Abstract
Angiogenesis plays a key role in glioblastoma biology and antiangiogenic agents are under clinical investigation with promising results. However, the angiogenic profiles of patients with glioblastoma and their clinical significance are not well understood. Here we characterize the serum angiogenic profile of patients with glioblastoma, and examine the prognostic significance of individual angiogenic factors. Serum samples from 36 patients with glioblastoma were collected on admission and simultaneously assayed for 48 angiogenic factors using protein microarrays. The data were analyzed using hierarchical cluster analysis. Vessel morphology was assessed histologically after immunostaining for the pan-endothelial marker CD31. Tumor samples were also immunostained for tissue inhibitor of metalloproteinase-1 (TIMP-1). Cluster analysis of the serum angiogenic profiles revealed 2 distinct subtypes of glioblastoma. The 2 subtypes had markedly different tumor microvessel densities. A low serum level of TIMP-1 was associated with significantly longer survival independent of patient age, performance status, or treatment. The serum angiogenic profile in patients with glioblastoma mirrors tumor biology and has prognostic value. Our data suggest the serum TIMP-1 level as an independent predictor of survival.
Keywords: angiogenesis, glioma, invasion, metalloproteinase, tumor invasion
Glioblastomas are highly vascular tumors that secrete several angiogenic factors.1,2 There is a substantial body of evidence that angiogenesis is essential for the proliferation and survival of malignant glioma cells.3,4 It has therefore been suggested that inhibition of angiogenesis might be an effective therapeutic strategy. Recent preclinical and clinical data confirm that inhibiting angiogenic pathways in glioblastoma results in objective responses.5–8
The angiogenic characteristics of glioblastoma have been investigated at the tissue level using immunohistochemistry primarily analyzing the vascular endothelial growth factor (VEGF) and the VEGF receptor 2, basic fibroblast growth factor (bFGF) and its receptors and epidermal growth factor receptor (EGFR) and its mutant.9–12 Assaying for angiogenic factors in tumor specimens has the major disadvantage of requiring surgery to obtain the tumor sample. Therefore there is increasing interest in detecting circulating markers of tumor angiogenesis, which do not require tumor sampling. Circulating markers may be soluble or cellular and can be measured noninvasively at any stage of treatment. The assessment of the concentrations of circulating angiogenic factors is potentially beneficial as a surrogate marker of the efficacy of antiangiogenic treatments and as a prognostic indicator. For example, the plasma level of bFGF in glioblastoma patients was reduced following successful antiangiogenic chemotherapy with the anti-VEGF agent cediranib.13 Such assessments might be most valuable in determining biological change in the tumor, particularly in the context of developed resistance to angiogenic chemotherapy.14 Despite the mounting interest in detecting circulating tumor angiogenic factors, little is known about the serum angiogenic signature of patients with glioblastoma.
Angiogenic profiling has several advantages over the detection of individual angiogenic factors.15 These relate to the opportunity to study multiple points in a given metabolic pathway and multiple pathways at the same time. Lack of reliance on a single detected marker may therefore improve the reliability of a test that looks at a biological process as a whole rather than at a single point. Additionally, given that protein profiling may study a whole pathway or a series of points along a pathway, there is the potential to evaluate biological characteristics of tumors more fully. Proteomic and more recently genetic profiling of glioblastoma tissue has been used successfully to define tumor subgroups.16,17 These techniques also suffer from the disadvantage of requiring tissue samples. It is unclear, however, whether serum angiogenic profiles are as informative as tissue angiogenic profiles. Many angiogenic proteins that function in a paracrine or autocrine manner have short half-lives, due to either serum degradation or hepatic metabolism that may make their serum levels extremely small when compared with levels in the tumor itself. Additionally, many, if not all, angiogenic factors are not exclusive to 1 tumor type, and so the serum measurements may be confounded by other biological processes in the patient. Here we determined serum angiogenic profiles in patients with glioblastoma. Our data indicate that serum angiogenic profiles provide important information about tumor biology. Serum angiogenic profiles can be used to classify glioblastomas into distinct histological subgroups and identify novel prognostic indicators. Some angiogenic factors, however, which carry significant biological information when detected in tumor tissue, are noninformative when assayed in the serum.
Methods
Serum Collection
Our study was preapproved by the Wandsworth Research Ethics Committee. Venous blood samples were collected preoperatively in plain 7 mL tubes from 36 newly diagnosed patients with glioblastoma and 5 control patients who were admitted to the Department of Neurosurgery at St George's Hospital in London. The control patients were admitted for elective spinal surgery for degenerative disease and had no history of malignancy. The samples were left for 60 minutes at room temperature and were then centrifuged at 80 g for 15 minutes. The supernatant (serum) was collected, aliquoted, and stored at −80°C. All patients received 16 mg of dexamethasone per day for at least 48 hours before the blood sample collection. The patients then had surgery (craniotomy with >75% debulking of the enhancing tumor or burrhole biopsy), followed by fractionated radiation therapy of 60 Gy at 4 weeks and temozolomide at 75 mg/m2 daily for 6 weeks, followed by 150–200 mg/m2 for 5 days per month, as tolerated, for 6 months of adjunctive treatment. Clinical data including age, extent of resection, Karnofsky performance score (KPS) at diagnosis, adjuvant treatment, and overall survival from diagnosis were recorded. All glioblastoma patients died during the course of this study.
Serum Angiogenic Factor Assays
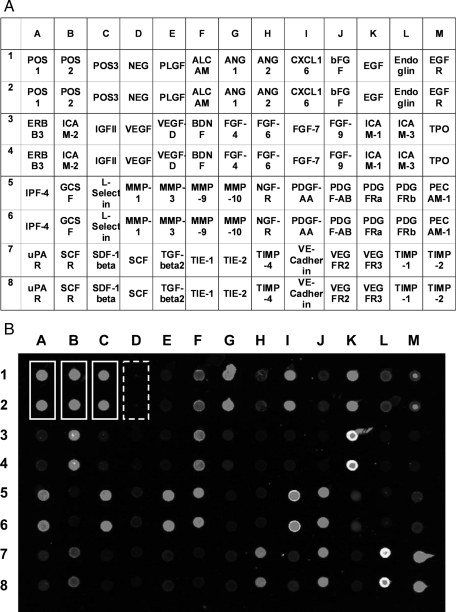
The serum samples were thawed and analyzed using protein arrays (Custom G-series Human Cytokines Antibody Array, RayBiotech, Inc., USA). Each sample was simultaneously assayed for 48 angiogenic factors, chosen for their implication in glioblastoma pathogenesis. We used 13 arrays in total with 48 factors per slide (Fig. 1A). The arrays were processed according to the manufacturer's instructions and 50 μL of undiluted thawed serum was added to each well and incubated overnight with biotin-conjugated antibodies.18 Streptavidin was then added to the antigen–antibody complex. The arrays were read using a GenePix 4000b reader (MDS Analytical Technologies USA) and GenePix Pro version 6.1.0.4 at a photomultiplier tube voltage of 600 kV to produce a signal fluorescence intensity for each spot (Fig. 1B).
Fig. 1.
Protein microarrays. (A) The table shows the position of each angiogenic protein on the protein microarray. (B) Single patient array of 52 duplicated spots comprising 4 control pairs, 3 positive (white boxes) and 1 negative (white dashed box), and 48 protein pairs implicated in glioblastoma angiogenesis.
Protein Array Data Analysis
The signal intensity generated from each spot was analyzed using XLStat Pro version 2007 (Addinsoft USA and Microsoft USA, 2007) and WinStat (R. Fitch Software, USA, 2009). The intensities for each duplicated assay were averaged to a single reading. The 3 pairs of positive control spots within each array, consisting of biotinylated protein only, were averaged. These averages were then used to normalize the intensity readings of all spots within each array. The coefficient of variation (CV) for each angiogenic factor was determined by repeating 48-factor arrays for 5 samples. The CV ranged from 3% to 173%. Only the 20 most reproducible factors (with CV < 25%) were used for cluster analysis (Table 1).
Table 1.
The 20 most reproducible serum angiogenic factors ranked according to their CV (%)
| Factor | Serum level for better prognosis | CV (%) | Univariate, P | Multivariate, P |
|---|---|---|---|---|
| NGF-R | Lower | 3.3 | .42 | .83 |
| VEGFR3 | Lower | 3.9 | .49 | .45 |
| ALCAM | Lower | 4.0 | .30 | .43 |
| VEGF | Lower | 5.8 | .39 | .31 |
| TIMP-1 | Lower | 5.9 | .05 | .01 |
| PECAM-1 | Lower | 7.7 | .35 | .63 |
| ICAM-3 | Higher | 7.9 | .44 | .30 |
| TIE-1 | Lower | 9.3 | .39 | .26 |
| FGF-9 | Higher | 10.6 | .30 | .23 |
| MMP-10 | Lower | 10.7 | .35 | .62 |
| TIE-2 | Lower | 13.4 | .48 | .66 |
| SCF | Lower | 15.5 | .53 | .12 |
| PDGFRa | Higher | 16.6 | .69 | .30 |
| TIMP-2 | Higher | 20.4 | .67 | .91 |
| PDGF-AA | Higher | 22.6 | .21 | .48 |
| VEGFR2 | Lower | 22.9 | .60 | .32 |
| bFGF | Lower | 23.2 | .27 | .23 |
| FGF-7 | Lower | 23.3 | .42 | .71 |
| Ang1 | Lower | 23.8 | .16 | .13 |
| FGF-4 | Lower | 23.9 | .42 | .65 |
The table also shows the univariate and multivariate prognostic value of each factor (P value) calculated using Cox regression. In the multivariate analysis the P value was adjusted for patient age, sex, Karnofsky score, and adjuvant treatment.
Factors excluded from further analysis due to high CV (>25%): ICAM-1. PLGF, FGF-6, SDF-1 beta, TPO, MMP-9, TIMP-4, Ang2, ERBB3, CXCL16, uPAR, TGF-beta2, VE-CADHERIN, Endoglin, BDNF, ICAM-2, MMP-3, SCF-R, GCSF, MMP-1, PDGF AB, EGFR, L-Selectin, VEGF-D, IPF-4, PDGFRb, IFG II, EGF.
Bold indicates factor with P < 0.05.
A Pearson similarity matrix was constructed based on these 20 most reliable proteins. From this matrix an unsupervised agglomerative hierarchical clustering technique (XLStat version 2007, Addinsoft USA and Microsoft USA, 2007) was used to establish whether the profile of these 20 proteins would group the patients into distinct groups based on their angiogenic signature. The groups of patients were then analyzed for survival using the Kaplan–Meier log-rank test.
Tumor Microvessel Density
For 5 patients from each angiogenic cluster, 4-μm sections from the formalin-fixed paraffin embedded (FFPE) tumor specimens were immunostained for the pan-endothelial marker CD31 using a monoclonal mouse antibody at 1:40 dilution at room temperature for 30 minutes (Dako), followed by horseradish peroxidase–linked antimouse secondary antibody (Dako), 1:30 for 30 minutes at room temperature. Immunostaining was visualized brown with diaminobenzidine (DAB) as chromogen. Sections were counterstained with hematoxylin. Human tonsil was used as positive control, and negative controls (primary antibody omitted) were performed for all samples. These sections were then visualized using a Zeiss Axiom system at low power (×40), high resolution (30 Mb), and the Tagged Image File Format–files were analyzed using ImageJ (version 1.4, NIH Freeware) according to a previously described color deconvolution process to segment out immunolabeled blood vessels.19,20 The segmented, binarized image was visually compared with the original image to confirm that blood vessels were reliably selected with minimal background staining. These segmented images were then automatically analyzed for small, medium, and large blood vessels, considered as clusters of pixels ≤49 (roughly corresponding to microvessel diameter of <10 μm), 50–99 pixels (10–15 μm), and ≥100 pixels (>15 μm). The numbers of blood vessels were normalized according to the area of tumor tissue and averaged across 5 different, randomly selected low-power fields per patient to give microvessel density (MVD) per unit tumor area in each low-power field.
Tissue Inhibitor of Metalloproteinase-1 Immunohistochemistry
FFPE sections from all 21 patients for whom sufficient tissue samples were available were immunostained for tissue inhibitor of metalloproteinase-1 (TIMP-1) using monoclonal mouse antibody (Novocastra, Leica UK) diluted 1:500 for 30 minutes at room temperature followed by horseradish peroxidase–linked antimouse secondary antibody (DakoCytomation, Denmark) 1:30 for 30 minutes at room temperature. Immunoreactivity was visualized brown with DAB and nuclei were counterstained with hematoxylin. The staining protocol was optimized using human small intestine. Five different fields selected at random from each sample were then scored by an observer who was unaware of the nature of each specimen. Each of the 5 fields received a score from 1 to 5 for overall TIMP-1 positivity modified from Aaberg-Jessen et al.21: 1 = no positive staining, corresponding to <2% positive cells, 2 = minimal focal positivity in widely separated areas (2–10% positive cells), 3 = marked positivity in separated areas (10–25% positive cells), 4 = marked positivity in confluent areas (25–50% positive cells), and 5 = marked positivity throughout (>50% positive cells). Examples of the different scores are shown in Fig. 3A. These scores were added to give an aggregate score between 5 and 25.
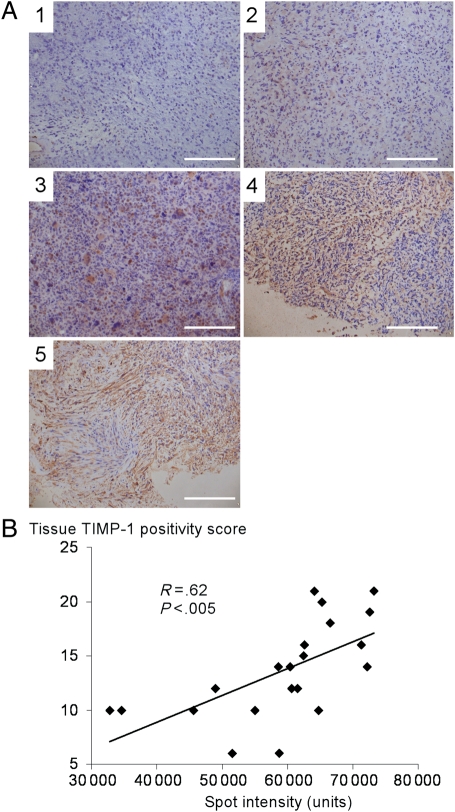
Fig. 3.
TIMP-1 expression in glioblastoma tissue. (A) Glioblastoma sections immunostained brown for TIMP-1 to illustrate the histological scoring system. 1 = no positive staining, corresponding to <2% positive cells, 2 = minimal focal positivity in widely separated areas, (2–10% positive cells), 3 = marked positivity in separated areas, (10–25% positive cells), 4 = marked positivity in confluent areas (25–50% positive cells), and 5 = marked positivity throughout (>50% positive cells). (B) Serum TIMP-1 spot intensity vs tissue TIMP-1 immunopositivity score (range 5–25) showing positive correlation. Bar = 100 μm (A1–A5).
Statistical Analysis
Kaplan–Meier survival curves were plotted for the 2 major clusters of glioblastoma patients as determined by their serum angiogenic profiles. Differences between the MVDs of each cluster were assessed using the analysis of variance (ANOVA) test for serial correlation. A Cox regression model was used to establish if any serum angiogenic proteins were individually predictive for survival either in univariate or multivariate analysis. Independent variables were classified as patient age in years, sex, KPS at presentation, extent of surgical resection (biopsy vs >75% debulking), and adjuvant treatment (none, radiotherapy only, radiotherapy and temozolomide).
Results
Glioblastoma Patient Characteristics
Of the 36 patients studied, 12 (33%) were female and 24 (67%) male. The mean age at presentation was 60 years (range 41–77) and 25 (69%) patients had a KPS at presentation ≥70, denoting independence. Biopsy or volume reduction surgery was undertaken in 31 (86%) patients, and 5 (14%) underwent gross total resection. Eight patients (22%) underwent no further treatment after biopsy, 22 patients (61%) received radiotherapy alone, and 6 (17%) received radiotherapy and temozolomide. The median survival was 30.5 weeks from diagnosis.
Assay Reproducibility
Reproducibility of the assays was quantified in 2 ways. First, since all spots on each array are duplicated, we calculated the correlation coefficient (R) between them. Reproducibility between individual assays was high, with correlation coefficient values of 0.98 or greater with a CV between duplicated assays of 9%. Assays were run in batches of 13 patient sera with high correlation within batches. Variability between arrays was more reliable for some factors and less reliable for others; in particular we found that the measurements of EGF, insulin-like growth factor–II and platelet-derived growth factor receptor–beta (PDGFRb) were poorly reproducible. Table 1 lists the angiogenic factors with CV < 25%. For subsequent analyses we included only the 20 factors with CV < 25%.
Analysis of Individual Angiogenic Factors
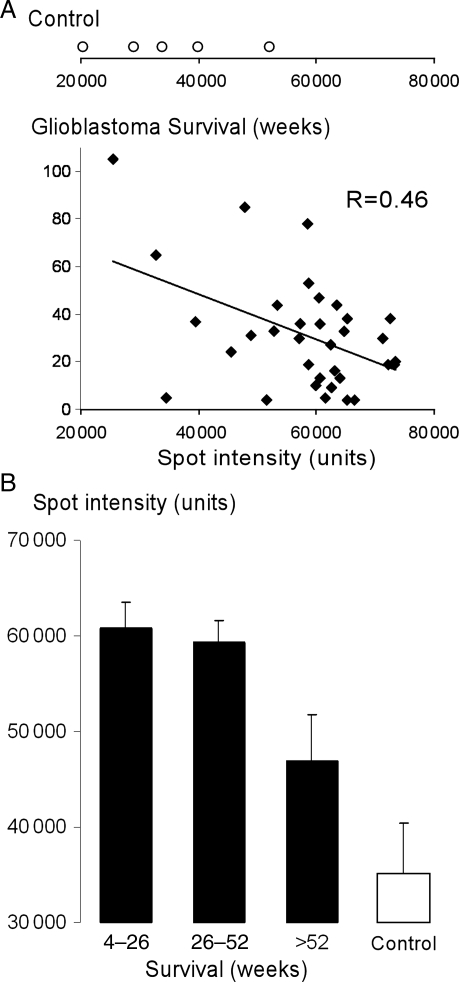
A Cox regression multivariate model was used to determine the survival predictive value of patient-related factors. We found that a better KPS at presentation, younger age, >75% resection, and adjuvant treatment with radiotherapy and temozolamide all predicted better survival, in keeping with previous series.22–24 Of the 48 serum angiogenic factors assayed, only TIMP-1 was correlated with survival, with a higher serum level associated with shorter survival (hazard ratio = 3.2 per 20 000 intensity units increase in TIMP-1; 95% CI 1.2–16.4, P = .01) independent of the other prognostic factors. This is also shown by the negative correlation between the TIMP-1 level and survival in glioblastoma patients (Fig. 2). TIMP-1 was one of the most reproducible factors (CV = 5.9%).
Fig. 2.
Serum TIMP-1 and survival. (A) Top: TIMP-1 spot intensity of nonglioblastoma control patients. Bottom: TIMP-1 spot intensity vs survival (weeks) for each glioblastoma patient. (B) TIMP-1 spot intensity for short (4–26 weeks, n = 15), medium (26–52 weeks, n = 14), and long (>52 weeks, n = 7) survival glioblastoma patients and nonglioblastoma controls (n = 5) (mean ± standard error).
We also compared the serum levels of the 20 most reproducible angiogenic factors in the 36 patients with glioblastoma vs the 5 control patients. The levels of 5 of 20 factors (platelet derived growth factor–AA, TIMP-1, PDGFRa, Ang1, and TIMP-2) were significantly different between the glioblastoma and the control patients (Table 2). The levels of the remaining 15 of 20 factors were not significantly different between the 5 control and 36 glioblastoma patients. The mean serum level of TIMP-1 was markedly lower in the control vs the glioblastoma patients (Fig. 2A), including the longest (>52 weeks) surviving group of glioblastoma patients (Fig. 2B).
Table 2.
Serum levels (normalized spot intensity units) of the 20 angiogenic factors with CV <25% in 36 patients with glioblastoma vs 5 control patients
| Angiogenic factor | Serum level in glioblastoma patients | Serum level in control subjects | P |
|---|---|---|---|
| PDGF-AA | 49 512 ± 1661 | 24 392 ± 3171 | .0000 |
| TIMP-1 | 56 982 ± 1866 | 35 103 ± 5306 | .0001 |
| PDGFRa | 3486 ± 831 | 12 099 ± 997 | .0003 |
| Ang1 | 20 804 ± 1205 | 8912 ± 1610 | .0005 |
| TIMP-2 | 40 315 ± 1298 | 32 935 ± 5298 | .0349 |
| SCF | 1640 ± 364 | 544 ± 48 | .1368 |
| VEGFR2 | 11 900 ± 571 | 10 155 ± 1179 | .1412 |
| bFGF | 2747 ± 424 | 1509 ± 102 | .1443 |
| PECAM-1 | 2888 ± 543 | 1323 ± 35 | .1474 |
| VEGF | 793 ± 136 | 409 ± 23 | .1529 |
| FGF-9 | 816 ± 189 | 327 ± 22 | .1725 |
| FGF-4 | 2640 ± 637 | 1187 ± 123 | .2029 |
| FGF-7 | 1992 ± 512 | 905 ± 55 | .2191 |
| TIE-1 | 1688 ± 420 | 811 ± 119 | .2230 |
| TIE-2 | 2098 ± 510 | 1040 ± 88 | .2246 |
| VEGFR3 | 1922 ± 480 | 987 ± 79 | .2386 |
| NGF-R | 1841 ± 466 | 1008 ± 80 | .2569 |
| ALCAM | 7819 ± 791 | 6666 ± 391 | .2974 |
| MMP-10 | 1642 ± 297 | 1398 ± 83 | .3820 |
| ICAM-3 | 853 ± 194 | 809 ± 71 | .4671 |
Values are mean ± SEM.
The glioblastoma and control groups were compared using the two-tailed t-test.
TIMP-1 Immunohistochemistry
To determine whether the TIMP-1 levels in the serum correlate with the TIMP-1 expression in the tumor, we immunostained the FFPE tumor samples for TIMP-1 (Fig. 3). We observed marked variability in TIMP-1 immunoreactivity between the samples. Characteristic TIMP-1 positivity could be seen around microvessels in some samples. In other samples, the interstitium as well as the endothelium stained positive; positive tumor cells were also seen. In some, despite clear features of glioblastoma (glomeruloid vascular proliferation and densely packed tumor cells), there was no appreciable TIMP-1 positivity. The overall TIMP-1 immunoreactivity score (range 5–25) was positively correlated with the TIMP-1 intensity from serum analysis with the Pearson correlation coefficient 0.62 (95% CI 0.12–0.83, P < .005; Fig. 3B).
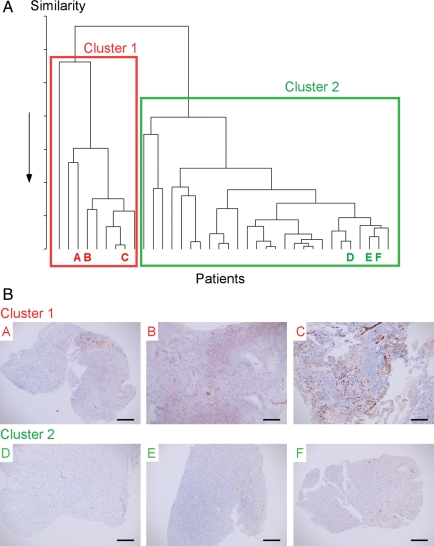
Analysis of Angiogenic Profiles
Cluster analysis revealed 2 distinct clusters, termed Cluster 1 and Cluster 2, consisting of 9 and 27 patients, respectively (Fig. 4A). Median survival was not significantly different between the 2 clusters, at 36 weeks for Cluster 1 and 30 weeks for Cluster 2. Since the 2 patient groups generated by cluster analysis have distinct angiogenic profiles, we reasoned that their respective tumors should also have different vascularities (Fig. 4B). We therefore compared MVDs between Cluster 1 and Cluster 2 for large (>15 μm diameter equivalent to >100 CD31 positive pixels), medium (10–15 μm diameter equivalent to 50–99 CD31 positive pixels), and small (<10 μm diameter equivalent to <50 CD31 positive pixels) vessels (Fig. 5A). MVD data for the 3 vessel size groups were analyzed by ANOVA, which suggested overall significantly (P < .01) higher MVD in Cluster 1 vs Cluster 2 (Fig. 5B). Taken together, these findings indicate that cluster analysis of serum angiogenic profiles can be used to define biologically distinct glioblastoma subtypes.
Fig. 4.
Cluster analysis of serum angiogenic profiles. (A) Dendrogram classifying the 36 glioblastoma patients into 2 major clusters (Cluster 1 [red, 9 patients] and Cluster 2 [green, 27 patients]) according to the serum levels of the 20 most reproducible (CV less than 25%) angiogenic proteins. (B) Sections of glioblastoma tissue from 3 patients in each cluster (Patients A, B, C [from Cluster 1]) and Patients D, E, F [from Cluster 2]) immunostained brown for CD31. Bar = 200 μm (all panels).
Fig. 5.
MVD of glioblastoma tumors from the 2 clusters. (A) Left: CD31-immunostained glioblastoma showing blood vessels (brown, arrowed) with “Right” same section after color deconvolution and thresholding to segment out the blood vessels (arrows). (B) Left: Number of microvessels per unit tumor area in each low-power field for small (<49 pixels approximately <10 μm diameter), medium (50–99 pixels ∼10–15 μm diameter), and large (>100 pixels approximately >15 μm diameter) blood vessels. Right: Overall % of CD31 immunopositive pixels. Both panels: Cluster 1 (black bar) and Cluster 2 (white bar). (Mean ± standard error). Bar = 200 μm (A).
Discussion
This study investigates the clinical value of serum markers of angiogenesis in glioblastoma obtained preoperatively. We have demonstrated that cluster analysis of multiple angiogenic factors may be used to define groups of tumors with microvascular differences. We have also shown that the level of TIMP1 in the serum at first admission is independently prognostic.
Previous studies have evaluated the role of individual serum angiogenic factors in glioblastoma patients. Rafat et al.25 showed that levels of serum VEGF and granulocyte-macrophage colony stimulating factor are raised in patients with glioblastoma when compared with healthy controls. Two further studies found that the serum levels of VEGF, bFGF, endostatin, and thrombospondin-1 in glioblastoma patients did not predict survival.26–28 In agreement with these studies, our data also indicated that the serum levels of VEGF, bFGF, and 45 other individual angiogenic factors or their soluble receptors (Table 1) do not individually have significant prognostic value. There are several reasons why the serum levels of individual angiogenic factors do not have prognostic value. Some factors may have short serum half-lives and cannot be reproducibly measured under the conditions of our assay, as indicated by high coefficients of variation. Factors with high coefficients of variation were therefore excluded from our analysis. The serum levels of some angiogenic factors may be influenced by a high hepatic degradation rate. Angiogenic protein sequestration in platelets has also been observed.29 All of these issues may produce significant disparity between the level of an angiogenic factor in tumor tissue vs serum.
A novelty of our work is the simultaneous measurement of many serum angiogenic factors. Rather than using individual angiogenic factors to subclassify glioblastomas, which may be inaccurate, we used many factors to identify tumors with distinct angiogenic profiles. We used unsupervised cluster analysis to identify 2 subgroups of glioblastoma. Cluster analysis classifies glioblastomas based on differences in multiple factors that may even be statistically insignificant when used individually.30 The different angiogenic profiles were associated with markedly different tumor tissue vascularities. We chose MVD as an index of tumor vascularity, which is easily quantified by an automated technique. We found that the 2 subgroups of glioblastoma had significantly different microvessel densities. Other indices of tumor vascularity, not studied here, may also differ between the glioblastoma subgroups. For example, we did not look for the presence of a few large glomeruloid tufts vs several morphologically normal vessels, which was previously associated with better prognosis.31
Our data suggest that, in glioblastoma patients, a higher serum TIMP-1 level at presentation predicts shorter survival and that TIMP-1 levels in the glioblastoma patients are significantly higher than in normal controls. We included TIMP-1 in the array of proteins studied due to its previous implication in glioma angiogenesis.32 TIMP-1 expression also simulates the production of VEGF in other carcinoma models.33 The finding that serum TIMP-1 is prognostic for survival is novel in glioblastoma. This finding agrees with Aaberg-Jessen et al.,21 who have recently shown that high TIMP-1 immunoreactivity in glioblastoma tissue predicts shorter patient survival. Our experiments show that the serum level of TIMP-1 positively correlates with TIMP-1 expression in the tumor tissue. High TIMP-1 expression also predicts shorter patient survival in several other tumor types. For example, overexpression of TIMP-1 is an independent marker of shorter survival in patients with non-small-cell lung cancer, and increased levels of TIMP-1 in the plasma were predictive of poor survival in breast and colorectal cancer.34–36 Higher serum levels of TIMP-1 have also been associated with shorter survival in metastatic breast cancer.37 TIMP-1, a natural inhibitor of matrix metalloproteinase (MMP) enzymes, inhibits in vitro and in vivo tumor cell invasion38 and binds several members of the metalloproteinase family. TIMP-1 is also a metastasis suppressor gene.39 In general, the expression of TIMPs is coordinated with that of MMPs. Thus, the activated MMPs are locally inhibited rapidly by TIMPs, and the degradation of extracellular matrix is tightly regulated.40 The finding that inhibition of MMP-2 causes decreased invasion suggests that TIMP-1 should improve survival.41 The significant inverse relationship between TIMP-1 and survival in our glioblastoma series and several other tumor types34–37 suggests that TIMP-1 may have activity beyond that of an MMP inhibitor. Recently TIMP-1 upregulation has been shown to be involved in mechanisms of developed resistance to anti-VEGF treatment and it is therefore likely to become more important in future glioblastoma research.42
Conclusions
We conclude that measuring multiple angiogenic factors in the serum of patients with glioblastoma defines biologically distinct tumor subtypes. Although the serum levels of some angiogenic factors cannot be reproducibly measured using proteomic techniques, measurement of the serum level of some factors was highly reproducible. Serum TIMP-1 concentration correlated directly with tumor tissue TIMP-1 expression and inversely with patient survival.
Funding
M.C. is funded by the Neurosciences Research Foundation, the London Deanery, and the St George's Hospital Charitable Trust. W.A. and A.H. are supported by Cancer Research UK (CRUK) grant number C309/A8274.
Acknowledgments
We are grateful to Kay Elderfield for histological expertise.
Conflict of interest statement. None declared.
References
- 1.Kirsch M, Schackert G, Black PM. Anti-angiogenic treatment strategies for malignant brain tumors. J Neurooncol. 2000;50:149–163. doi: 10.1023/a:1006487412567. doi:10.1023/A:1006487412567. [DOI] [PubMed] [Google Scholar]
- 2.Anderson JC, McFarland BC, Gladson CL. New molecular targets in angiogenic vessels of glioblastoma tumors. Expert Rev Mol Med. 2008;10:e23. doi: 10.1017/S1462399408000768. doi:10.1017/S1462399408000768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jensen RL. Brain tumor hypoxia: tumorigenesis, angiogenesis, imaging, pseudoprogression, and as a therapeutic target. J Neurooncol. 2009;92:317–335. doi: 10.1007/s11060-009-9827-2. doi:10.1007/s11060-009-9827-2. [DOI] [PubMed] [Google Scholar]
- 4.Chi AS, Sorensen AG, Jain RK, Batchelor TT. Angiogenesis as a therapeutic target in malignant gliomas. Oncologist. 2009;14:621–636. doi: 10.1634/theoncologist.2008-0272. doi:10.1634/theoncologist.2008-0272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kreisl TN, Kim L, Moore K, et al. Phase II trial of single-agent bevacizumab followed by bevacizumab plus irinotecan at tumor progression in recurrent glioblastoma. J Clin Oncol. 2009;10:740–745. doi: 10.1200/JCO.2008.16.3055. doi:10.1200/JCO.2008.16.3055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zuniga RM, Torcuator R, Jain R, et al. Efficacy, safety and patterns of response and recurrence in patients with recurrent high-grade gliomas treated with bevacizumab plus irinotecan. J Neurooncol. 2009;91:329–336. doi: 10.1007/s11060-008-9718-y. doi:10.1007/s11060-008-9718-y. [DOI] [PubMed] [Google Scholar]
- 7.Schiff D, Purow B. Bevacizumab in combination with irinotecan for patients with recurrent glioblastoma multiforme. Nat Clin Pract Oncol. 2008;5:186–187. doi: 10.1038/ncponc1077. doi:10.1038/ncponc1077. [DOI] [PubMed] [Google Scholar]
- 8.Martens T, Laabs Y, Günther HS, et al. Inhibition of glioblastoma growth in a highly invasive nude mouse model can be achieved by targeting epidermal growth factor receptor but not vascular endothelial growth factor receptor-2. Clin Cancer Res. 2008;14:5447–5458. doi: 10.1158/1078-0432.CCR-08-0147. doi:10.1158/1078-0432.CCR-08-0147. [DOI] [PubMed] [Google Scholar]
- 9.Shinojima N, Tada K, Shiraishi S, et al. Prognostic value of epidermal growth factor receptor in patients with glioblastoma multiforme. Cancer Res. 2003;63:6962–6970. [PubMed] [Google Scholar]
- 10.Puputti M, Tynninen O, Sihto H, et al. Amplification of KIT, PDGFRA, VEGFR2, and EGFR in gliomas. Mol Cancer Res. 2006;4:927–934. doi: 10.1158/1541-7786.MCR-06-0085. doi:10.1158/1541-7786.MCR-06-0085. [DOI] [PubMed] [Google Scholar]
- 11.Hassler M, Seidl S, Fazeny-Doerner B, et al. Diversity of cytogenetic and pathohistologic profiles in glioblastoma. Cancer Genet Cytogenet. 2006;166:46–55. doi: 10.1016/j.cancergencyto.2005.08.021. doi:10.1016/j.cancergencyto.2005.08.021. [DOI] [PubMed] [Google Scholar]
- 12.Felsberg J, Rapp M, Loeser S, et al. Prognostic significance of molecular markers and extent of resection in primary glioblastoma patients. Clin Cancer Res. 2009;15:6683–6693. doi: 10.1158/1078-0432.CCR-08-2801. doi:10.1158/1078-0432.CCR-08-2801. [DOI] [PubMed] [Google Scholar]
- 13.Batchelor TT, Sorensen AG, di Tomaso E, et al. AZD2171, a pan-VEGF receptor tyrosine kinase inhibitor, normalizes tumor vasculature and alleviates edema in glioblastoma patients. Cancer Cell. 2007;11:83–95. doi: 10.1016/j.ccr.2006.11.021. doi:10.1016/j.ccr.2006.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ellis LM, Hicklin DJ. Pathways mediating resistance to vascular endothelial growth factor-targeted therapy. Clin Cancer Res. 2008;14:6371–6375. doi: 10.1158/1078-0432.CCR-07-5287. doi:10.1158/1078-0432.CCR-07-5287. [DOI] [PubMed] [Google Scholar]
- 15.Jain RK, Duda DG, Willett CG, et al. Biomarkers of response and resistance to antiangiogenic therapy. Nat Rev Clin Oncol. 2009;6:327–338. doi: 10.1038/nrclinonc.2009.63. doi:10.1038/nrclinonc.2009.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Whittle IR, Short DM, Deighton RF, Kerr LE, Smith C, McCulloch J. Proteomic analysis of gliomas. Br J Neurosurg. 2007;21:576–582. doi: 10.1080/02688690701721691. doi:10.1080/02688690701721691. [DOI] [PubMed] [Google Scholar]
- 17.Verhaak RG, Hoadley KA, Purdom E, et al. Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR, and NF1. Cancer Cell. 2010;17:98–110. doi: 10.1016/j.ccr.2009.12.020. doi:10.1016/j.ccr.2009.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. http://www.raybiotech.com/manual/antibody%20array/AAH-CYT-G.pdf. Accessed Jan 25, 2010.
- 19.Rasband WS, Image J. Bethesda, Maryland, USA: U. S. National Institutes of Health; http://rsb.info.nih.gov/ij/ 1997–2009. [Google Scholar]
- 20.Ruifrok AC, Johnston DA. Quantification of histochemical staining by color deconvolution. Anal Quant Cytol Histol. 2001;23:291–299. [PubMed] [Google Scholar]
- 21.Aaberg-Jessen C, Christensen K, Offenberg H, et al. Low expression of tissue inhibitor of metalloproteinases-1 (TIMP-1) in glioblastoma predicts longer patient survival. J Neurooncol. 2009;95:117–128. doi: 10.1007/s11060-009-9910-8. doi:10.1007/s11060-009-9910-8. [DOI] [PubMed] [Google Scholar]
- 22.Lacroix M, Abi-Said D, Fourney DR, et al. A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg. 2001;95:190–198. doi: 10.3171/jns.2001.95.2.0190. doi:10.3171/jns.2001.95.2.0190. [DOI] [PubMed] [Google Scholar]
- 23.Laws ER, Parney IF, Huang W, et al. Survival following surgery and prognostic factors for recently diagnosed malignant glioma: data from the Glioma Outcomes Project. J Neurosurg. 2003;99:467–473. doi: 10.3171/jns.2003.99.3.0467. doi:10.3171/jns.2003.99.3.0467. [DOI] [PubMed] [Google Scholar]
- 24.Stupp R, Mason WP, van den Bent MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352:987–996. doi: 10.1056/NEJMoa043330. doi:10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- 25.Rafat N, Beck GC, Schulte J, Tuettenberg J, Vajkoczy P. Circulating endothelial progenitor cells in malignant gliomas. J Neurosurg. 2010;112:43–49. doi: 10.3171/2009.5.JNS081074. doi:10.3171/2009.5.JNS081074. [DOI] [PubMed] [Google Scholar]
- 26.Kesari S, Schiff D, Doherty L, et al. Phase II study of metronomic chemotherapy for recurrent malignant gliomas in adults. Neuro Oncol. 2007;9:354–363. doi: 10.1215/15228517-2007-006. doi:10.1215/15228517-2007-006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peles E, Lidar Z, Simon AJ, Grossman R, Nass D, Ram Z. Angiogenic factors in the cerebrospinal fluid of patients with astrocytic brain tumors. Neurosurgery. 2004;55:562–567. doi: 10.1227/01.neu.0000134383.27713.9a. doi:10.1227/01.NEU.0000134383.27713.9A. [DOI] [PubMed] [Google Scholar]
- 28.Fine HA, Figg WD, Jaeckle K, et al. Phase II trial of the antiangiogenic agent thalidomide in patients with recurrent high-grade gliomas. J Clin Oncol. 2000;18:708–715. doi: 10.1200/JCO.2000.18.4.708. [DOI] [PubMed] [Google Scholar]
- 29.Klement GL, Yip TT, Cassiola F, et al. Platelets actively sequester angiogenesis regulators. Blood. 2009;19:2835–2842. doi: 10.1182/blood-2008-06-159541. doi:10.1182/blood-2008-06-159541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Miller DJ, Wang Y, Kesidis G. Emergent unsupervised clustering paradigms with potential application to bioinformatics. Front Biosci. 2008;13:677–690. doi: 10.2741/2711. doi:10.2741/2711. [DOI] [PubMed] [Google Scholar]
- 31.Sharma S, Sharma MC, Sarkar C. Morphology of angiogenesis in human cancer: a conceptual overview, histoprognostic perspective and significance of neoangiogenesis. Histopathology. 2005;46:481–489. doi: 10.1111/j.1365-2559.2005.02142.x. doi:10.1111/j.1365-2559.2005.02142.x. [DOI] [PubMed] [Google Scholar]
- 32.Groft LL, Muzik H, Rewcastle NB, et al. Differential expression and localization of TIMP-1 and TIMP-4 in human gliomas. Br J Cancer. 2001;85(1):55–63. doi: 10.1054/bjoc.2001.1854. doi:10.1054/bjoc.2001.1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yoshiji H, Harris SR, Raso E, et al. Mammary carcinoma cells over-expressing tissue inhibitor of metalloproteinases-1 show enhanced vascular endothelial growth factor expression. Int J Cancer. 1998;75:81–87. doi: 10.1002/(sici)1097-0215(19980105)75:1<81::aid-ijc13>3.0.co;2-g. doi:10.1002/(SICI)1097-0215(19980105)75:1<81::AID-IJC13>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 34.Gouyer V, Conti M, Devos P, et al. Tissue inhibitor of metalloproteinase 1 is an independent predictor of prognosis in patients with nonsmall cell lung carcinoma who undergo resection with curative intent. Cancer. 2005;15:1676–1684. doi: 10.1002/cncr.20965. doi:10.1002/cncr.20965. [DOI] [PubMed] [Google Scholar]
- 35.Ree AH, Florenes VA, Berg JP, Maelandsmo GM, Nesland JM, Fodstad O. High levels of messenger RNAs for tissue inhibitors of metalloproteinases (TIMP-1 and TIMP-2) in primary breast carcinomas are associated with development of distant metastases. Clin Cancer Res. 1997;3:1623–1628. [PubMed] [Google Scholar]
- 36.Holten-Andersen MN, Stephens RW, Nielsen HJ, et al. High preoperative plasma tissue inhibitor of metalloproteinase-1 levels are associated with short survival of patients with colorectal cancer. Clin Cancer Res. 2000;6:4292–299. [PubMed] [Google Scholar]
- 37.Lipton A, Ali SM, Leitzel K, et al. Elevated plasma tissue inhibitor of metalloproteinase-1 level predicts decreased response and survival in metastatic breast cancer. Cancer. 2007;15:1933–1939. doi: 10.1002/cncr.22637. doi:10.1002/cncr.22637. [DOI] [PubMed] [Google Scholar]
- 38.Fillmore HL, VanMeter TE, Broaddus WC. Membrane-type matrix metalloproteinases (MT-MMPs): expression and function during glioma invasion. J Neurooncol. 2001;53:187–202. doi: 10.1023/a:1012213604731. doi:10.1023/A:1012213604731. [DOI] [PubMed] [Google Scholar]
- 39.Che G, Chen J, Liu L, et al. Transfection of nm23-H1 increased expression of beta-Catenin, E-Cadherin and TIMP-1 and decreased the expression of MMP-2, CD44v6 and VEGF and inhibited the metastatic potential of human non-small cell lung cancer cell line L9981. Neoplasma. 2006;53:530–537. [PubMed] [Google Scholar]
- 40.Ylisirniö S, Höyhtyä M, Mäkitaro R, et al. Elevated serum levels of type I collagen degradation marker ICTP and tissue inhibitor of metalloproteinase (TIMP) 1 are associated with poor prognosis in lung cancer. Clin Cancer Res. 2001;7:1633–1637. [PubMed] [Google Scholar]
- 41.Kargiotis O, Chetty C, Gondi CS, et al. Adenovirus-mediated transfer of siRNA against MMP-2 mRNA results in impaired invasion and tumor-induced angiogenesis, induces apoptosis in vitro and inhibits tumor growth in vivo in glioblastoma. Oncogene. 2008;14:4830–4840. doi: 10.1038/onc.2008.122. doi:10.1038/onc.2008.122. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 42.Lucio-Eterovic AK, Piao Y, de Groot JF. Mediators of glioblastoma resistance and invasion during antivascular endothelial growth factor therapy. Clin Cancer Res. 2009;15:4589–4599. doi: 10.1158/1078-0432.CCR-09-0575. doi:10.1158/1078-0432.CCR-09-0575. [DOI] [PubMed] [Google Scholar]