ABSTRACT
Background
Racial and ethnic disparities in cancer care and survival are well documented. Patient navigation has been shown to improve timely follow-up of abnormal breast screenings for underserved patients. Few studies showed the impact of navigation on patient experiences of care.
Objective
We compared the experiences of patients enrolled in a patient navigator program and non-navigated patients referred to a hospital breast center for follow-up of abnormal mammogram in an underserved community health center population.
Design
Group comparison study using data from a mail and telephone survey to measure the experience of navigated and non-navigated patients.
Participants
English- and Spanish-speaking patients with abnormal mammography attending the Avon Breast Center between April 1, 2005 and April 30, 2007. Seventy-two navigated patients and 181 non-navigated patients completed surveys; the survey response rate was 53.6%.
Main Measures
Timeliness of care, preparation for the visit to the breast center, ease of access, quality of care, provider communication, unmet need and patient satisfaction.
Key Results
Most measures of the patient experience did not differ between navigated and non-navigated patients. Overall quality of care was rated as excellent (55% vs 62%, p = 0.294). Navigated patients were significantly more likely than non-navigated to ‘definitely’ understand what to expect at their visit (79% vs 60%, p = 0.003), to receive a reminder letter or telephone call (89% vs 77%, p = 0.029), and to feel welcome (89% vs 75%, p = 0.012). Navigated patients were less likely than non-navigated to rate the concern shown for their cultural/religious beliefs as excellent (45% vs 54%, p = 0.014).
Conclusions
Assessing patient perspectives is essential to evaluate the success of quality improvement interventions. In our center, we measured few significant disparities in the perceptions of care of these two very different populations of patients, although, there are still areas in which our program needs improvement. Further research is needed to understand the effectiveness of patient navigation programs in reducing racial and ethnic disparities.
KEY WORDS: disparities, patient satisfaction, community-based interventions, evaluation, breast cancer
INTRODUCTION
Throughout the past decade, several national studies have demonstrated racial, ethnic and sociodemographic differences in cancer screening, timely abnormal test follow-up, treatments and mortality1–4. Financial and structural barriers to accessing health care services persist in the US in populations where poverty, lack of insurance, health illiteracy and limited English proficiency lead to disparities in patient care5–14. Despite some progress in reducing disparities in breast and cervical cancer screening, local and regional data on cancer treatment adherence and outcomes make clear that those efforts still fall short15–19.
During the period 2001–2004 in Massachusetts, while breast cancer screening rates were similar by race and ethnicity, available data pointed to racial and ethnic differences in greater tumor size at breast cancer diagnosis among black and Hispanic women and higher mortality from breast cancer among black women as compared with white women20. A report from the Massachusetts Department of Public Health emphasized the need to encourage timely follow-up of abnormal mammography and to reduce barriers in access to treatment of breast cancer, noting national data showing racial and ethnic disparities in waiting times between an abnormal mammogram and a follow-up diagnostic appointment20,21.
A patient navigation program to overcome barriers to breast cancer screening, diagnosis and treatment was first reported by Freeman and colleagues22–24. Our review of prior studies demonstrates that there are several patient navigation programs and other initiatives in place nationally to improve access to screening and timely follow-up for women with breast abnormalities25–32, though only a few report on patient-centered outcomes from patient navigation, and only one includes comparative patient reported experience of care between navigated and other patients28. Given that patient navigator programs are designed to assist patients in overcoming barriers to clinical care, and that patient experience of care is associated with screening and treatment adherence, the patient’s perspective on health care service process and outcomes may be important in evaluating the success of those programs33–36.
Our Cancer Center wants to reduce racial and ethnic disparities, including those in patient perceptions of the accessibility and quality of care, and has started initiatives to measure and document success. In 2001 we initiated patient navigation efforts in breast cancer and in 2005 began to collect data on the experiences of patients in the Avon Breast Center. Key outcomes assessed include patient perceptions of and experiences with timeliness of care, preparation for the visit, ease of access to breast evaluation services and patient satisfaction with multiple dimensions of care. We report initial findings from these efforts here.
METHODS
Setting
The Avon Foundation Comprehensive Breast Evaluation Center (“the Avon Breast Center”) at Massachusetts General Hospital (MGH) focuses on comprehensive evaluation of breast problems including abnormal mammograms and breast lumps. Patients seen in the Center may be referred by primary care physicians or self-referred. The Avon Breast Care Program (“the Avon Program”) was founded in 2001 to facilitate access to Avon Breast Center services and assure the timely follow-up of abnormal mammographic findings among women referred to the Center by three local community health centers (HC): MGH Chelsea HC, Geiger Gibson HC/Harbor Family HC and Mattapan. These health centers serve populations that are traditionally medically underserved, racial, ethnic or linguistic minorities of low socioeconomic status. Patient navigators assist with appointments and help patients access an array of services as needed, including transportation, financial, insurance, interpretation and other barriers to follow-up care.
Study Population
The data reported here come from a mixed-mode survey of patients who were seen for follow-up of abnormal mammography findings for at least one visit at the Avon Breast Center between April 1, 2005 and April 30, 2007. Eligible patients included women and men who were not diagnosed with breast cancer and attended MGH Chelsea HC and Geiger Gibson/Harbor Family HC. Patients from Mattapan HC receive follow-up care at a different tertiary care center and were not included in this survey. Eligible patients spoke Spanish or English, and had a telephone and/or mailing address available. We excluded patients diagnosed with breast cancer because they were eligible for different services and were surveyed in other efforts conducted by our institution during the survey period. We included in our samples all navigated patients who met eligibility criteria (n = 200) and a random sample drawn from lists of all eligible patients in the Avon Breast Center who were not known to the Avon navigator program (n = 390).
Pilot Study: Survey Method Development
The sampling and fieldwork approaches were developed in a pilot study conducted in the navigated-only population in 2004–2005. We used this approach to test the accuracy of our patient registration data about language and telephone and mail address information, as well as the cost, number and mode of contacts needed to achieve adequate response rates. Patients in our pilot study could describe their experience with clinical care, but could not reliably report whether they were assisted by a navigator. As a result, we decided to survey both navigated patients and a random sample of non-navigated patients using administrative data to flag navigated patients for analyses. We opted to use an outside vendor who was not part of the study team for reasons of privacy and data quality. For reasons of cost and sample size we gathered data in waves on a periodic rather than continual basis. Given the higher response rates for Spanish-speaking patients by telephone, we planned a mixed-mode data collection approach to avoid selection and response bias in favor of the non-navigated group.
Questionnaire
The tables, figures and results in this paper show virtually all of the items in our questionnaire. The three-page questionnaire (available upon request from the authors) measured patient-reported experiences with scheduling and check-in procedures as well as experience and satisfaction with clinical care services commonly found in other patient satisfaction instruments in use in our hospital and ambulatory care departments, but with modified response scales tested in our pilot for use in lower literacy and limited English proficiency populations. Since we were surveying both navigated and non-navigated patients, we tested respondent-perceived need for and assistance with multiple aspects of support that might be provided by the navigator or someone else (making and getting to appointments, family care, interpreters, finances, emotional support, information and education). Translation for all written materials was performed by a certified translation specialist.
Data Collection
The survey was conducted by International Communications Research (ICR). Data collection occurred in multiple waves of mailing and telephone calls during the period from July 2006–August 2007. All patients were first contacted by mail using a bilingual cover letter signed by our Cancer Center director, a bilingual return postcard and a three-page questionnaire. Non-respondents were contacted by telephone beginning 10–14 days after the initial mailing and continued through the field period. Telephone follow-up calls were made by bilingual interviewers. Patients were contacted within 1 year of their visit to the Avon Breast Center, but recall periods were variable due to the periodic waves of interviewing. If patients had multiple visits, we asked them to respond about their most recent visit.
Survey Response and Analysis
The data reported here come from questionnaires that were completed by 72 navigated and 181 non-navigated patients (total n = 253). The overall response rate for the survey was 53.6%, calculated using the AAPOR formula RR3, a formula that takes into account non-response because of non-contact and uses an estimate of the proportion of cases where eligibility is unknown that is truly eligible37. Although men were eligible for participation, no men were included in our navigated or non-navigated populations. Navigated patients were more likely than non-navigated patients to complete the survey by telephone (54% vs 34%, p = 0.01), but there were no significant differences in mode of completion between participants who spoke English or Spanish.
Statistical Analysis
Data analyses were completed using SPSS Version 18.0. Chi-square tests were used to test for significant differences between proportions of navigated and non-navigated responses in domains of interest. We used binary logistic regression to explore the impact of race, ethnicity and language on our analysis of navigation as a predictor of ratings of patient-reported experience of care for several measures where navigated vs. non-navigated patients reported significantly different ratings. Patients who did not provide ratings for these items were excluded from these analyses. Because of the high correlation of language and ethnicity, we combined these two into one variable with three categories: Hispanic/Latina and Spanish-speaking, Hispanic/Latina and English speaking, and non-Hispanic/Latina and English speaking (there were no cases of non-Hispanic/Latina Spanish speakers). Language was coded as that in which the respondent completed the survey.
In the model used to predict the patient perceptions of overall quality of care, we controlled for navigation and also independent variables that measured the patient perception of key aspects of patient navigation—timely appointments, appointment reminders, preparation for the visit, care coordination and cultural competence measures (treatment with dignity and respect, sensitivity to cultural and religious issues). We selected these items because they may be seen also as measures of timeliness, equity and patient-centeredness of care, three core elements in the Institute of Medicine (IOM) construct of overall quality of care38. Demographics in this model included race, ethnicity/language, age, gender and education. Education (measured as “years in school”) was not reported by 20 respondents—we imputed the value using the median before creating a categorical variable for education. This had little impact on the overall variance explained or on the direction or significance of education in the model. Participants who were missing values for any other independent variable were excluded from the regression models.
The pilot study, and the secondary analyses of quality improvement data, was approved by the Partners Healthcare Institutional Review Board.
RESULTS
Table 1 shows demographics for navigated and non-navigated patients. Compared with non-navigated patients, navigated patients are significantly younger, more likely to be racial and ethnic minorities, to speak Spanish, to be uninsured and to have lower education levels.
Table 1.
Participant Characteristics, 2005–2007
| Navigated, n = 72 n (%) | Non-navigated, n = 181 n (%) | P-value | |
|---|---|---|---|
| Age* | |||
| 18–39 | 19 (26%) | 39 (22%) | p = 0.011 |
| 40–59 | 44 (61%) | 86 (48%) | |
| 60+ | 8 (11%) | 52 (29%) | |
| No answer | 1 (1%) | 4 (2%) | |
| Race* | |||
| White | 28 (39%) | 158 (87%) | p < 0.001 |
| Non-white (including black, Asian, other, more than one race) | 35 (45%) | 14 (8%) | |
| Refused | 9 (13%) | 9 (5%) | |
| Ethnicity* | |||
| Hispanic/Latina | 46 (64%) | 9 (5%) | p < 0.001 |
| Non-Hispanic/Latina | 25 (35%) | 167 (92%) | |
| Refused | 1 (1%) | 5 (3%) | |
| Primary language spoken* | |||
| English | 35 (49%) | 176 (97%) | p < 0.001 |
| Spanish | 37 (51%) | 5 (3%) | |
| Insurance status* | |||
| Insured | 57 (79%) | 176 (97%) | p < 0.001 |
| Uninsured | 14 (19%) | 4 (2%) | |
| Refused | 1 (1%) | 1 (1%) | |
| Education* | |||
| High school level or below | 49 (68%) | 48 (27%) | p < 0.001 |
| Above high school level | 17 (24%) | 119 (66%) | |
| No answer | 6 (8%) | 14 (8%) | |
*Differences between navigated and non-navigated groups are significant for each demographic (p < 0.05)
Table 2 shows comparisons of navigated and non-navigated patients on several measures of experience prior to and at the point of check-in for the visit. Navigated patients were significantly more likely to rate their understanding of what to expect at the visit, receipt of an appointment reminder and feeling welcomed at the Avon Breast Center more highly than non-navigated patients. After controlling for race and ethnicity/language, navigation remained a significant predictor of understanding what to expect (p = 0.022), but for the items on feeling welcomed and receipt of an appointment reminder, navigation was not significant. Hispanic ethnicity and Spanish language are significantly associated (p = 0.025) with higher likelihood of reporting a reminder call or letter.
Table 2.
Comparative Perceptions of Scheduling and Check-in between Navigated and Non-navigated Patients
| When you think about your care, please tell us whether each was true for you using the following answers (response: definitely yes, somewhat yes, somewhat no, definitely no) | Total % definitely yes (n = 253) | Navigated % definitely yes (n = 72) | Non-navigated % definitely yes (n = 181) | P-value |
|---|---|---|---|---|
| You were able to schedule an appointment as soon as you and your doctor thought you needed it | 86 | 90 | 84 | p = 0.196 |
| Your doctor or health center helped you understand what to expect at your visit to the Avon Breast Center | 65 | 79 | 60 | p = 0.003 |
| You received a reminder letter or telephone call about your appt | 80 | 89 | 77 | p = 0.029 |
| The staff answered the telephone promptly when you called | 62 | 63 | 61 | p = 0.862 |
| The Massachusetts General Hospital was easy to find | 88 | 88 | 88 | p = 0.940 |
| The Avon Breast Center was easy to find | 84 | 82 | 85 | p = 0.615 |
| The waiting room area was comfortable | 80 | 86 | 78 | p = 0.139 |
| You felt welcomed at the Avon Breast Center | 79 | 89 | 75 | p = 0.012 |
*Comparison of navigated and non-navigated patients by chi-square tests. Responses other than ‘definitely yes’ were grouped together for comparison against the group who responded ‘definitely yes’
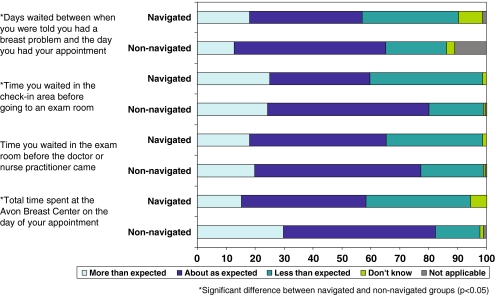
Given the program emphasis on timely appointments, participants were asked about waiting times prior to and during the appointment at the Avon Breast Center. Figure 1 shows that navigated patients were more likely than non-navigated patients to report that waiting times were less than expected to get appointments (33% navigated vs 21% non-navigated, p = 0.004), to move through the check-in area (39% vs 19%, p = 0.007) and in the total amount of time spent at the Avon Breast Center (36% vs 16%, p < 0.001). There was no significant difference between groups in expected wait times to see a clinician once in the exam room.
Figure 1.
Length of waiting times at different stages of appointment at the Avon Center (navigated n = 72, non-navigated n = 181).
In Table 3, we show the results of bivariate analysis of patient-reported experiences with several aspects of the clinical visit and interaction with health care staff and providers (on a 5-point scale of “excellent,” “very good,” “good,” “fair,” “poor”). We tested significance in the comparisons of navigated and non-navigated patients by looking both at “excellent” vs. all other responses, and by grouping “excellent/very good” vs. other response (see appendix for the results combining “excellent and very good”). The only significant item in the “excellent” vs. other analysis was the item about cultural sensitivity, which is highlighted in the table showing that navigated patients were more likely to rate their care as less than excellent. When we test for the combined “excellent/very good” vs. other responses, this item is still significantly different for our two groups, and two additional items (“you were treated with dignity and respect” and “the way staff helped pain and discomfort”) were rated significantly higher by the non-navigated patient group. After controlling these variables for navigation, race, ethnicity and language only, the item on cultural sensitivity was significantly associated with race, but not with navigation or ethnicity/language.
Table 3.
Patient Experience with Clinical Care, Navigated and Non-Navigated Patients, 2005–2007 (% rating ‘excellent’)
| Total % (n = 253*) | Navigated patients % (n = 72*) | Non-navigated patients % (n = 181*) | P-value | |
|---|---|---|---|---|
| The way the staff explained what to expect during your examination | 52 | 54 | 51 | p = 0.702 |
| You were treated with dignity and respect | 65 | 59 | 67 | p = 0.236 |
| The concern the staff showed for your privacy | 63 | 58 | 65 | p = 0.337 |
| The concern the staff showed about your cultural and religious beliefs and customs | 56 | 45 | 54 | p = 0.014 |
| The way the staff helped your pain and discomfort | 50 | 42 | 55 | p = 0.102 |
| The instructions about how to care for yourself at home | 57 | 58 | 57 | p = 0.893 |
| The way the doctors and nurses answered your questions | 60 | 58 | 62 | p = 0.586 |
| The concern the staff showed for your concerns and worries | 60 | 57 | 61 | p = 0.658 |
| The respect the staff showed for your family and friends who were helping you | 60 | 56 | 62 | p = 0.467 |
| Helpfulness of information about your diagnosis and test results | 55 | 53 | 56 | p = 0.647 |
| Communication between the Avon Breast Center and your primary care doctor or nurse | 54 | 55 | 54 | p = 0.956 |
| Overall quality of care provided to you | 60 | 55 | 62 | p = 0.294 |
**n varies for each item as respondents could indicate that the item “did not apply” to them, so the tests for significance include only those people who provided a rating for the item (navigated, n = 52–72; non-navigated, n = 90–181)
We used logistic regression to model the overall rating of quality of care. Patient navigation was not a significant predictor of a patient’s rating of overall quality of care, nor were demographic variables. Significant predictors of higher overall ratings included the greater ability to schedule an appointment as soon as needed (p = 0.027), better communication between the PCP and the Avon Breast Center (p < 0.001), and higher perception of being treated with dignity and respect (p < 0.001). People who rated the degree of concern shown by staff for their cultural and religious beliefs as less than excellent were less likely to rate quality of care as excellent (p = 0.036).
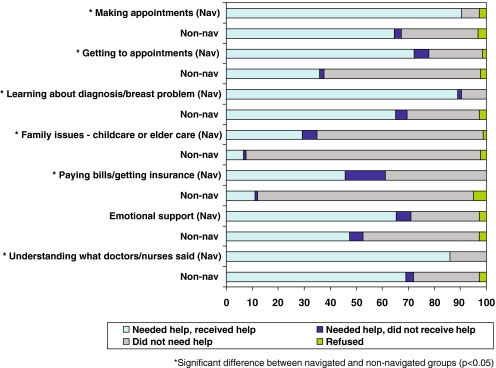
Figure 2 shows responses about the need for and experience with several types of assistance, including activities provided for some patients as part of the navigator program. In most dimensions, the perceived need for assistance is significantly higher for navigated than for non-navigated patients.
Figure 2.
Needs for support and assistance received in each domain (navigated n = 72, non-navigated n = 181).
DISCUSSION
This paper reports the perspectives of patients seen for follow-up of abnormal mammograms in our Center from 2005–2007. The goal of the program is to ensure equal access to care for patients who are referred to our center from community health centers that serve populations that are significantly more likely to be poor, lower income, and to be racial and ethnic minorities than other patients in our health system. Our study sought to understand whether the patients attending our Center perceived differences in the care they received if they were enrolled in the Avon navigator program. One of our institutional goals is to reduce racial and ethnic disparities in access to care and in the experience of care, and several internal research and quality efforts have been directed toward achieving this goal39,40.
While very few studies on navigator programs have included a component to evaluate patients’ experiences throughout the navigator program using patient surveys, some have shown that navigation can increase patient satisfaction among program participants28,36. Perhaps the most striking finding of our study is how many dimensions of the perceptions of navigated and non-navigated patients were not significantly different. Navigated patients were more likely to say they felt prepared for their visit, were reminded of their appointment and felt welcomed on arrival at the Avon Breast Center. They were more likely to say they waited less time than expected for several aspects of their appointments and were more likely to need, and to receive, assistance with appointments, support, information, transportation, interpretation and other services. However, they were less likely to rate a measure of cultural sensitivity as “excellent.” Given the obvious differences between the navigated group and non-navigated group, we controlled these analyses for race, ethnicity and language, and many significant bivariate differences resolved. The samples here are small, and the non-navigated patient population has few minorities—a large proportion of the minority patients served by our hospital are referred from community health centers where they receive primary care—so we do not have an adequate minority subgroup among the non-navigated patients for a well-controlled analysis.
Our comparative study of patients in and out of these programs shows no significant difference between the groups in their overall perception of the quality of care by navigation group or by any of several demographics tested. Rather, the multivariate analysis shows that other factors than patient demographics play a role in determining patient satisfaction—perceptions of timeliness, equity and patient-centeredness of care were all significant predictors of high satisfaction ratings in this population. Consistent with the IOM’s construct of quality of care38, these data show that the patient perception of these same aspects of quality may be important drivers of the patient experience.
Our study has several limitations. Many of the services provided by the navigators are not uniquely available through the navigator, and so the navigators may not have been the sole source of interventional assistance for patients participating in our survey. Navigator records were not detailed as to the intensity and array of services for each patient, so we relied on patient self-report of their experience of navigation and of care. These data come from 2 years of patient experiences within a program that had, at the time, been in existence for 5 years and may not represent the views of all patients at all times in the program. While we endeavored to complete surveys within 6 months of a visit, patients had different periods of recall, and we cannot control for that in our analyses. We surveyed the patients attending only one breast cancer tertiary care center and one navigator program (although administered at two different sites and two different navigators), so results may not be generalizable to other clinical settings. While we tried to include most of the patients served by the navigator program, we did exclude people who did not speak English or Spanish. We also excluded patients diagnosed with breast cancer in an effort to reduce the survey burden on that population since they are the subject of several other patient experience quality improvement surveys in our institution. We also were unable to reach a number of patients in our target samples. We acknowledge that all of these people may have had different experiences than the patients we did reach and did include.
In a complex health system, many health care providers and researchers are focused on ways to engage and assist patients in getting health care. Patient navigation, outreach and coaching initiatives are proliferating, along with challenges in how to measure and compare the impact of these diverse local and regional initiatives. Several studies have shown that navigation improves timely follow-up for patients with abnormal mammograms or breast cancer25–28, but still standard patient satisfaction efforts often do not include multilingual or low-literacy surveys28. Our experiences in creating, managing and evaluating our local program, although not generalizable, may be instructive as other organizations struggle to define comparison groups, measure patient experiences and assess outcomes of these programs. Federally funded efforts36 will help continue needed research in who is best served by these programs, what training is needed for navigators, where navigation programs are most effective, and ultimately, whether racial and ethnic disparities are reduced by these programs nationwide. Efforts to measure and improve access and quality can improve care at the local level while national efforts take shape.
ACKNOWLEDGEMENTS
The authors acknowledge the significant contributions to this project of patient navigators Atala Esquilin and Deborah Crowley, RN, BSN, clinical team members Connie Roche, NP, and Kevin Hughes, MD, of the Avon Breast Center, and Nessa Rodgers of the MGH Center for Community Health Improvement (formerly of Partners Healthcare Community Benefits).
Funding This work was funded in part by the MGH Cancer Center and in part by the Avon Foundation.
Conflict of interest One of our authors (David Dutwin) is employed by the survey research firm that conducted our survey, International Communications Research. No other author has a conflict of interest, financial or otherwise.
APPENDIX
Table 4 Alternative View
Table 4.
Patient Experience with Clinical Care, Navigated and Non-navigated Patients, 2005–2007 [% Rating Positively (Excellent or Very Good)]
| Total % (n = 253**) | Navigated patients % (n = 72**) | Non-navigated patients % (n = 181**) | P-value | |
|---|---|---|---|---|
| The way the staff explained what to expect during your examination | 80 | 76 | 81 | p = 0.381 |
| You were treated with dignity and respect | 92 | 90 | 92 | p = 0.539 |
| The concern the staff showed for your privacy | 88 | 85 | 90 | p = 0.242 |
| The concern the staff showed about your cultural and religious beliefs and customs | 80 | 71* | 86 | p = 0.025 |
| The way the staff helped your pain and discomfort | 77 | 68* | 82 | p = 0.028 |
| The instructions about how to care for yourself at home | 87 | 87 | 88 | p = 0.937 |
| The way the doctors and nurses answered your questions | 85 | 82 | 86 | p = 0.439 |
| The concern the staff showed for your concerns and worries | 86 | 87 | 85 | p = 0.732 |
| The respect the staff showed for your family and friends who were helping you | 90 | 83* | 94 | p = 0.042 |
| Helpfulness of information about your diagnosis and test results | 79 | 74 | 81 | p = 0.198 |
| Communication between the Avon Breast Center and your primary care doctor or nurse | 79 | 81 | 78 | p = 0.551 |
| Overall quality of care provided to you | 86 | 82 | 87 | p = 0.283 |
*Significant difference (p < 0.05) between navigated vs. non-navigated groups
**n varies for each question because of those who did not answer an item or selected that the item ‘did not apply’ to them (navigated, n = 52–72; non-navigated, n = 90–181)
REFERENCES
- 1.Ries LAG, Melbert D, Krapcho M et al (eds). SEER Cancer Statistics Review, 1975–2004, National Cancer Institute. Available from URL: http://seer.cancer.gov/csr/1975_2004/ [accessed June 8, 2010].
- 2.Smedley BD, Stith AY, Nelson AR (eds). Unequal treatment: Confronting racial and ethnic disparities in health care. Institute of Medicine Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press 2003. [PubMed]
- 3.US Department of Health and Human Services. Making cancer health disparities history. Trans-HHS Cancer Health Disparities Progress Review Group. March 2004. Available from URL: http://www.hhs.gov/chdprg/pdf/chdprg.pdf [accessed June 8, 2010].
- 4.Bradley CJ, Given CW, Roberts C. Disparities in cancer diagnosis and survival. Cancer. 2001;91(1):178–188. doi: 10.1002/1097-0142(20010101)91:1<178::AID-CNCR23>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 5.Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284(16):2061–2069. doi: 10.1001/jama.284.16.2061. [DOI] [PubMed] [Google Scholar]
- 6.Blendon RJ, Donelan K, Lukas CV, et al. The uninsured and the debate over the repeal of the Massachusetts universal health care law. JAMA. 1992;267(8):1113–1117. doi: 10.1001/jama.267.8.1113. [DOI] [PubMed] [Google Scholar]
- 7.Donelan K, Blendon RJ, Hill CA, et al. What ever happened to the health insurance crisis in the United States? Voices from a national survey. JAMA. 1996;276(16):1346–1350. doi: 10.1001/jama.276.16.1346. [DOI] [PubMed] [Google Scholar]
- 8.Blendon RJ, Scheck AC, Donelan K, et al. How white and African Americans view their health and social problems. Different experiences, different expectations. JAMA. 1995;273(4):341–346. doi: 10.1001/jama.273.4.341. [DOI] [PubMed] [Google Scholar]
- 9.Epstein AM, Ayanian JZ. Racial disparities in medical care. N Engl J Med. 2001;344(19):1471–1473. doi: 10.1056/NEJM200105103441911. [DOI] [PubMed] [Google Scholar]
- 10.Lurie N, Dubowitz T. Health disparities and access to health. JAMA. 2007;297(10):1118–1121. doi: 10.1001/jama.297.10.1118. [DOI] [PubMed] [Google Scholar]
- 11.Lurie N. Health disparities–less talk, more action. N Engl J Med. 2005;353(7):727–729. doi: 10.1056/NEJMe058143. [DOI] [PubMed] [Google Scholar]
- 12.Jacobs EA, Lauderdale DS, Meltzer D, Shorey JM, Levinson W, Thisted RA. Impact of interpreter services on delivery of health care to limited-English-proficient patients. J Gen Intern Med. 2001;16(7):468–474. doi: 10.1046/j.1525-1497.2001.016007468.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Flores G. Language barriers to health care in the United States. N Engl J Med. 2006;355(3):229–231. doi: 10.1056/NEJMp058316. [DOI] [PubMed] [Google Scholar]
- 14.Cheng EM, Chen A, Cunningham W. Primary language and receipt of recommended health care among Hispanics in the United States. J Gen Intern Med. 2007;22(Suppl 2):283–288. doi: 10.1007/s11606-007-0346-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koutoujian Rep. PJ, Wilkerson Sen. D. Massachusetts State Commission to End Racial and Ethnic Disparities. August 2007. Available from URL: http://www.mahealthcouncil.org/2007_Disparities_Report.pdf [accessed June 8, 2010].
- 16.Mulligan D, Auerbach J. The health of Boston 2006. The Boston Public Health Commission. Mar 2006. Available from URL: http://www.bphc.org/about/Documents/Health%20of%20Boston%202006.pdf [accessed June 8, 2010].
- 17.Patrick DL, Murray TP, Bigby J, Auerbach J, O’Keefe J, Cohen B. Racial and ethnic disparities by EOHHS regions in Massachusetts. Massachusetts Department of Public Health. Nov 2007. Available from URL: http://www.mass.gov/Eeohhs2/docs/dph/research_epi/disparity_report.pdf [accessed June 8, 2010].
- 18.Liu MJ, Hawk H, Gershman ST, et al. The effects of a national breast and cervical cancer early detection program on social disparities in breast cancer diagnosis and treatment in Massachusetts. Cancer Causes Control. 2005;16(1):27–33. doi: 10.1007/s10552-004-1289-4. [DOI] [PubMed] [Google Scholar]
- 19.Bigby J, Ko LK, Johnson N, David MM, Ferrer B. REACH Boston 2010 Breast and Cervical Cancer Coalition. A community approach to addressing excess breast and cervical cancer mortality among women of African descent in Boston. Public Health Rep. 2003;118(4):338–347. doi: 10.1093/phr/118.4.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Massachusetts Department of Public Health. Cancer in Massachusetts by race and ethnicity, 2000–2004. The Massachusetts Cancer Registry. Available from URL: http://www.mass.gov/Eeohhs2/docs/dph/cancer/race_ethnicity.pdf [accessed June 8, 2010].
- 21.US Department of Health and Human Services. Addressing racial and ethnic disparities in health care (fact sheet). Agency for Healthcare Research and Quality. Available from URL: http://www.ahrq.gov/research/disparit.htm [accessed June 8, 2010].
- 22.Freeman HP, Muth BJ, Kerner JF. Expanding access to cancer screening and clinical follow-up among the medically underserved. Cancer Pract. 1995;3(1):19–30. [PubMed] [Google Scholar]
- 23.Freeman HP. A Model Patient navigation program. Oncol Issues. Sep–Oct 2004:44–46.
- 24.Freeman HP. Patient navigation: A community centered approach to reducing cancer mortality. J Cancer Educ. 2006;21(1 Suppl):S11–14. doi: 10.1207/s15430154jce2101s_4. [DOI] [PubMed] [Google Scholar]
- 25.Battaglia TA, Roloff K, Posner MA, Freund KM. Improving follow-up to abnormal breast cancer screening in an urban population. A patient navigation intervention. Cancer. 2007;109(2 Suppl):359–367. doi: 10.1002/cncr.22354. [DOI] [PubMed] [Google Scholar]
- 26.Ell K, Vourlekis B, Lee PJ, Xie B. Patient navigation and case management following an abnormal mammogram: A randomized clinical trial. Prev Med. 2007;44(1):26–33. doi: 10.1016/j.ypmed.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 27.Hiatt RA, Pasick RJ, Stewart S, et al. Community-based cancer screening for underserved women: Design and baseline findings from the breast and cervical cancer intervention study. Prev Med. 2001;33(3):190–203. doi: 10.1006/pmed.2001.0871. [DOI] [PubMed] [Google Scholar]
- 28.Ferrante JM, Chen PH, Kim S. The effect of patient navigation on time to diagnosis, anxiety, and satisfaction in urban minority women with abnormal mammograms: a randomized controlled trial. J Urban Health. 2008;85(1):114–124. doi: 10.1007/s11524-007-9228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Palmieri FM, DePeri ER, Mincey BA, et al. Comprehensive diagnostic program for medically underserved women with abnormal breast screening evaluations in an urban population. Mayo Clin Proc. 2009;84(4):317–322. doi: 10.4065/84.4.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Psooy BJ, Schreuer D, Borgaonkar J, Caines JS. Patient navigation: Improving timeliness in the diagnosis of breast abnormalities. Can Assoc Radiol J. 2004;55(3):145–150. [PubMed] [Google Scholar]
- 31.Freund KM, Battaglia TA, Calhoun E, et al. National Cancer Institute Patient Navigation Research Program: methods, protocol, and measures. Cancer. 2008;113(12):3391–3399. doi: 10.1002/cncr.23960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. National breast and cervical cancer early detection program. Available from URL: http://www.cdc.gov/cancer/NBCCEDP/ [accessed June 8, 2010].
- 33.Dohan D, Schrag D. Using navigators to improve care of underserved patients: current practices and approaches. Cancer. 2005;104(4):848–855. doi: 10.1002/cncr.21214. [DOI] [PubMed] [Google Scholar]
- 34.Tang TS, Patterson SK, Roubidoux MA, Duan L. Women’s mammography experience and its impact on screening adherence. Psychooncology. 2009;18(7):727–734. doi: 10.1002/pon.1463. [DOI] [PubMed] [Google Scholar]
- 35.Davies E, Shaller D, Edgman-Levitan S, et al. Evaluating the use of a modified CAHPS survey to support improvements in patient-centered care: lessons from a quality improvement collaborative. Health Expect. 2008;11(2):160–176. doi: 10.1111/j.1369-7625.2007.00483.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Campbell C, Craig J, Eggert J, Bailey-Dorton C. Implementing and measuring the impact of patient navigation at a comprehensive community cancer center. Oncol Nurs Forum. 2010;37(1):61–68. doi: 10.1188/10.ONF.61-68. [DOI] [PubMed] [Google Scholar]
- 37.American Association for Public Opinion Research. Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. Available from URL: http://www.aapor.org/AM/Template.cfm?Section=Standard_Definitions1&Template=/CM/ContentDisplay.cfm&ContentID=1814 [accessed June 8, 2010].
- 38.Crossing the quality chasm: a new health system for the twenty-first century. Washington: National Academy Press; 2001. [Google Scholar]
- 39.See for example: Massachusetts General Hospital Disparities Solution Center. Available from URL: http://www2.massgeneral.org/disparitiessolutions/mgh.html [accessed June 8, 2010].
- 40.Percac-Lima S, Grant RW, Green AR, et al. A culturally tailored navigator program for colorectal cancer screening in a community health center: a randomized, controlled trial. J Gen Intern Med. 2009;24(2):211–217. doi: 10.1007/s11606-008-0864-x. [DOI] [PMC free article] [PubMed] [Google Scholar]