Abstract
Background
General practitioners (GPs) are often faced with complicated, vague problems in situations of uncertainty that they have to solve at short notice. In such situations, gut feelings seem to play a substantial role in their diagnostic process. Qualitative research distinguished a sense of alarm and a sense of reassurance. However, not every GP trusted their gut feelings, since a scientific explanation is lacking.
Objective
This paper explains how gut feelings arise and function in GPs’ diagnostic reasoning.
Approach
The paper reviews literature from medical, psychological and neuroscientific perspectives.
Conclusions
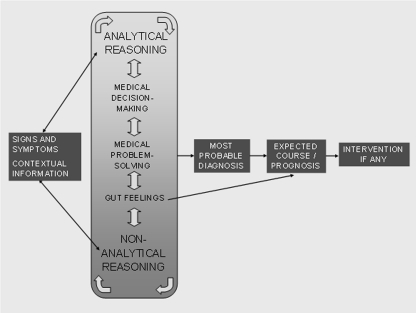
Gut feelings in general practice are based on the interaction between patient information and a GP’s knowledge and experience. This is visualized in a knowledge-based model of GPs’ diagnostic reasoning emphasizing that this complex task combines analytical and non-analytical cognitive processes. The model integrates the two well-known diagnostic reasoning tracks of medical decision-making and medical problem-solving, and adds gut feelings as a third track. Analytical and non-analytical diagnostic reasoning interacts continuously, and GPs use elements of all three tracks, depending on the task and the situation. In this dual process theory, gut feelings emerge as a consequence of non-analytical processing of the available information and knowledge, either reassuring GPs or alerting them that something is wrong and action is required. The role of affect as a heuristic within the physician’s knowledge network explains how gut feelings may help GPs to navigate in a mostly efficient way in the often complex and uncertain diagnostic situations of general practice. Emotion research and neuroscientific data support the unmistakable role of affect in the process of making decisions and explain the bodily sensation of gut feelings.The implications for health care practice and medical education are discussed.
KEY WORDS: gut feelings, diagnostic reasoning, non-analytical reasoning, general practitioner, family physician, dual processes, intuition
INTRODUCTION
General practitioners (GPs) recognize the feeling of sudden heightened awareness or alarm that sometimes emerges during a consultation: ‘There’s something wrong with this patient but I don’t know exactly what. I have to do something because a delay can be harmful.’1–4 These intuitive feelings, which are generally defined as thoughts that come to mind without apparent effort,5,6 seem to play a role in the diagnostic process of GPs when they have to deal with uncertainty and unpredictability in complex situations. Since these situations are characteristic of medical practice,7–9 it is remarkable that in medicine this role has hardly been studied among doctors and is not well understood.
In contrast, the role of intuition in diagnostic reasoning has been extensively investigated in nursing, and results show that intuition is an integral part of nurses’ decision making and is assumed to be based in expert knowledge.10–14 Recent research into the role of intuition in general practice found that many GPs experience so-called gut feelings in their diagnostic reasoning about patients.15 These gut feelings can be regarded as a specific kind of intuitive feelings since they are usually confined to prognostic assessments of the patient’s situation and are often accompanied by bodily sensations. They may act as a compass, steering GPs through busy office hours and enabling them to handle complex problems. Two types of gut feelings can be discerned: a sense of alarm and a sense of reassurance.16 The ‘sense of alarm’ implies that a GP worries about a patient’s health status, even though they have found no specific indications yet; it is the sense of ‘there’s something wrong here.’ It means that the GP needs to initiate specific management to prevent serious health problems. The ‘sense of reassurance’ means that a GP feels secure about the further management and course of a patient’s problem, even though they may not be certain about the diagnosis: ‘everything fits in.’ Although the role of gut feelings in GP’s diagnostic reasoning has been described, a scientific explanation for the phenomenon is still lacking.
The purpose of this article is to show that gut feelings in general practice as a specific form of intuition are based on the interaction between patient information and a GP’s own knowledge and experience. Gut feelings may provide useful information in the diagnostic reasoning process, prompting further thinking and action. To explain the role of gut feelings in diagnostic reasoning, we first discuss the two main approaches used to describe the cognitive processes underlying clinical diagnosis, i.e., medical decision-making and medical problem-solving.17 We then review relevant literature on intuition and intuitive processes in medicine and highlight dual-process theories. We describe the role of affect as a mental shortcut in diagnostic reasoning. Next, we provide neuroscientific data supporting the view that emotions play a role in cognitive processes and can be bodily experienced. Subsequently, we present a model of the diagnostic reasoning process, in which the role of gut feelings as a non-analytical mode of reasoning has been added to the well-defined diagnostic tracks of medical decision-making and medical problem-solving. Finally, the implications of this model for health care practice and medical education are discussed, and options for further research are outlined.
MEDICAL DECISION-MAKING
Medical decision-making (MDM) models are concerned with diagnostic reasoning as an opinion revision process.17 They make use of Bayes’ theorem, likelihood ratios, prior and posterior odds, thresholds, schemes and decision trees to arrive at the best diagnostic and therapeutic decisions.17–21 These mathematical models, incorporating clinical epidemiological data, are related to the concept of evidence-based medicine and constitute a standard for best practice. It is assumed that these models help physicians avoid cognitive biases and mistakes that arise by relying on one’s own knowledge base.17,22,23 The MDM literature emphasizes that intuitive hunches may be false and therefore advocates the use of analytical models and decisions aids, as well as the monitoring of intuitive ideas by checking for biases before deciding. For example, when physicians diagnose a patient with a disease related to but outside their specialty, they impose their prior knowledge on the situation24 and interpret the case from their frame of reference, activating other hypotheses than specialists do. Ideas that first spring to mind determine further thinking and actions, so other relevant information may be ignored or only data confirming the current hypothesis may be considered and sought.
However, the use of analytical methods does not always seem to guarantee objective outcomes. Although clinicians are Bayesians by nature in their diagnostic reasoning, and the patient’s history, signs and symptoms represent powerful information for updating prior probabilities,25 GPs do not calculate a running tally of likelihood ratios.26,27 The assessment of prior probabilities is based on their knowledge of patients and their expertise, and is usually expressed on an ordinal scale from very unlikely to almost certain. GPs add evidence to a prior probability instead of multiplying evidence by a prior chance.28 They base the values needed for use in formulas on subjective evaluations.29,30 Furthermore, the power of a diagnostic indicator to confirm or exclude is mostly assessed in terms like insignificant, weak, good, strong or very strong, and GPs usually apply their own estimated decision thresholds when deciding whether to wait, initiate further examinations or take action.21,31
Whereas evidence-based medicine originally closely followed the MDM approach,32 it now stands for ‘integrating individual clinical expertise with the best available external clinical evidence from systematic research.’33 Scientific knowledge alone is not a sufficient guide, as based on their expertise and skills clinicians need to acquire and integrate information on the condition of the individual patient, his or her preferences, and the best evidence.33,34 We may conclude that in medical decision-making practitioners have to find a balance between analytical reasoning and a kind of intuitive assessment.
MEDICAL PROBLEM-SOLVING
Research into medical problem-solving regards diagnostic reasoning as a process of generating and testing hypotheses.17,35,36 This process has not been found to differ between successful and unsuccessful diagnosticians, nor between experts and novices.36,37 The difference between them arise from the underlying knowledge base that enables experienced physicians, in routine cases, to automatically retrieve the correct diagnostic hypotheses based on only a few relevant signs and symptoms.36,38,39 Their knowledge also guides them in an efficient information search and treatment planning. The direct retrieval of relevant knowledge is an automatic, non-analytical process that, in the case of diagnosis, is often referred to as pattern recognition.17,39 Clinicians immediately understand a patient’s problem in diagnostic terms based on an automatic information integration process such as categorization and problem representation17,40,41 or on the instant recognition of similarity to a previously seen case stored in memory.39,42 In general practice, contextual factors such as age, gender, prior medical history, drug use, family history and social context play an important role in generating accurate diagnostic hypotheses since they may make the presence of a disease more likely or less likely.38 GPs generally know the way their patients normally behave or speak, enabling them to compare this with the current presentation. GPs’ contextual knowledge is a major diagnostic tool in recognizing disorders.43–45
Analytical reasoning is invoked in more complex cases when a diagnosis is not readily available and in the deliberate verification and testing of hypotheses.17,39. Clinicians may then rely on their clinical knowledge by listing patient features, weighing them up, and mapping them to the signs and symptoms known to be associated with certain diseases. Alternatively, they can engage in causal reasoning with biomedical knowledge to bridge the gaps between the elements in the clinical picture.46,47 If we conceptualize medical knowledge as an associative network including interconnected knowledge parts such as contextual information, signs and symptoms, causes of disease, diagnostics, pathophysiological mechanisms, high-level clinical concepts in the form of diagnostic labels, treatments, drugs and previously seen cases,41,48 we can explain the flexibility of knowledge use when experience is gained in a domain. As medical expertise develops, the knowledge network becomes richer, more diversified, better coordinated and attuned to the patients encountered, so the right knowledge will be activated at the right time.39,41,48 With experience, therefore, clinical reasoning becomes more automatic and non-analytical, allowing fast and efficient diagnosis and treatment, while the rich knowledge base can be accessed, if necessary, in a more deliberate and analytical way.
INTUITION
Whereas the literature discussed above does not use intuition as a concept, the role of intuition in medical problem-solving is explicitly addressed in other traditions.49–52 In the cognitive continuum theory, intuition and analysis are defined as two modes of cognition that can be placed at the ends of a continuum, where intuition refers to rapid, unconscious processing and low control, and analysis refers to slow, conscious and controlled processing.30,52 A lot of thinking is situated somewhere in between, and the appropriate mode of thought depends on the specific task characteristics. Doctors need to match the cognitive processes to the task requirements to be accurate. In their theory of expertise, Dreyfus and Dreyfus emphasize49 that expertise develops with experience and thinking proceeds in several stages from analytical to almost completely intuitive. Intuitive processes are so fast that one just knows or acts without being aware where the thought or action comes from. The knowledge on which it is based is not directly accessible and in any case not explicitly used. Hence, it is referred to by some authors as tacit knowledge.50,53,54 Polanyi introduced this term to emphasize that personal knowledge is built on a wealth of experience that is not verbalizable: ‘that which we know but cannot tell.’53 It is tied to the practices from which it is acquired, and often results from informal and implicit learning.48,50 This experiential knowledge is part of the highly interconnected network of knowledge of medical experts,39,48 and may lead to both routine action and reflection.55 ‘Not feeling right,’ for example, is regarded as the outcome of an implicit monitoring process that may trigger immediate intervention, further thinking or even deliberate learning, depending on the situation.50
Intuition can thus be explained as the outcome of highly personalized knowledge-based, non-analytical processes that may help physicians deal with the complexity of the tasks they face.51
DUAL PROCESSES
Psychological dual-process theories contrast analytical reasoning and non-analytical reasoning as two modes of knowing and thinking.6,56–59 The analytical system is explicit, controlled, rational, effortful and relatively slow. In clinical reasoning, analytical thinking is present in deliberately generating and testing of diagnostic hypotheses, in causal reasoning with biomedical knowledge and in the use of decision tools. The non-analytical system is implicit, based on automatic and effortless thought processes, and is associative, intuitive and fast. Non-analytical reasoning can be recognized both in medical decision-making and in medical problem-solving, for instance in automatic chance assessment processes and in pattern recognition. The interaction between these two systems is considered to determine the output of the whole thought process. The outcomes of the non-analytical system can be reflected upon by the analytical system and accepted or elaborated upon for further understanding and investigation or to provide explanations.6
Non-analytical, intuitive thinking is explained in terms of the high accessibility of the immediate thoughts.6,60 Prolonged practice and specific training make useful thoughts more easily accessible, enabling accurate intuitive performance. This explanation concurs with the knowledge acquisition processes described in the medical problem-solving tradition, and the explanation of intuition in clinical reasoning research. The cognitive continuum theory30,52 in particular can be regarded as an early form of dual process theory. Although gut feelings as such do not feature in any of these theories, the affect heuristic described in decision-making research6,60,61 as the intuitive positive and negative feelings guiding decisions comes close to our description of a sense of reassurance and a sense of alarm. We assume that these (gut) feelings also originate in the knowledge and experience gained over time and may therefore contribute to the diagnostic process.
EMOTIONS IN MAKING DECISIONS
The guiding role of affect in making decisions has been demonstrated in various research traditions. In research on judgment and choice, affect is defined as a feeling of ‘goodness’ or ‘badness’ that is elicited by the positive or negative quality attached by experience to the object of thought.61,62 This response depends on the interaction between an individual and a specific context. Reliance on such feelings is characterized as the affect heuristic, a mental shortcut preceding deliberate, analytical thinking that helps people to navigate in a mostly efficient way in complex, uncertain and sometimes dangerous situations. This function of affect and emotions is the hallmark of the experiential system in Epstein’s dual process theory.58
Research on emotions encompasses affect but is broader in scope.62 It includes many theories and definitions of emotions that vary in focus63–67 For our purpose, it seems important to note that emotions may be triggered by the unconscious interpretation of information in the environment, are often accompanied by bodily sensations and physical changes, provide information that motivates and directs action or further thinking, and have adaptive value. Of particular interest for the sense of alarm are emotions invoked by stimuli like signs and symptoms that do not fit into a familiar pattern of a disease or a patient. These unusual stimuli arouse curiosity and explorative behavior, but also keen expectation and fear.65
Cognitive neuroscience research also provides support for the view that emotions significantly contribute to decision-making processes.68,69 Patient studies have shown that this complex process is disrupted when emotions are ‘eliminated.’ Patients who have sustained damage in the ventromedial prefrontal cortex evinced a generally flat affect and an inability to react to emotional situations, in addition to repeatedly making decisions that were detrimental to their well-being.68,69 Notwithstanding perfectly functioning intellectual capacities, this damage led to incorrect assessments of the social impact of their behavior in terms like ‘good, safe and advantageous’ or ‘bad, risky and disadvantageous.’ It seemed as if they did not learn from previous experiences. Further experimental studies showed that although they could register the consequences of their behavior, they could not anticipate them.68,70
These findings have been explained by the somatic-marker hypothesis,68,69 which describes how brain structures are involved in decision-making processes. Consequences of behavior processed in the sensory cortex induce the amygdala to elicit emotional bodily responses via effector nuclei in the brain stem. Through a learning process, these responses (somatic markers) become linked to mental representations of this specific behavior in the ventromedial prefrontal cortex, which are stored in the dorsolateral prefrontal cortex. In decision making, therefore, the same emotional responses are elicited when experiencing or envisioning the behavior that brought them about in the past. Subsequently, they are processed either at the cortical level, evoking conscious “gut feelings” of positive or negative affect, or at the subcortical level, influencing decision making in a nonconscious way. At the cortical level, functional imaging studies suggest that the insular cortex is involved in representing awareness of subjective feelings and has a role in guiding mental and physical behavior.68,71,72
The brain is a complex, integrated system of functional networks distributed across multiple sites, and other structures have also been found to be involved in decision making.63,64,71 However, the above discussion clearly suggests that emotions are a vital component of this cognitive process, helping us to thread our ways through the huge amount of information and knowledge available.
DIAGNOSTIC REASONING MODEL
Summarizing our narrative review of the literature, we may learn that medical decision-making models make use of intuitive assessments of chances based on experiential knowledge, although their proponents generally warn against any form of intuitions. Medical problem-solving theories afford the insight that knowledge and experience underlie non-analytical (including gut feelings) and analytical diagnostic reasoning, although the role of emotions is not made explicit at all. Dual process theories describe the role of intuition in making decisions and can provide an explanation for gut feelings as an affect heuristic. Emotion research and neuroscientific data support the unmistakable role of emotions in the decision-making process and explain the bodily sensation of gut feelings. We propose therefore to consider gut feelings as a separate track in GPs’ diagnostic reasoning that complements the other two tracks.
We present a model of GPs’ diagnostic reasoning in which it is visualized as a mix of analytical and non-analytical reasoning processes, where the three tracks of diagnostic reasoning, medical decision-making, medical problem-solving and gut feelings, collaborate within a GP’s knowledge network (Fig. 1). Depending on the task (routine or more complicated) and the situation (being familiar with a patient and a disease or not), GPs use elements of all three tracks. With increasing experience, their knowledge network will become richer and more coherent, and non-analytical reasoning will more often be invoked, but experienced GPs are able to switch to analytical reasoning when the automatic approach is not enough to explain the patient’s situation. The sense of alarm can be regarded as the first warning sign that automatically pops up from the knowledge network to slow down when no familiar pattern can be identified. Sometimes no satisfactory explanation can as yet be found, but prompt intervention is necessary bypassing a diagnosis. And sometimes GPs can feel reassured about the expected course of an illness even if they have as yet no clear diagnosis.
Figure 1.
Knowledge-based model of GPs’ diagnostic reasoning.
IMPLICATIONS
Our explanation of the role of gut feelings in GPs’ diagnostic reasoning has several important implications for health care practice and medical education. At the very least, it means that gut feelings need to be taken seriously. When GPs and trainees recognize a sense of alarm, they should be alerted to slow down and switch to analytical reasoning. Sharing these experiences with colleagues might help to understand what pattern of signs and symptoms caused these feelings and to determine the best step to take next. In medical education, trainees should be given the opportunity to tell their consultation stories and evaluate the role of gut feelings in the diagnostic reasoning process. Increased awareness of gut feelings can help GPs to learn when to trust them and when to slow down.
Currently, medical educators teach students to reason in an analytical way, and when GP trainers explain their diagnostic reasoning about a patient’s problem, they often make it seem like a logical process of testing plausible hypotheses or the outcome of a mathematical process. This retrospective reconstruction of seemingly objective reasoning often excludes the tacit clues and intuitive hunches hidden in the patient’s story and context, on which the original diagnosis depended. It also denies the coordinated processes of analytical and non-analytical reasoning.42,73 Knowing the patient’s narrative and its interpretation by an experienced GP can help trainees and medical students to understand both aspects of diagnostic reasoning and enable them to refine their knowledge base.35,74–76 “Reflection-in-action” by medical practitioners during the diagnostic process contributes to awareness of their feelings of certainty or uncertainty, assessing the limitations of their knowledge, and stimulating them to search for feedback and follow-up.4,55,77,78 Personal reflection is a trainable, professional quality that might be improved even in the early stages of education.79 Studying and discussing written clinical cases or video’s of real or simulated patients, specifically aimed at the diagnostic role of gut feelings, may promote student recognition of their own gut feelings and sharing of knowledge and experience. Finally, instructions to use a combination of analytical and non-analytical reasoning have been demonstrated to improve diagnostic accuracy.80,81
In further research, the incidence of the sense of alarm and the sense of reassurance in daily general practice should be charted, as well as the way GP-trainers and their trainees deal with them in the short as well as longer term. This raises questions such as whether gut feelings trigger reevaluation, feedback seeking and learning, and whether these initial feelings are useful compared to the outcomes of further diagnostics and treatments in the course of the disease. Follow-up research into outcomes may also be used to determine the diagnostic value of gut feelings. Assessing the differences in these predictive values between trainees and experienced GPs can shed light on the role of experience in the diagnostic process. Similarly, research into the effects of knowledge about the context and the patient can be done by examining differences between situations in which GPs deal with patients they know or patients they see for the first time (e.g., when they are on call). We are addressing these topics using a short questionnaire we have developed to record gut feelings in general practice based on the consensus statements about the sense of alarm and sense of reassurance.16 This questionnaire is now being validated using a set of written clinical cases that differ in the type and extent of gut feelings to be triggered, as classified by a group of experienced GPs and diagnosed by a large group of experienced GPs. This instrument could also be used to study the role of gut feelings in diagnostic reasoning in a more fundamental and experimental way. For example, clinical cases could be written that vary in the amount of contextual and patient knowledge, and could be presented for diagnosis to trainees and GPs with different levels of expertise, followed by the questionnaire. This would also allow the effects of educational interventions to be tested. Finally, physiological measurements of emotions and imaging studies of GPs’ diagnostic reasoning processes with different clinical cases may test the somatic-marker hypothesis in a realistic medical setting.
Acknowledgments
Funded by Maastricht University and University of Antwerp.
Conflict of Interest
None disclosed.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
Funded by Maastricht University and University of Antwerp.
References
- 1.Hull F. The consultation process. In: Sheldon M, Brooke J, Rector A, editors. Decision Making in General Practice. London: Macmillan; 1985. pp. 13–26. [Google Scholar]
- 2.Andre M, Borgquist L, Foldevi M, Molstad S. Asking for ‘rules of thumb’: a way to discover tacit knowledge in general practice. Fam Pract. 2002;19(6):617–622. doi: 10.1093/fampra/19.6.617. [DOI] [PubMed] [Google Scholar]
- 3.Stolper CF, Van Royen P, Dinant GJ. ‘Gut feelings’ in general practice in Europe. A short report about recognition and expressions. Eur J Gen Practice. 2010;(2):72-74 [DOI] [PubMed]
- 4.Groopman J. How Doctors Think. Boston-New York: Houghton Mifflin Company; 2007. [Google Scholar]
- 5.Simpson J, Wein E. Oxford English Dictionary. Oxford: Oxford University Press; 2005. [Google Scholar]
- 6.Kahneman D. A perspective on judgment and choice: mapping bounded rationality. Am Psychol. 2003;58(9):697–720. doi: 10.1037/0003-066X.58.9.697. [DOI] [PubMed] [Google Scholar]
- 7.Dinant GJ, et al. Diagnosis and decision. Undifferentiated illness and uncertainty in diagnosis and management. In: Jones R, Britten N, Gulpepper L, Gass D, Grol R, Mant D, et al., editors. Oxford Textbook of Primary Medical Care. Oxford: Oxford University Press; 2004. pp. 201–203. [Google Scholar]
- 8.Griffiths F, Green E, Tsouroufli M. The nature of medical evidence and its inherent uncertainty for the clinical consultation: qualitative study. BMJ. 2005;330(7490):511–557. doi: 10.1136/bmj.38336.482720.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Innes AD, Campion PD, Griffiths FE. Complex consultations and the ‘edge of chaos’. Br J Gen Pract. 2005;55(510):47–52. [PMC free article] [PubMed] [Google Scholar]
- 10.Rew L, Barrow EM., Jr State of the science: intuition in nursing, a generation of studying the phenomenon. ANS Adv Nurs Sci. 2007;30(1):E15–25. doi: 10.1097/00012272-200701000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Lee J, Chan AC, Phillips DR. Diagnostic practise in nursing: a critical review of the literature. Nurs Health Sci. 2006;8(1):57–65. doi: 10.1111/j.1442-2018.2006.00267.x. [DOI] [PubMed] [Google Scholar]
- 12.Hams SP. A gut feeling? Intuition and critical care nursing. Intensive Crit Care Nurs. 2000;16(5):310–318. doi: 10.1054/iccn.2000.1500. [DOI] [PubMed] [Google Scholar]
- 13.McCutcheon HHI. Intuition: an important tool in the practice of nursing. J Adv Nurs. 2001;35(3):342–348. doi: 10.1046/j.1365-2648.2001.01882.x. [DOI] [PubMed] [Google Scholar]
- 14.King L, Appleton JV. Intuition: a critical review of the research and rhetoric. J Adv Nurs. 1997;26(1):194–202. doi: 10.1046/j.1365-2648.1997.1997026194.x. [DOI] [PubMed] [Google Scholar]
- 15.Stolper CF, Van Bokhoven MA, Houben PHH, Van Royen P, Van de Wiel M, Van der Weijden T et al. The diagnostic role of gut feelings in general practice. A focus group study of the concept and its determinants. BMC Fam Pract. 2009; 10(17). [DOI] [PMC free article] [PubMed]
- 16.Stolper CF, Van Royen P, Van Bokhoven MA, Houben PHH, Van de Wiel M, Van der Weijden T, et al. Consensus on gut feelings in general practice. BMC Fam Pract. 2009;10:66. doi: 10.1186/1471-2296-10-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Elstein AS, Schwarz A. Clinical problem solving and diagnostic decision making: a selective review of the cognitive literature. BMJ. 2002;324(7339):729–732. doi: 10.1136/bmj.324.7339.729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chapman GB, Sonnenberg F. Decision making in health care: theory, psychology, and applications. New York: Cambridge University Press; 2000. [Google Scholar]
- 19.Sackett DL, Haynes RB, Guyatt GH, Tugwell P. Clinical epidemiology: a basic science for clinical medicine. 2. Boston: Little, Brown; 1991. [Google Scholar]
- 20.Richardson WS, Wilson MC, Guyatt GH, Cook DJ, Nishikawa J. Users’ guides to the medical literature: XV. How to use an article about disease probability for differential diagnosis. Evidence-Based Medicine Working Group. JAMA. 1999;281(13):1214–1219. doi: 10.1001/jama.281.13.1214. [DOI] [PubMed] [Google Scholar]
- 21.Pauker SG, Kassirer JP. The threshold approach to clinical decision making. N Engl J Med. 1980;302(20):1109–1117. doi: 10.1056/NEJM198005153022003. [DOI] [PubMed] [Google Scholar]
- 22.Klein JG. Five pitfalls in decisions about diagnosis and prescribing. BMJ. 2005;330(7494):781–783. doi: 10.1136/bmj.330.7494.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med. 2003;78(8):775–780. doi: 10.1097/00001888-200308000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Hashem A, Chi MTH, Friedman CP. Medical errors as a result of specialization. J Biomed Inform. 2003;36:61–69. doi: 10.1016/S1532-0464(03)00057-1. [DOI] [PubMed] [Google Scholar]
- 25.Gill CJ, Sabin L, Schmid CH. Why clinicians are natural Bayesians. BMJ. 2005;330(7499):1080–1083. doi: 10.1136/bmj.330.7499.1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Steurer J, Fischer JE, Bachmann LM, Koller M, ter Riet G. Communicating accuracy of tests to general practitioners: a controlled study. BMJ. 2002;324(7341):824–826. doi: 10.1136/bmj.324.7341.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reid MC, Lane DA, Feinstein AR. Academic calculations versus clinical judgments: practicing physicians’ use of quantitative measures of test accuracy. Am J Med. 1998;104(4):374–380. doi: 10.1016/S0002-9343(98)00054-0. [DOI] [PubMed] [Google Scholar]
- 28.Van den Ende J, Van Gompel A, Van den Ende E, Van Damme W, Janssen PA. Bridging the gap between clinicians and clinical epidemiologists: Bayes theorem on an ordinal scale. Theor Surg. 1994; 9(195).
- 29.Kleinmuntz B. Why we still use our heads instead of formulas: Toward an integrative approach. Psychol Bull. 1990;107(3):296–310. doi: 10.1037/0033-2909.107.3.296. [DOI] [PubMed] [Google Scholar]
- 30.Hammond KR, Hamm RM, Grassia JL, Pearson T. Direct comparision of the efficacy and analytical cognition in expert judgement. IEEE Transactions on Systems, Man and Cybernetics ed. 1987.
- 31.Van Puymbroeck H, Remmen R, Denekens J, Scherpbier A, Bisoffi Z, Van den Ende J. Teaching problem solving and decision making in undergraduate medical education: an instructional strategy. Med Teach. 2003;25(5):547–550. doi: 10.1080/0142159031000137490. [DOI] [PubMed] [Google Scholar]
- 32.Elstein AS. On the origins and development of evidence-based medicine and medical decision making. Inflamm Res. 2004;53(Suppl 2):184–189. doi: 10.1007/s00011-004-0357-2. [DOI] [PubMed] [Google Scholar]
- 33.Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312(7023):71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haynes RB, Devereaux PJ, Guyatt GH. Clinical expertise in the era of evidence-based medicine and patient choice. ACP J Club. 2002;136(2):A11–14. [PubMed] [Google Scholar]
- 35.Bowen JL. Educational strategies to promote clinical diagnostic reasoning. N Engl J Med. 2006;355(21):2217–2225. doi: 10.1056/NEJMra054782. [DOI] [PubMed] [Google Scholar]
- 36.Elstein AS, Shulman L, Sprafka S. Medical Problem Solving: an analysis of clinical reasoning. Cambridge: Harvard University Press; 1978. [Google Scholar]
- 37.Neufeld VR, Norman GR, Feightner JW, Barrows HS. Clinical problem-solving by medical students: a cross-sectional and longitudinal analysis. Med Educ. 1981;15(5):315–322. doi: 10.1111/j.1365-2923.1981.tb02495.x. [DOI] [PubMed] [Google Scholar]
- 38.Hobus PP, Schmidt HG, Boshuizen HP, Patel VL. Contextual factors in the activation of first diagnostic hypotheses: expert-novice differences. Med Educ. 1987;21(6):471–476. doi: 10.1111/j.1365-2923.1987.tb01405.x. [DOI] [PubMed] [Google Scholar]
- 39.Norman GR, Eva K, Brooks LR, Hamstra S. Expertise in Medicine and Surgery. In: Ericsson KA, Charness N, Feltovich PJ, Hoffman RR, editors. The Cambridge Handbook of Expertise and Expert Performance. New York: Cambridge University Press; 2006. pp. 339–354. [Google Scholar]
- 40.Bordage G. Prototypes and semantic qualifiers: from past to present. Med Educ. 2007;41(12):1117–1121. doi: 10.1111/j.1365-2923.2007.02919.x. [DOI] [PubMed] [Google Scholar]
- 41.Van de Wiel M, Boshuizen HPA, Schmidt H. Knowledge restructuring in expertise development: Evidence from pathophysiological representations of clinical cases by students and physicians. Eur J Cogn Psychol. 2000;12(3):323–355. doi: 10.1080/09541440050114543. [DOI] [Google Scholar]
- 42.Norman G, Young M, Brooks L. Non-analytical models of clinical reasoning: the role of experience. Med Educ. 2007;41(12):1140–1145. doi: 10.1111/j.1365-2923.2007.02914.x. [DOI] [PubMed] [Google Scholar]
- 43.Lykke K, Christensen P, Reventlow S. “This is not normal…”–signs that make the GP question the child’s well-being. Fam Pract. 2008;25(3):146–153. doi: 10.1093/fampra/cmn021. [DOI] [PubMed] [Google Scholar]
- 44.Hjortdahl P. The influence of general practitioners’ knowledge about their patients on the clinical decision-making process. Scand J Prim Health Care. 1992;10(4):290–294. doi: 10.3109/02813439209014076. [DOI] [PubMed] [Google Scholar]
- 45.Jones I, Morrell D. General practitioners’ background knowledge of their patients. Fam Pract. 1995;12(1):49–53. doi: 10.1093/fampra/12.1.49. [DOI] [PubMed] [Google Scholar]
- 46.Patel VL, Groen GJ, Arocha JF. Medical expertise as a function of task difficulty. Mem Cogn. 1990;18(4):394–406. doi: 10.3758/bf03197128. [DOI] [PubMed] [Google Scholar]
- 47.Norman GR, Trott AD, Brooks LR, Smith EKM. Cognitive differences in clinical reasoning related to postgraduate training. Teach Learn Med. 1994;6(2):114–120. doi: 10.1080/10401339409539657. [DOI] [Google Scholar]
- 48.Patel VL, Arocha JF, Kaufman DR. Expertise and tacit knowledge in medicine. In: Sternberg RJ, Horvath JA, editors. Tacit knowledge in professional practice: Researcher and practitioner perspectives. Mahwah: Lawrence Erlbaum; 1999. pp. 75–120. [Google Scholar]
- 49.Dreyfus HL, Dreyfus SE. Mind over machine: The power of human intuition and expertise in the era of the computer. Oxford: 1986.
- 50.Eraut M. Non-formal learning and tacit knowledge in professional work. Br J Educ Psychol. 2000;70(Pt 1):113–136. doi: 10.1348/000709900158001. [DOI] [PubMed] [Google Scholar]
- 51.Abernathy CM, Hamm RM. Surgical intuition: What it is and how to get it. Philadelphia: 1995.
- 52.Hamm RM. Clinical intuition and clinical analysis: Expertise and the Cognitive Continuum. In: Dowie J, Elstein A, editors. Professional judgement. A reader in clinical decision making. Cambridge: Cambridge University Press; 1988. pp. 78–104. [Google Scholar]
- 53.Polanyi M. The Tacit Dimension. London: Routledge and Kegan Paul; 1967. [Google Scholar]
- 54.Sternberg RJ, Horvath JA. Tacit knowledge in professional practice: Researcher and practitioner perspectives. Mahwah: Lawrence Erlbaum; 1999. [Google Scholar]
- 55.Schon D. The reflective practitioner: How professionals think in action. New York: Basic Books; 1983. [Google Scholar]
- 56.Boreham NC. The dangerous practice of thinking. Med Educ. 1994;28(3):172–179. doi: 10.1111/j.1365-2923.1994.tb02695.x. [DOI] [PubMed] [Google Scholar]
- 57.Ferreira MB, Garcia-Marques L, Sherman SJ, Sherman JW. Automatic and controlled components of judgment and decision making. J Pers Soc Psychol. 2006;91(5):797–813. doi: 10.1037/0022-3514.91.5.797. [DOI] [PubMed] [Google Scholar]
- 58.Epstein S. Integration of the cognitive and the psychodynamic unconscious. Am Psychol. 1994;49(8):709–724. doi: 10.1037/0003-066X.49.8.709. [DOI] [PubMed] [Google Scholar]
- 59.Evans JSBT, Frankish K. In Two Minds. Dual processes and beyond. Oxford: Oxford University Press; 2009. [Google Scholar]
- 60.Kahneman D, Frederick S. A Model of Heuristic Judgement. In: Holyoak KJ, Morrison R, editors. The Cambridge Handbook of Thinking and Reasoning. New York: Cambridge University Press; 2005. pp. 267–293. [Google Scholar]
- 61.Slovic P, Finucane M, Peters E, MacGregor DG. The Affect Heuristic. In: Gilovich T, Griffin D, Kahneman D, editors. Heuristics and biases. New York: Cambridge University Press; 2002. pp. 397–420. [Google Scholar]
- 62.Finucane M, Peters E, Slovic P. Judgement and decision making: The dance of affect and reason. In: Schneider SL, Shanteau J, editors. Emerging Perspectives on Judgement and Decision Research. Cambridge: Cambridge University Press; 2003. pp. 327–364. [Google Scholar]
- 63.Rolls ET. Emotion Explained. Oxford: Oxford University Press; 2005. [Google Scholar]
- 64.Berthoz A. Decision making and emotion. Emotion and Reason. The cognitive science of decision making. Oxford: Oxford University Press; 2006. pp. 23–50. [Google Scholar]
- 65.Frijda NH. The Emotions. Cambridge: Cambridge University Press; 1986. [Google Scholar]
- 66.Niedenthal PM, Krauth-Gruber S, Ric F. Psychology of Emotion: Interpersonal, Experential and Cognitive Approaches. New York: Psychology Press; 2006. [Google Scholar]
- 67.Thiele LP. The Heart of Judgment. Practical Wisdom, Neuroscience, and Narrative. New York: Cambridge University Press; 2006. [Google Scholar]
- 68.Naqvi N, Shiv B, Bechara A. The Role of Emotions in Decision Making: a Cognitive Neuroscience Perspective. Curr Dir Psychol Sci. 2006;15(5):260–264. doi: 10.1111/j.1467-8721.2006.00448.x. [DOI] [Google Scholar]
- 69.Damasio AR. Descartes’ Error: Emotion, Reason, and the Human Brain. New York: Avon; 1994. [Google Scholar]
- 70.Bechara A, Damasio H, Damasio AR. Emotion, decision making and the orbitofrontal cortex. Cereb Cortex. 2000;10(3):295–307. doi: 10.1093/cercor/10.3.295. [DOI] [PubMed] [Google Scholar]
- 71.Craig AD. How do you feel—now? The anterior insula and human awareness. Nat Rev Neurosci. 2009;10:59–70. doi: 10.1038/nrn2555. [DOI] [PubMed] [Google Scholar]
- 72.LeDoux JE. Emotion circuits in the brain. Annu Rev Neurosci. 2000;23:155–184. doi: 10.1146/annurev.neuro.23.1.155. [DOI] [PubMed] [Google Scholar]
- 73.Eva KW. What every teacher needs to know about clinical reasoning. Med Educ. 2004;39(1):98–106. doi: 10.1111/j.1365-2929.2004.01972.x. [DOI] [PubMed] [Google Scholar]
- 74.Greenhalgh T. Narrative based medicine: narrative based medicine in an evidence based world. BMJ. 1999;318(7179):323–325. doi: 10.1136/bmj.318.7179.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gaver A, Borkan JM, Weingarten MA. Illness in context and families as teachers: a year-long project for medical students. Acad Med. 2005;80(5):448–451. doi: 10.1097/00001888-200505000-00007. [DOI] [PubMed] [Google Scholar]
- 76.Macnaughton J. Anecdote in clinical practice. In: Greenhalgh T, Hurwitz B, editors. Narrative based medicine: dialogue and discourse in clininal practice. London: BMJ Publications; 1999. pp. 202–211. [Google Scholar]
- 77.Baarts C, Tulinius C, Reventlow S. Reflexivity—a strategy for a patient-centred approach in general practice. Fam Pract. 2000;17(5):430–434. doi: 10.1093/fampra/17.5.430. [DOI] [PubMed] [Google Scholar]
- 78.Mann K, Gordon J, MacLeod A. Reflection and reflective practice in health professions education: a systematic review. Adv Health Sci Educ Theory Pract. 2009;14(4):595–621. doi: 10.1007/s10459-007-9090-2. [DOI] [PubMed] [Google Scholar]
- 79.Aukes LC, Geertsma J, Cohen-Schotanus J, Zwierstra RP, Slaets JP. The effect of enhanced experiential learning on the personal reflection of undergraduate medical students. Med Educ Online. 2008;13:15. doi: 10.3885/meo.2008.Res00279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Eva KW, Hatala RM, Leblanc VR, Brooks LR. Teaching from the clinical reasoning literature: combined reasoning strategies help novice diagnosticians overcome misleading information. Med Educ. 2007;41(12):1152–1158. doi: 10.1111/j.1365-2923.2007.02923.x. [DOI] [PubMed] [Google Scholar]
- 81.Ark TK, Brooks LR, Eva KW. The benefits of flexibility: the pedagogical value of instructions to adopt multifaceted diagnostic reasoning strategies. Med Educ. 2007;41(3):281–287. doi: 10.1111/j.1365-2929.2007.02688.x. [DOI] [PubMed] [Google Scholar]