kessler for his comments.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
A 20-fold risk of HIV/AIDS was also found, but this is probably unreliable given the low rates in both samples.
References
- Abramowitz JS, Franklin ME, Schwartz SA, Furr JM. Symptom presentation and outcome of cognitive-behavioral therapy for obsessive-compulsive disorder. Journal of Consulting and Clinical Psychology. 2003;71:1049–1057. doi: 10.1037/0022-006X.71.6.1049. [DOI] [PubMed] [Google Scholar]
- Adler DA, McLaughlin TJ, Rogers WH, Chang H, Lapitsky L, Lerner D. Job performance deficits due to depression. American Journal of Psychiatry. 2006;163:1569–1576. doi: 10.1176/appi.ajp.163.9.1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd Revised ed. Washington, DC: Author; 1987. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th Text Revision ed. Washington, DC: Author; 2000. [Google Scholar]
- Biederman J, Faraone SV. The effects of attention-deficit/hyperactivity disorder on employment and household income. Medscape General Medicine. 2006;8:12. [PMC free article] [PubMed] [Google Scholar]
- Brown TA, DiNardo PA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV. San Antonio, TX: The Psychological Corporation; 1994. [Google Scholar]
- Calamari JE, Wiegartz PS, Riemann BC, Cohen RJ, Greer A, Jacobi DM, Jahn SC, Carmin C. Obsessive-compulsive disorder subtypes: an attempted replication and extension of a symptom-based taxonomy. Behaviour Research and Therapy. 2004;42:647–670. doi: 10.1016/S0005-7967(03)00173-6. [DOI] [PubMed] [Google Scholar]
- Carlbring P, Brunt S, Bohman S, Austin D, Richards J, Ost LG, Andersson G. Internet vs. paper and pencil administration of questionnaires commonly used in panic/agoraphobia research. Computers in Human Behavior. 2007;23:1421–1434. [Google Scholar]
- Centers for Disease Control and Prevention. Defining overweight and obesity [Internet] 2006 Retrieved April 4, 2007, from the World Wide Web: http://www.cdc.gov/nccdphp/dnpa/obesity/defining.htm.
- Coles ME, Cook LM, Blake TR. Assessing obsessive compulsive symptoms and cognitions on the internet: Evidence for the comparability of paper and Internet administration. Behaviour Research and Therapy. 2007 doi: 10.1016/j.brat.2006.12.009. [DOI] [PubMed] [Google Scholar]
- Fitch KE, Tolin DF, Frost RO, Steketee G. Compulsive hoarding: Assessing insight; Paper presented at the Annual Meeting of the Association of Behavioral and Cognitive Therapies; Philadelphia. 2007. Nov, [Google Scholar]
- Frost RO, Hartl TL. A cognitive-behavioral model of compulsive hoarding. Behaviour Research and Therapy. 1996;34:341–350. doi: 10.1016/0005-7967(95)00071-2. [DOI] [PubMed] [Google Scholar]
- Frost RO, Steketee G. Community response to hoarding problems; Paper presented at the Annual Meeting of the Obsessive-Compulsive Foundation; Nashville, TN. 2003. Jul, [Google Scholar]
- Frost RO, Steketee G, Tolin DF, Brown TA. Comorbidity and diagnostic issues in compulsive hoarding; Paper presented at the Annual Meeting of the Anxiety Disorders Association of America; Miami, Florida. 2006. Mar, [Google Scholar]
- Frost RO, Steketee G, Williams L. Hoarding: a community health problem. Health and Social Care in the Community. 2000;8:229–234. doi: 10.1046/j.1365-2524.2000.00245.x. [DOI] [PubMed] [Google Scholar]
- Frost RO, Steketee G, Williams LF, Warren R. Mood, personality disorder symptoms and disability in obsessive compulsive hoarders: a comparison with clinical and nonclinical controls. Behaviour Research and Therapy. 2000;38:1071–1081. doi: 10.1016/s0005-7967(99)00137-0. [DOI] [PubMed] [Google Scholar]
- Frost RO, Steketee G, Youngren VR, Mallya GK. The threat of the housing inspector: a case of hoarding. Harvard Review of Psychiatry. 1999;6:270–278. doi: 10.3109/10673229909000339. [DOI] [PubMed] [Google Scholar]
- Gosling SD, Vazire S, Srivastava S, John OP. Should we trust web-based studies? A comparative analysis of six preconceptions about internet questionnaires. American Psychologist. 2004;59:93–104. doi: 10.1037/0003-066X.59.2.93. [DOI] [PubMed] [Google Scholar]
- Greenberg PE, Kessler RC, Birnbaum HG, Leong SA, Lowe SW, Berglund PA, Corey-Lisle PK. The economic burden of depression in the United States: how did it change between 1990 and 2000? Journal of Clinical Psychiatry. 2003;64:1465–1475. doi: 10.4088/jcp.v64n1211. [DOI] [PubMed] [Google Scholar]
- Greenberg PE, Sisitsky T, Kessler RC, Finkelstein SN, Berndt ER, Davidson JR, Ballenger JC, Fyer AJ. The economic burden of anxiety disorders in the 1990s. Journal of Clinical Psychiatry. 1999;60:427–435. doi: 10.4088/jcp.v60n0702. [DOI] [PubMed] [Google Scholar]
- Hartl TL, Duffany SR, Allen GJ, Steketee G, Frost RO. Relationships among compulsive hoarding, trauma, and attention-deficit/hyperactivity disorder. Behaviour Research and Therapy. 2005;43:269–276. doi: 10.1016/j.brat.2004.02.002. [DOI] [PubMed] [Google Scholar]
- Jason LA, Richman JA, Rademaker AW, Jordan KM, Plioplys AV, Taylor RR, McCready W, Huang CF, Plioplys S. A community-based study of chronic fatigue syndrome. Archives of Internal Medicine. 1999;159:2129–2137. doi: 10.1001/archinte.159.18.2129. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The impairments caused by social phobia in the general population: implications for intervention. Acta Psychiatrica Scandinavica (Suppl.) 2003:19–27. doi: 10.1034/j.1600-0447.108.s417.2.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Frank RG. The impact of psychiatric disorders on work loss days. Psychological Medicine. 1997;27:861–873. doi: 10.1017/s0033291797004807. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Mickelson KD, Barber CB, Wang PS. The effects of chronic medical conditions on work impairment. In: Rossi AS, editor. Caring and doing for others: Social responsibility in the domains of the family, work, and community. Chicago: University of Chicago Press; 2001. pp. 403–426. [Google Scholar]
- Kraut R, Olson J, Banaji M, Bruckman A, Cohen J, Couper M. Psychological research online: report of Board of Scientific Affairs' Advisory Group on the Conduct of Research on the Internet. American Psychologist. 2004;59:105–117. doi: 10.1037/0003-066X.59.2.105. [DOI] [PubMed] [Google Scholar]
- Mataix-Cols D, Marks IM, Greist JH, Kobak KA, Baer L. Obsessive-compulsive symptom dimensions as predictors of compliance with and response to behaviour therapy: results from a controlled trial. Psychotherapy and Psychosomatics. 2002;71:255–262. doi: 10.1159/000064812. [DOI] [PubMed] [Google Scholar]
- Mataix-Cols D, Wooderson S, Lawrence N, Brammer MJ, Speckens A, Phillips ML. Distinct neural correlates of washing, checking, and hoarding symptom dimensions in obsessive-compulsive disorder. Archives of General Psychiatry. 2004;61:564–576. doi: 10.1001/archpsyc.61.6.564. [DOI] [PubMed] [Google Scholar]
- Meunier SA, Tolin DF, Frost RO, Steketee G, Brady RE. Prevalence of hoarding symptoms across the anxiety disorders; Paper presented at the Annual Meeting of the Anxiety Disorders Association of America; Atlanta. 2006. Mar, [Google Scholar]
- Meunier SA, Tolin DF, Frost RO, Steketee G, Brady RE, Brown TA. ADHD symptoms in compulsive hoarders; Paper presented at the Annual Meeting of the Association of Behavioral and Cognitive Therapies; Chicago. 2006. Nov, [Google Scholar]
- Olatunji BO, Williams BJ, Haslam N, Abramowitz JS, Tolin DF. The latent structure of obsessive-compulsive symptoms: A taxometric study. 2007 doi: 10.1002/da.20387. Submitted for publication. [DOI] [PubMed] [Google Scholar]
- Samuels JF, Bienvenu OJ, Pinto A, Fyer AJ, McCracken JT, Rauch SL, Murphy DL, Grados MA, Greenberg BD, Knowles JA, Piacentini J, Cannistraro PA, Cullen B, Riddle MA, Rasmussen SA, Pauls DL, Willour VL, Shugart YY, Liang KY, Hoehn-Saric R, Nestadt G. Hoarding in obsessive-compulsive disorder: Results from the OCD Collaborative Genetics Study. Behaviour Research and Therapy. 2007;45:673–686. doi: 10.1016/j.brat.2006.05.008. [DOI] [PubMed] [Google Scholar]
- Samuels JF, Bienvenu OJ, Riddle MA, Cullen BA, Grados MA, Liang KY, Hoehn-Saric R, Nestadt G. Hoarding in obsessive compulsive disorder: results from a case-control study. Behaviour Research and Therapy. 2002;40:517–528. doi: 10.1016/s0005-7967(01)00026-2. [DOI] [PubMed] [Google Scholar]
- Saxena S, Brody AL, Maidment KM, Smith EC, Zohrabi N, Katz E, Baker SK, Baxter LR., Jr Cerebral glucose metabolism in obsessive-compulsive hoarding. American Journal of Psychiatry. 2004;161:1038–1048. doi: 10.1176/appi.ajp.161.6.1038. [DOI] [PubMed] [Google Scholar]
- Skitka LJ, Sargis EG. The internet as psychological laboratory. Annual Review of Psychology. 2006;57:529–555. doi: 10.1146/annurev.psych.57.102904.190048. [DOI] [PubMed] [Google Scholar]
- Snowdon J, Shah A, Halliday G. Severe domestic squalor: a review. International Psychogeriatrics. 2007;19:37–51. doi: 10.1017/S1041610206004236. [DOI] [PubMed] [Google Scholar]
- Steketee G, Frost RO. Compulsive hoarding: Current status of the research. Clinical Psychology Review. 2003;23:905–927. doi: 10.1016/j.cpr.2003.08.002. [DOI] [PubMed] [Google Scholar]
- Steketee G, Frost RO, Kim HJ. Hoarding by elderly people. Health and Social Work. 2001;26:176–184. doi: 10.1093/hsw/26.3.176. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Frost RO, Steketee G. A brief interview for assessing compulsive hoarding: The Hoarding Rating Scale-Interview. 2007a doi: 10.1016/j.psychres.2009.05.001. Submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF, Frost RO, Steketee G. An open trial of cognitive-behavioral therapy for compulsive hoarding. Behaviour Research and Therapy. 2007b;45:1461–1470. doi: 10.1016/j.brat.2007.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF, Kiehl KA, Worhunsky P, Book GA, Maltby N. A pilot study of the neural mechanisms of decision-making in compulsive hoarding. 2007 doi: 10.1017/S0033291708003371. Submitted for publication. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Poverty thresholds 2005 [Internet] 2006 Retrieved April 4, 2007, from the World Wide Web: http://www.census.gov/hhes/www/poverty/threshld/thresh06.html.
- White KP, Speechley M, Harth M, Ostbye T. The London Fibromyalgia Epidemiology Study: the prevalence of fibromyalgia syndrome in London, Ontario. Journal of Rheumatology. 1999;26:1570–1576. [PubMed] [Google Scholar]
- Wittchen HU. Generalized anxiety disorder: prevalence, burden, and cost to society. Depression and Anxiety. 2002;16:162–171. doi: 10.1002/da.10065. [DOI] [PubMed] [Google Scholar]
- Woods DW, Flessner CA, Franklin ME, Keuthen NJ, Goodwin RD, Stein DJ, Walther MR. The Trichotillomania Impact Project (TIP): exploring phenomenology, functional impairment, and treatment utilization. Journal of Clinical Psychiatry. 2006;67:1877–1888. doi: 10.4088/jcp.v67n1207. [DOI] [PubMed] [Google Scholar]
- Wu EQ, Birnbaum HG, Shi L, Ball DE, Kessler RC, Moulis M, Aggarwal J. The economic burden of schizophrenia in the United States in 2002. Journal of Clinical Psychiatry. 2005;66:1122–1129. doi: 10.4088/jcp.v66n0906. [DOI] [PubMed] [Google Scholar]
- Wu KD, Watson D. Hoarding and its relation to obsessive-compulsive disorder. Behaviour Research and Therapy. 2005;43:897–921. doi: 10.1016/j.brat.2004.06.013. [DOI] [PubMed] [Google Scholar]