Abstract
We have demonstrated in several studies that obesity and adipokines are more strongly associated with asthma in women than in men. The reason for this controversial sex difference is not known. Based on our prior studies, we hypothesize that sex-related difference in ectopic fat may explain the obesity-asthma association in women.
Keywords: adipokine, leptin, adiponectin, physical activity, gonadal hormones, obesity
Introduction: Rising Trends in Obesity, Inactivity and Asthma
There is an increasing prevalence of obesity (Body mass index or BMI ≥ 30 kg/m2) worldwide, particularly in the United States. Data from the two National Health and Nutrition Examination surveys show that the prevalence of obesity has increased among adults aged 20–74 yrs in the United States from 15.0% (in the 1976–1980 survey) to 32.9% (in the 2003–2004 survey). In addition, there has been a decline in physical activity during the same period. Contemporaneous with the rise in obesity and decline in physical activity, there has been a rise in asthma incidence and prevalence in the world, including the United States. The age-adjusted asthma prevalence of 7.9% reported based on the 2005 United States National Health Interview Survey data is more than twice that reported in the 1984-1986 National Ambulatory Medical Care Survey data. We have demonstrated in several studies that obesity and adipokines (proteins produced by adipose tissue) are more strongly associated with asthma in women than in men (31-34). The reason for this controversial sex difference is not known. Based on our prior studies, we hypothesize that sex-related difference in ectopic fat (present within cells of non-adipose tissue) may explain the obesity-asthma association in women. This review also deals with the complex inter-relationships between obesity, adipokines, physical inactivity and asthma, and examines whether these relationships are different between men and women.
Fat distribution is Different between Men and Women
Obesity is a heterogeneous phenotype, including excess amounts of physiological and ectopic fat. While physiological fat is present within cells of adipose tissue, ectopic fat is present within cells of non-adipose tissue (such as viscera and skeletal muscle) that normally contain minimal amounts of fat. It has long been known that fat distribution is different between men and women (Fig. 1). Women typically collect physiological fat on their hips and buttocks, giving them a “pear” shape (also referred to as the gynoid pattern), while men generally collect physiological fat around their belly, giving them an “apple” shape (also referred to as the android pattern). Dual-energy X-ray absorptiometry (DEXA) data show that women have higher physiological fat mass and lower lean mass than men, both overall, as well as in arms, legs, and trunk (34). Recent studies suggest that ectopic fat within the viscera and skeletal muscle may be more metabolically active and more relevant for metabolic syndrome than physiological fat, although its role in asthma has not been studied. Computed tomography of abdomen shows that although women have approximately 60% greater abdominal wall subcutaneous fat mass, they have 19%-37% lower visceral fat mass than men. Furthermore, as compared to men, visceral fat in women may be lower in amount but its metabolic activity may in fact be greater vis-à-vis insulin resistance, serum lipids, and sex-hormonal alterations (18-19,25). Further, women have approximately 40% greater intramyocellular triglyceride content of soleus muscle based on magnetic resonance spectroscopy than men do (24). To summarize, women not only have greater amounts of physiological fat and intramuscular fat but also have more metabolically active visceral fat than men.
Figure 1.
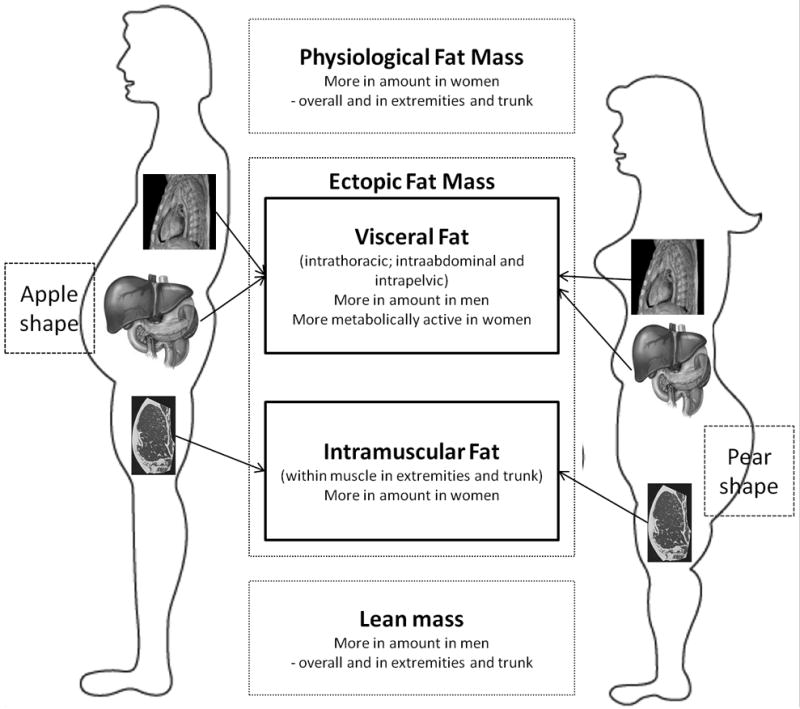
Differences in fat and lean mass distribution between men and women.
Systemic Adipokine Concentrations are Different between Men and Women
It is now known that adipose tissue is not an inert organ simply for energy storage but regulates systemic inflammation via a variety of secreted proteins, called adipokines. Although adipokines include a number of cytokines, chemokines, and cytokine receptors, recent studies have focused on the inflammatory and metabolic role of energy regulating hormones — adiponectin and leptin.
Adiponectin
Adiponectin is a predominantly anti-inflammatory adipokine. Adiponectin inhibits pro-inflammatory proteins such as tumor necrosis factor-alpha (TNF-α), Interleukin (IL)-6, and nuclear factor-κB (NF-κB), as well as induces anti-inflammatory proteins such as IL-10 and IL-1 receptor antagonist. Adiponectin and all of the known receptors for adiponectin (AdipoR1, AdipoR2, T-cadherin, and calreticulin) are expressed on multiple cell types in the lung. Adiponectin is also transported from blood into the alveolar lining fluid via the T-cadherin molecule on the endothelium. Although visceral adipocytes are the most important source of adiponectin, serum adiponectin concentrations are lower among obese subjects. This may be explained by hypoxia-related necrosis of adipocytes in obese subjects, resulting in activation of macrophages. These activated macrophages produce TNF- α and IL-6, which in turn may directly inhibit the local production of adiponectin in a paracrine fashion.
Circulating adiponectin includes three isoforms — low molecular weight (trimers); medium-molecular weight (hexamers) and high-molecular weight or HMW (higher order multimers), as shown in Figure 2. Three monomers of adiponectin form a trimer. Trimers linked by a disulfide bond form a hexamer. Several combined hexamer and trimer forms constitute the higher multimeric form. The proportion of HMW adiponectin is disproportionately reduced in obesity. Interestingly, there is a marked sexual dimorphism of the distribution of adiponectin isoforms in humans. Compared to men, women have higher circulating concentrations of total adiponectin and higher proportions of its high molecular weight isoform, despite greater levels of overall adiposity (2). It is believed that testosterone production during puberty lowers the adiponectin concentrations in men, particularly the HMW isoform (2). Further, castration results in increased total adiponectin concentrations in mice. Recent studies suggest that the HMW isoform of adiponectin is the most biologically active form of adiponectin in regulating insulin resistance. It is not known whether HMW isoform of adiponectin is more strongly associated with asthma than other adiponectin isoforms.
Figure 2.
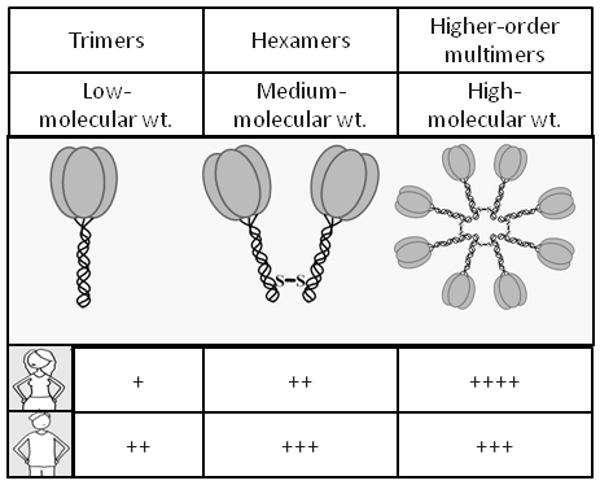
Schematic representation of the sexual dimorphism of the adiponectin isoforms.
Leptin
Serum concentrations of leptin, an energy-regulating hormone, increase with obesity. Leptin and leptin receptors are expressed by the lung. Leptin has overall pro-inflammatory systemic effects — it may stimulate the production of TNF-α and IL-6 from adipose tissue; negatively modulate the function of regulatory T cells (Treg); and promote T-helper1 (Th1) proliferation with increased production of interferon-gamma (IFN-γ).
Women and postpubertal girls have 40%-200% higher concentrations of circulating leptin than their male counterparts, after adjustment for percent body fat. The rate of increase in circulating leptin concentrations is about three-fold greater as a function of BMI in women than in men. Although estrogen supplementation increases and testosterone supplementation decreases leptin concentrations, the sex difference in circulating leptin is not entirely explained by either sex hormones or body fat distribution; and may involve greater leptin gene expression in subcutaneous fat, or greater release of leptin from non-adipose sources such as the brain in women than men. Further, leptin receptor expression in skeletal muscle among women is 41% higher than men — it is possible that the same is true in lung. Thus, as compared to men, women have greater leptin production and possibly greater leptin receptor expression.
Serum leptin to adiponectin ratio, representing the balance of pro- and anti-inflammatory adipokines, is greater in women than in men. This ratio is associated with stronger odds of having the metabolic syndrome than either adipokine alone, even after adjusting for adiposity.
Sex Differences in Physical Activity
Previous population-based studies have found that women are less physically active than men. However, these studies were based on self-report and were designed to capture primarily leisure-time activity, which may not fully capture sources of physical activity for women such as childcare and household activities. On the other hand, a meta-analysis of pedometer-assessed steps per day in developed countries did not find any significant difference between men and women. Yet, women have lower exercise capacity and oxygen consumption relative to their body weight during maximal exercise than men. Of note, women have greater fat and lower muscle mass than men. Therefore, when exercise capacity and oxygen consumption is expressed relative to muscle mass instead of total body mass, the sex differences for these variables is greatly reduced. Further, as compared to men, women tend to have smaller heart size and therefore smaller stroke volumes, as well as lower hemoglobin concentrations. These factors lower oxygen delivery to the exercising skeletal muscle and may further explain the sex difference in exercise capacity and oxygen consumption. Despite these differences, the therapeutic benefits from exercise are, however, similar between the two sexes. For instance, similar decreases in intramyocellular lipid content after submaximal exercise has been reported for both men and women (40).
Clinical Manifestations of Asthma Differ between Men and Women
Although boys are at substantially higher risk for asthma than girls, the incidence and prevalence of asthma is higher among women of childbearing age than in men. Asthma is also more severe in women of childbearing age than men of comparable age. Among children less than 10 yrs, the number of hospital admissions is twice as high for boys as for girls. At age 20 yrs, the admissions are about the same and between the ages of 20 to 50 yrs, the number of admissions for women is three times as high as for men. There are inconsistent reports on the sex predilection for prevalence of methacholine hyperreactivity although there may be a greater prevalence of peak expiratory flow rate variability among women. Women also have greater systemic oxidant stress, as assessed by plasma F2-isoprostane concentration, as compared to men (effect size was approximately 22% higher — further adjustment for BMI did not change the effect size; (33)). Despite that, exhaled nitric oxide (NO) and serum immunoglobulin E (IgE) concentrations are lower among women than men. The lower exhaled NO concentrations may be the result of difference in the surface area of airway epithelium and resulting differences in NO production by the airways; or sex-related differences in endogenous NO production. In summary, sexual dimorphism is observed in the prevalence and severity of asthma.
Physical Inactivity is Associated with Risk for Asthma
The steady increase in physical inactivity over the last three decades corresponds well, in time course, to the increased prevalence of asthma. Several cross-sectional and longitudinal studies have shown that physical activity or fitness is inversely related to the risk of asthma although sex differences in these associations are unclear. It has also been shown that exercise conditioning in asthma improves various subjective parameters (such as decreased intensity of wheezing attacks) and objective parameters (such as increased aerobic fitness), although interestingly it does not appear to influence the degree of methacholine airway responsiveness. Physiological explanations include decreased mucus and edema caused by improved mucociliary clearance from increased epithelial stimulation, and decreased smooth muscle latching and increased chest wall force from increased deep inspiration and sigh rate. Habitual physical activity is associated with reduced serum leptin levels, possibly mild increase in serum adiponectin levels, and reduced levels of IL-6 (Fig. 3). However, untangling the independent contributions of physical activity to asthma vis-a-vis the contributions that are mediated through loss of excess weight or change in systemic adipokines is not an easy matter because these variables are difficult to measure accurately and are highly interrelated (Fig. 3).
Figure 3.
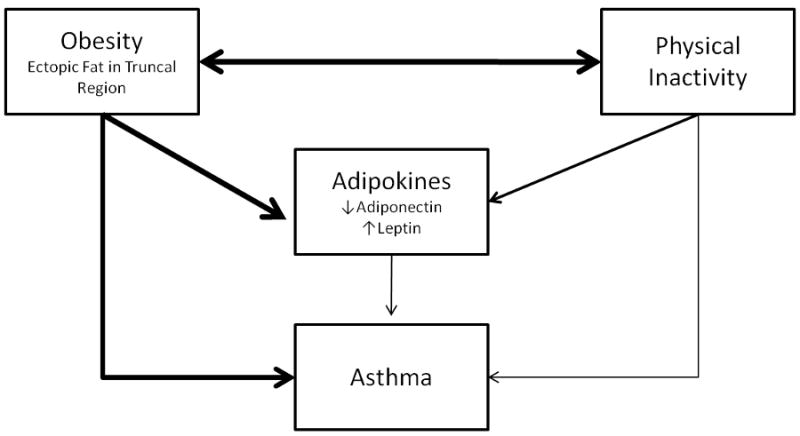
Complex inter-relationships of obesity, adipokines and activity with asthma. Untangling the independent contributions of these predictors to asthma is not an easy matter because these variables are highly interrelated. The approximate strength of the relationship is depicted by the width of the connecting arrow.
Phenotypes of Obesity are Associated with Risk for Asthma Among Women
Obesity has been established as a risk factor for asthma, independent of smoking. The mechanistic basis for this association is not known and includes mechanical and inflammatory effects of obesity on the airway. Further, obesity may be associated with several genetic, epigenetic, hormonal, environmental and developmental factors that may also be associated with asthma.
Whether the relationship between obesity and asthma differs by sex is however controversial. One of the first prospective studies showing that obesity increased asthma incidence was conducted in women (9). Additional early prospective studies also showed that obesity was a risk factor for asthma among women but not among men (6). Thus, the conventional wisdom in this field initially was that obesity was a risk factor among women but not among men. However, other studies did not support this paradigm; some even showed the opposite — that the risk of asthma with obesity was higher among men than women (4,13). A 2007 meta-analysis of seven prospective studies demonstrated no significant interaction (p=0.20) between sex and obesity on incident asthma (Fig. 4; (7)). Despite the findings of this meta-analysis, several large recent studies have continued to demonstrate that the obesity-asthma association is either significant only in women or stronger in women than men (8,11,21-22,34) with odds ratio reportedly ranging from 1.3-2.1 in obese women, compared to normal weight women. A few studies even report a statistically significant interaction between female sex and obesity on asthma (21,34). Most studies also show that asthma severity or occurrence of inadequate control increases with obesity (8,15,39) with some studies further showing that this effect is more marked in women than in men (15). The potential sex-modification of the association between obesity and asthma and its mechanistic basis therefore needs to be explored further.
Figure 4.
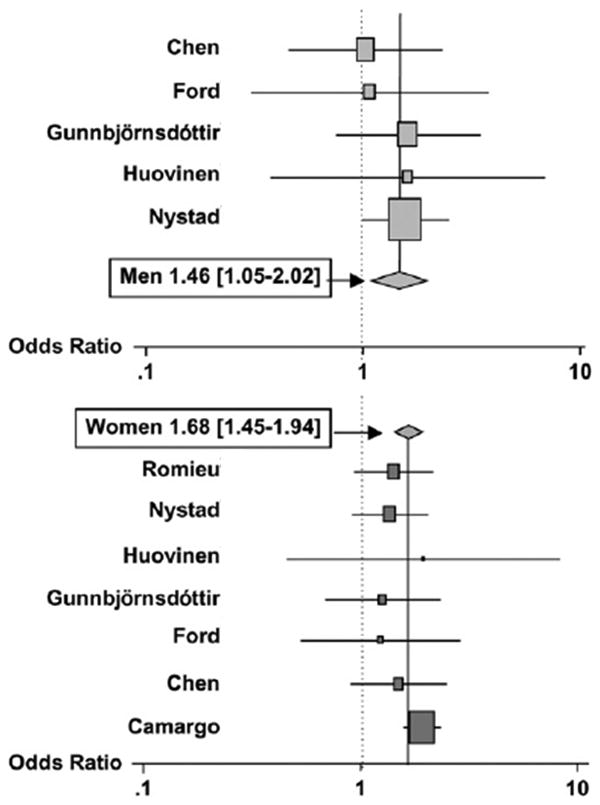
Point estimate for the summary odds of incident asthma, comparing overweight and obese men versus normal-weight men (top) and overweight and obese women versus normal weight women (bottom). The interaction between gender and overweight/obese status on incident asthma was not significant (p=0.20). The names refer to the first authors of the prospective studies included in the meta-analysis. (Reprinted from Beuther DA, Sutherland ER. Overweight, obesity, and incident asthma: a meta-analysis of prospective epidemiologic studies. Am J Respir Crit Care Med. 2007;175(7):661-6. Copyright © 2007 American Thoracic Society. Used with permission.)
It should be noted that few studies have adjusted the obesity-asthma association for self-reported physical inactivity and found that physical inactivity is not an intermediary variable in this association (6,34). It is also unclear whether the obesity-asthma association is modified by atopy, the genetic propensity to develop IgE antibodies in response to exposure to allergen. Interestingly and in contrast to asthma, the prevalence of atopy is higher in men than women. A large Canadian cross-sectional study showed the obesity-asthma association to be stronger in non-atopic women than atopic women with a significant interaction between obesity and atopy on asthma in women (p<0.001) (11). Other studies have however failed to confirm this effect modification by atopy (21). None of these studies have used objective measures of either physical activity or atopy.
Most studies evaluating this association have used excess body mass (i.e., high BMI) to define the obesity phenotype. It is now known that high BMI is in fact a collection of various phenotypes, some but not all relating to excess fat. Further, BMI might be a less reliable measure of body fat in men than in women given the large contribution by lean mass towards the BMI value in men.
Fat Mass, Lean Mass and Asthma
A study where percent body fat (using bioelectrical impedance) was measured found a significant association between body fat and asthma in women (p=0.04) but not in men (p=0.75) (22). We studied the relative contribution towards the odds of asthma between DEXA-assessed fat mass and lean mass (the latter being primarily skeletal muscle and viscera) (34). While DEXA accurately identifies relatively large physiological fat depots as fat mass, it inaccurately classifies some smaller and highly metabolically active ectopic fat within the skeletal muscle and viscera as lean mass. This study suggested that increased total “lean” mass was associated with higher odds for asthma among women and possibly lower odds among men, both without and with adjustment for self-reported physical activity (34). This study also suggested that lean mass may be a better predictor than fat mass for asthma among women. Although there may be a sex difference in the validity of self-report of physical activity, the author does not think that physical activity can explain the sex difference in the lean mass-asthma association. Instead, a plausible explanation for these interesting findings is that the smaller ectopic fat depots (inaccurately assessed by DEXA as components of lean mass) may be more important from the inflammatory standpoint than the larger, physiological fat depots for asthma in women. Sutherland et al. in their 2008 study of lung function suggested that while lean mass was a measure of muscle bulk in men, excess lean mass in women was a measure of obesity. “Lipidization” of lean tissues, such as skeletal muscle (described in lay terms as ‘marbling of muscle’ as shown in Fig. 5) is interestingly more pronounced in women than men, independent of overall obesity. Intramuscular fat is highly associated with systemic leptin and TNF-α concentrations and inversely associated with systemic adiponectin concentrations. Leptin gene polymorphisms are associated with intramuscular fat in the ribeye area in observational studies involving Harton del Valle Columbian cattle breed. It is therefore possible that sex differences in systemic leptin may explain the sex difference in lipidization of lean tissues. However, lipidization of skeletal muscle in various parts of the body may have varying metabolic and inflammatory effects. Unlike upper extremity lean mass that was positively associated with asthma among women, we reported that lower extremity lean mass may be inversely associated with asthma among women (34).
Figure 5.

‘Marbling’ of muscle: The term derived from gross description of beef steak refers to intramuscular fat deposition, giving an appearance similar to marble pattern. Marbled muscle is metabolically more active. Further, leptin is involved in the marbling of muscle in beef cattle.
Android Body Shape and Asthma
An android body shape is characterized by fat primarily localized around the waist. Like BMI, a greater waist circumference, using sex-specific normative values, is associated with asthma primarily among women than men. In one of the few studies to associate body fat distribution and asthma risk prospectively, Romieu et al. showed that the transition from a self-perceived leaner body silhouette to one that was progressively more android (suggesting predominantly abdominal fat distribution) after menarche was associated with a substantial increase in asthma risk among French women (Fig. 6) (26). In another study involving California women teachers, a large waist circumference (>88 cms.) was associated with 37% greater odds of asthma prevalence, even among women with a normal BMI (39). Among obese women, the odds for asthma were greater in those who were also abdominally obese than in women whose waist was ≤ 88 cms (39). These studies suggested that android pattern of obesity in women may be associated with asthma.
Figure 6.
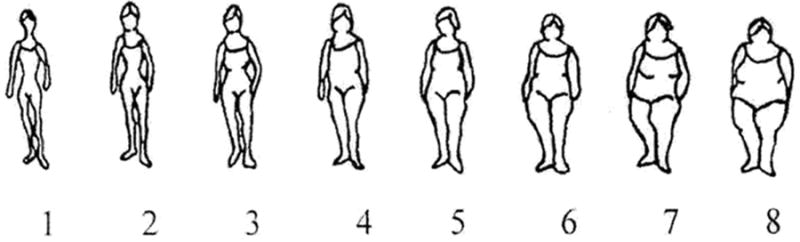
Body silhouettes used to assess body mass by Romieu et al (26). The silhouettes are represented by figure drawings ranked from 1-8, corresponding to increasing body size (from the leanest to the largest). Women reported the drawing that reflected their perceived body size at menarche and at the time of questionnaire administration. (Reprinted from Romieu I, Avenel V, Leynaert B, Kauffmann F, Clavel-Chapelon F. Body mass index, change in body silhouette, and risk of asthma in the E3N cohort study. Am J Epidemiol. 2003;158(2):165-74. Copyright © 2003 Oxford University Press.)
Visceral Fat and Asthma
There are currently no studies in the literature that have evaluated the association between visceral fat, as measured by computed tomography or magnetic resonance spectroscopy and asthma. We studied the relative contribution towards the odds of asthma between arm, leg and trunk distributions of DEXA-assessed fat and lean mass (34). Surprisingly, lean mass in the truncal area was noted to be the strongest predictor for asthma in women, compared to other regional distributions of DEXA-assessed fat and lean mass (including truncal fat; (34)). One should not forget that DEXA-assessed truncal fat may not be a uniform compartment but includes two subcomponents with varying metabolic activity — superficial abdominal subcutaneous fat that is “metabolically benign” and deep abdominal subcutaneous fat that is metabolically active (quite like visceral fat). However, since DEXA can't separate these two subcomponents, the net effect of truncal fat mass on asthma in women may be neutralized. The authors postulated that DEXA-assessed truncal lean mass includes visceral fat components that surround and infiltrate internal organs in the intrathoracic, intraabdominal, and intrapelvic compartments. Pro-inflammatory adipokines expressed by such visceral fat components may have direct access to portal and systemic circulation, accounting for the disproportionately greater inflammatory effect of visceral fat relative to its small size. Further, truncal mass (of which there is disproportionate lean than fat mass) may have direct mechanical effects on diaphragmatic position and movement and chest wall recoil that may increase airway responsiveness.
Upper and Lower Extremity Fat and Asthma
Women have relatively larger gluteofemoral fat deposits than men, giving rise to the “pear-shaped” or gynoid pattern, as shown in Figure 1. Our data suggests that lower extremity (i.e., gluteofemoral) fat is a weaker predictor for asthma than upper extremity fat among women (34). Gynoid obesity is exemplified by adipocyte hyperplasia, instead of adipocyte hypertrophy. Adipocyte hyperplasia in the gluteofemoral region may be associated with a more favorable adipokine milieu as well as higher sex-specific levels of lipoprotein lipase (a key enzyme involved in lipogenesis) than fat in other regions (5). Relative to other fat compartments, lower extremity fat may therefore be metabolically benign (37). Thus, the gynoid pattern of obesity in women is an unlikely explanation for the obesity-asthma association.
Sex Differences in Adipokine-Asthma Association
Leptin and Asthma
A causal role for leptin in asthma is supported by murine studies — administration of exogenous leptin in normal-weight mice augments airway hyperreactivity following allergen challenge as well as lung inflammation following ozone exposure (28-29). On the other hand, human data is currently inconclusive regarding the independent association between serum leptin concentrations and asthma prevalence or control (12,15-16,23,31-32). A large cross-sectional population-based study in the United States showed a positive association between the highest quartile of serum leptin concentration and the risk for asthma in women (odds ratio of 3.2, 95% confidence interval 1.3-7.7), independent of triceps skinfold thickness (32). On the other hand, two large studies, based in Finland and New Zealand did not show an association (14,35). Studies in children and adolescents similarly showed variable results (12,15-16,23). Among the positive studies, the association appears to be stronger among prepubertal boys, peripubertal girls, and premenopausal women (12,23,31-32). Prepubertal boys have lower serum leptin concentrations than girls of the same age and weight. On the other hand, peripubertal girls and premenopausal women have higher serum leptin concentrations than boys and men of the same age and weight respectively, as discussed previously.
Adiponectin and Asthma
A causal role for adiponectin in asthma is supported by murine studies — exogenous adiponectin administration prevents the development of allergen-induced airway hyperreactivity (30). However, human data on the independent association between serum adiponectin concentrations and asthma are currently inconclusive (14,16,23,31,35). Two studies involving German children and American adults separately showed a protective association between serum adiponectin concentrations and odds of prevalent asthma, among non-atopic peripubertal girls and premenopausal women (23,31), independent of BMI; the American study additionally adjusted for physical activity (31). In our unpublished longitudinal study examining this association, low serum adiponectin predicted significantly higher risk of incident asthma in women and in pre-menopausal women, and particularly among current smokers. Further, low serum adiponectin was more important than BMI in predicting the risk of incident asthma among women. On the other hand, two large studies, based in Finland and New Zealand did not show an association between serum adiponectin and asthma (14,35). Systemic adiponectin is associated with good asthma control in adolescent boys (15), although our unpublished data suggests that the opposite is true in men. It is possible that these conflicting results may be explained by the change in adiponectin isoform distribution (towards a lower proportion of HMW isoform) that occurs with puberty in males, as discussed previously.
Although the mouse data suggests that adipokines may mediate the obesity-asthma association, the picture in humans is less clear. The obesity-asthma association is not entirely explained by systemic adipokines. This implies multiplicity of mechanistic pathways for the obesity-asthma association. Further, even among the studies that do show an adipokine-asthma association, this association is not entirely explained by obesity. This implies that adipokine regulation by factors other than obesity may also be important in asthma — such factors could include physical activity, insulin resistance, sex hormones, race, and menopausal status. Smoking is however an unlikely explanation since studies showing associations between adipokines and asthma adjusted for smoking behavior (31-32). Consistent with the possibility that adipokine-asthma association is not entirely explained by obesity, the reported correlation between BMI and adiponectin is modest at -0.19 in women (2). Thus, untangling the independent contributions of obesity and adipokines to asthma is not an easy matter because the relationships between these interrelated variables are complex (Fig. 3).
Possible Causes of Sex Differences in the Associations of Obesity and Adipokines with Asthma
Sex-specific differences in obesity characteristics
Although women typically have a gynoid pattern of fat deposition, it is the acquisition of android pattern of obesity in women that appears to be associated with asthma. Further, ectopic fat deposition in specific regions of the body — such as the viscera or skeletal muscle of arms and trunk- in women may be associated with asthma. It is possible that the inflammatory effects of ectopic fat vis-à-vis the airway are greater among women than men, possibly due to the effect of gonadal hormones. Therefore, there is a need to understand the ectopic fat pattern in women with asthma, using sophisticated techniques such as computed tomography and magnetic resonance spectroscopy. Further, there is a need to understand the functional properties of these ectopic fat deposits in women and their possible regulation by gonadal hormones.
Role of estrogen
Although androgen levels are increased in obesity, peripheral aromatisation of androstenedione to estrone and testosterone to estrogen occurs within the stroma of adipose tissue. Combined with decreased sex hormone binding globulin concentrations found in obesity, this results in an estrogen amplification effect on sensitive tissues, including the airway. Increased estrogen is associated with early menarche in females and delayed puberty in males. In children, Castro-Rodríguez et al. showed that while there was no association between BMI and asthma at age 6, the development of overweight or obesity in girls between ages 6 and 11 yrs was associated with a seven-fold increased risk of new asthma symptoms, and the effect was strongest among girls beginning puberty before age 11 (10). A recent study showed that the association between BMI and asthma severity was stronger in women with early menarche than in women without early menarche (p for interaction = 0.02; (38)). During the menstrual cycle, peak estrogen levels have been associated with increased symptoms and decreased pulmonary function in asthmatic women. The Nurses' Health Study showed that postmenopausal estrogen supplementation was associated with an increased incidence of asthma and that there was a dose-response relation between asthma incidence and the current dose and duration of use of estrogen (36).
The mechanisms by which estrogen leads to increase in asthma are unknown but are worthy of further investigation. Recent data have shown that estrogen administration results in a shift in the immunological reaction from a Th1 to a Th2 type; increase in IL-4 and IL-13 production by peripheral blood mononuclear cells; and increase in eosinophil recruitment and degranulation. Estrogen can also enhance histamine release from rats, probably via an IgE mechanism. It is also possible that there are estrogen receptors on airway smooth muscle or other airway cells and that estrogen directly impacts airway function, although the mechanism remains unknown. Further, estrogen also increases serum leptin concentrations and increases leptin sensitivity in organs such as the brain. Thus, it is possible that estrogen modifies the obesity-asthma and leptin-asthma associations.
Role of testosterone
Interestingly, asthma risk is negatively related to Tanner stage in boys (relative risk of 0.3 for stage V compared with stage I), suggesting a mitigating role for testosterone in asthma. Testosterone is negatively associated with leptin and adiponectin concentrations, particularly the HMW isoform (2). Further, castration results in increased total adiponectin concentrations in mice. Systemic adiponectin is associated with good asthma control in adolescent boys (15), although our unpublished data suggests that the opposite is true in men. It is possible that these conflicting results may be explained by the change in adiponectin isoform distribution (towards a lower proportion of HMW isoform) that occurs with puberty in males.
Role of progesterone
Progesterone upregulates β2 receptors. During the menstrual cycle, the luteal phase increase in progesterone and estradiol is associated with an increased density of β2 adrenoreceptors on lymphocytes. As little as 40 μg of exogenously administered progesterone in a study was shown to cause an eightfold increase in the bronchorelaxant effect of the catecholamine isoprenaline. One hypothesis is that obesity reduces progesterone levels, which reduces β2 adrenoreceptor function, which in turn reduces bronchial smooth muscle relaxation. In support of this hypothesis is the observation that weight loss increases progesterone level, adrenoreceptor density, and catecholamine sensitivity.
Sex-specific misclassification of obesity
In a cross-sectional study of 961 Mexican adults, use of measured BMI revealed that obesity was a risk factor for asthma in both men and women. In contrast, use of self-reported BMI showed that only women and not men were at increased risk of asthma. This study suggested that the use of self-reported BMI underestimated the prevalence of obesity and obscured the relationship between obesity and asthma to a greater extent among men than among women (27). However, it is unlikely that this measurement bias explains the observed sex difference in the obesity-asthma association since many studies using objectively measured BMI continue to show the sex difference (6,34)
Sex-specific misclassification of asthma
It is possible that the misclassification rates are higher among women than men in reporting asthma in function of excess weight. This is especially pertinent since most studies have used self reported information for establishing asthma. In a longitudinal Canadian study involving 254 nonobese (BMI 20-25) and 242 obese (BMI ≥ 30) individuals with asthma that had been diagnosed by a physician, objective testing after tapering of medications excluded asthma in 31.8% in the obese group and in 28.7% in the nonobese group (1). Overdiagnosis of asthma was no more likely to occur among obese individuals than among nonobese individuals (p = 0.46). Men, rather than women were more likely to be at increased risk of overdiagnosis, although no interaction term was reported (1). In a cross-sectional population-based Australian study of 4060 individuals including 380 current asthmatics undiagnosed asthma rates (defined by bronchodilator response in the presence of respiratory impairment) were similar between normal-weight and obese participants, irrespective of sex (3). In a study of 2258 children in Florida, BMI did not alter the diagnostic correlation for asthma between a general physician and a specialist physician; the sex distribution for asthma between the two sets of physicians was further identical (17). Thus, it is unlikely that the measurement bias from asthma definition explains the observed sex difference in the obesity-asthma association.
Airway size effect
The sex difference noted in obese asthmatic subjects may be just a reflection of the increased incidence and prevalence of asthma in women of any size. This has been postulated as a primary airway size effect. However, the obesity-asthma association persists in women, despite adjustment for airway size using height-adjusted values of forced expiratory volume in one second or FEV1 in the statistical model.
Sex-specific differences in obesity threshold
It is possible that the value of an anthropometric measure at which the risk of asthma development is lowest might differ between the two sexes. For instance, a large cross-sectional Canadian study demonstrated that the obesity-asthma association is more evident in women with BMI of ≥ 30 kg/m2, while in men it seemed to increase only in those with morbid obesity (BMI of ≥40 kg/m2) (8). Yet, the sex-specific difference in obesity threshold for asthma is unlikely to explain away the sex difference in obesity-asthma association since the risk for asthma remained disproportionately higher among morbidly obese women than morbidly obese men (8).
Epigenetics (i.e., changes in gene function through heritable changes in chromatin structure without change in DNA sequence) may play an important role in both asthma and obesity but have not been studied in relation to the obesity-asthma association. Interestingly, a recent study showed that adiponectin administration decreases in vitro methylation of selected genes in cancer cells (20). Epigenetic changes may be sex-specific, as has been shown to occur with cytochrome P450 genes. Thus, it possible that epigenetics may explain the sex differences in the associations of obesity and adiponectin with asthma. However, this area needs more research.
In summary, there are various mechanisms that can possibly explain the sex differences in the associations of asthma on obesity and adipokines. We hypothesize a primary role of gonadal hormones in regulating both the adipokine secretion by ectopic fat and the adipokine effect on the airway. Additional research is however needed to test these hypotheses.
Summary
In humans, sexual dimorphism is observed in the prevalence and severity of many diseases, including obesity and asthma. Obesity is a risk factor for asthma. Some studies have also demonstrated an association between adipokines and asthma. In our studies, we have demonstrated that obesity and adipokines are more strongly associated with asthma in women than in men. However, the possible effect modification of these associations by sex remains controversial and needs further research. Based on our prior studies, we hypothesize that sex-related differences in ectopic fat (such as intramuscular fat and visceral fat) may explain these associations in women. We also hypothesize a primary role of gonadal hormones in regulating both the adipokine secretion by ectopic fat and the adipokine effect on the airway. Further, the majority of the literature suggests that the association of obesity and adipokines with asthma is independent of physical activity. However, the relationship between sex, obesity, adipokines, and activity is complex and needs additional research.
Acknowledgments
The author acknowledges the careful critique of this review by Mark Schuyler, M.D., University of New Mexico School of Medicine. The author also recognizes the work of other researchers which could not be cited due to the reference limitations for this review.
Disclosure of Funding: This work was supported in part by NIH NCRR M01-RR-00997 and NIH 1 K23 HL 094531-01 A1/A.
References
- 1.Aaron SD, Vandemheen KL, Boulet LP, et al. Overdiagnosis of asthma in obese and nonobese adults. CMAJ. 2008;179(11):1121–31. doi: 10.1503/cmaj.081332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andersen KK, Frystyk J, Wolthers OD, Heuck C, Flyvbjerg A. Gender differences of oligomers and total adiponectin during puberty: a cross-sectional study of 859 Danish school children. J Clin Endocrinol Metab. 2007;92(5):1857–62. doi: 10.1210/jc.2006-2310. [DOI] [PubMed] [Google Scholar]
- 3.Appleton SL, Adams RJ, Wilson DH, Taylor AW, Ruffin RE. Central obesity is associated with nonatopic but not atopic asthma in a representative population sample. J Allergy Clin Immunol. 2006;118(6):1284–91. doi: 10.1016/j.jaci.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Appleton SL, Wilson DH, Tucker G, Ruffin RE, Taylor AW, Adams RJ. Sex differences in asthma morbidity associated with obesity in a representative population sample. J Allergy Clin Immunol. 2008;121(5):1285–7 e1. doi: 10.1016/j.jaci.2008.03.022. [DOI] [PubMed] [Google Scholar]
- 5.Arner P, Lithell H, Wahrenberg H, Bronnegard M. Expression of lipoprotein lipase in different human subcutaneous adipose tissue regions. J Lipid Res. 1991;32(3):423–9. [PubMed] [Google Scholar]
- 6.Beckett WS, Jacobs DR, Jr, Yu X, Iribarren C, Williams OD. Asthma is associated with weight gain in females but not males, independent of physical activity. Am J Respir Crit Care Med. 2001;164(11):2045–50. doi: 10.1164/ajrccm.164.11.2004235. [DOI] [PubMed] [Google Scholar]
- 7.Beuther DA, Sutherland ER. Overweight, obesity, and incident asthma: a meta-analysis of prospective epidemiologic studies. Am J Respir Crit Care Med. 2007;175(7):661–6. doi: 10.1164/rccm.200611-1717OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boulet LP, Des Cormiers A. The link between obesity and asthma: a Canadian perspective. Can Respir J. 2007;14(4):217–20. doi: 10.1155/2007/101640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Camargo CA, Jr, Weiss ST, Zhang S, Willett WC, Speizer FE. Prospective study of body mass index, weight change, and risk of adult-onset asthma in women. Arch Intern Med. 1999;159(21):2582–8. doi: 10.1001/archinte.159.21.2582. [DOI] [PubMed] [Google Scholar]
- 10.Castro-Rodriguez JA, Holberg CJ, Morgan WJ, Wright AL, Martinez FD. Increased incidence of asthmalike symptoms in girls who become overweight or obese during the school years. Am J Respir Crit Care Med. 2001;163(6):1344–9. doi: 10.1164/ajrccm.163.6.2006140. [DOI] [PubMed] [Google Scholar]
- 11.Chen Y, Dales R, Jiang Y. The association between obesity and asthma is stronger in nonallergic than allergic adults. Chest. 2006;130(3):890–5. doi: 10.1378/chest.130.3.890. [DOI] [PubMed] [Google Scholar]
- 12.Guler N, Kirerleri E, Ones U, Tamay Z, Salmayenli N, Darendeliler F. Leptin: does it have any role in childhood asthma? J Allergy Clin Immunol. 2004;114(2):254–9. doi: 10.1016/j.jaci.2004.03.053. [DOI] [PubMed] [Google Scholar]
- 13.Huovinen E, Kaprio J, Koskenvuo M. Factors associated to lifestyle and risk of adult onset asthma. Respir Med. 2003;97(3):273–80. doi: 10.1053/rmed.2003.1419. [DOI] [PubMed] [Google Scholar]
- 14.Jartti T, Saarikoski L, Jartti L, et al. Obesity, adipokines and asthma. Allergy. 2009;64(5):770–7. doi: 10.1111/j.1398-9995.2008.01872.x. [DOI] [PubMed] [Google Scholar]
- 15.Kattan M, Kumar R, Bloomberg GR, et al. Asthma control, adiposity, and adipokines among inner-city adolescents. J Allergy Clin Immunol. 2010;125(3):584–92. doi: 10.1016/j.jaci.2010.01.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim KW, Shin YH, Lee KE, Kim ES, Sohn MH, Kim KE. Relationship between adipokines and manifestations of childhood asthma. Pediatr Allergy Immunol. 2008;19(6):535–40. doi: 10.1111/j.1399-3038.2007.00690.x. [DOI] [PubMed] [Google Scholar]
- 17.Lang JE, Feng H, Lima JJ. Body mass index-percentile and diagnostic accuracy of childhood asthma. J Asthma. 2009;46(3):291–9. doi: 10.1080/02770900802712963. [DOI] [PubMed] [Google Scholar]
- 18.Leenen R, van der Kooy K, Seidell JC, Deurenberg P. Visceral fat accumulation measured by magnetic resonance imaging in relation to serum lipids in obese men and women. Atherosclerosis. 1992;94(2-3):171–81. doi: 10.1016/0021-9150(92)90242-9. [DOI] [PubMed] [Google Scholar]
- 19.Leenen R, van der Kooy K, Seidell JC, Deurenberg P, Koppeschaar HP. Visceral fat accumulation in relation to sex hormones in obese men and women undergoing weight loss therapy. J Clin Endocrinol Metab. 1994;78(6):1515–20. doi: 10.1210/jcem.78.6.8200956. [DOI] [PubMed] [Google Scholar]
- 20.Liu J, Lam JB, Chow KH, et al. Adiponectin stimulates Wnt inhibitory factor-1 expression through epigenetic regulations involving the transcription factor specificity protein 1. Carcinogenesis. 2008;29(11):2195–202. doi: 10.1093/carcin/bgn194. [DOI] [PubMed] [Google Scholar]
- 21.Loerbroks A, Apfelbacher CJ, Amelang M, Sturmer T. Obesity and adult asthma: potential effect modification by gender, but not by hay fever. Ann Epidemiol. 2008;18(4):283–9. doi: 10.1016/j.annepidem.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 22.McLachlan CR, Poulton R, Car G, et al. Adiposity, asthma, and airway inflammation. J Allergy Clin Immunol. 2007;119(3):634–9. doi: 10.1016/j.jaci.2006.10.029. [DOI] [PubMed] [Google Scholar]
- 23.Nagel G, Koenig W, Rapp K, Wabitsch M, Zoellner I, Weiland SK. Associations of adipokines with asthma, rhinoconjunctivitis, and eczema in German schoolchildren. Pediatr Allergy Immunol. 2009;20(1):81–8. doi: 10.1111/j.1399-3038.2008.00740.x. [DOI] [PubMed] [Google Scholar]
- 24.Perseghin G, Scifo P, Pagliato E, et al. Gender factors affect fatty acids-induced insulin resistance in nonobese humans: effects of oral steroidal contraception. J Clin Endocrinol Metab. 2001;86(7):3188–96. doi: 10.1210/jcem.86.7.7666. [DOI] [PubMed] [Google Scholar]
- 25.Rattarasarn C, Leelawattana R, Soonthornpun S, Setasuban W, Thamprasit A. Gender differences of regional abdominal fat distribution and their relationships with insulin sensitivity in healthy and glucose-intolerant Thais. J Clin Endocrinol Metab. 2004;89(12):6266–70. doi: 10.1210/jc.2004-0209. [DOI] [PubMed] [Google Scholar]
- 26.Romieu I, Avenel V, Leynaert B, Kauffmann F, Clavel-Chapelon F. Body mass index, change in body silhouette, and risk of asthma in the E3N cohort study. Am J Epidemiol. 2003;158(2):165–74. doi: 10.1093/aje/kwg131. [DOI] [PubMed] [Google Scholar]
- 27.Santillan AA, Camargo CA. Body mass index and asthma among Mexican adults: the effect of using self-reported vs measured weight and height. Int J Obes Relat Metab Disord. 2003;27(11):1430–3. doi: 10.1038/sj.ijo.0802395. [DOI] [PubMed] [Google Scholar]
- 28.Shore SA, Rivera-Sanchez YM, Schwartzman IM, Johnston RA. Responses to ozone are increased in obese mice. J Appl Physiol. 2003;95(3):938–45. doi: 10.1152/japplphysiol.00336.2003. [DOI] [PubMed] [Google Scholar]
- 29.Shore SA, Schwartzman IN, Mellema MS, Flynt L, Imrich A, Johnston RA. Effect of leptin on allergic airway responses in mice. J Allergy Clin Immunol. 2005;115(1):103–9. doi: 10.1016/j.jaci.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 30.Shore SA, Terry RD, Flynt L, Xu A, Hug C. Adiponectin attenuates allergen-induced airway inflammation and hyperresponsiveness in mice. J Allergy Clin Immunol. 2006;118(2):389–95. doi: 10.1016/j.jaci.2006.04.021. [DOI] [PubMed] [Google Scholar]
- 31.Sood A, Cui X, Qualls C, et al. Association between asthma and serum adiponectin concentration in women. Thorax. 2008;63(10):877–82. doi: 10.1136/thx.2007.090803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sood A, Ford ES, Camargo CA., Jr Association between leptin and asthma in adults. Thorax. 2006;61(4):300–5. doi: 10.1136/thx.2004.031468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sood A, Qualls C, Arynchyn A, et al. Obesity-asthma association: is it explained by systemic oxidant stress? Chest. 2009;136(4):1055–62. doi: 10.1378/chest.09-0493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sood A, Qualls C, Li R, et al. “Lean” mass predicts asthma better than fat mass among females. Eur Respir J. 2010 doi: 10.1183/09031936.00193709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sutherland TJ, Sears MR, McLachlan CR, Poulton R, Hancox RJ. Leptin, adiponectin, and asthma: findings from a population-based cohort study. Ann Allergy Asthma Immunol. 2009;103(2):101–7. doi: 10.1016/S1081-1206(10)60161-5. [DOI] [PubMed] [Google Scholar]
- 36.Troisi RJ, Speizer FE, Willett WC, Trichopoulos D, Rosner B. Menopause, postmenopausal estrogen preparations, and the risk of adult-onset asthma. A prospective cohort study. Am J Respir Crit Care Med. 1995;152(4 Pt 1):1183–8. doi: 10.1164/ajrccm.152.4.7551368. [DOI] [PubMed] [Google Scholar]
- 37.Van Pelt RE, Evans EM, Schechtman KB, Ehsani AA, Kohrt WM. Contributions of total and regional fat mass to risk for cardiovascular disease in older women. Am J Physiol Endocrinol Metab. 2002;282(5):E1023–8. doi: 10.1152/ajpendo.00467.2001. [DOI] [PubMed] [Google Scholar]
- 38.Varraso R, Siroux V, Maccario J, Pin I, Kauffmann F. Asthma severity is associated with body mass index and early menarche in women. Am J Respir Crit Care Med. 2005;171(4):334–9. doi: 10.1164/rccm.200405-674OC. [DOI] [PubMed] [Google Scholar]
- 39.Von Behren J, Lipsett M, Horn-Ross PL, et al. Obesity, waist size and prevalence of current asthma in the California Teachers Study cohort. Thorax. 2009;64(10):889–93. doi: 10.1136/thx.2009.114579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.White LJ, Ferguson MA, McCoy SC, Kim H. Intramyocellular lipid changes in men and women during aerobic exercise: a (1)H-magnetic resonance spectroscopy study. J Clin Endocrinol Metab. 2003;88(12):5638–43. doi: 10.1210/jc.2003-031006. [DOI] [PubMed] [Google Scholar]


