Abstract
The personality trait of conscientiousness is an important predictor of health and longevity. The present research examined how conscientiousness, in combination with educational attainment and health-related behaviours, predicted self-reported physical health across adulthood. These relations were investigated in two studies, one using a large, representative sample of Illinois residents (N = 617) and the other using a community sample with a multi-method assessment of conscientiousness (N = 274). Across both studies, structural path analyses provided evidence for a model wherein conscientiousness predicted health, in part, through its relationship to both educational attainment and health-related behaviours. The findings suggest conscientiousness predicts health through a diverse set of mechanisms including, but not limited to, educational attainment and health-related behaviours.
Keywords: conscientiousness, health, health-related behaviours, education, personality
Introduction
Conscientiousness refers to individual differences in the propensity to follow socially prescribed norms for impulse control, to be task- and goal-directed, to be planful, delay gratification, and follow social customs and rules (John & Srivastava, 1999). A number of studies clearly point to conscientiousness as an important predictor of mortality (Friedman et al., 1993; Weiss & Costa, 2005). In addition to predicting longevity, conscientiousness is negatively related to the experience of chronic illnesses such as diabetes, high blood pressure, arthritis, skin problems, strokes, ulcers and tuberculosis (Goodwin & Friedman, 2006; Marks & Lutgendorf, 1999). However, these associations are not explanations as to why these relations exist. Research needs to move beyond simply establishing the association between conscientiousness and health to evaluating the mechanisms through which conscientiousness affects health (Smith, 2006).
Educational attainment is accepted as an important contributor to better health and is positively correlated with multiple health outcomes and longevity (Adler et al., 1994; Adler, Marmot, McEwen, & Stewart, 1999; Elo & Preston, 1996; Hampson, Goldberg, Vogt, & Dubanoski, 2007). There is an accumulating evidence that conscientiousness plays a significant role in determining level of educational attainment. Specifically, conscientiousness is a robust predictor of academic achievement (Noftle & Robins, 2007) and, in turn, educational and occupational attainment (Judge, Higgins, Thoresen, & Barrick, 1999; Ozer & Benet-Martinez, 2006). By helping to shape educational attainment, conscientiousness contributes to a life path that promotes better health.
Conscientiousness also has important implications for health and longevity through its relationship to health-related behaviours. Health-related behaviours such as tobacco use, diet, level of physical activity, excessive alcohol use, shootings, sexual behaviour, risky driving/accidents and drug use are among the primary behavioural contributors to poor health outcomes such as cardiovascular disease, cancer and accidental death (Mokdad, Marks, Stroup, & Gerberding, 2004). Conscientiousness is negatively related to risky health behaviours such as alcohol and drug abuse (Walton & Roberts, 2004), as well as driving without a seatbelt and consuming illicit substances (Chuah, Drasgow, & Roberts, 2006). In turn, conscientiousness is positively related to preventive health behaviours, such as seeing a doctor regularly and checking smoke alarms (Chuah et al., 2006). A comprehensive meta-analyses of the relationship between conscientiousness and the leading behavioural contributors to mortality – alcohol use, disordered eating (including obesity), drug use, physical activity, risky sexual practices, risky driving practices, tobacco use, suicide and violence – demonstrated that conscientiousness was related to every category of health-related behaviour relevant to longevity (Bogg & Roberts, 2004). These findings indicate that people who are not conscientious have a number of ways by which they are at risk for poor health outcomes and that people who are conscientious have a number of ways by which they promote good health outcomes.
Recent empirical findings support the supposition that conscientiousness influences health outcomes through its relationship to education and health-related behaviours. In a sample of over 1000 participants assessed in grade school and again in midlife, teacher ratings of childhood conscientiousness impacted health status at midlife. The relationship of childhood conscientiousness to health was due, in part, to both educational attainment and health-related behaviours including physical activity, eating habits and smoking (Hampson et al., 2007).
The present research aims to provide further evidence for the mechanisms through which conscientiousness impacts health by using a modified transactional model that represents a blend of models proposed by Smith (2006) and Adler and Mathews (1994). In the current model, we propose that conscientiousness directly affects the types of the life paths people follow, which in turn affect health behaviours and health. Specifically, we hypothesise that conscientiousness will predict self-report physical health and that this relationship will be accounted for by the intervening variables of education, risky health-related behaviours and preventative health-related behaviours.
The present research examines this mediational model within two studies. Each study allows for a unique contribution to the existing literature on the relationship between conscientiousness and health outcomes. First, much of the existing research investigating the role of personality traits in the health process has not utilised systematic sampling procedures. To address this issue, Study 1 tests the proposed transactional model within an age-stratified sample selected to be representative of Illinois residents. Second, previous research has been predominantly mono-method, either relying exclusively on observer reports (Friedman et al., 1993) or self-reports (e.g. Weiss & Costa, 2005). To address this issue, Study 2 extends the model developed in Study 1 by reporting findings in which conscientiousness was assessed with multiple self-report indices as well as observer ratings to expand the assessment of conscientiousness beyond the mono-method design commonly used in studying the relationship between conscientiousness and health. With the addition of observer ratings of conscientiousness to the transactional model, we are able to address the possibility that Study 1 findings are due to shared method variance rather than to actual relationships among study variables.
Study 1
Method
Participants
A total of 351 female and 266 male (N = 617) participants participated in Study 1 from 2001 to 2004. Participants ranged in age from 19 to 86 years (M = 47.88, SD = 17.89) and were racially diverse (66.6% Caucasian, 16.5% African American, 5.8% Asian American, 4.9% Hispanic/Chicano/Mexican American, 2.9% Other, 2.4% Multiracial and 0.8% Native American).
Participants were contacted by interviewers from the University of Illinois at Chicago Survey Research Lab in their homes and asked to complete the survey on a laptop computer. The Study 1 sample is a multi-stage, age-stratified sample. In the first stage, nine Illinois counties were sampled with probabilities proportionate to size (PPS), where the measure of size is the adult population. PPS sampling gives more populous counties a higher probability of selection, while still ensuring that all counties have some probability of selection. In the second stage, five census tracts were sampled from each of the sampled counties. In the third stage, four residential blocks were sampled from the sampled census tracts. Census tracts and blocks were also sampled with PPS.
Once the blocks were selected, interviewers listed all households on the sampled blocks and completed interviews with five households. The response rate for the study was 13.3% with a cooperation rate of 38.2% and a refusal rate of 21.5%. The sample was stratified into three age strata: 20–39-year-old (N = 235), 40–59-year-old (N = 223) and those aged 60 years and above (N = 155). In order to ensure an equal number of completed interviews within each of these strata, selection procedures at the household level were adjusted to over-sample the smallest stratum.
Measures
Conscientiousness
Participants completed the nine scales that assess conscientiousness from the AB5C-IPIP (Goldberg, 1999) – conscientiousness (‘Am careful to avoid making mistakes’, M = 3.86, SD = 0.55, α = 0.77), efficiency (‘Finish what I start’, M = 3.71, SD = 0.68, α = 0.84), dutifulness (‘Follow directions’, M = 4.14, SD = 0.50, α = 0.78), purposefulness (‘Am not easily distracted’, M = 3.71, SD = 0.68, α = 0.80), organisation (‘Have an eye for detail’, M = 3.98, SD = 0.53, α = 0.80), cautiousness (‘Never spend more than I can afford’, M = 3.27, SD = 0.58, α = 0.71), rationality (‘Do things in a logical order’, M = 3.40, SD = 0.44, α = 0.58), perfectionism (‘Want everything to be done “just right”’, M = 3.59, SD = 0.66, α = 0.78) and orderliness (‘Work according to a routine’, M = 3.73, SD = 0.65, α = 0.78). These scales are comprised of 9–13 items and were rated on a five-point scale from strongly disagree (1) to strongly agree (5).
Educational attainment
Participants indicated their highest education level from some elementary school (1) to doctoral degree (9). Table 1 provides details on the percentage of participants at each level of educational attainment compared to national educational attainment statistics from the period of sampling (United States Census Bureau, 2003).
Table 1.
Educational attainment percentages for Study 1 participants, Study 2 participants, and a national sample (United States Census Bureau, 2003).
| Education level | Study 1 (N = 617) | Study 2 (N = 274) | National sample (N = 601, 051) |
|---|---|---|---|
| Some elementary school | 1.6 | 0.0 | 3.5 |
| Completed elementary school | 3.6 | 0.0 | 3.1 |
| Some high school | 10.5 | 1.8 | 10.0 |
| High school degree or equivalent | 25.3 | 8.9 | 31.9 |
| Some college/associates degree | 27.9 | 27.3 | 26.4 |
| Bachelor’s degree | 17.2 | 18.4 | 16.8 |
| Some graduate school | 1.8 | 11.0 | NA |
| Master’s degree | 8.4 | 19.5 | 5.7 |
| Professional degree | 3.2 | 9.9 | 2.5 |
| Unspecified | 0.5 | 3.2 | NA |
Health-related behaviours
Two measures were used to assess health-related behaviours. The Health Behaviour Checklist (HBC; Vickers, Conway, & Hervig, 1990) assessed the health-related behaviours of wellness maintenance (‘I see a doctor for regular checkups’, M = 3.43, SD = 0.76, α = 0.74), accident control (‘I learn first aid techniques’, M = 3.67, SD = 0.80, α = 0.59), traffic risk (‘I carefully obey traffic rules so I will not have accidents’ – reverse scored, M = 2.28, SD = 0.77, α = 0.67) and substance use (‘I do not smoke’ – reversed item, M = 2.16, SD = 1.09, α = 0.36). Participants responded to 26 items on a five-point scale of strongly agree (1) to strongly disagree (5).
Health-related behaviours were also assessed using scales and scale items drawn from the Behavioural Risk Factor Surveillance System (BRFSS; National Center for Chronic Disease Prevention and Health Promotion, 2000) and the Youth Risk Behaviour Surveillance System (YRBSS; National Center for Chronic Disease Prevention and Health Promotion, 1999). Scales assessing seven behaviours were administered to participants: cigarette consumption (‘During the past year, approximately how often did you smoke cigarettes?’, M = −0.04, SD = 0.56, α = 0.80), alcohol consumption (‘During the past year, on average, how many days per week did you have at least one drink of alcohol?’, M = 0.00, SD = 0.68, α = 0.83), illicit drug consumption (‘During the past year, how often did you use marijuana or hashish?’, M = 1.04, SD = 0.16, α = 0.68; two items assessing glue-sniffing and heroin use were excluded due to their low relationship to other drug use measures), violence (‘During the past year, how many times were you in a physical fight?’, M = 0.00, SD = 0.67, α = 0.68), physical activity (‘During the past year, approximately how many times per week did you exercise or participate in a physical activity for at least 20 min that made you sweat and breathe hard?’, M = 2.33, SD = 1.14, α = 0.61), eating patterns (‘During the past 7 days, how many times did you eat green salad?’, M = 2.41, SD = 0.69, α = 0.64), and risky driving (‘During the past year, how many times did you drive a car or other vehicle when you had been drinking alcohol?’, M = 0.74, SD = 1.20, α = 0.67). Participants also rated their sexual history and suicidal feelings as part of the BRFSS. However, the response rate on these questions was so low that we did not include them in the present analyses. Participants rated the frequency or quantity of activities within each domain. Items were averaged to form composite scores indicating greater or lesser frequency/quantity for each domain. For the alcohol and tobacco consumption scales, items were z-scored before the composite was computed because of different rating scales used for certain items.
In order to reduce the number of variables considered in the analyses, the health-related behaviour measures were factor analysed using Principal Axis Factoring. A two-factor solution best represented the data, with the factors split cleanly between risky health-related behaviours (eigenvalue = 3.21) and preventive health-related behaviours (eigenvalue = 1.66). This two-factor solution was present when using both Principle Components Analysis and Maximum Likelihood Factor Analysis and parallels prior research on the dimensionality of health-behaviours (Vickers et al., 1990). The risky health-related behaviour factor consisted of the alcohol consumption, tobacco consumption, drug consumption, risky driving and violence scales from the BRFSS and YRFSS and the substance use and traffic risk scales from the HBC. The preventive health-related behaviour factor consisted of the healthy eating and physical activity scales from the BRFSS and the wellness maintenance and accident control scales from the HBC.
Health Status
An abbreviated 33-item version of the Medical Outcomes Study (MOS) 36-item short-form health survey (SF-36; Ware & Sherbourne, 1992) was used to assess self-reported physical health status. The original 36-item SF-36 was consolidated from its original form to address only general health concerns. For example, the two items asking how much (1) physical health concerns and (2) emotional problems ‘cut down on the amount of time you spend on work or other activities’ were combined to just ask for, in general, agreement with the statement ‘The amount of time I have spent on work or other activities has been reduced’. This modification produced six subscales of the SF-36 dealing with general physical health status rather than emotional health status: general health perceptions (‘I am as healthy as anybody I know, M = 4.86, SD = 1.51, α = 0.65), physical functioning (‘Walking more than a mile’, M = 4.37.74, SD = 1.05, α = 0.83), role limitations due to physical problems (‘The amount of time I have spent on work or other activities has been reduced’, M = 5.14, SD = 1.24, α = 0.80), energy (‘I feel full of pep’, M = 4.45, SD = 1.65, α = 0.91), pain (‘Extent to which pain interfered with normal work’, M = 5.55, SD = 1.56, α = 0.79) and a single-item measure of social functioning (‘My health problems interfered with normal social activities’, M = 5.26, SD = 2.21). Each item was rated on a seven-point Likert scale reflecting frequency (1 = never, 7 = more than once a day) or agreement (1 = strongly disagree, 7 = strongly agree).
Analyses
All structural analyses were conducted in AMOS 7.0. In order to optimise model fit, the conscientiousness, health-related behaviour and health measures were parcelled using an item-to-construct balance technique (Little, Cunningham, Shahar, & Widaman, 2002). Variables within each parcel were averaged together to form the manifest variables used to construct the latent variables in the model. Conscientiousness facets were parcelled into three groups: (1) conscientiousness, dutifulness and rationality; (2) purposefulness, organisation and perfectionism and (3) efficiency, orderliness and cautiousness. The health-related behaviour scales loading on each factor were z-scored before parcelling. Risky health-related behaviours consisted of three parcels: (1) alcohol consumption and illicit drug consumption; (2) tobacco consumption and traffic risk and (3) risky driving, substance use and violence-related behaviour. Preventive health-related behaviours consisted of two parcels: (1) wellness and physical activity and (2) accident control and health habits. Finally, the six SF-36 subscales were parcelled to form three parcels: (1) social functioning and physical functioning; (2) general health and pain and (3) role limitations and energy. Model fit was assessed with the comparative fit index (CFI) and the root-mean square error of approximation (RMSEA) statistics. Chi-square difference testing was used to test model fit when comparing models. Gender, age and ethnicity were controlled for each model.
Results
Because we were interested in whether education and health behaviours mediated the relation between conscientiousness and health, we first tested the direct relation within a structural equation framework. As seen in Table 2, the direct relation between the latent trait of conscientiousness and the latent measure of physical health was 0.34 (p <0.05). We also tested the simple relations between the remaining variables and all were significantly related to appropriate outcomes with the exception of risky behaviours not predicting overall health. In terms of the mediational model, conscientiousness was positively related to education and preventive health-related behaviours and negatively related to risky health-related behaviours. Both education and preventive health-related behaviours were positively related to self-report health.1
Table 2.
Standardised estimates of structural coefficients for relations among conscientiousness, education, health-related behaviours and self-report physical health in Study 1.
| Path | Zero order | Model 1 | Model 2 |
|---|---|---|---|
| Conscientiousness → Physical health | 0.34* | 0.21* | |
| Conscientiousness → Education | 0.11* | 0.11* | 0.11* |
| Conscientiousness → Risky health behaviours | −0.12* | −0.11* | −0.11* |
| Conscientiousness → Preventive health behaviours | 0.44* | 0.49* | 0.43* |
| Education → Physical health | 0.29* | 0.12* | 0.18* |
| Education → Risky health behaviours | −0.17* | −0.15* | −0.15* |
| Education → Preventive health behaviours | 0.35* | 0.31* | 0.29* |
| Risky health behaviours → Physical health | −0.06 | 0.03 | 0.05 |
| Preventive health behaviours → Physical health | 0.41* | 0.45* | 0.24* |
| Model fit statistics | |||
| χ2 | 332.36 | 318.90 | |
| df | 68 | 67 | |
| CFI | 0.93 | 0.93 | |
| RMSEA | 0.08 | 0.08 | |
Notes: N = 617,
p <0.05.
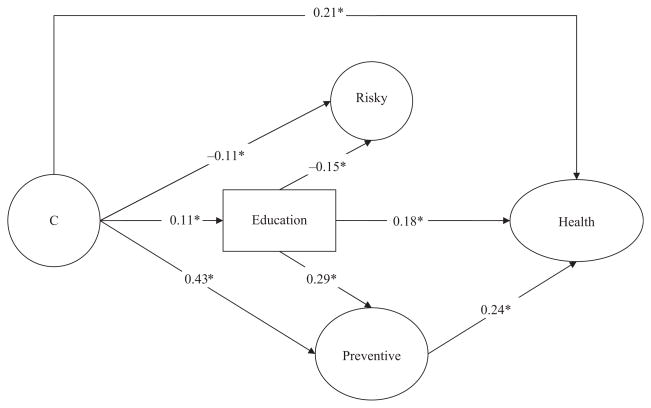
To examine the hypothesis that education and health-related behaviours mediated the relationship between conscientiousness and health, we compared a model without the direct path between conscientiousness and health (Model 1) to a model including this path (Model 2), while simultaneously including the effect of education and health behaviours on physical health. The full model had significantly better fit than did the model excluding the health-conscientiousness link, , p <0.05. Therefore, we cannot conclude that education and health-related behaviours fully mediate the relationship between conscientiousness and health. However, because the direct relation without considering mediators was significantly decreased by controlling for education and health-related behaviours (Z = 2.47, p <0.05), we can conclude that education and health-related behaviours partially mediated the conscientiousness-health path. Figure 1 presents the significant pathways of the full structural equation model depicting the relations among conscientiousness, education, health-related behaviours and self-report physical health while controlling for gender, age and ethnicity. The removal of any of the significant pathways in this model led to a significantly worse fit for the model.2
Figure 1.
Structural model showing relations among conscientiousness (C), education, risky and preventive health-related behaviours and self-report physical health in Study 1. *p <0.05.
Discussion
Study 1 provided support for the hypothesis that conscientiousness influences health, in part, because of its relationship to education and health-related behaviours. The effects of conscientiousness on health were partially mediated by education and health-related behaviours such that individuals who were more conscientious tended to be better educated and participate in more preventive health-related behaviours which, in turn, contributed to better physical health. Study 2 sought to extend the findings of Study 1 by using multiple methods to assess conscientiousness, which addresses the problem that shared method variance from self-reported traits and health could have inflated the nature and size of the associations observed in Study 1.
Study 2
Method
Participants
A total of 168 female and 104 male and 2 participants who did not report their gender (N = 274) were recruited from 2001 to 2003 through newspaper advertisements, flyers and postings on a list-serve serving the employees and retired employees of the University of Illinois. Advertisements asked for volunteers who were willing to participate in interviews about their life and complete several surveys in return for monetary compensation. Participants completed the measures described below as part of a larger battery of questionnaires assessing personality, health, daily behaviours and psychological well-being. Participants were reimbursed $8–$10 an hour. Participants ranged from 19 to 94 years of age (M = 51.25, SD = 16.43) and were primarily Caucasian (88%).
Measures
Self-reported conscientiousness
Two independent measures were used to assess self-report conscientiousness. First, participants rated themselves on the Conscientiousness Adjective Checklist (CAC; Jackson et al., in press). Participants rated five facets of conscientiousness: conventionality (M = 3.41, SD = 0.64, α = 0.64), reliability (‘dependable’, M = 4.48, SD = 0.48, α = 0.77), self-control (‘careful’, M = 3.81, SD = 0.58, α = 0.75), orderliness (‘neat’, M = 3.56, SD = 0.68, α = 0.82) and industriousness (‘thorough’, M = 3.91, SD = 0.54, α = 0.60). Participants also completed the nine scales that assess conscientiousness from the AB5C-IPIP as in Study 1 (Goldberg, 1999): conscientiousness (M = 3.94, SD = 0.52, α = 0.76), efficiency (M = 3.65, SD = 0.65, α = 0.83), dutifulness (M = 4.10, SD = 0.54, α = 0.83), purposefulness (M = 3.65, SD = 0.62, α = 0.84), organisation (M = 4.12, SD = 0.53, α = 0.86), cautiousness (M = 3.06, SD = 0.58, α = 0.73), rationality (M = 3.26, SD = 0.49, α = 0.62), perfectionism (M = 3.46, SD = 0.68, α = 0.80) and orderliness (M = 3.69, SD = 0.62, α = 0.80). Both measures were rated on a five-point scale from strongly disagree (1) to strongly agree (5).
Observer-rated conscientiousness
Observer ratings were obtained in two ways. The majority of participants supplied the contact information for one or more close associate (friends and family members). Close associates were contacted by phone and asked to complete a battery of measures including ratings of personality traits using the CAC measure described above in return for a small monetary reimbursement (Jackson et al., in press). In addition to the questionnaires described below, participants completed a structured McAdams Life Story Interview (McAdams, 1995) with a trained graduate student. The McAdams Life Story Interview contains a series of questions through which participants describe the story of their life, significant moments in their life (e.g. high point, low point, turning point), important characters in their life story, their future goals and personal beliefs and values. After the completion of the interview, the interviewer rated the participant on the CAC. Additionally, after listening to tape recordings of the interviews, trained undergraduate students also rated the participant on the CAC. A total of 1023 observer ratings were completed with a modal number of four ratings (M = 3.70) per participant. Observer ratings were averaged together to form a composite index of each of the five facets of conscientiousness from the ABC: conventionality (M = 3.41, SD = 0.64, ICC = 0.46), reliability (M = 4.07, SD = 0.62, ICC = 0.46), self-control (M = 3.72, SD = 0.57, ICC = 0.68), orderliness (M = 3.58, SD = 0.57, ICC = 0.34) and industriousness (M = 3.53, SD = 0.52, ICC = 0.39). Interclass-correlation coefficient (ICC) reliability ranged from 0.67 to 0.89. Agreement between close associate and student raters ranged between 0.21 and 0.35.
Educational attainment
Educational attainment was rated as described in Study 1. See Table 1 for comparison with national statistics.
Health-related behaviours
As given in Study 1, participants rated themselves on the four subscales of the HBC: wellness maintenance (M = 3.77, SD = 0.74, α = 0.77), accident control (M = 3.53, SD = 0.89, α = 0.73), traffic risk (M = 2.35, SD = 0.81, α = 0.74) and substance use (M = 2.11, SD = 0.93, α = 0.46) and six of the seven subscales of the BRFSS and YRBSS used in Study 1: cigarette consumption (M = 0.00, SD = 0.67, α = 0.99), alcohol consumption (M = 0.00, SD = 0.86, α = 0.83), illicit drug consumption (M = 0.05, SD = 0.19, α = 0.56), physical activity (M = 1.93, SD = 1.40, α = 0.62), eating patterns (M = 1.67, SD = 0.68, α = 0.64) and risky driving (M = 0.79, SD = 1.19, α = 0.78). Because 87% of the Study 2 sample reported no violence-related behaviours, this subscale was excluded from Study 2 analyses. Participants rated the frequency of activities within each domain. Items were z-scored and summed to form composite scores indicating greater or lesser risk for each domain. The two factor structure found in Study 1 was replicated in Study 2.
Health status
Physical health was assessed with the same SF-36 subscales used in Study 1: general health perceptions (M = 5.10, SD = 1.34, α = 0.65), physical functioning (M = 4.76, SD = 0.94, α = 0.83), role limitations due to physical problems (M = 5.21, SD = 1.18, α = 0.80), energy (M = 4.64, SD = 1.56, α = 0.91), pain (M = 5.60, SD = 1.36, α = 0.79) and a single-item measure of social functioning (M = 5.72, SD = 1.88).
Analyses
All analyses were conducted as in Study 1. Health-related behaviours and self-report physical health were parcelled as in Study 1 (with the exclusion of violence-related behaviours). Self-report conscientiousness facets were parcelled into three groups: (1) AB5C purposefulness, AB5C orderliness, ABC self-control, AB5C cautiousness and AB5C perfectionism; (2) AB5C efficiency, AB5C dutifulness, CAC orderliness, AB5C rationality and CAC conventionality and (3) AB5C conscientiousness, AB5C organisation, CAC industriousness and CAC reliability. Observer-rated conscientiousness facets were parcelled into two groups: (1) reliability, industriousness and conventionality and (2) self-control and orderliness.
Results
Paralleling Study 1 findings, zero-order correlations showed that both self-report and observer-rated conscientiousness were positively related to self-report physical health. In addition, self-report conscientiousness was positively related to preventive health-related behaviours and negatively related to risky health-related behaviours. Observer-rated conscientiousness was also negatively related to risky health-related behaviours as well as being positively related to level of educational attainment. In contrast to Study 1 findings, self-report conscientiousness was uncorrelated with education and observer-rated conscientiousness was uncorrelated with preventive health-related behaviours. Finally, Study 1 results were replicated in that education and preventive health-related behaviours were positively associated with health.
As in Study 1, we compared a model without the direct paths between conscientiousness and health (Model 1) to a model including these paths (Model 2), as shown in Table 3. The full model did not have significantly better fit than the model excluding the health-conscientiousness links, , p >0.05. However, because zero-order coefficients were not significantly decreased by controlling for education and health-related behaviours in the paths between either self-report (Z = 0.82, p >0.05) or observer-rated conscientiousness and health (Z = 1.22, p >0.05) we can, as in Study 1, only conclude that education and health-related behaviours partially mediate the conscientiousness-health paths. Figure 2 presents the significant pathways of the full structural model while controlling for gender, age and ethnicity. Excluding the removal of the path between observer-rated conscientiousness and health and the removal of the path between preventive health-related behaviours and health, the removal of significant pathways in this model led to a significantly worse fit for the model.3
Table 3.
Standardized estimates of structural coefficients for relations among conscientiousness, education, health-related behaviours, and self-report physical health in Study 2.
| Path | Zero order | Model 1 | Model 2 |
|---|---|---|---|
| S Conscientiousness → Physical health | 0.14* | 0.07 | |
| O Conscientiousness → Physical health | 0.26* | 0.16* | |
| S Conscientiousness → Education | 0.08 | −0.01 | −0.01 |
| S Conscientiousness → Risky health behaviours | −0.27* | −0.20* | −0.20* |
| S Conscientiousness → Preventive health behaviours | 0.33* | 0.41* | 0.39* |
| O Conscientiousness → Education | 0.40* | 0.39* | 0.40* |
| O Conscientiousness → Risky health behaviours | −0.40* | −0.34* | −0.34* |
| O Conscientiousness → Preventive health behaviours | 0.06 | 0.12 | 0.08 |
| Education → Physical health | 0.27* | 0.24* | 0.20* |
| Education → Risky health behaviours | −0.15* | −0.01 | −0.01 |
| Education → Preventive health behaviours | −0.01 | −0.01 | −0.01 |
| Risky health behaviours → Physical health | −0.15 | −0.07 | −0.01 |
| Preventive health behaviours → Physical health | 0.36* | 0.30* | 0.21* |
| Model fit statistics | |||
| χ2 | 216.03 | 211.48 | |
| Df | 91 | 89 | |
| CFI | 0.94 | 0.94 | |
| RMSEA | 0.07 | 0.07 | |
Notes: N = 274.
p <0.05.
Figure 2.
Structural model showing relations among self-report (SR C) and observer-rated conscientiousness (OBS C), education, risky and preventive health-related behaviours and self-report physical health outcomes in Study 2. *p <0.05.
General discussion
The two studies presented in the current research examined the way in which conscientiousness, educational attainment and health-related behaviours predict health using representative sampling techniques and multiple methods of assessing conscientiousness. Consistent with previous research, conscientiousness played a role in determining health. This relationship was explained, in part, by both education and health-related behaviours.
In both the studies conscientiousness was an important predictor of self-report health. While this relationship was not fully explained by the intermediate variables considered in the studies, both educational attainment and health-related behaviours accounted for a portion of the relationship between conscientiousness and health. Thus, our proposed transactional model was partially confirmed and we can conclude that conscientiousness helps individuals to shape their health in part by shaping their environment and their daily patterns of behaviour.
Educational attainment was an important predictor of self-report health in both studies. In addition, conscientiousness was related to educational attainment in both studies – though only observer-rated conscientiousness was related to education in Study 2. Education helps shape the conscientiousness-health link in two ways. First, education directly impacted health outcomes. It may be the case that people with more education are more likely to recognise illness and subsequently seek treatment (Gottfredson, 2004). Educational attainment also facilitates better access to medical resources, thereby promoting improved health outcomes (Fiscella, Franks, Gold, & Clancy, 2000). In addition to directly affecting health, in Study 1, education impacted health outcomes through preventive health-related behaviours. In the representative sample, people who were well educated engaged in preventive health-related behaviours. It may be that people who are better educated have more knowledge about the risks and benefits associated with various behaviours. While this indirect pattern was not present in Study 2, this may be due to sample differences with the Study 2 participants being significantly better educated than their Study 1 counterparts, t (889) = 2.92, p <0.05, with less variance in education level.
Preventive health-related behaviours were also related to health in the present research. In both studies, individuals who characterised themselves as being conscientious engaged in more preventive and less risky health-related behaviours. In addition, people who were rated as being conscientious by observers engaged in less risky health-related behaviours. Thus, conscientious individuals were more likely to engage in preventive health-related behaviours and less likely to engage in risky health-related behaviours as expected and, therefore, at least in the case of preventive health-related behaviours, had better self-reported physical health.
The present research provides a number of additional avenues for future research. First, while both studies had methodological strengths – Study 1’s representative sample and Study 2’s multiple-method approach to assessing conscientiousness – neither strength was replicated across studies. Ideally, future research would include both representative sampling and multiple methods of assessment. In addition, future research could benefit from extending multiple methods of assessment beyond just personality traits to encompass other target measures of study. For example, one of the most surprising findings in the present research was that risky health-related behaviours did not correspond to lower levels of self-report health. It may be the case that individuals who engage in risky health-related behaviours may not perceive and/or report expected levels of poor health. By including additional measures of health such as body-mass index, number of medical conditions and physician evaluations of health, future research may be able to establish risky health-related behaviours as a meaningful mediator of the relationship between conscientiousness and health.
One of the most prominent limitations of the present research was that it was cross-sectional and cannot address the causal pathways implied by the models tested. For example, it is quite possible that conscientiousness and educational attainment have a more reciprocal relationship than is implied within the present model. While conscientiousness certainly fosters educational attainment, greater education likely stimulates strengthening conscientiousness over time, in keeping with the correspondence principle of personality development (Caspi, Roberts, & Shiner, 1995; Roberts & Wood, 2006). Future research should extend the present work to follow the trajectories of personality, education, health-related behaviours and health over time.
In addition to the primary outcomes of the present research, two additional findings are of particular importance for planning future research into the mechanisms of the conscientiousness-health relationship. First, both self and observer reports of conscientiousness had independent effects on health. This complementarity suggests that the use of multiple measures of assessing personality is not redundant and, instead, adds a greater validity in predicting health. While the observer ratings of personality in Study 2 are not without fault – for example, the interjudge agreement of personality trait ratings was modest, in keeping with the majority of the literature on person perception (Funder, Kolar, & Blackman, 1995) – the marked difference between self and observer ratings of personality in the transactional model suggests that the commonly reported link between conscientiousness and health is not due to method variance. Given the present findings within a relatively small sample of adults, it is critical that future research investigating the mechanisms underlying important life outcomes examine individual differences and do so using multiple methods of assessment to capture the full nuance of personality characteristics.
Second, while the central finding of the present research was that conscientiousness may facilitate better health by fostering both educational attainment and protective health-related behaviours, there are many other factors that facilitate the relationship between conscientiousness and health. This is evidenced in both studies by only a partial mediation of the direct relationship between conscientiousness and health when controlling for education and health-related behaviours, replicating previous research (Hampson et al., 2007). Clearly, there are many other pathways between conscientiousness and health. The present research did not exhaustively assess every possible health behaviour and any number of additional health behaviours not considered in the present research may be involved in the path between conscientiousness and health. In addition, conscientiousness may be linked to basic psychophysiological mechanisms underlying good health (Segerstrom, 2000). Conscientiousness has also been linked to medical adherence, which is itself a robust predictor of health outcomes (Christensen & Smith, 1995). Conscientious individuals also may be able to avoid stressful situations and take actions to quickly ameliorate stress through effective coping strategies (Vollrath & Torgersen, 2000). Finally, conscientiousness is related to social support systems linked to better health including relationship and community involvement (Lodi-Smith & Roberts, 2007). These factors are not an exhaustive list and future research should continue to develop the critical mechanisms of the conscientiousness-health relationship.
Modern medicine operates on specific behavioural prescriptions for maintaining and developing good physical health. However, we are just beginning to understand the nuances underlying the ‘when and why’ of how these prescriptions benefit individuals. The present research suggests that factors that are commonly linked to health are, in part, determined by individual differences. Our hope for the future is that the present line of research, when combined with knowledge that individual differences can change in response to environmental presses, will help to promote a healthier culture not just through prescribing specific behaviours but through helping people shape their individual identity to a healthier personality profile.
Acknowledgments
This research was supported by a grant from National Institute of Aging (AG211778).
Footnotes
For both studies, a full correlation matrix of all of the manifest variables is available on request.
Participants were categorised as young adult (age 19–39, n = 235), middle aged (age 40–59, n = 223) or older adult (age 60–86, n = 155). Multiple-group analysis on these age groups showed that the full model (Model 2) was significantly moderated by age; , p <0.05. The anticipated mediational pathway was not present in young adult or middle-aged participants. Education and health-related behaviours partially mediated the conscientiousness-health path for older adults.
Participants were categorised as young adult (age 19–39, n = 66), middle aged (age 40–59, n = 127) or older adult (age 60–94, n = 80). Multiple-group analysis showed that, in contrast to the findings of Study 1 the full model (Model 2) was not significantly moderated by age; , p > 0.05. Mediational analysis within each age group did not differ from the overall mediational findings for the entire sample.
References
- Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL, et al. Socioeconomic status and health: The challenge of the gradient. American Psychologist. 1994;49:15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- Adler NE, Marmot M, McEwen B, Stewart J, editors. Socioeconomic Status and Health in Industrial Nations: Social, Psychological, and Biological Pathways. New York: New York Academy of Science; 1999. [PubMed] [Google Scholar]
- Adler N, Matthews K. Health psychology: Why do some people get sick and some stay well? Annual Review of Psychology. 1994;45:229–259. doi: 10.1146/annurev.ps.45.020194.001305. [DOI] [PubMed] [Google Scholar]
- Bogg T, Roberts B. Conscientiousness and health-related behaviors: A meta-analysis of the leading behavioral contributors to mortality. Psychological Bulletin. 2004;130:887–919. doi: 10.1037/0033-2909.130.6.887. [DOI] [PubMed] [Google Scholar]
- Caspi A, Roberts BW, Shiner RL. Personality development: Stability and change. Annual Review of Psychology. 1995;56:17.1–17.32. doi: 10.1146/annurev.psych.55.090902.141913. [DOI] [PubMed] [Google Scholar]
- Christensen AJ, Smith TW. Personality and patient adherence: Correlates of the fivefactor model in renal dialysis. Journal of Behavioral Medicine. 1995;18:305–313. doi: 10.1007/BF01857875. [DOI] [PubMed] [Google Scholar]
- Chuah S, Drasgow F, Roberts B. Personality assessment: Does the medium matter? No. Journal of Research in Personality. 2006;40:359–376. [Google Scholar]
- Elo IT, Preston SH. Educational differentials in mortality: United States, 1979–1985. Social Science & Medicine. 1996;42:47–57. doi: 10.1016/0277-9536(95)00062-3. [DOI] [PubMed] [Google Scholar]
- Fiscella K, Franks P, Gold MR, Clancy CM. Inequality in quality addressing socioeconomic, racial, and ethnic disparities in health care. Journal of the American Medical Association. 2000;283:2579–2584. doi: 10.1001/jama.283.19.2579. [DOI] [PubMed] [Google Scholar]
- Friedman H, Tucker JS, Tomlison-Keasey C, Schwartz J, Wingard D, Criqui M. Does childhood personality predict longevity? Journal of Personality and Social Psychology. 1993;65:176–185. doi: 10.1037//0022-3514.65.1.176. [DOI] [PubMed] [Google Scholar]
- Funder DC, Kolar DC, Blackman MC. Agreement among judges of personality: Interpersonal relations, similarity, and acquaintanceship. Journal of Personality and Social Psychology. 1995;69:656–72. doi: 10.1037//0022-3514.69.4.656. [DOI] [PubMed] [Google Scholar]
- Goldberg LR. A broad-bandwidth, public domain, personality inventory measuring the lower-level facets of several five-factor models. In: Mervielde I, Deary I, DeFruyt F, Ostendorf F, editors. Personality psychology in Europe. Vol. 7. Tilburg, The Netherlands: Tilburg University Press; 1999. pp. 7–28. [Google Scholar]
- Goodwin RD, Friedman HS. Health status and the five-factor personality traits in a nationally representative sample. Journal of Health Psychology. 2006;11:643–654. doi: 10.1177/1359105306066610. [DOI] [PubMed] [Google Scholar]
- Gottfredson LS. Intelligence: Is it the epidemiologists’ elusive “fundamental cause” of social class inequalities in health? Journal of Personality and Social Psychology. 2004;86:174–199. doi: 10.1037/0022-3514.86.1.174. [DOI] [PubMed] [Google Scholar]
- Hampson SE, Goldberg LR, Vogt TM, Dubanoski JP. Mechanisms by which childhood personality traits influence adult health status: Educational attainment and healthy behaviors. Health Psychology. 2007;26:121–125. doi: 10.1037/0278-6133.26.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson J, Walton K, Bogg T, Wood D, Harms P, Lodi-Smith J, et al. Not all conscientiousness scales change alike: A multi-method, multi-sample study of age differences in the facets of conscientiousness. Journal of Personality and Social Psychology. 2009;96:446–459. doi: 10.1037/a0014156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John OP, Srivastava S. The Big-Five trait taxonomy: History, measurement, and theoretical perspectives. In: Pervin L, John O, editors. Handbook of personality. Vol. 2. New York: Guilford Press; 1999. pp. 102–138. [Google Scholar]
- Judge TA, Higgins CA, Thoresen CJ, Barrick MR. The big five personality traits, general mental ability, and career success across the life span. Personnel Psychology. 1999;52:621–652. [Google Scholar]
- Little TD, Cunningham WA, Shahar G, Widaman KF. To parcel or not to parcel: Exploring the question, weighing the merits. Structural Equation Modeling. 2002;9:151–173. [Google Scholar]
- Lodi-Smith J, Roberts B. Social investment and personality: A meta-analysis of the relationship of personality traits to investment in work, family, religion, and volunteerism. Personality and Social Psychology Review. 2007;11:68–86. doi: 10.1177/1088868306294590. [DOI] [PubMed] [Google Scholar]
- Marks GR, Lutgendorf SK. Perceived health competence and personality factors differentially predict health behaviors in older adults. Journal of Aging and Health. 1999;11:221–239. doi: 10.1177/089826439901100205. [DOI] [PubMed] [Google Scholar]
- McAdams D. The life story interview. 1995 Retrieved February 3, 2009, from http://www.sesp.northwestern.edu/foley/instruments/interview/
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. Journal of the American Medical Association. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- National Center for Chronic Disease Prevention and Health Promotion. YRBSS: Youth Risk Behavior Surveillance System. 1999 Retrieved February 3, 2009, from http://www.cdc.gov/HealthyYouth/yrbs/
- National Center for Chronic Disease Prevention and Health Promotion. BRFSS: Behavioral Risk Factor Surveillance System. 2000 Retrieved February 3, 2009, from http://www.cdc.gov/brfss/
- Noftle E, Robins R. Personality predictors of academic outcomes: Big five correlates of GPA and SAT scores. Journal of Personality and Social Psychology. 2007;93:116–130. doi: 10.1037/0022-3514.93.1.116. [DOI] [PubMed] [Google Scholar]
- Ozer DJ, Benet-Martinez V. Personality and the prediction of consequential outcomes. Annual Review of Psychology. 2006;57:401–421. doi: 10.1146/annurev.psych.57.102904.190127. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Wood D. Personality development in the context of the neo-socioanalytic model of personality. In: Mroczek D, Little TD, editors. Handbook of Personality Development. Mahwah, New Jersey: Lawrence Erlbaum; 2006. pp. 11–39. [Google Scholar]
- Segerstrom SC. Personality and the immune system: Models, methods, and mechanisms. Annals of Behavioral Medicine. 2000;22:180–190. doi: 10.1007/BF02895112. [DOI] [PubMed] [Google Scholar]
- Smith TW. Personality as risk and resilience in physical health. Current Directions in Psychological Science. 2006;15:227–231. [Google Scholar]
- United States Census Bureau. Educational Attainment in the United States: 2003. 2003 Retrieved February 3, 2009, from http://www.census.gov/prod/2004pubs/p20-550.pdf.
- Vickers RR, Conway TL, Hervig LK. Demonstration of replicable dimensions of health behaviors. Preventive Medicine. 1990;19:377–401. doi: 10.1016/0091-7435(90)90037-k. [DOI] [PubMed] [Google Scholar]
- Vollrath M, Torgersen S. Personality types and coping. Personality and Individual Differences. 2000;29:367–378. [Google Scholar]
- Walton KE, Roberts BW. On the relationship between substance use and personality traits: Abstainers are not maladjusted. Journal of Research in Personality. 2004;38:515–535. [Google Scholar]
- Ware J, Sherbourne C. The MOS 36-item short-form health survey(SF-36) Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- Weiss A, Costa PT. Domain and facet personality predictors of all-cause mortality among Medicare patients aged 65 to 100. Psychosomatic Medicine. 2005;67:724–733. doi: 10.1097/01.psy.0000181272.58103.18. [DOI] [PubMed] [Google Scholar]