Abstract
Introduction: The first stage of this nationwide study and analysis of the occupational burnout and psychological risk parameters showed a high consistency of emotional exhaustion, depersonalization and low personal accomplishment for doctors working in Emergency Departments and Emergency and Resuscitation Services. These workers were then set in the highest risk group for burnout syndrome and depression. This stageⅡ of our research will focus on those two groups analyzing causal factors, coping mechanisms and possible repercussions of these findings.
Material and methods: Demographics: We have issued a total of 272 surveys from which we have received a total of 263 complete and valid ones (n=263, response rate=96, 69%).
Instruments: The Maslach Burnout Inventory–Human Services Survey MBI–HSS is an instrument designed to assess the three components of the burnout syndrome: emotional exhaustion (EE), depersonalization (DP), and reduced personal accomplishment (PA). The COPE questionnaire is a 52 item addressing different ways of coping with stress. The Center for Epidemiologic Studies Depression Scale (CES-D) has been shown to be a reliable measure in assessing the number, types, and duration of depressive symptoms across racial, gender, and age categories.
Results and discussion: Results were not correlated with gender, age or marital status, but an important correlation was found with professional experience in the Emergency Departments. We have shown that during the first 4 years of experience, the EE factor has been at a satisfying average of 2.4, this variable rising to an average of 2.85 after another 3 years of work. The same type of correlation was found with the CES–D results.
Conclusions: Of the two surveyed groups, the EMD group showed higher values for all risk parameters and low personal accomplishment on the MBI–HSS survey. Also, emotional exhaustion and depression were found to have a powerful correlation with work experience. Coping mechanisms were found to be invariable to the general population, with a slight incline towards active coping and behavioral disengagement
Keywords: Emergency Medicine, burnout syndrome, depression, coping mechanisms, work environment, human resources, stress, psychological traits
Introduction
The first stage of this nationwide study and analysis of the occupational burnout and psychological risk parameters showed a high consistency of emotional exhaustion, depersonalization and low personal accomplishment for doctors working in Emergency Departments and Emergency and Resuscitation Services [1]. These workers were then set in the highest risk group for burnout syndrome and depression. This stage Ⅱ of our research will focus on those two groups analyzing causal factors, coping mechanisms and possible repercussions of these findings.
In the background, most studies linking the specialist's increased professional stress levels with a low quality medical act have a specific reference to emergency medicine. The average percentage given for doctors that have a higher than normal stress level has been an over–time constant in the area of 28%, in comparison with the 18% shown by the general population[2]. What has shown a clear change in the last years is the openness of the doctors to admit the existence of these problems and discuss them with colleagues or take part in group sessions of therapy. [3]
The far most important factor has been established as the lack of sleep on behalf of the doctor. This aspect has recently been given a high level of attention both by researchers and by management branches of the medical world. In the US and other countries following US protocols the maximum on–call period for an EM specialist has been dropped to 12 hours, half of that established for all other specialties, in recognition of the increased level of both physical and psychical stress that the doctor is subjected to. This being said, there is still no measurement taken that prohibits the medic to do overtime in private clinics or other hospitals, therefore a lot of controversies have arisen about the exact efficiency of these measurements.[5,4]
Either individual or conjectural, professional stress sources for EM specialists arise from many aspects of their activities. Among the most discussed are self criticizing attitudes, lack of communication, deficiencies in team–work and lack of professional support, deficient financial rewards, lack of personal time and the lack of self esteem caused by a faulty and unfounded hierarchy that places emergency medical specialists at the bottom of the list.
Material and method
Demographics
We have issued a total of 272 surveys from which we have received a total of 263 complete and valid ones (n=263, response rate=96, 69%). All surveys were anonymous; subjects were randomly selected from the Emergency Departments of state hospitals and were instructed to complete them individually, in their free time. Only M.D. degree subjects were chosen either with or without specialization in Emergency Medicine or Critical Care.
Demographics included age, gender, marital status, children, professional status and work experience. The survey contained detailed instructions on how to complete the demographics and questionnaires, and also offered the subjects the option to receive their own results via e–mail written on a part of the survey that would be detached after the analysis for anonymity purposes.
Instruments
The Maslach Burnout Inventory–Human Services Survey MBI–HSS is an instrument designed to assess the three components of the burnout syndrome: emotional exhaustion (EE), depersonalization (DP), and reduced personal accomplishment (PA). There are 22 items, which are divided into three subscales. The items are written in the form of statements about personal feelings or attitudes (e.g., ‘I feel burned out from my work’, ‘I don't really care what happens to some recipients’). The items are answered in terms of the frequency with which the respondent experiences these feelings, on a 7–point, fully anchored scale (ranging from 0, ‘never’ to 6, ‘every day’). [7]
The reliability coefficients for the MBI–HSS were based on samples that were not used in the item selections to avoid any improper inflation of the reliability estimates. Internal consistency was estimated by Cronbach's coefficient alpha (n=1,316). The reliability coefficients for the subscales were the following: 0.90 for Emotional Exhaustion, 0.79 for Depersonalization, and 0.71 for Personal Accomplishment. The standard error of measurement for each subscale is as follows: 3.80 for Emotional Exhaustion, 3.16 for Depersonalization, and 3.73 for Personal Accomplishment. [8,9]
The COPE questionnaire is a 52 item addressing different ways of coping with stress. Items are rated on a 4–point scale ranging from 1 (I usually don't do this at all) to 4 (I usually do this a lot). These items are then analyzed as 13 different subscales, from which, for the efficacy of the study, we have selected 6: active coping, denial, seeking social support for emotional reasons, behavioral disengagement, substance abuse disengagement and seeking social support for instrumental reasons.[10]
The Center for Epidemiologic Studies Depression Scale (CES-D) has been shown to be a reliable measure for assessing the number, types, and duration of depressive symptoms across racial, gender, and age categories. [11]. Scores may vary from 0 to 80, with a risk threshold at 50, and risk score values being over 60. High internal consistency has been reported with Cronbach's alpha coefficients ranging from 0.85 to 0.90 across studies. Concurrent validity by clinical and self–report criteria, as well as substantial evidence of construct validity has been demonstrated [13].
Final analysis of surveys was made by personnel specialized in psychometric sciences, statistics were made by using Microsoft Excel software and SPSS software, only percentages and linear regression methods were used, all results verify a 95% confidence interval.
Results and discussion
Average age among subjects was 39 years old with an average work experience of 7,4 years. Gender distribution was 68% male and 32% female (Graph 1). Marital status (Graph 2) shows a higher percentage of married subjects (66%) than the single ones (27%), while divorced (7%) rates are lower than the general population shown to be close to 11% [6]. Only 42% of the subjects have children (Graph 3), and further results show that there is a higher percentage of male workers who have children, which may be due to the fact that an important percentage of females change specialties or leave the Emergency Department after having a child (Graph 4).
Graph 1.
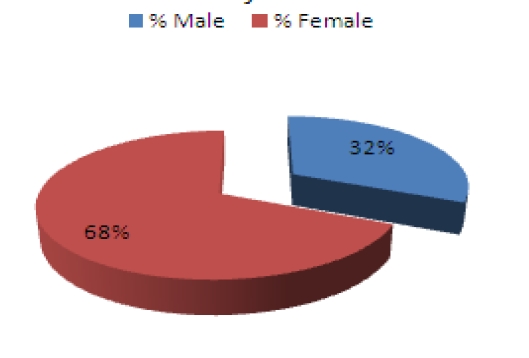
Gender percentages among subjects
Graph 2.
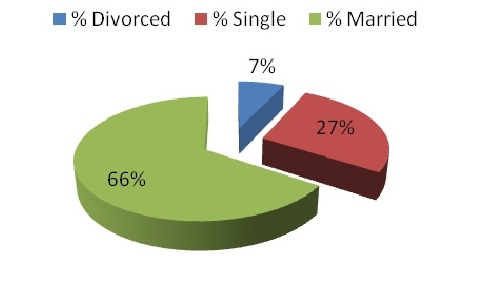
Marital Status among Subjects
Graph 3.
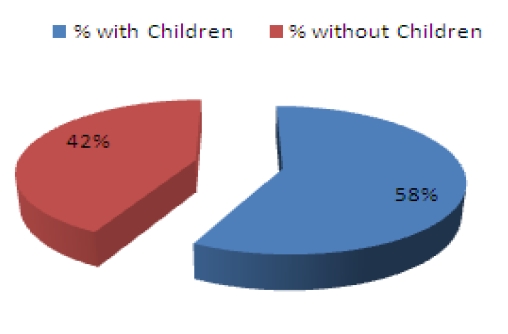
Percetange of subject with/without children
Graph 4.
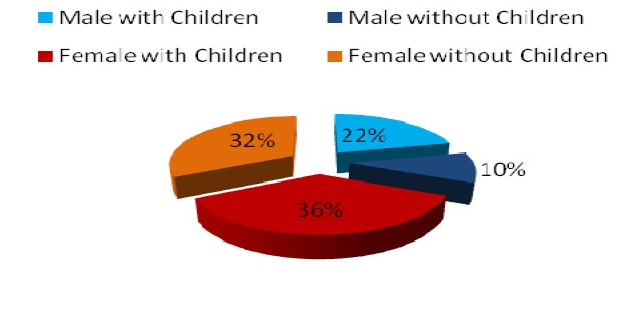
Child siblings
Professional categories include Emergency Department physicians (EMD), SMURD service doctors (SMU). Also, we have added a checkbox for those who have a private practice job besides the regular hospital working hours (Table 1).
Table 1.
Number of subjects by professional category and private practice variable
| nEMD | 186 |
| nSMU | 87 |
| nPRV | 28 |
Results state that 70,07% of subjects worked only in the Emergency Department, while 29.03% had also mobile unit (SMURD) competences. Moreover, an important fact to be noted is that 10.64% of the surveyed workers also have a private practice job besides the state hospital job, adding to a total of 12 to 16 working hours per day.
Average MBI–HSS results confirm those in the first stage of our study [1], showing a higher rate of emotional exhaustion (EE) and depersonalization (DP) among EMD and SMU subjects than all other studied groups of emergency medical personnel. The EE factor was higher in EMD subjects (2.79) than in the SMU (2.16) reversely correlated with the professional accomplishment (PA) factor (Table 2). Also, the DP factor is higher in the EMD group, making these subjects the most vulnerable group for professional stress and burnout syndrome.
Table 2.
MBI–HSS subscales average results stratified by professional category
| GEN | EMD | SMU | |
| EE | 2,594 | 2,794 | 2,160 |
| PA | 4,062 | 4,075 | 4,034 |
| DP | 1,528 | 1,608 | 1,353 |
Results were not correlated with gender, age or marital status, but an important correlation was found with professional experience in the Emergency Departments (Table 3). We have shown that during the first 4 years of experience, the EE factor has been at a satisfying average of 2.4, this variable rising to an average of 2.85 after another 3 years of work. Also, the percentage of personnel showing higher values of EE have been shown to rise in the same parameters (Table 6) from an average of 10,89% showing EE>4 before the 4th year of work experience and to 17,36% before the 7th. Work experience has a powerful influence on the burnout liability of emergency department doctors. Out of all work environment factors, experience time and patient flow were found to be the most important in setting the risk behavior pattern on these subjects[12].
Table 3.
Variation of EE value averages correlated with professional experience in the EMD
| EE value | Experience < 4 years | Experience > 4 years | Experience < 7 years | Experience > 7 years |
| Average | 2,4 | 2,67 | 2,36 | 2,85 |
Table 6.
High risk CES–D results among subjects stratified by work experience
| CES–D result | Experience < 4 years | Experience > 4 years | Experience < 7 years | Experience > 7 years |
| > 40 | 0,072 | 0,0574 | 0,051 | 0,074 |
| > 50 | 0,036 | 0,0056 | 0,022 | 0,008 |
The same correlation was found with the CES-D results. Average CES–D results do not vary significantly with age, gender or marital status, but work experience in the emergency department, again, shows an increase in both parameter average values (Table 5) and percentage of personnel showing risk values (Table 6). Burnout and depression have been shown to lower the quality of life, work environment satisfaction [13] and even quality of medical care [14].
Table 5.
Average CES–D results among subjects stratified by work experience
| Experience | Experience < 4 years | Experience > 4 years | Experience < 7 years | Experience > 7 years |
| CES–D Average | 18,10 | 18,95 | 17,30 | 20,23 |
Coping strategies as surveyed with the short version of the COPE questionnaire do not show a powerful alignment to certain coping mechanisms, although from the 6 selected (active coping, denial, seeking social support for emotional reasons, behavioral disengagement, substance abuse disengagement and seeking social support for instrumental reasons), the highest prevalence seems to be for active coping and behavioral disengagement (Table 7). Substance abuse is in the same limits as all other studied coping mechanisms, which confirms medical workers’ tendency to use alcohol and nicotine for disengagement purposes[15, 16].
Table 7.
COPE results stratified by coping mechanism
| Coping Mechanism | Gen avg | EMD avg | SMU avg |
| Active coping | 2,386 | 2,394 | 2,367 |
| Denial | 2,197 | 2,118 | 2,370 |
| Seeking social support for emotional reasons | 2,119 | 2,112 | 2,133 |
| Behavioral disengagement | 2,417 | 2,432 | 2,386 |
| Substance abuse | 2,224 | 2,244 | 2,179 |
Table 4.
Variation of EE factor value percentages correlated with work experience in the Emergency Department
| EE value | Experience < 4 years | Experience > 4 years | Experience < 7 years | Experience > 7 years |
| >2 | 51,49% | 70,11% | 55,56% | 75,21% |
| >3 | 27,72% | 37,35% | 25,19% | 46,28% |
| >4 | 10,89% | 13,21% | 8,15% | 17,36% |
Conclusions
Of the two surveyed groups, the EMD group showed higher values for all risk parameters and low personal accomplishment on the MBI–HSS survey. Also, emotional exhaustion and depression were found to have a powerful correlation with work experience. Possible explanations for these findings might be linked to different organizations of work within the studied groups (e.g. aspects such as patient flow, crowding, working hours) but also to different individual characteristics, such as social development. None of the studied factors were found to be related with gender, age or marital status.
Coping mechanisms were found to be invariable to the general population, with a slight incline towards active coping and behavioral disengagement.
Study limitations include the risk of conformism for some subjects (due to the vertical top–down distribution of questionnaires), a relatively low n–value in comparison to the first stage of our study due to the scarcity of subjects and their geographical distribution, but the powerful correlations between the two separate studies that form the stages of our research may compensate for these limitations.
Acknowledgments
Ziais Deaconescu–Cambridge University
References
- 1.Popa F, Arafat R, Purcarea V, Lala A, Bobirnac G. Occupational Burnout in Emergency Medicine–A nationwide study and analysis. JMedLife. 2010;3:325–331. [PMC free article] [PubMed] [Google Scholar]
- 2.Firth–Cozens J. Stress in health professionals: psychological and organizational causes and interventions. London: Wiley; 1999. pp. 149–155. [Google Scholar]
- 3.Firth–Cozens J. Interventions to improve physicians' wellbeing and patient care . Soc Sci Med. 2001;52:215–222. doi: 10.1016/s0277-9536(00)00221-5. [DOI] [PubMed] [Google Scholar]
- 4.U.S.A. Congress Patient and Physician Safety and Protection Act of 2001. 2001.
- 5.Berliner H. Patient Dumping–No One Wins and We All Lose. American Journal of Public Health. 1994;74:494. doi: 10.2105/ajph.78.10.1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.U.S.A. Congress Divorce statistics collection: Summary of findings so far, Americans for Divorce Reform.
- 7.Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory . Consulting Psychologists Press. 1996:7–12. [Google Scholar]
- 8.Zalaquet C, Wood RJ. Evaluating Stress. London: The Scarecrow Press; 1997. pp. 14–30. [Google Scholar]
- 9.Carver CS, Scheier MF. Assessing coping strategies: A theoretical based approach . J. Pers. Soc. Psychol. 1989;56:267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 10.Knight RG, Williams S, McGee R, Olaman S. Psychometric properties of the Center for Epidemiologic Studies Depression Scale (CES–D) in a sample of women in middle life . Behavior Research and Therapy. 1993;35:373–380. doi: 10.1016/s0005-7967(96)00107-6. [DOI] [PubMed] [Google Scholar]
- 11.Radloff LS. The CES–D Scale: A self–report depression scale for research in the general population . Applied Psychological Measurement. 1997;1:385–401. [Google Scholar]
- 12.Roberts R, Vernon SW, Rhoades HM. Effects of language and ethnic status on reliability and validity of the CES-D with psychiatric patients . Journal of Nervous and Mental Disease. 1989;177:581–592. doi: 10.1097/00005053-198910000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Campbell SG. Strategies for managing a busy emergency department . CJEM. 2004;6:271–276. [PubMed] [Google Scholar]
- 14.Kuhn G. Tolerance for uncertainty, burnout, and satisfaction with the career of emergency medicine . Ann Emerg Med. 2009;54(1):106–113. doi: 10.1016/j.annemergmed.2008.12.019. [DOI] [PubMed] [Google Scholar]
- 15.Malik AK, Chaudhry A. Cigarette smoking and health care professionals at Mayo Hospital, Lahore, Pakistan . J Pak Med Assoc. 2010;60(6):509–512. [PubMed] [Google Scholar]
- 16.Etter JF. Smoking prevalence, cigarette consumption and advice received from physicians: Change between 1996 and 2006 in Geneva, Switzerland . Addict Behav. 2010;35:355–358. doi: 10.1016/j.addbeh.2009.10.021. [DOI] [PubMed] [Google Scholar]


