Abstract
BACKGROUND
Many studies have found that earlier drinking initiation predicts higher risk of later alcohol and substance use problems, but the causal relationship between age of initiation and later risk of substance use disorder remains unknown.
METHOD
We use a ‘natural experiment’ study design to compare the 12-month prevalence of DSM-IV alcohol and substance use disorders among adult subjects exposed to different minimum legal drinking age laws MLDA in the 1970’s and 1980’s. The sample pools 33,869 respondents born in the US 1948–1970, drawn from two nationally representative cross-sectional surveys: the 1991 National Longitudinal Alcohol Epidemiological Survey (NLAES) and the 2001 National Epidemiological Study of Alcohol and Related Conditions (NESARC). Analyses control for state and birth year fixed effects, age at assessment, alcohol taxes, and other demographic and social background factors.
RESULTS
Adults who had been legally allowed to purchase alcohol before age 21 were more likely to meet criteria for an alcohol use disorder (OR 1.31, 95% c.i. 1.15, 1.46, p < .0001) or another drug use disorder (OR 1.70, 95% c.i. 1.19 to 2.44, p = .003) within the past year, even among subjects in their 40’s and 50’s. There were no significant differences in effect estimates by respondent gender, black or Hispanic ethnicity, age, birth cohort, or self-reported age of initiation of regular drinking; furthermore, the effect estimates were little changed by inclusion of age of initiation as a potential mediating variable in the multiple regression models.
CONCLUSION
Exposure to a lower minimum legal purchase age was associated with a significantly higher risk of a past-year alcohol or other substance use disorder, even among respondents in their 40’s or 50’s. However, this association does not seem to be explained by age of initiation of drinking, per se. Instead, it seems plausible that frequency or intensity of drinking in late adolescence may have long-term effects on adult substance use patterns.
Keywords: ALCOHOL ABUSE, NATURAL EXPERIMENT, MINIMUM DRINKING AGE LAWS, ECONOMETRICS, HEALTH POLICY
INTRODUCTION
Harmful alcohol use is one of the leading causes of preventable death and disability in the world (Mokdad et al, 2004, WHO 2002), and hazardous use of alcohol and other psychotropic drugs are important contributors to other adverse social and economic outcomes (WHO 2002). In the United States, many studies have found that age at initiation of drinking is one of the strongest predictors of risk for alcohol and other substance use problems in adulthood (e.g., Robins and Przybeck, 1985, Grant and Dawson 1997, and Hingson et al, 2006). However, the causal relationship between age of drinking initiation and later alcohol use disorder remains controversial. On the one hand, early drinking may simply be a marker for genetic risk factors that increase risk of both early initiation of alcohol use and later substance dependence (e.g., Liu et al 2004; McGue & Ianocco 2008, Prescott & Kendler 1999). On the other hand, secular trends in adult alcohol dependence track secular trends in age of initiation across time periods that are too short to be explained by changes in the genetic composition of the population (Grucza et al, 2008), It is also possible that early drinking is a non-causal marker for other behaviors or environmental factors that increase the risk of later substance use disorders. These might include the intensity or frequency of adolescent drinking (rather than initiation per se), or cultural factors shaping the role of alcohol in social settings across the life cycle. Whether or not variations in age of initiation across adolescence in is a causal risk factor itself, or a marker for other environmental factors governing adolescent drinking, there are several lines of evidence suggesting that habits acquired in adolescence might have more persistent effects than habits acquired at older ages. For example, although alcohol and nicotine are legally sanctioned only for adults in the United States, the onset of alcohol and nicotine dependence is concentrated in adolescence and young adulthood and does not increase with increasing age beyond the early 20’s (Grant et al, 2004), and imaging studies show that the human brain areas involved in judgment and self-control do not reach their adult form until the early 20’s (Lenroot and Giedd, 2006; Crews et al 2007). However, the results of experimental studies using animal models are mixed, with some studies finding significant long-term effects of adolescent exposure on voluntary consumption of alcohol in adulthood (e.g., Barron et al 2005, and Pautassi et al 2008), and other studies finding no effect (Vetter 2007, Tambour et al 2008).
It would be difficult to conduct a randomized trial of alcohol initiation in human adolescents, but a natural experiment of this kind was created by changing minimum legal drinking age (MLDA) laws in the United States during the 1970’s and 1980’s. From the repeal of alcohol prohibition in 1933 until the early 1970’s, most US states maintained a minimum legal alcohol drinking age of 21 years. Then, in the early 1970’s, as the federal voting age was being lowered to 18, 26 states lowered the age of majority for possession or purchase of alcohol as well (Wechsler & Sands, 1980). By the mid-1970’s, research studies began to report a link between lower drinking ages and rising rates of motor vehicle crashes among young drivers; 16 states increased their MLDA’s between 1976 and 1983 and in 1984, Congress passed the National Minimum Drinking Age Act (23 USC §158) directing the Secretary of Transportation to withhold a percentage of otherwise allocable federal highway funds from States “in which the purchase or public possession … of any alcoholic beverage by a person who is less than twenty-one years of age is lawful.” This act led most remaining states to increase their MLDA’s to age 21 by 1988, with the exception of the state of Louisiana, which permittedde facto alcohol sales to 18 to 20 year olds until 1995 (Table S1). All states now prohibit public possession of alcoholic beverages by minors, and prohibit furnishing of alcoholic beverages to minors by commercial enterprises. Most states also explicitly prohibit minors from purchasing or consuming alcoholic beverages, but many states allow certain exceptions in non-commercial settings; for example, 20 states currently allow alcoholic beverages to be furnished to a minor by a parent, guardian or spouse (NIAAA APIS, 2009).
MLDA laws have been among the most widely studied substance use policies in the world, and most studies have found that higher MLDA’s led to later initiation of drinking and reduced frequency of heavy drinking (e.g., Cook and Moore, 2001, Dee 1999, and O’Malley and Wagenaar 1991). In a study using 28 years of cross-sectional surveys from the Monitoring the Future Study (MTF), Carpenter et al (2007) found that about 60% of high school seniors reported drinking in the past 30 days, and 34% reported drinking 5 or more drinks in a row at least once in the past two weeks; exposure to an MLDA of 18 increased the proportion of drinkers by about 3 percentage points, and increased the proportion reporting heavy episodic drinking by about 1.7 percentage points. Other studies have found that higher MLDA’s led to fewer alcohol-related traffic crashes (e.g. Kypri et al, 2006, Ponicki et al 2007, Schults et al 2001), and lower rates of crime and suicide among persons below age 21 (e.g., see reviews in Cook 2007, Carpenter et al 2007, and Wagenaar and Toomey 2002). However, very few studies have considered whether under age drinking policies might have persistent effects beyond the age of 21.; Birkmayer and Hemenway (1999) found that states with a more lenient MLDA had no difference in the suicide rate for persons aged 15 to 17, but had an 8% higher suicide rate among persons aged 18 to 20, (P<.01), and a 6% higher suicide rate among persons age 21–24 (p < .05). Four studies have found that young adults exposed to lower legal drinking ages were more likely to continue to be episodic heavy drinkers in their early 20’s (Cook and Moore 2001, Moore and Cook 1995, O’Malley and Wagenaar 1991, and Pacula 1997). We are unaware of any previous studies evaluating the persistent effects of youth alcohol policies among subjects in their 30’s or beyond,
In the present study, we use these MLDA policy experiments to investigate the relationship between adolescent drinking exposures and the past-year prevalence of DSMIV alcohol and substance use disorders in cohorts evaluated from age 20 to age 54. The state-by-state variation in the timing of changes in the MLDA allows us to use state and year fixed effects to purge our estimates of potentially confounding influences that are relatively constant within a state, or common to each birth cohort across states (e.g., Angrist and Pischke 2009, Cook and Campbell 1979), and the pooling of two large, nationally representative cross-sectional surveys conducted in 1991–1992 and 2001–2002 makes it possible to distinguish the effects of birth cohort from the effects of age at assessment. Some of our regression models also control for parental alcoholism, state-specific linear time trends, and for per capita alcohol consumption and state beer taxes in the year that the respondent turned 18. However, a possible concern in a study design of this kind is that some other, unobserved social process might better explain an apparent link between MLDA policies and adult substance use patterns. In the case of MLDA laws, it is possible to further narrow the field of competing explanations by comparing MLDA effects in birth cohorts that fall naturally in to two contrasting periods. In the earlier wave, born 1948–1955, legal purchase ages were being lowered along with the age of majority for many other legal rights; younger respondents in this era were exposed to a more permissive political and drinking environment than older respondents living in the same state. In the later wave, born 1956–1970, legal purchase ages were rising because of specific public concerns about youth drinking, and younger subjects were exposed to a less permissive drinking environment. If higher purchase ages have similar effects in both earlier and later cohorts, then the association cannot be explained by age at assessment or by trends that moved in the same direction across both periods. In another set of analyses, we limit the sample to subjects who were coming of age within two years of a change in MLDA law affecting 20-year olds. In this age-restricted sample, respondents in each state/period cell are very closely matched in demographic characteristics, and are likely to have experienced similar exposures to other economic, social, cultural or political trends. In both the full and age-restricted sample, we test whether the MLDA laws are likely to be working through age of initiation, per se, by evaluating the change in the MLDA estimate in models that control for lifetime abstention status and age of onset of regular drinking. Overall, we find that earlier age at drinking initiation predicts higher risk of past-year alcohol or substance use disorder, and exposure to a lower minimum legal purchase age predicts higher risk of a past-year alcohol or other substance use disorder, even when respondents are evaluated in their 40’s or 50’s., However, the MLDA association does not seem to be explained by self-reported age of initiation of drinking.
A remaining concern is that cross-state migration could lead to a spurious association if persons at greater risk for developing a substance use disorder were more likely to have moved to a state with more lenient drinking age laws. To explore this hypothesis, we use evidence from the NLAES survey and from the US Census years 1970 through 2000 to investigate (1) the prevalence of cross-state migration (2) the prevalence of a change in apparent MLDA exposure status when this is calculated based on state of birth or state of current residence, and (3) whether MLDA exposure based on state of birth is a better predictor of current substance use disorder, than MLDA exposure based on current state of residence.
MATERIALS AND METHODS
Source Data
The primary sample for the present study was pooled from two large, nationally representative and publicly-available US surveys: the National Longitudinal Alcohol Epidemiological Survey (NLAES), conducted in 1991–92 (Grant et al, 1994), and the National Epidemiological Survey on Alcohol and Related Conditions (NESARC), wave 1, conducted in 2001–02 (Grant et al, 2003). Both were face-to-face surveys using similar sampling designs and survey measures, conducted by the U.S. Bureau of the Census under supervision of the National Institute of Alcohol Abuse and Alcoholism. NLAES sampled 42,862 subjects drawn from the adult, non-institutionalized, civilian population of the 48 contiguous United States and the District of Columbia, with over-samples of Blacks and of persons 18 to 29 years old, and with a household-response rate of 91.9 percent. NESARC interviewed 43,093 respondents drawn from a sampling frame that included adult, non-institutionalized civilians in all 50 states (plus the District of Columbia) with over-samples of Blacks and Hispanics, and of respondents aged 18 to 24 years old; the household response rate was 89 percent. Both sampling frames included military personnel living off base and residents in non-institutionalized group quarters, such as boarding houses, shelters, and dormitories, and both surveys provide respondent month and year of birth. NLAES provides state identifiers for both state of birth and state of current residence, and the public-use version of the first wave of NESARC provided identifiers for state of current residence. Both surveys were conducted using computer assisted personal interviewing (CAPI), and used versions of the Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS), a fully structured diagnostic interview designed to ascertain the presence of past-year and lifetime alcohol and substance use disorders according to the Diagnostic and Statistical Manual, Fourth Edition (DSM-IV™) (American Psychiatric Association 1994, Grant et al, 2001.). Informed consent was obtained from all subjects, and the U.S. Census Bureau and U.S. Office of Management and Budget reviewed and approved all procedures.
For the present study, we limit our sample to 33,869 respondents (18539 from NLAES and 15,330 from NESARC) who were born in the United States between 1948 and 1970. For comparisons across waves, subjects were divided into cohorts born between 1948 and 1955 (who were reaching age 18 in the era when minimum purchase ages were being lowered), and cohorts born between 1956 and 1970 (who were coming of age in the era when minimum purchase ages were being raised). In our age-restricted analysis, the sample was further limited to the 18,136 subjects who had reached the ages of 18, 19, or 20 within two years of an MLDA law change affecting alcohol purchase by 20 year olds.
To investigate the correlates of cross-state migration, we supplemented these analyses with evidence from 1% extracts of the Public Use Micro samples of the U.S. Censuses of 1970, 1980, 1990, and 2000 (Ruggles et al, 2008), using census respondents born in the US between 1948 and 1970, and tracking their apparent MLDA exposures and cross-state migration patterns based on state of birth and current state of residence.
Outcome measures
The main outcome measures for the present study were binary variables reflecting whether the respondent met DSM-IV criteria for alcohol, marijuana, or other illegal substance abuse or dependence within the previous 12 months. A diagnosis of DSM-IV alcohol or drug abuse requires that a person meet at least one of four abuse criteria, and a diagnosis of alcohol or drug dependence requires that a person meet at least three of seven dependence criteria. Supplementary table 1 gives examples of the NESARC items related to past-year alcohol dependence; the NLAES items, and items related to other substance use disorders, are similar. The aggregated category of ‘substance use disorders’ included abuse of or dependence on alcohol, marijuana, stimulants, cocaine, opiates, heroin, sedatives, benzodiazepines, solvents, hallucinogens, or other illegal drugs. We also investigated the effects of MLDA exposure on self-reported age of onset of ‘regular’ drinking, based on NLAES and NESARC respondent answers to the question “about how old were you when you first started drinking, not counting small tastes or sips of alcohol?” (NIAAA 2006, page 7).
Other covariates
Other covariates were selected based on factors known to be associated with risk of substance use disorders, and possibly correlated with the state decisions to change their MLDA laws in specific years. All analyses controlled for gender, survey, self-identified non-Hispanic Black or Hispanic race or ethnicity, indicators for five roughly equal-population quintiles of age at assessment (20–29, 30–34, 35–39, 40–44, and 45–54 years of age), and unordered indicators for single year of birth and either state of residence or state of birth. Some analyses also controlled for a binary indicator of (subject-reported) maternal or paternal alcohol problems, and inflation-adjusted state beer taxes in effect when the subject was 18 years old (Beer Institute 2008). Other analyses investigated the role of demographic factors in later adulthood that might lie in the causal pathway between MLDA exposure and drug or alcohol use; these factors included age of onset of drinking (both as a linear mesure, and using unordered indicators for the following categories: under 14, 14–15, 16–17, 18, 19, 20, 21, > 21, and lifetime abstention), educational attainment, whether currently employed or not, current marital status (spouse present in the household, or not), and presence of children under the age of 13 in the home.
Law coding
We coded the month and year of changes in state-wide minimum purchase age laws, including ‘grandfathering’ clauses, from published peer-reviewed articles (DuMouchel 1987, O’Malley and Wagenaar 1991, Wagenaar 1981–82), from unpublished tables provided by the Statewide Availability Data System (Ponicki 2004), and from a Lexis-Nexis search of news sources (Associated Press 1996). These sources did not make distinctions between laws preventing adults from furnishing alcohol to persons under 21, or preventing persons under-21 from possessing, purchasing, or consuming alcohol. We made no attempt to capture ‘dry counties’ or other local ordinances that may have been stricter than the state-wide minimum purchase ages. Discrepancies between sources were resolved by the authors, based on internal evidence from these sources (see Table S2); however, alternate coding decisions did not lead to substantial changes in our results. Exposures based on current state of residence could be estimated in both samples, and exposures based on state of birth could be estimated in NLAES. To maximize agreement across coding alternatives, and for simplicity of exposition, exposure status was summarized in a binary variable coded as ‘1’ if the respondent could have legally purchased some form of beer, wine, or liquor in the reference state (either state of current residence or state of birth) before the age of 21, and coded ‘0’ otherwise; odds ratios in our logistic regression models can therefore be interpreted as the difference in the odds of the specified outcome associated with an MLDA below 21, compared to the odds of the outcome with an MLDA set at 21 years. All of our results were similar using a continuous measure of exposure. Exposure to an MLDA under 21 varied across birth years from about 26% for native-born residents born before 1950, to a peak of 72.9 % among those born in 1959, and falling to zero among those born after 1969.
MLDA Statistical methods
Because our dependent variables were categorical indicators, we used both logistic and probit regression models to estimate the relative odds or relative risk of a past-year alcohol or drug use disorder or cross-state migration among ‘exposed’ and ‘unexposed’ subjects (Breslow and Day 1980; Hosmer and Lemeshow 1989), and to investigate the possibility of differences in effect estimates across demographic groups. In most of these models, the response variable was an indicator of past-year alcohol or drug use disorder, and the predictor of interest was MLDA exposure; indicators for each state controlled for factors that vary across states but not over time, and indicators for single year of birth controlled for factors that vary across birth years but not across states. Although estimates from logistic models can be biased when strata are sparse (Kalbfleisch and Sprott, 1970), our pooled sample sizes are large enough that nearly identical estimates and standard errors were generated by ordinary fixed effect logistic models with state indicators, and by conditional logistic models stratified by state. However, ordinary logistic models gave better convergence and the ability to use sampling weights that vary within state. In analyses restricted to individuals coming of age within two years of a law change, we use separate indicators for early and later cohorts in each state.
The basic structure of our regression model is given by:
where Yist refers to an outcome of interest for individuals i living in state s and born in year t. In the case of a logit model, Y is Ln(R/1−R)i, where R may be the probability of a past-year alcohol or substance use disorder, or the probability of a cross-state move for individuals with a vector of characteristics Xi …Xn; in the case of a probit model, Y is the inverse of the cumulative normal distribution function for R. The vector of covariates always includes survey, gender, ethnicity, and unordered indicators of state of residence, age group, and year of birth. Some models also included interaction terms between MLDA exposure and demographic subgroups (e.g., gender or race), and others included an interaction between state and a linear measure of birth year, to further control for state-specific time trends. Some “long” models included other control variables, including family history of alcohol problems, state beer taxes when the respondent was 18, and state per capita alcohol consumption when the respondent was 18. The ‘longest’ models tested whether a few potential mediating variables – such as age of onset of regular drinking, educational attainment, current marital status or presence of young children in the home – seemed to explain the association between legal purchase age and later substance use problems. We also compared interaction terms in both probit and logit models to test for additive or multiplicative interactions between MLDA exposure and gender, race, survey, age at assessment, parental alcohol problems, early versus later cohort, and onset of own drinking before or after age 16. Age-restricted models were limited to respondents living in the 39 states with changing MLDA laws, and included separate indicators for early and later cohorts for each state. In each of these models, the coefficient of interest is bMLDA, which captures the average effect of legal purchase age on the outcome of interest.
We investigated the effects of MLDA exposure on self-reported age of onset of drinking in two types of model. First, we used ordinary logistic models (as described above) to test the association between MLDA exposure and age of drinking onset before age 16. We then extended this analysis using multinomial logistic regression to test the association between MLDA exposure and onset of drinking in the following unordered categories: under age 16, age 16–17, age 18, age 19 to 20, age 21, over age 21, and lifetime abstention, with onset under age 16 as the reference group. All analyses were conducted in STATA v.10, using ’robust’ standard errors clustered by state; these adjust for the correlation of observations within state, and capture most of the clustering of observations generated by the complex survey design. (Arellano 1987, Liang and Zeger, 1986). For all models, we report 95% confidence intervals with two-sided p-values.
RESULTS
Sample description
Table 1 describes the combined NLAES/NESARC samples. Subjects ranged from 20 to 44 years old at the time of the NLAES interview, and from 30 to 54 years old at the time of the NESARC interview. 10.3 % of the sample met DSM-IV criteria for past-year alcohol use disorder, 1.5% met criteria for past-year marijuana use disorder, 1.7% for other illegal drug use disorders, and 11.3% met DSM-IV criteria for any past-year alcohol or other substance use disorder. 51.8% of the full sample and 78.2% of the age-restricted sample would have been legally allowed to purchase alcohol before the age of 21.
Table 1.
Sample Description:
| Full Sample | Age-restricted samplea | |
|---|---|---|
| N | 33,869 | 18,136 |
| Interview year | 1991–2002 | 1991–2002 |
| Mean Birth year (SD) | 1958.0 (.068) | 1957.8 (.26) |
| Mean Age at interview (SD) | 39.5 (.29) | 39.7 (.49) |
| Sex (%) | ||
| Female | 51.0 | 51.2 |
| Male | 49.0 | 48.8 |
| Race (%) | ||
| Non-hispanic Black | 12.8 | 13.6 |
| Hispanic | 5.0 | 3.9 |
| Non-black, non-Hispanic | 82.4 | 82.5 |
| Birth cohort | ||
| Early: born 1948–1955 | 33.8 | 56.7 |
| Later: born 1956–1970 | 66.2 | 51.8 |
| Education (%, Highest Completed) | ||
| No High School | 9.4 | 9.3 |
| High school | 61.9 | 61.9 |
| College | 28.7 | 28.8 |
| Substance Use and Disorder (%) | ||
| Past year alcohol use disorder | 10.3 | 10.1 |
| Past year marijuana use disorder | 1.5 | 1.3 |
| Other past year drug use disorder | 1.7 | 1.5 |
| Any past year substance use disorder | 11.3 | 10.9 |
| Onset drinking before age 16 | 12.3 | 12.2 |
| Lifetime Abstainer | 16.5 | 15.8 |
| Parent had alcohol problem | 28.2 | 27.8 |
| Risk Factor Exposure, All subjects: | ||
| MLDA < 21, state of residence | 51.8 | 78.2 |
| State beer tax, age 18 (1982 dollars per gallon) | .259(.034) | .284 (.037) |
| Risk Factor Exposure, NLAES sample | ||
| Moved from state of birth d | 36.9 | 38.8 |
| MLDA < 21, state of birth d | 50.2 | 68.6 |
| Switched MLDA status d | 16.2 | 16.9 |
Note: Weighted means and frequencies; for means, linearized standard error is in parentheses. ‘MLDA’= Minimum Legal Purchase Age; coded 1 if responded could have legally purchased alcohol before age 21. Data source = subjects born in US 1948–1970, pooled from the 1991–1992 National Longitudinal Alcohol Epidemiological Survey (NLAES), and the 2001–2002 National Epidemiological Survey of Alcoholism and Related Conditions (NESARC).
Respondents who were aged 18, 19, or 20 within two years before or after a change in MLDA law in state of residence.
Married subjects only.
Respondents with children only.
NLAES only.
Prediction from MLDAs to age of onset
As in other studies, we found that exposure to a lower legal purchase age did predict earlier self-reported ages at onset of regular drinking. In a logistic regression controlling for sex, ethnicity, age group, study, parental alcohol problems and state and birth year fixed effects, MLDA exposure based on current state of residence was not a significant predictor of self-reported onset of drinking before age 16 (OR .1.02, 95% ci .92 to 1.14, p = .70), but in multinomial logistic regressions controlling for the same covariates, (with onset before age 16 as the omitted group) we found that respondents exposed to a lower MLDA were significantly more likely to have started drinking at age 18 (OR 1.16, 95% ci 1.00, 1.35, p = .05), and less likely to have started drinking at age 21 (OR .66, 95% c.i. 54 to .81, p <.0001), However, an earlier legal purchase age had no significant effect on the likelihood of onset of drinking at 16 or 17 (OR 1.03, 95% ci .91, 1.16, p=.68), age 19 or 20 (OR .88, 95% ci .75 to 1.05, p = .16), or after age 21, (OR .94, 95% ci .79 to 1.11, p = .46), nor on the likelihood of lifetime abstention (OR .96, 95% c.i. .84, 1.08, p = .48). Supplementary figure 1 illustrates this pattern in the raw data, and supplementary table 3 gives further details of the multinomial logit results.
Prediction from MLDA exposure to mid-life alcohol and substance use disorders
Figures 1 and 2 illustrate our core results. Figure 1 shows that an association between MLDA exposure and prevalence of past-year alcohol and substance use disorders is discernable in the raw data using the age-restricted sample. Although there is also a trend for the difference between 21 and under-21 MLDA exposure groups to increase at older ages, Figure 2 gives odds ratio estimates from multiple logistic regression models controlling for state and birth year fixed effects, gender, race/ethnicity, survey, and age group, using the full sample. This figure shows a more constant effect of MLDA exposure across age groups, suggesting that the apparent age trend in Figure 1 may be due to confounding effects of state or birth cohort characteristics. The regression results suggest that the MLDA effects were statistically significant in most age groups and of approximately similar magnitude among respondents in their 20’s, 30’s, 40’s, and 50’s.
Figure 1.
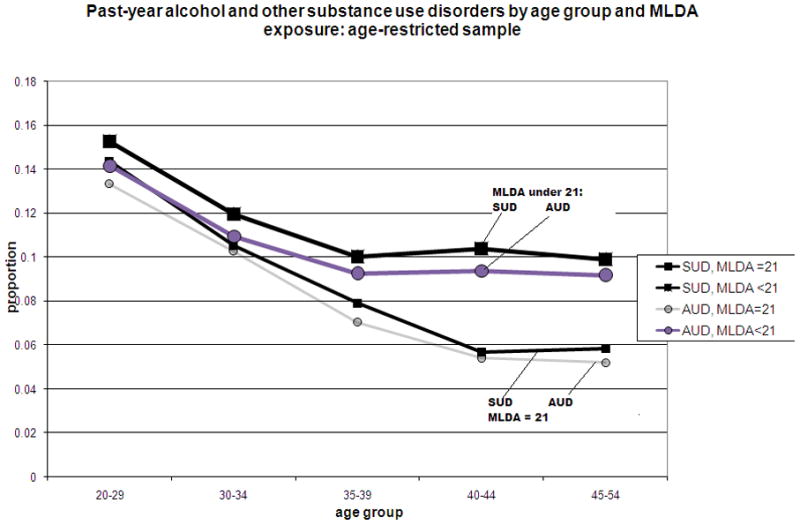
Prevalence of past-year alcohol and substance use disorders (AUD’s and SUD’s), by minimum legal purchase age (MLDA) exposure status and current age at assessment. Plot of weighted frequencies. N = 18,136 respondents in age-restricted NLAES/NESARC sample (see text).
Figure 2.
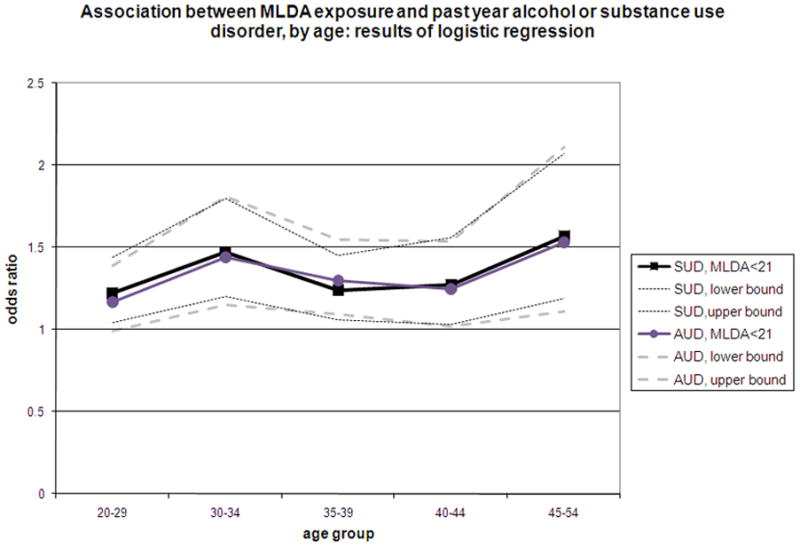
Effect of minimum legal drinking age (MLDA) exposure on past-year alcohol and substance use disorders, by age at assessment. Plot of odds ratios for exposure to MLDA under 21, relative to MLDA of 21, for past-year DSM-IV alcohol and substance use disorders (AUD’s and SUD’s), based on logistic regressions controlling for state and birth year fixed effects, gender, race, and survey (see text). N = 33869 respondents in combined NLAES/NESARC sample
Tables 2 and 3 further quantify these associations. In Table 2, respondents exposed to a lower MLDA were significantly more likely to have a past-year alcohol use disorder. Column 1 shows logistic regression results using the NLAES sample, controlling for state and year fixed effects, gender, black and Hispanic ethnicity, and age group. The odds ratio for a current alcohol use disorder associated with exposure to a lower drinking age was 1.33 (95% c.i. 1.15 to 1.54, p < .0001). In the NESARC sample (Column 2), the odds ratio is 1.31, (95% c.i.1.07 to 1.61, p = .009), and in the combined sample (Column 3), the odds ratio is again 1.31 (95% c.i. 1.18 to 1.46, p < .0001)). The similarity of the MLDA estimates in the NLAES and NESARC samples and the non-significance of an interaction term between MLDA status and sample indicator supports the statistical appropriateness of the pooling of samples. In Column 4, the estimate was little changed by inclusion of lifetime abstention status and a linear measure of age of onset of regular drinking, parental drinking problems, state beer taxes and per capital alcohol consumption when the respondent was 18, educational attainment, current marital status, current employment status, and presence of children under 13 in the respondent’s current household (OR 1.30, 95% c.i. 1.16 to 1.44, p< .0001) Effect estimates were similar for each age group (20–29, 30–34, 35–39, 40–44, and 45+) (Figure 2, and supplementary Table 4). The results were identical when age of onset was modeled as unordered age categories, (1.30, 95% c.i. 1.16 to 1.44, p< .0001), nearly identical for alcohol abuse (1.27, 95% ci 1.04 to 1.54, p = .017) and for alcohol dependence (1.27, 95% c.i. 1.11 to 1.45, p = .001) when these diagnoses were considered separately, and similar when we specified probit models rather than logits.
Table 2.
Minimum Legal Drinking Age Exposure and Past-year Alcohol Use Disorder: Logistic Regression
| Sample | NLAES | NESARC | Combined Sample | |
|---|---|---|---|---|
| Model | Core variables | Core variables | Core variables | Extended model |
| N | 18,539 | 15,330 | 33,869 | 27,704 |
| OR (95% c.i.) | OR (95% c.i.) | OR (95% c.i.) | OR (95% c.i.) | |
| Exposure | ||||
| MLDA<21 | 1.32 (1.13, 1.54)**** | 1.33(1.08, 1.64)** | 1.32(1.19. 1.46)**** | 1. 29(1.16,1.44)**** |
| Age group: | ||||
| Age 30–34 | .40 (.20, .77)** | 1.31 (.56, 3.05) | 0.61 (0.45, 0.82)*** | 0.71 (0.51, .99)* |
| Age 35–39 | .36(.14, .90)* | .88 (.52, 1.50) | 0.69 (0.47, 1.02) | 0.76 (0.50, 1.16) |
| Age 40–44 | .31(.09, .97)* | 1.00 (--) | 0.65 (0.36, 1.16) | 0.68 (0.37, 1.28) |
| Age 45–54 | -- | 1.12 (.54, 2.32) | 0.85 (0.39, 1.83) | 0.76 (0.33, 1.74) |
| Survey | ||||
| NESARC | -- | -- | 1.00 (0.73, 1.38) | 0.85 (0.60,1.21) |
| Sex | ||||
| Female | .33(.29, .37)**** | .38(.34, .43)**** | 0.36(0.33, 0.39)**** | 0.44 (0.40, 0.49)**** |
| Race/Ethnicity | ||||
| Black | .68(.54, .85)*** | .92(.76, 1.12) | 0.79 (0.68, 0.91)**** | 1.04(0.89, 1.20) |
| Hispanic | .84(.61, 1.16) | .84(.64, 1.11) | 0.84 (0.66, 1.09) | 0.93 (0.70, 1.24) |
| Family background | ||||
| Parental alcohol | 1.84(1.62, 2.07)**** | 1.71(1.50, 1.95)**** | 1.77(1.63, 1.93)**** | 1.52(1.40, 1.67)**** |
| Age of drinking onset | -- | -- | -- | .93(.91,.94)**** |
| Lifetime abstention | -- | -- | -- | [dropped] |
| Current demographics | ||||
| Spouse present | -- | -- | -- | .86(.79,.94)*** |
| Currently employed | -- | -- | -- | .97(.88, 1.08) |
| Child under 13 | -- | -- | -- | .63(57,70)**** |
| Education | -- | -- | -- | .94(.92, .96)**** |
| Beer tax at 18 | -- | -- | -- | 1.01(.56, 1.82) |
| State per capita alcohol consumption at 18 | -- | -- | -- | 1.12(.94, 1.32) |
Notes: Odds ratio given in table, with 95% confidence interval in parentheses
Each column gives the result of one fixed-effect logistic regression; ‘MLDA’= Minimum Legal Purchase Age; coded 1 if responded could have legally purchased alcohol before age 21. Data source = respondents born in US 1948–1970, (n = 33,869) pooled from the 1991–1992 National Longitudinal Alcohol Epidemiological Survey (NLAES), and the 2001–2002 National Epidemiological Survey of Alcoholism and Related Conditions (NESARC). All models include indicators of state of residence and single year of birth as covariates; omitted categories are MLDA=21(exposure), NLAES (survey), male (sex), agegroup 20–29 (age in NLAES and combined sample), agegroup 40–44 (age in NESARC), neither parent had alcohol problem (parental alcohol) and non-Black, non-Hispanic (ethnicity).
Because extended model includes age of onset of drinking, 6054 lifetime abstainers are dropped from regression.
p < .10
p<.05
p<.01
p<.001
p<.0001
Table 3.
Minimum Legal Drinking Age Exposure and Past-year Drug Use Disorders
| Type of drug use disorder: | Marijuana | Other illegal drug | Marijuana or other drug | Alcohol, marijuana, or other drug |
|---|---|---|---|---|
| N | 33,026 | 33,604 | 33,869 | 33,869 |
| OR (95% c.i.) | OR (95% c.i.) | OR (95% c.i.) | OR (95% c.i.) | |
| Exposure | ||||
| MLDA<21 | 1.55 (.95, 2.52)# | 2.60(1.48, 4.58)** | 1.73(1.19. 2.49)** | 1. 33(1.22,1.46)**** |
| Age group: | ||||
| Age 30–34 | 0.75 (.40, 1.39) | 1.26(.59, 3.20) | 1.03 (0.58, 1.85) | 0.64 (0.48, .85)** |
| Age 35–39 | 0.85(.31, 2.32) | 1.68(.45, 6.24) | 1.22 (0.50, 2.94) | 0.75 (0.53, 1.09) |
| Age 40–44 | 1.14(.36, 3.63) | 2.33(.35,14,86) | 1.87 (0.59, 5.95) | 0.72 (0.41, 1.25) |
| Age 45–54 | 1.38(.27, 7.07) | 4.55(.33,, 62,70) | 2.49 (0.47, 13.08) | 0.94 (0.45, 1.99) |
| Survey | ||||
| NESARC | 0.54(..26, 1.13) | 0.64(.22, 1.85) | 0.53 (0.25, 1.09) | 0.96 (0.70,1.31) |
| Sex | ||||
| Female | 0.30(.25, .36)**** | 0.61(.48, .78)**** | 0.41 (0.34,0.49)**** | 0.37 (0.34, 0.40)**** |
| Race/Ethnicity | ||||
| Black | 0.95(.69, 1.31) | 1.27(.84, 1.93) | 1.11 (0.83,1.46) | .82(0.11, .94)** |
| Hispanic | 0.49(.31, .75)*** | 0.66(.36, 1.22)*** | 0.54 (0.37, .78)*** | 0.82 (0.65, 1.05) |
| Family background: | ||||
| Parental alcohol | 2.13(1.69, 2.67)**** | 2.43(1.87, 3.17)**** | 2.20(1.86,2.60)**** | 1.82(1.67,1.98)**** |
Notes: Results of logistic regression analyses; odds ratio given in table, with 95% confidence interval in parentheses. Outcome measures = presence or absence of past-year marijuana or other substance use disorder, using DSM-IV criteria. For other variable definitions and description of combined NLAES/NESARC sample, see notes for table 2
p < .10
p<.05
p<.01
p<.001
p<.0001
It has been suggested that decreased availability of alcohol might lead young adults to increase their use of other drugs, but Table 3 shows that exposures to lower MLDA’s were associated with significant increases in the risk of current substance use disorders in later adulthood. In column two, the association between a lower drinking age and any current illegal drug use disorder is statistically significant, and even larger than the association between MLDA exposure and alcohol use disorder (OR 1.70, 95% ci 1.19, 2.44, p =.003. In column three, the net association between MLDA exposure and past-year substance use disorder is slightly stronger than the association with alcohol use disorder alone (OR 1.33, 95% c.i. 1.21 to 1.45, p<.0001). Again, there is little change in the estimate in models that include age of drinking initiation or current demographic outcomes
MLDA effects in the age-restricted sample
In our strictest test for the effects of other unobserved social trends, Table 4 presents a similar set of analyses using the sample of respondents coming of age within two years of a law change. Columns one and two describe regression results predicting current alcohol use disorders, and columns three and four pertain to overall substance use disorders. In each pair of regressions, both the ‘short’ and ‘long’ models give estimates that are very similar to the estimates in Tables 2 and 3 using the full sample..
Table 4.
Minimum Legal Drinking Age Exposure and Past-year Alcohol or Substance Use Disorders Age-restricted sample (N=18,136)
| Alcohol Use Disorders |
Substance Use Disorders |
|||
|---|---|---|---|---|
| Model 1 |
Model 2 a |
Model 1 |
Model 2 |
|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| N | 18,136 | 15017 | 18,136 | 18,136 |
| Exposure | ||||
| MLDA<21 | 1.29 (1.06, 1.56)* | 1.28 (1.05, 1.55)* | 1.25 (1.05, 1.50)* | 1.25 (1.05, 1.49)* |
| Age group: | ||||
| Age 30–34 | 0.68 (0.48, .98)* | 0.67 (0.46, 0.98) | 0.67 (0.47, 0.97)* | 0.67 (0.45, 0.98)* |
| Age 35–39 | 0.65 (0.39, 1.10) | 0.66 (0.39, 1.12) | 0.67 (0.40, 1.12) | 0.68 (0.41, 1.14) |
| Age 40–44 | 0.63 (0.28, 1.46) | 0.65 (0.28, 1.50) | 0.65 (0.28, 1.51) | 0.67 (0.29, 1.57) |
| Age 45–54 | 0.75 (0.28, 2.01) | 0.78 (0.29, 2.08) | 0.78 (0.29, 2.15) | 0.82 (0.30. 2.24) |
| Survey | ||||
| NESARC | 1.18(0.74, 1.87) | 1.01(0.63, 1.60) | 1.14 (0.71, 1.82) | 0.98 (0.62, 1.57) |
| Sex | ||||
| Female | 0.35 (0.31, 0.40)**** | 0.42 (0.37, 0.48)**** | 0.36(0.32, .41)**** | 0.43(0.38, .49)**** |
| Race/Ethnicity | ||||
| Black | 0.88 (0.74, 1.05) | 1.15 (0.96, 1.37) | 0.89 (0.74, 1.07) | 1.15 (0.95, 1.38) |
| Hispanic | 0.77 (0.49, 1.24) | 0.87 (0.50, 1.50) | 0.73 (0.45, 1.17) | 0.82 (0.48, 1.41) |
| Family background | ||||
| Parental alcohol | 1.65(1.46, 1.87)**** | 1.45(1.27,1.,65)**** | 1.71(1.51,1.95)**** | 1.51(1.33, 1.72)**** |
| Initiation of drinking | ||||
| Age of onset | .93(.91, .95)**** | .93 (.91, .95)**** | ||
| Lifetime abstainer | -- | .09(.04, .19)**** | ||
Notes: Odds ratio given in table, with 95% confidence interval in parentheses
See notes for Table 2; in column 2, 3119 abstainers not used in calculation.
p < .10
p<.05
p<.01
p<.001
p<.0001
Similarity of MLDA effects among early- and later-onset drinkers and other subgroups
If MLDA laws were working primarily through age at initiation, then we might also expect that the association between MLDA exposure and later outcome would be stronger among the ‘compliant’ respondents whose (self-reported) drinking initiation conformed to the law. However, in supplementary analyses (not shown) the MLDA effect estimates were nearly identical among respondents who had already started to drink regularly before the age 16 - and among those who had not yet started to drink by age 16. There were also no significant additive or multiplicative interactions between exposure status and gender, age at assessment, ethnicity, survey, early or later birth cohort, or parental history of alcohol problems.
MLDA’s and cross-state migration
Finally, we tested whether cross-state migration could be a confounder of the apparent MLDA effect, using information about state of birth and state of residence in the NLAES and in the US Census. Supplementary figure 2 compares the proportion of respondents in the target cohort who were no longer living in their birth state in the 1991–92 NLAES sample and in the 1970 through 2000 US Census. We found that 63.1% of NLAES respondents were still living in their state of birth; 22.4 % were no longer living in their state of birth, but would have had no change in their MLDA status, and 14.5 % would have changed their MLDA exposure status in moving from birth state to present state. The trends were similar in the US Census, which shows two peaks in cross-state migration, the first between birth and age five, and the second between 18 and 21. Even in the large Census sample, respondents who would have been exposed to an earlier legal drinking age in their birth states were no more or less likely to migrate than respondents who would have been exposed to a later legal drinking age (logistic regression with birth year and birth state fixed effects: OR of 1.00, 95% c.i .93 to 1.07, p = .92), and in the NLAES sample, migration status was not a significant predictor of past-year alcohol or substance use disorder (OR 1.00, 95% c.i .87, 1.13, p = .88). Most importantly, in the NLAES sample, MLDA exposure based on state of birth was still a significant predictor of current alcohol or substance use disorder (e.g., alcohol use disorder, OR 1.15, 95% c.i. 1.02 to 1.31, p = .024), although the association was not as strong as the estimates based on current state of residence (Supplementary table 5)
DISCUSSION
MLDA laws in the US are still controversial, and though the vast majority of previous studies have found that changing MLDA’s did affect the frequency of heavy drinking, alcohol-related traffic crashes, and suicide among persons in the targeted age groups of 18 to 20, there have been recent claims that stricter MLDA laws may have worsened the incidence of clandestine binge drinking or other drug use, especially on college campuses (e.g., DiNardo and LeMieux 2001; Amethyst Initiative 2008), and concerns that stricter laws might have reduced the opportunities for ‘apprenticeship’ in responsible drinking (e.g., Rehm et al 2003). However, in the present study, we find that exposure to a younger legal purchase age is associated with more than a 30% increase in the odds of a past-year alcohol use disorder, even among respondents evaluated in their 40’s and 50’s. Remarkably, earlier MLDA exposure also predicts elevated risk for a past-year drug use disorder in middle adulthood. Approximately 51.8% of adults in our target cohort would have been allowed to purchase alcohol before the age of 21, and we found that MLDA exposure increased the odds of a current substance use disorder by 33%; together, these figures suggest that if the minimum legal purchase age had been set at 21 years in all states throughout the 1970’s and 1980’s, then the prevalence of past-year alcohol or substance abuse disorders among adults born in the US between 1948 and 1970 would have been about 14.6% lower than we observe it to have been over the past 20 years.1 Our estimates were similar for alcohol and other drug use disorders, for clinical diagnoses of both substance abuse and dependence, for both males and females, for blacks, Hispanics, and others, in all age groups, and among respondents who had already started to drink before the age of 16 as well as among those who had not.
This surprisingly strong association suggests that alcohol-related experiences in adolescence may have persistent effects on alcohol and substance use patterns, even into middle adulthood. However, the MLDA effects do not seem to be working through age of drinking initiation: although MLDA exposures did predict age of onset of regular and weekly drinking, the effect estimates for alcohol and substance use disorders were little changed in regression models that also included lifetime abstention status and age of initiation, and were similar and separately significant among subjects who had already started to drink by the age of 16 and among those who had not. Although age of onset may indeed be a causal risk factor for later substance use disorders, these results suggest that the long-term effects of MLDA exposures on harmful drinking may work through other aspects of late adolescent drinking, such as the intensity or patterning of drinking.. This ‘drinking pattern’ hypothesis is consistent with the many studies finding that more restrictive purchase ages do reduce the frequency and intensity of alcohol use among underage drinkers, even though underage drinking remains common (e.g., reviewed in Wagenaar and Toomey, 2002). Furthermore, it is plausible that the effects of MLDA laws on patterns of drinking among early-onset drinkers could be explained by the influence of MLDA laws on the behavior of their more law-abiding peers. For example, if young adults prefer to drink with friends than to drink alone, then even among respondents who had already begun to drink before age 18, a more restrictive purchase age could influence the frequency, activities, and social composition of the encounters around which people form enduring social relationships (Glaeser et al, 2003; Kremer and Levy, 2008).
What are we to make of the apparently increasing effects of MLDA exposure with age shown in figure 1? The regression models illustrated in figure 2 and supplementary table 4 suggest that after controlling for year of birth and state fixed effects, the MLDA effects are probably similar across age. However, an increasing effect with age would in fact be possible. For example, MLDA exposure might affect the persistence of alcohol problems, but not the incidence in early adulthood. It is also possible that DSM-IV criteria are better at discriminating ‘problem’ use from ‘normal’ use when evaluation occurs at later ages.
There are a number of important limitations to the present study. The 1970’s were a turbulent era, and MLDA laws were not the only social processes that might have affected lifetime patterns of alcohol and other substance use for cohorts coming of age in this period. However, we have greatly narrowed the range of possible explanations by comparing cohorts coming of age in the 1970’s (when drinking ages were being lowered) and in the 1980’s (when drinking ages were being raised again), and by comparing subjects close in age who were coming of age just before and after a change in state law. If the apparent MLDA effects are not attributable to changing drinking-age laws themselves, then they are due to an environmental factor closely tied to the timing of these changing laws.
There are also the usual problems associated with retrospective surveys, including social desirability and other possible reporting biases, limited information about the timing of law changes, but a particularly important concern is the lack of information about respondents’ state of residence at age 18. . Cross-state migration was common enough that it might have significantly affected our estimates; for example, if individuals at higher risk for alcoholism were more likely to have moved to a lenient-drinking-age state, then MLDA estimates based on current state of residence may overstate the effects of MLDA exposure on later outcomes. On the other hand, if cross-state migration wer uncorrelated with exposure status or other risk factors for alcoholism, then MLDA estimates based on current state of residence may have underestimated the full effect of MLDA exposure on later outcomes. In the NLAES sample, we found a statistically significant association between current alcohol or other substance use disorder and MLDA exposure calculated from state of birth; this provides a plausibly unbiased lower bound for our estimates, and suggests that selective migration cannot completely explain our results.
It is important to note that, except for coding related to the state of Louisiana, we have not tried to account for cross-state differences in law enforcement or ease of access to alcohol in neighboring states; furthermore, our law coding is based on secondary sources that did not distinguish between furnishing, purchase, possession, and consumption, we do not incorporate the effects of any within-state variation in local drinking ordinances, and (in part because of the uncertainty about state of residence at age 18) we did not distinguish between legal possession of alcohol at ages 18, 19, or 20. Never the less, our ‘reduced form’ analyses do provide an estimate of the average effects of changing MLDA exposures across the United States as they were actually implemented across states and years, and the consistency of our results across age at assessment, survey, gender, ethnicity, family background, and statistical approach provide overall reassurance about the meaningfulness of our findings. Longitudinal data with more exact information about state(s) of residence in late adolescence would control for selective migration, and would allow investigation of the relative importance of legal access to alcohol at specific ages. The interpretation of the DSM-IV constructs of substance abuse and dependence remain controversial (Day and Homish, 2002), and another useful step will be to study MLDA effects on other outcomes, including the quantity and frequency of drinking, adverse health events, employment, income, and family function.
This is the first study to document a long-term association between policies governing access to alcohol in young adulthood and risk of alcohol or substance use disorders in later adulthood. We find a clinically large and statistically robust association. For example, adults who would have been legally allowed to purchase alcohol before age 21 were about 33% more likely to have a past-year alcohol or drug use disorder than adults who could not legally purchase alcohol until age 21 (odds ratio 1.33, p < .0001), and the association persists even among respondents in their 40’s and 50’s. These surprisingly strong results are consistent with the hypothesis that late adolescence may be a ‘sensitive period’ for an environmental exposure closely tied to the timing of changing minimum legal purchase age laws. However, the MLDA effects do not seem to be working through age of drinking initiation, per se; instead, we hypothesize that the long term effects of MLDA exposure may work through the frequency and intensity of drinking or the social networks and social norms around drinking that develop in late adolescence. Estimates of the costs and benefits of alcohol control policies should consider long-term as well as short-term consequences of such policies. A better understanding of the mechanism linking MLDA exposures and later alcohol and substance use problems may also help to illuminate fundamental processes pertaining to adolescent development.
Supplementary Material
Figure S1: Proportion of respondents who had begun drinking regularly by specific ages, by minimum legal drinking age exposure. Combined NLAES-NESARC sample; respondents born in US between 1948 and 1970.. N=33,869
Figure S2: Proportion of respondents no longer living in state of birth, and proportion of respondents changing apparent MLDA exposure when calculated based on state of birth or state of current residence. US Census sample from 1% extracts of US Census, 1970–2000 (Ruggles et al, 2008); NLAES = National Longitudinal Alcohol Epidemiological Survey 1991–1992. Both NLAES and Census samples restricted to subjects born in US between 1948 and 1970.
Acknowledgments
We would like to thank Dan Feenberg, Stephan Pischke, Gautam Gowrisankaran, Robert Kaestner, Robert Pollak, three anonymous reviewers, and seminar participants at University of Illinois in Chicago, the NESARC research network, the Olin School of Business at Washington University, and Washington University School of Medicine and the spring 2009 Cohort Studies meeting of the NBER for many valuable comments. Christopher Carpenter and Bill Ponicki shared unpublished materials used in our law coding Leah Kemper provided research assistance. KEN, LJB and RAG designed the study, reviewed results and prepared the manuscript. All authors had full access to the data in the study. KEN conducted the analyses and takes responsibility for the integrity of the data and the accuracy of the data analysis. KEN and RAG declare no conflicts of interest. LJB is listed as an inventor on a patent (US 20070258898) held by Perlegen Sciences, Inc, covering the use of certain SNPs in determining the diagnosis, prognosis, and treatment of addiction, and has also acted as a consultant for Pfizer, Inc in 2008.
Funding sources included the Center for Health Policy, Washington University (KEN), NIH-k01DA16618 (RAG), R21DA026612 (RAG and KEN), and U10AA08401, HG-U01-004422, and K02DA021237 (LJB). Computing resources and technical support were also provided by the National Bureau of Economic Research.
Footnotes
Based on attributable risk calculation AR = [p(RR-1)]/([p(RR-1)]+1) X 100, where relative risk (RR) = 1.33, and the proportion of the population exposed to a lower MLDA = .518.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: 1994. [Google Scholar]
- [accessed October 2008];Amethyst Initiative. http://www.ameythstinitiative.org/statement.
- Angrist J, Pischke JP. Mostly Harmless Econometrics. Princeton University Press; Princeton, NJ: 2009. [Google Scholar]
- Arellano M. Computing Robust Standard Errors for Within-Groups Estimators. Oxford Bulletin of Economics and Statistics. 1987;49(4):431–434. [Google Scholar]
- Associated Press. Louisiana Court Upholds Drinking Age of 21. 1996. published in The New York Times, section A, page 17, July 3, 1996. [Google Scholar]
- Barron S, White A, Swartzwelder HS, Bell RL, Rodd ZA, Slawecki CJ, Ehlers CL, Levin ED, Rezvani AH, Spear LP. Adolescent vulnerabilities to chronic alcohol or nicotine exposure: findings from rodent models. Alcohol Clin Exp Res. 2005;29(9):1720–1725. doi: 10.1097/01.alc.0000179220.79356.e5. [DOI] [PubMed] [Google Scholar]
- Beer Institute. Brewer’s Almanac. 2008 Electronic text accessed 10/1/2008 at: www.beerinstitute.org.
- Birkmayer J, Hemenway D. Minimum-age drinking laws and youth suicide, 1970–1990. Am J Public Health. 1999;89:1365–1368. doi: 10.2105/ajph.89.9.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslow N, Day N. IIARC Scientific Publications No 32. Lyon, France: 1980. Statistical Methods in Cancer Research, Vol 1: the Analysis of Case-Control Studies. [PubMed] [Google Scholar]
- Carpenter CS, Kloska DD, O’Malley P, Johnston L. Alcohol Control Policies and Youth Alcohol Consumption: Evidence from 28 Years of Monitoring the Future. The BE Journal of Economic Analysis and Policy. 2007;7(1):25. [Google Scholar]
- Chen CM, Yi H, Falk D, Stinson F, Dawson D, Grant B. US Alcohol Epidemiologic Data Reference Manual. 1. Vol. 8. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2006. Alcohol use and alcohol use disorders in the United States: main findings from the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) [Google Scholar]
- Cook PJ. Paying the Tab: the Costs and Benefits of Alcohol Control. Princeton University Press; Princeton NJ: 2007. [Google Scholar]
- Cook PJ, Moore MJ. Environment and Persistence in Youthful Drinking Patterns. In: Gruber J, editor. Risky Behavior among youths: an economic analysis. University of Chicago Press; Chicago, Ill: 2001. pp. 375–437. [Google Scholar]
- Cook TD, Campbell DT. Quasi-Experimentation: Design & Analysis Issues for Field Settings. Houghton Mifflin Company; Boston, MA: 1979. [Google Scholar]
- Crews F, He J, Hodge C. Adolescent cortical development: a critical period of vulnerability for addiction. Pharmacol Biochem Behav. 2007;86(2):189–199. doi: 10.1016/j.pbb.2006.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day NL, Homish GG. The epidemiology of alcohol use, abuse, and dependence in Textbook. In: Tsuang MT, Tohen M, editors. Psychiatric Epidemiology. 2. John Wiley & Sons; New York, NY: 2002. pp. 459–477. [Google Scholar]
- Dee TS. State alcohol policies, teen drinking, and traffic fatalities. Journal of Political Economics. 1999;72(2):289–315. [Google Scholar]
- DiNardo J, Lemieux T. Alcohol, marijuana and American youth: the unintended consequences of government regulation. Journal of Health Economics. 2001;20(6):991–1010. doi: 10.1016/s0167-6296(01)00102-3. [DOI] [PubMed] [Google Scholar]
- DuMouchel W, Williams AF, Zador PL. Raising the alcohol purchase age: its effect on fatal motor vehicle crashes in twenty-six states. Journal of Legal Studies. 1987;16:249–266. [Google Scholar]
- Glaeser E, Sacerdote B, Scheinkman J. The Social Multiplier. Journal of the European Economics Association. 2003;1(2):345–353. [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou SP, Dufour M, Pickering RP. Prevalence of alcohol abuse and dependence: United States, 1992. Alcohol Health Res World. 1994;18:43–48. [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Age at onset of alcohol use and its association with alcohol abuse and dependence: results from the National Longitudinal Alcohol Epidemiologic Survey. J Subst Abuse. 1997;9:103–10. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Hasin DS. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-Version 2. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2001. [Google Scholar]
- Grant BF, Moore TC, Shepard J, Kaplan K. Source and Accuracy Statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2003. [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States 1991–1992 and 2001–2002. Drug and Alcohol Dependence. 2004;74(3):223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant JD, Scherrer JF, Lynskey MT, Lyons Mj, Eisen SA, Tsuang MT, True WR, Bucholz KK. Adolescent alcohol use is a risk factor for adult alcohol and drug dependence: evidence from a twin design. Psychol Med. 2006 Jan;36(1):109–118. doi: 10.1017/S0033291705006045. [DOI] [PubMed] [Google Scholar]
- Grossman M, Chaloupka FJ, Saffer H. The effects of Price on Alcohol Consumption and Alcohol-Related Problems. Alcohol Research and Health. 2002;26(1):22–34. [PMC free article] [PubMed] [Google Scholar]
- Grucza RA, Norberg KE, Bucholz KK, Bierut LJ. Correspondence between secular changes in alcohol dependence and age of drinking onset among women in the United States. Alcohol Clin Exp Res. 2008;32(8):1493–1501. doi: 10.1111/j.1530-0277.2008.00719.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, Winter MR. Age at drinking onset and alcohol dependence: age at onset, duration, and severity. Arch Pediatr Adolesc Med. 2006;160(7):739–46. doi: 10.1001/archpedi.160.7.739. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied Logistic Regression. John Wiley & Sons; New York, NY: 1989. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JB, Schulenber JE. College students and adults ages 19–45 (NIH Publication No 08-6418B) II. National Institute on Drug Abuse; Bethesda, MD: 2008. Monitoring the Future national survey results on drug use, 1975–2004. [Google Scholar]
- Kalbfleisch JD, Sprott DA. Application of likelihood methods to models involving large numbers of parameters (with discussion) JR Statist Soc B. 1970;32:175–208. [Google Scholar]
- Kremer M, Levy D. Peer effects and alcohol use among college students. Journal of Economic Perspectives. 2008;22(3):189–206. [Google Scholar]
- Kyprie K, Voas RB, Langley JD, Stephenson SCR, Begg DJ, Tippetts AS, Davie GS. Minimum purchase age for alcohol and traffic crash injuries among 15- to 19-year-olds in New Zealand. Am J Pub Health. 2006;96(1):126–131. doi: 10.2105/AJPH.2005.073122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenroot RK, Giedd JN. Brain development in children and adolescents: insights from anatomical magnetic resonance imaging. Neuroscience and Biobehavioral Reviews. 2006;30(6):718–729. doi: 10.1016/j.neubiorev.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22. [Google Scholar]
- Liu I, Blacker DL, Xu R, Fitzmaurice G, Lyons ML, Tsuang MT. Genetic and Environmental Contributions to the Development of Alcohol Dependence in Male Twins. Arch Gen Psychiatry. 2004;61:897–903. doi: 10.1001/archpsyc.61.9.897. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup D, Fetal Actual Causes of Death in the United States, 2000. JAMA. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Moore M, Cook PJ. NBER working paper No 5152. National Bureau of Economic Research; Cambridge, MA: 1995. Habit and heterogeneity in the youthful demand for alcohol. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Alcohol Policy Information System. 2009 http://www.alcoholpolicy.niaaa.nih.gov/
- National Institute on Alcohol Abuse and Alcoholism. US Alcohol Epidemiologic Data Reference Manual. 1. Vol. 8. Bethesda, MD: NIH; 2006. [Google Scholar]
- O’Malley P, Wagenaar A. Effects of minimum drinking age laws on alcohol use, related behavior and traffic crash involvement among American youth. J Stud Alcohol. 1991;52:478–491. doi: 10.15288/jsa.1991.52.478. [DOI] [PubMed] [Google Scholar]
- Pacula RL. Women and substance use: Are women less susceptible to addiction? American Economic Review. 1997;87(2):454–459. [Google Scholar]
- Pautassi RM, Myers M, Spear LP, Molina JC, Spear NE. Adolescent but Not Adult Rats Exhibit Ethanol-Mediated Appetitive Second-Order Conditioning. Alcohol Clin Exp Res. 2008;32(11):2016–2027. doi: 10.1111/j.1530-0277.2008.00789.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ponicki WR. National Institute on Alcohol Abuse and Alcoholism Research Center Grant P60-AA006282-23. Pacific Institute for Research and Evaluation Prevention Research Center; Berkeley, CA: 2004. Statewide Availability Data System II: 1933–2003. [Google Scholar]
- Ponicki WR, Gruenwald P, LaScala EA. Joint Impacts of Minimum Legal Drinking Age and Beer Taxes on US Youth Traffic Fatalities, 1975 to 2001. Alcohol Clin Exp Res. 2007;31(5):804–813. doi: 10.1111/j.1530-0277.2007.00363.x. [DOI] [PubMed] [Google Scholar]
- Prescott CA, Kendler KS. Age at first drink and risk for alcoholism: a noncausal association. Alcohol Clin Exp Res. 1999;23(1):101–107. [PubMed] [Google Scholar]
- Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction. 2003;98(9):1209–28. doi: 10.1046/j.1360-0443.2003.00467.x. [DOI] [PubMed] [Google Scholar]
- Robins L, Przybeck TR. Age of onset of drug use as a factor in drug and other disorders. in Etiology of Drug Abuse: Implications for Prevention. In: Jones CL, Battjes RJ, editors. US Dept of Health and Human Services, NIDA Research Monogram 56. Rockville, MD: 1985. pp. 178–192. [PubMed] [Google Scholar]
- Ruggles S, Sobek M, Alexander T, Fitch C, Goeken R, Hall PK, King M, Ronnander C. Integrated Public Use Microdata Series: Version 4.0 [Machine-readable database] Minneapolis, MN: Minnesota Population Center; 2008. [producer and distributor] http://usa.ipums.org/usa/ [Google Scholar]
- Scharnberg K. States weighing lower age to drink. Chicago Tribune. 2008 March;9:2008. [Google Scholar]
- Schults RA, Elder RW, Sleet DA, Nichols JL, Alao MO. Reviews of evidence regarding interventions to reduce alcohol-impaired driving. Am J Prev Med. 2001;21(4 suppl1):66–88. doi: 10.1016/s0749-3797(01)00381-6. [DOI] [PubMed] [Google Scholar]
- Stata Corporation. STATA (computer program) Version 10. College Station; Texas: 2007. [Google Scholar]
- Tambour S, Brown L, Crabbe J. Gender and Age at Drinking Onset affect Voluntary Alcohol Consumption but Neither the Alcohol Deprivation Effect nor the Response to Stress in Mice. Alcohol Clin Exp Res. 2008;32 (12):2100–2106. doi: 10.1111/j.1530-0277.2008.00798.x. [DOI] [PubMed] [Google Scholar]
- Vetter CS, Doremus-Fitzwater TL, Spear LP. Time course of elevated ethanol intake in adolescent relative to adult rats under continuous, voluntary-access conditions. Alcohol Clin Exp Res. 2007;31(7):1159–1168. doi: 10.1111/j.1530-0277.2007.00417.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagenaar AC. Legal minimum drinking age changes in the United States: 1970–1981. Alcohol Health and Research World. 1981/1982 Winter;:21–26. [Google Scholar]
- Wagenaar AC, Toomey TL. Effects of minimum drinking age laws: review and analyses of the literature from 1960 to 2000. J Stud Alcohol Suppl. 2002;(14):206–225. doi: 10.15288/jsas.2002.s14.206. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Sands E. Minimum-age laws and youthful drinking: An introduction. In: Wechsler H, editor. Minimum Drinking Age Laws. Lexington Books; Lexington, MA: 1980. pp. 1–10. [Google Scholar]
- World Health Organization (WHO) World Health Report 2002: reducing risks, promoting healthy life. World Health Organization; Geneva, Switzerland: 2002. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1: Proportion of respondents who had begun drinking regularly by specific ages, by minimum legal drinking age exposure. Combined NLAES-NESARC sample; respondents born in US between 1948 and 1970.. N=33,869
Figure S2: Proportion of respondents no longer living in state of birth, and proportion of respondents changing apparent MLDA exposure when calculated based on state of birth or state of current residence. US Census sample from 1% extracts of US Census, 1970–2000 (Ruggles et al, 2008); NLAES = National Longitudinal Alcohol Epidemiological Survey 1991–1992. Both NLAES and Census samples restricted to subjects born in US between 1948 and 1970.


