Abstract
BACKGROUND
Information technology offers the promise, as yet unfulfilled, of delivering efficient, evidence-based health care.
OBJECTIVE
To evaluate whether a primary care network-based informatics intervention can improve breast cancer screening rates.
DESIGN
Cluster-randomized controlled trial of 12 primary care practices conducted from March 20, 2007 to March 19, 2008.
PATIENTS
Women 42–69 years old with no record of a mammogram in the prior 2 years.
INTERVENTIONS
In intervention practices, a population-based informatics system was implemented that: connected overdue patients to appropriate care providers, presented providers with a Web-based list of their overdue patients in a non-visit-based setting, and enabled “one-click” mammography ordering or documented deferral reasons. Patients selected for mammography received automatically generated letters and follow-up phone calls. All practices had electronic health record reminders about breast cancer screening available during clinical encounters.
MAIN MEASURES
The primary outcome was the proportion of overdue women undergoing mammography at 1-year follow-up.
KEY RESULTS
Baseline mammography rates in intervention and control practices did not differ (79.5% vs 79.3%, p = 0.73). Among 3,054 women in intervention practices and 3,676 women in control practices overdue for mammograms, intervention patients were somewhat younger, more likely to be non-Hispanic white, and have health insurance. Most intervention providers used the system (65 of 70 providers, 92.9%). Action was taken for 2,652 (86.8%) intervention patients [2,274 (74.5%) contacted and 378 (12.4%) deferred]. After 1 year, mammography rates were significantly higher in the intervention arm (31.4% vs 23.3% in control arm, p < 0.001 after adjustment for baseline differences; 8.1% absolute difference, 95% CI 5.1–11.2%). All demographic subgroups benefited from the intervention. Intervention patients completed screening sooner than control patients (p < 0.001).
CONCLUSIONS
A novel population-based informatics system functioning as part of a non-visit-based care model increased mammography screening rates in intervention practices.
TRIAL REGISTRATION
ClinicalTrials.gov; NCT00462891
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-010-1500-0) contains supplementary material, which is available to authorized users.
KEY WORDS: primary care, screening, mammography, health information technology, randomized controlled trial
INTRODUCTION
Breast cancer is the most common cancer among women worldwide and is the second most common cause of cancer death.1 Considerable scientific evidence supports screening for breast cancer, and mammography is widely recommended as the preferred screening modality for women at average risk.2–4 Despite broad consensus for routine screening, especially for women 50 to 69 years of age, many eligible women do not receive regular mammograms.5,6
Reminder-based interventions increase rates of breast cancer screening with mammography,7–10 but many are labor intensive and few have taken advantage of recent advances in health information technology that support more efficient population-based screening.11–13 Prior studies have used electronic health records to trigger visit-based reminders, but these reminders compete with other demands during limited clinical visits, are not applicable to patients without a recent office visit, and have been shown to have only a modest impact.14,15 Improving the quality and safety of care through the use of information technology16 will require overcoming barriers at every level: the clinical system, the individual provider, and the patient.11,17,18
We developed and implemented a population-based clinical informatics system for non-visit-based management of primary care patient panels that was efficiently integrated into provider and practice workflow. This system was designed to correctly identify all eligible and at-risk patients in our practice network and to direct pertinent clinical information to the responsible provider so they could easily take action outside of a clinical encounter.19 Our approach was based on a conceptual model of primary care delivery that takes a system-wide population perspective, but assigns responsibility to either individual providers or the practice where an individual receives the most care.19 In a 12-practice cluster randomized effectiveness trial, we tested the impact of this new system on breast cancer screening rates.
METHODS
Study Design and Randomization
We conducted a controlled, cluster randomized trial in 12 primary care practices. Because the intervention was implemented at the practice level, we allocated practices to intervention or usual care control groups. To minimize imbalance between groups, practices were stratified by practice type, the number of eligible patients, baseline mammography rates, and unaffiliated outside facility screening rates. Practices were first categorized based on practice type (block): health centers (4 practices) and non-health centers (8 practices), and then matched on the other three factors within the two blocks. The four health centers were manually matched by the study biostatistician into two sub-blocks. The eight non-health centers were also divided into two sub-blocks; one sub-block had two practices with low baseline mammogram rates, and the other sub-block had the remaining six practices that were similar in terms of the other three factors. Half of the practices within each sub-block were randomized to the intervention (n = 6) or control (n = 6) groups. The lead author enrolled intervention group practices. Providers could not be blinded to group assignment. The Massachusetts General Hospital institutional review board approved the study.
Setting and Participants
Practices in the Massachusetts General Hospital Primary Care Practice-Based Research Network have a uniform management structure with integrated administrative and clinical information systems. Each practice uses a fully functioning electronic health record that has information about preventive screening measures, including mammography, available for use during a clinical encounter, but no uniform system existed for screening referrals outside of a clinical encounter.
From January 1, 2004 to December 31, 2006, 163,028 unique patients were seen in the network, which includes predominantly general internal medicine trained primary care physicians (PCPs). Since some patients may not be connected to a specific PCP, but may rather receive their care in a single practice from several providers, we applied a validated measure of “connectedness” to assign each eligible patient to either a specific PCP or (for patients who could not be connected to a specific physician) to the primary care practice where they received most of their care. This ensured that PCPs were asked to complete non-visit-based mammography ordering only on their own patients. This measure of connectedness was developed using a previously validated algorithm designed to predict how likely a physician is to identify a patient as “my patient.”20,21
Eligible patients had at least one visit to a study practice, were women 42 to 69 years of age, and had no record of having a mammogram in the 2 years prior to March 20, 2007. Patients were excluded if they had a PCP outside of the network, had previously undergone bilateral mastectomy, or had died.
Study Intervention
The informatics application was implemented in the six intervention practices for a 1-year period from March 20, 2007 until March 19, 2008. Intervention practice physicians had access to a Web page listing all of their own eligible patients. Each intervention practice designated one individual as a population manager that had access to a Web page listing all patients in their practice not connected to a specific physician. Population managers, including practice nurses, medical assistants, and non-clinical staff previously involved in case management activities, performed the same functions for practice-connected patients as physicians did for their own patients. Each physician and population manager was linked with a practice delegate with their own version of the population management Web page used to facilitate tracking, scheduling, and documenting mammograms for those patients needing contact.
Provider Training Study staff scheduled time with intervention practice personnel before the study start date to describe study goals and to demonstrate the system. Step-by-step instructions were available through a help function within the system.
Physician and Practice Population Manager Role In the intervention practices, physicians (for physician-connected patients) and population managers (for practice-connected patients) received an initial e-mail describing the system with a hyperlink directing them to a population screening Web page that included a list of their patients overdue for screening mammography. Providers also received reminder e-mails at approximately 3 and 8 months after study initiation. Mailed reminder letters and a step-by-step instruction sheet were sent after 2 months to physicians who had not yet used the system.Each provider could also access the application directly from the hospital’s electronic health record (EHR) system. This population management page included: (1) a list of eligible patients overdue for mammography, (2) clinically relevant decision support information to help providers decide whether or not to initiate patient contact (including patient age, date of last completed screening mammogram, date of next scheduled visit, and EHR health maintenance notes that contained free text information such as prior or pending testing at unaffiliated facilities, or prior refusals), and (3) an actionable component (electronic checkboxes) that was used to initiate or defer the mammography screening process (Online Video 1). The list of overdue patients initially included those who had not completed mammography screening in at least 2 years prior to our study start date. This list was updated on a nightly basis through an automated process that added patients to provider lists if they became overdue for screening during the study period and removed patients if screening was completed. When using the system, a provider could schedule a patient for mammography through a centralized process that started with a patient letter. Providers could also document a reason to defer screening if mammography was not needed or appropriate for a patient, which removed the patient from their list.
Central Administration Role A project coordinator acted as the system’s administrator. Patients designated for mammography screening received practice-specific, personalized letters (written in English only) from the patient’s physician or from the practice’s medical director (for practice-connected patients) that informed patients of the value of mammography screening and included instructions for patients to schedule mammograms directly with the hospital’s radiology department. The patient was then transferred to a practice delegate list to facilitate follow-up. For patients who may have had a mammogram outside the Partners Healthcare System, the letter contained a central phone and fax number to leave confidential information about test results. Study personnel entered this information into the patient’s EHR as “patient reported data,” and the patient was removed from the overdue registry.
Practice Delegate Role Practice delegates (10 individuals, either administrative staff or medical assistants, 2 who spoke Spanish) facilitated follow-up among patients selected as needing screening by their physician or the practice’s population manager. Delegates contacted patients for scheduling if they had been on their list for at least 3 weeks (to give patients time to schedule a test on their own or provide outside test information) (Online Video 2). Patients who scheduled their own mammogram were automatically removed from the practice delegate’s list by the informatics tool. Delegates could remove patients from their list by scheduling them for a mammogram or documenting an appropriate deferral reason. If a scheduled mammogram was not completed, the tool added the patient back to the delegate’s list.
Outcomes and Follow-up
Patient characteristics and mammography data were obtained from an electronic central data repository at Partners Healthcare.22 Mammograms and the date of completion over a 1-year follow-up period were obtained from electronic reports or billing data. A 10% random chart review was performed to determine the rate of mammograms performed outside of our network during the 2 years prior to the study start date. Physician characteristics (age, gender, practice location, and years since medical school graduation) were obtained from the hospital registrar. The informatics system collected information on usage by providers and delegates (including date and time of all actions).
The primary outcome was the proportion of patients overdue at baseline who completed a mammogram during the study period in intervention and control practices using intention-to-treat analyses. A mammogram was considered to have been completed if there was an electronic report for an imaging test at a Partners institution or if a mammogram was listed in billing data for the patient. This ascertainment of mammograms was performed identically in intervention and control groups. To estimate the percentage of eligible patients who did not have an electronic report or bill but may have had a mammogram performed at an unaffiliated facility during the 1-year follow-up study period, we randomly reviewed 5% of medical records weighted by practice size searching for information on outside tests. Secondary outcomes included time to mammography completion in overdue patients in intervention and control groups. Other outcomes included provider and delegate use of the electronic system and mammography deferral information.
Statistical Analyses
We compared patient and physician/practice characteristics between intervention and control groups using two-sample t-tests or chi-square tests, as appropriate. Chi-square tests were used to compare physician and practice population manager usage of the Web-based system in intervention practices. For the primary outcome, we compared the proportion of patients who completed a mammogram during the study period in intervention and control practices. To account for the clustering of patients from the same physician or population manager, we used logistic regression with generalized estimating equations techniques23 (PROC GENMOD, SAS version 9.1.3, SAS Institute, Cary, NC) in the analyses. The physician was considered as the unit of cluster for patients connected with a specific study physician, and the population manager was considered the unit of cluster for patients who could be connected with a practice but not a specific physician. To control for differences in patient and practice characteristics among intervention and control practices, patient age, patient-physician connectedness, race/ethnicity, insurance status, English language proficiency, practice type (health center vs non-health center), and number of months since last practice visit were included in the models as covariates to adjust for potential confounders. As an exploratory data analysis, we also compared the proportion of patients who completed a mammogram in intervention and control practices within relevant demographic subgroups and calculated adjusted odds ratios and confidence intervals. Subgroups included patient age, race/ethnicity, English language proficiency, and insurance status. The time to screening completion survival distributions between intervention and control practices were depicted with Kaplan-Meier curves and compared using a log-rank test. Cox proportional hazard models with the robust sandwich covariance matrix estimate were used to account for clustering while adjusting for potential confounders.
The study was powered so that a sample size of approximately 3,300 patients in each group (equivalent to an effective sample size of 917 patients per group after accounting for clustering) had a >90% power to detect a 10% absolute increase in mammography rates among intervention patients assuming a 20% screening rate among control patients.
RESULTS
Practice/Physician and Patient Characteristics
Figure 1 depicts the flow of practice clusters and patients through the trial. Among 32,688 eligible women, 6,730 (20.6%) had not completed a mammogram in at least 2 years at the start of the study and represented the study population (3,054 in intervention and 3,676 in control groups). Baseline mammography rates in intervention and control groups were similar (79.5% vs 79.3%, p = 0.73).
Figure 1.
CONSORT diagram for cluster randomized trials depicting the flow of study practice clusters and patients through eligibility assessment, randomization, intervention, and outcome analysis.
Practice, physician, and patient characteristics are shown in Table 1. Two practices in each arm were community health centers. There were 64 physicians in the 6 intervention arm practices and 74 physicians in the 6 control arm practices. There were no significant differences between intervention and control practice physicians in age, gender, years since medical school graduation, and years in the network. A similar percentage of patients in intervention and control practices was connected to a specific physician. Intervention patients were slightly younger, more likely to be non-Hispanic white, speak English, and have commercial health insurance.
Table 1.
Practice and Patient Characteristics by Intervention Group Status at Baseline
| Total | Intervention group | Control group | P-Value | |
|---|---|---|---|---|
| Practice/physician characteristics, N | ||||
| Number of practice sites | 12 | 6 | 6 | |
| Community health center | 4 | 2 | 2 | |
| Number of physicians (median per practice) | 138 (12.5) | 64 (10.5) | 74 (13.5) | |
| Age, mean (SD) | 47.2 (9.8) | 47.4 (9.9) | 47.0 (9.8) | 0.78 |
| Gender, % female (SD) | 69 (50%) | 31 (48%) | 38 (51%) | 0.86 |
| Years since medical school graduation, mean (SD) | 19.5 (10.0) | 19.9 (10.2) | 19.2 (9.9) | 0.67 |
| Years in primary care network, mean (SD) | 14.6 (10.0) | 14.2 (10.4) | 14.8 (9.8) | 0.72 |
| Patient characteristics, N (%) | N = 6,730 | N = 3,054 (45%) | N = 3,676 (55%) | |
| Patient-physician connectedness status | 0.49 | |||
| Physician-Connected | 3,691 | 1,689 (55%) | 2,002 (54%) | |
| Practice-Connected | 3,039 | 1,365 (45%) | 1,674 (46%) | |
| Age, mean (SD) | 54.0 (8.0) | 53.7 (7.9) | 54.2 (8.0) | 0.02 |
| Median | 52.9 | 52.7 | 53.2 | |
| Ethnicity | <0.001 | |||
| Non-Hispanic white | 5,068 | 2,395 (78%) | 2,673 (73%) | |
| Hispanic | 554 | 143 (5%) | 411 (11%) | |
| African-American | 500 | 211 (7%) | 289 (8%) | |
| Asian | 317 | 170 (6%) | 147 (4%) | |
| Other /unknown | 291 | 135 (4%) | 156 (4%) | |
| Primary language spoken, English | 6,062 | 2,820 (92%) | 3,242 (88%) | <0.001 |
| Insurance status | <0.001 | |||
| Commercial health insurance | 4,163 | 2,057 (67%) | 2,106 (57%) | |
| Government insurance | 1,832 | 748 (24%) | 1,084 (29%) | |
| Medicare | 933 | 393 (13%) | 540 (15%) | |
| With secondary Medicaid | 383 | 134 (4%) | 249 (7%) | |
| Medicaid | 899 | 355 (12%) | 544 (15%) | |
| No insurance, self-pay | 735 | 249 (8%) | 486 (13%) | |
| Months since last practice visit, mean (SD) | 10.7 (9.7) | 10.8 (9.8) | 10.6 (9.6) | 0.50 |
| Practice visits in past 3 years, mean number (SD) | 6.6 (7.0) | 6.5 (6.7) | 6.6 (7.3) | 0.73 |
Random chart review to determine the rate of documented mammograms performed outside of our network during the 2 years prior to the study start date showed that overdue intervention patients were more likely to have had an outside mammogram than overdue control patients (16.0% vs 8.3%, p = 0.004).
Mammography Screening Rates at Study Completion
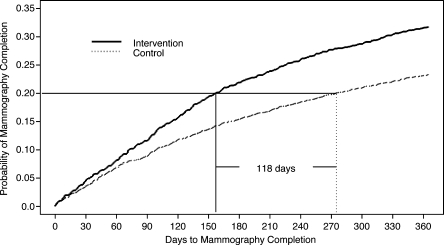
Among women overdue for a mammogram, adjusted mammography rates after 1-year follow-up were significantly higher in the intervention arm compared with the control arm [31.4% vs 23.3%, difference: 8.1% (5.1–11.2), p < 0.001] (Table 2). Adjusted screening rates were higher for intervention practice patients connected with a physician [36.3% vs 28.3% in control arm, difference: 8.0% (4.0–12.3), p < 0.001] or with a practice [25.5% vs 17.4% in control arm, difference: 8.1% (4.9–11.7), p = 0.01]. The time to screening completion was shorter among patients in the intervention group (Fig. 2). For example, the time from the start of the study to the point when 20% of patients had obtained mammograms was 4 months sooner in the intervention population relative to the control population. The hazard ratio for the intervention group was 1.4 [95% confidence interval (CI) 1.26–1.57, p < 0.001] after controlling for potential confounding factors.
Table 2.
Mammography Rates Among Intervention and Control Patients at Least 2 Years Overdue for Breast Cancer Screening
| Unadjusted rates | Adjusted rates* | |||||
|---|---|---|---|---|---|---|
| Intervention | Control | Difference (95% CI) | P-value | Difference (95% CI) | P-value | |
| All patients | 969/3,054 (31.7%) | 857/3,676 (23.3%) | 8.4% (6.3–10.6) | <0.001 | 8.1% (5.1–11.2) | <0.001 |
| Physician-Connected | 628/1,689 (37.2%) | 566/2,002 (28.3%) | 8.9% (5.9–11.9) | <0.001 | 8.0% (4.0–12.3) | <0.001 |
| Practice-Connected | 341/1,365 (25.0%) | 291/1,674 (17.4%) | 7.6% (4.7–10.5) | <0.001 | 8.1% (4.9–11.7) | 0.01 |
*Adjusted rates and p-values were obtained from multiple logistic regression models comparing intervention and control groups controlling for patient age, race/ethnicity, insurance status, English language proficiency, practice type (health center vs non-health center), and number of months since last practice visit using cluster analysis with generalized estimating equations methods. The “All Patients” model also adjusted for patient-provider connectedness. Models were adjusted to the covariate levels that produced the same adjusted and unadjusted rates in the control group.
Figure 2.
Kaplan-Meier curve of time to mammography completion during the 1st year of follow-up among women overdue for breast cancer screening in intervention and control groups. The time from the start of the study to the point when 20% of patients had completed screening is depicted by the horizontal line. The difference between the intervention and control populations is depicted by the vertical lines.
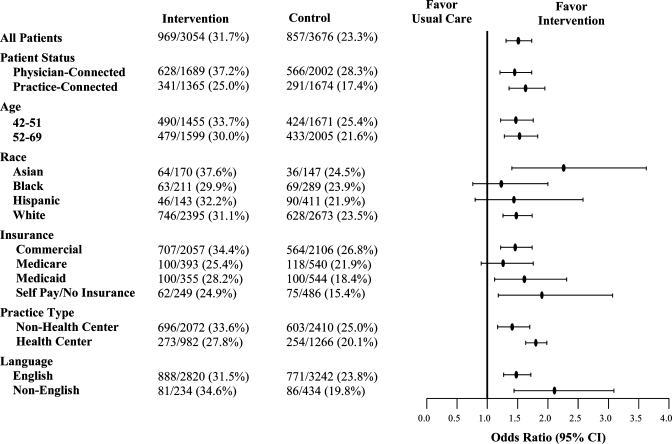
The overall adjusted relative odds of a patient completing a mammogram was significantly higher for intervention vs. control patients (odds ratio 1.51; 95% CI 1.31–1.73). The intervention was similarly beneficial for patients regardless of patient-physician connectedness, age, race/ethnicity, insurance status, language spoken, and practice type (Fig. 3). There were no significant interactions between intervention status and patient or practice characteristic (all p-values >0.15), though the intervention may have been slightly more effective in health center practices (OR 1.80: 95% CI 1.63–1.98) than non-health center practices (OR 1.41: 95% CI 1.17–1.70, p-value for interaction = 0.18). There was no difference in the relative impact of the intervention among physicians based upon years in practice. However, the relative impact of the intervention was greater in younger physicians (≤47 years old; OR 1.90: 95% CI 1.54–2.36) than older physicians (>47 years old; OR 1.17: 95% CI 0.91–1.50, p-value for interaction 0.01).
Figure 3.
Adjusted odds ratios and unadjusted rates for breast cancer screening in intervention and control groups in patient and practice subgroups. Odds ratios compare patients in intervention and control groups controlling for patient age, patient-physician connectedness, race/ethnicity, English language proficiency, practice type (health center vs non-health center), and number of months since last practice visit using cluster analysis with generalized estimating equation methods. For each subgroup analysis, the analogous covariable was removed from the model.
To assess whether intervention patients also had higher rates of mammogram performed at a facility outside of our network, a random chart review of patients who did not have a mammogram report or bill during the 1-year follow-up period was performed. Among 245 randomly selected patients, those in the intervention group were more likely to have an outside mammogram than patients in the control group (9.2% vs 2.3%, p = 0.02).
Use of the Population-Based Informatics System
All intervention practice population managers (6 of 6, 100%) and 59 of 64 intervention physicians (92.2%) used the Web-based system during the study period. Action was taken by physicians in 1,317 (80.0%) physician-connected intervention patients [1,042 (61.7%) were contacted and 275 (16.3%) were deferred] and by population managers in 1,335 (97.8%) practice-connected intervention patients [1,232 (90.3%) were contacted and 103 (7.6%) were deferred] (Table 3). The most commonly chosen reason for deferring patient contact was mammography completion at a non-Partners Healthcare System facility (43.3% of physician-connected and 68.0% of practice-connected intervention patients).
Table 3.
Mammography Informatics System Utilization for Intervention Practices
| Process measures, N (%) | Physician system usage N = 1,689 (55.3) | Population manager system usage N = 1,365 (44.7) | P- value |
|---|---|---|---|
| Any action taken | 1,317/1,689 (78.0) | 1,335/1,365 (97.8) | <0.001 |
| No action taken | 372/1,689 (22.0) | 30/1,365 (2.2) | <0.001 |
| Patient contacted via letter | 1,042/1,689 (61.7) | 1,232/1,365 (90.3) | <0.001 |
| Returned/un-mailed letters | 28/1,042 (2.7) | 147/1,232 (11.9) | <0.001 |
| Patient deferred | 275/1,689 (16.3) | 103/1,365 (7.6) | <0.001 |
| Mammogram complete | 119/275 (43.3) | 70/103 (68.0) | |
| Mammogram scheduled | 20/275 (7.3) | 8/103 (7.8) | |
| Patient deceased | 8/275 (2.9) | 0/103 (0.0) | |
| Informed refusal | 62/275 (22.6) | 20/103 (19.4) | |
| Not eligible | 9/275 (3.3) | 1/103 (1.0) | |
| Not my patient | 2/275 (0.7) | 1/103 (1.0) | |
| Prior bilateral mastectomy | 29/275 (10.6) | 3/103 (3.1) | |
| Other | 26/275 (9.5) | 0/103 (0.0) |
DISCUSSION
We conducted a cluster-randomized clinical trial to test the impact of a novel population-based informatics intervention to increase mammography rates in a primary care network. We demonstrated significantly higher mammography rates in intervention practices for women who were overdue for screening compared to control practices. The easy-to-use Web-based electronic system was accessed by over 90% of intervention providers, and intervention mammography rates were higher in all examined patient demographic sub-groups.
Our results extend prior studies demonstrating the benefit of reminder systems for improving preventive cancer screening rates in general and for mammography in particular.7–10,12–14,17,24–27 To date, most computerized systems have focused on reminders during office visits,9,14,28,29 although some have used population-based reminder systems targeted to all eligible women.7,13,26 While traditional point-of-care reminder systems involve physicians directly in clinical decision making, we are not aware of population-based electronic systems with the screening intervention controlled by a clinician. Chaudhry et al. studied a Web-based population-based system used by secretaries in a single practice.7 Our study extends this work by focusing on patients who have not had breast cancer screening for at least 2 years, efficiently involving clinicians, and performing the study in a large, heterogeneous primary care network. To address limitations of existing approaches, we developed a conceptual model of primary care preventive services that relies on an inclusive, system-wide population perspective to connect patients with their specific physician or the practice where they received the most care. Because taking a position of inclusive population management requires moving beyond the confines of an outpatient visit, we implemented a visit-independent clinical information system to collect, organize, and present clinical data, and support and enhance provider workflow.19 This population-based perspective required training practice personnel in patient outreach efforts. This approach parallels the vision of the “medical home” where care is not episodic and office-based, but instead is continuous and location independent.30 Our study provides rigorous evidence that a non-visit-based population surveillance approach represents a feasible and effective approach to deliver preventive care.
Prior research has shown that systematic screening initiatives are more successful when they take advantage of established patient-provider relationships.31,32 We hypothesized that correctly categorizing patients based on their connection to a specific physician would let physicians use their unique knowledge to better allocate resources and interventions to improve care.20 Higher rates of appropriate deferrals by physicians support the role of such personal knowledge. Our approach of efficiently including physicians in the decision-making process for patients closely linked to them while using a practice population manager to screen patients without a close physician connection represents a novel model of care that seeks to maximize the benefit of non-visit-based care without diminishing the role of the traditional patient-provider relationship.20 Removing routine but time-consuming tasks that could be amenable to non-visit-based care plans may have the additional benefit of allowing more time during the office visit to address other important topics.33,34 In this way, our care model is designed to augment the face-to-face contact that both fosters patient-physician connectedness and provides the physician with the unique knowledge needed to use such systems.
For overdue patients not connected to a specific physician, we used practice population managers to help ensure screening for these patients. Most of these population managers were already performing similar activities to meet pay-for-performance contract activities for our managed care population. Efforts to increase the use of office personnel for such non-visit-based care will require new payment mechanisms.35
Our study is one of the largest controlled trials of an informatics-based primary care intervention. The major study limitation is generalizing results beyond a single primary care network with a well-developed information technology infrastructure. However, our results may be viewed as a goal for integrated care, such as proposed in the medical home model.30 Because of the nature of our intervention, we could not randomize at the patient level, but rather performed a practice level, cluster-randomized trial. The heterogeneous nature of our practices also support the generalizability of our findings, but led to small differences in patient and practice characteristics between intervention and control groups. We adjusted results to control for these differences, and our subgroup analyses show similar benefit for the intervention across each of these characteristics.
The 8% absolute increase in screening between intervention and control groups is relatively modest, but we believe is clinically relevant. Given the high baseline rate of screening in our network (79.4%), networks with lower baseline screening rates may expect to see larger increases in screening if they instituted such a program. Our reported mammography rates also likely underestimate the true number of individuals who had a mammogram performed during the study period because we only had access to reports within our health care system. The slightly higher baseline rate of outside mammograms in the intervention group found during a random chart review suggests our results likely underestimate the system’s true benefit since fewer patients in the intervention group were truly overdue for screening. This is also supported by higher rates of outside mammograms among women in the intervention who did not have a mammogram completed within our health care system during the follow-up period.
Health information technology is often cited as a key to overcoming deficiencies in the quality and safety of care that continue to exist.36 However, the hope that information technology will usher in a transformational change in health care remains largely unfulfilled.16,37,38 We developed and tested a novel informatics tool for population-based breast cancer screening in a primary care network that was designed to redefine rather than simply support traditional models of care delivery. Our trial demonstrated a high level of provider participation and a significant increase in mammography rates. These results support the integral role of information technology to help transform the delivery of health care from visit-based to visit-independent primary care management.
Electronic Supplementary Materials
Below is the link to the electronic supplementary material.
Provider use of the population management Web page: A demonstration of how physicians and population managers accessed the informatics tool, reviewed their list of overdue patients, and used clinically relevant decision support information to initiate or defer the mammography screening process. File Format: .mov (MOV 9599 kb)
Practice delegate use of the population management Web page: A demonstration of how practice delegates accessed the informatics tool, reviewed their list of patients to contact, and directly used the radiology scheduling system for patients who wished to schedule a mammogram or documented deferral reasons for patients who did not. File Format: .mov (MOV 10152 kb)
Acknowledgments
Funding Sponsor This study was supported by a grant from the National Cancer Institute (NCI 1 R21 CA121908) and by institutional funding through the Massachusetts General Hospital Primary Care Operations Improvement program. Dr. Grant is supported by an NIDDK Career Development Award (K23 DK067452). No funding source had a role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. The authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentations Presented at the Society of General Internal Medicine Annual Meeting, Pittsburgh, PA, April 10, 2008 and the 2008 AHRQ PBRN Research Conference, Bethesda, MD, June 11, 2008.
Conflict of Interest None disclosed.
References
- 1.Jemal A, Siegel R, Ward E, et al. Cancer statistics. CA Cancer J Clin. 2008;58(2):71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 2.Armstrong K, Moye E, Williams S, et al. Screening mammography in women 40 to 49 years of age: a systematic review for the American College of Physicians. Ann Intern Med. 2007;146(7):516–26. doi: 10.7326/0003-4819-146-7-200704030-00008. [DOI] [PubMed] [Google Scholar]
- 3.Nelson HD, Tyne K, Naik A, et al. Screening for breast cancer: an update for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;151(10):727–37. doi: 10.1059/0003-4819-151-10-200911170-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tabar L, Yen MF, Vitak B, et al. Mammography service screening and mortality in breast cancer patients: 20-year follow-up before and after introduction of screening. Lancet. 2003;361(9367):1405–10. doi: 10.1016/S0140-6736(03)13143-1. [DOI] [PubMed] [Google Scholar]
- 5.Adams EK, Breen N, Joski PJ. Impact of the National Breast and Cervical Cancer Early Detection Program on mammography and Pap test utilization among white, Hispanic, and African American women: 1996-2000. Cancer. 2007;109(2):348–58. doi: 10.1002/cncr.22353. [DOI] [PubMed] [Google Scholar]
- 6.Smith-Bindman R, Miglioretti DL, Lurie N, et al. Does utilization of screening mammography explain racial and ethnic differences in breast cancer? Ann Intern Med. 2006;144(8):541–53. doi: 10.7326/0003-4819-144-8-200604180-00004. [DOI] [PubMed] [Google Scholar]
- 7.Chaudhry R, Scheitel SM, McMurtry EK, et al. Web-based proactive system to improve breast cancer screening: a randomized controlled trial. Arch Intern Med. 2007;167(6):606–11. doi: 10.1001/archinte.167.6.606. [DOI] [PubMed] [Google Scholar]
- 8.Dietrich AJ, Tobin JN, Cassells A, et al. Telephone care management to improve cancer screening among low-income women: a randomized, controlled trial. Ann Intern Med. 2006;144(8):563–71. doi: 10.7326/0003-4819-144-8-200604180-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shea S, DuMouchel W, Bahamonde L, Bahamonde L. A meta-analysis of 16 randomized controlled trials to evaluate computer-based clinical reminder systems for preventive care in the ambulatory setting. J Am Med Inform Assoc. 1996;3(6):399–409. doi: 10.1136/jamia.1996.97084513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wagner TH. The effectiveness of mailed patient reminders on mammography screening: a meta-analysis. Am J Prev Med. 1998;14(1):64–70. doi: 10.1016/S0749-3797(97)00003-2. [DOI] [PubMed] [Google Scholar]
- 11.Baron RJ. Quality improvement with an electronic health record: achievable, but not automatic. Ann Intern Med. 2007;147(8):549–52. doi: 10.7326/0003-4819-147-8-200710160-00007. [DOI] [PubMed] [Google Scholar]
- 12.Goel A, George J, Burack RC. Telephone reminders increase re-screening in a county breast screening program. J Health Care Poor Underserved. 2008;19(2):512–21. doi: 10.1353/hpu.0.0025. [DOI] [PubMed] [Google Scholar]
- 13.Saywell RM, Jr, Champion VL, Skinner CS, et al. A cost-effectiveness comparison of three tailored interventions to increase mammography screening. J Womens Health (Larchmt) 2004;13(8):909–18. doi: 10.1089/jwh.2004.13.909. [DOI] [PubMed] [Google Scholar]
- 14.Schellhase KG, Koepsell TD, Norris TE. Providers' reactions to an automated health maintenance reminder system incorporated into the patient's electronic medical record. J Am Board Fam Pract. 2003;16(4):312–7. doi: 10.3122/jabfm.16.4.312. [DOI] [PubMed] [Google Scholar]
- 15.Stone EG, Morton SC, Hulscher ME, et al. Interventions that increase use of adult immunization and cancer screening services: a meta-analysis. Ann Intern Med. 2002;136(9):641–51. doi: 10.7326/0003-4819-136-9-200205070-00006. [DOI] [PubMed] [Google Scholar]
- 16.McDonald CJ. Protocol-based computer reminders, the quality of care and the non-perfectability of man. N Engl J Med. 1976;295(24):1351–5. doi: 10.1056/NEJM197612092952405. [DOI] [PubMed] [Google Scholar]
- 17.Engelman KK, Ellerbeck EF, Perpich D, et al. Office systems and their influence on mammography use in rural and urban primary care. J Rural Health. 2004;20(1):36–42. doi: 10.1111/j.1748-0361.2004.tb00005.x. [DOI] [PubMed] [Google Scholar]
- 18.Lester WT, Zai AH, Grant RW, et al. Designing healthcare information technology to catalyse change in clinical care. Inform Prim Care. 2008;16(1):9–19. doi: 10.14236/jhi.v16i1.670. [DOI] [PubMed] [Google Scholar]
- 19.Lester WT, Ashburner JM, Grant RW, et al. Mammography FastTrack: an intervention to facilitate reminders for breast cancer screening across a heterogeneous multi-clinic primary care network. J Am Med Inform Assoc. 2009;16(2):187–95. doi: 10.1197/jamia.M2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Atlas SJ, Grant RW, Ferris TG, et al. Patient-physician connectedness and quality of primary care. Ann Intern Med. 2009;150:325–35. doi: 10.7326/0003-4819-150-5-200903030-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Atlas SJ, Chang Y, Lasko TA, et al. Is this "my" patient? Development and validation of a predictive model to link patients to primary care providers. J Gen Intern Med. 2006;21(9):973–8. doi: 10.1007/BF02743147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murphy SN, Chueh HC. A security architecture for query tools used to access large biomedical databases. Proc AMIA Symp. 2002:552-6. PMC2244204 [PMC free article] [PubMed]
- 23.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–30. doi: 10.2307/2531248. [DOI] [PubMed] [Google Scholar]
- 24.Bonfill X, Marzo M, Pladevall M, et al. Strategies for increasing women participation in community breast cancer screening. Cochrane Database Syst Rev. 2001(1):CD002943. [DOI] [PMC free article] [PubMed]
- 25.Champion V, Skinner CS, Hui S, et al. The effect of telephone versus print tailoring for mammography adherence. Patient Educ Couns. 2007;65(3):416–23. doi: 10.1016/j.pec.2006.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.DeFrank JT, Rimer BK, Gierisch JM, et al. Impact of mailed and automated telephone reminders on receipt of repeat mammograms: a randomized controlled trial. Am J Prev Med. 2009;36(6):459–67. doi: 10.1016/j.amepre.2009.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taplin SH, Barlow WE, Ludman E, et al. Testing reminder and motivational telephone calls to increase screening mammography: a randomized study. J Natl Cancer Inst. 2000;92(3):233–42. doi: 10.1093/jnci/92.3.233. [DOI] [PubMed] [Google Scholar]
- 28.Burack RC, Gimotty PA, George J, et al. Promoting screening mammography in inner-city settings: a randomized controlled trial of computerized reminders as a component of a program to facilitate mammography. Med Care. 1994;32(6):609–24. doi: 10.1097/00005650-199406000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Ornstein SM, Garr DR, Jenkins RG, et al. Computer-generated physician and patient reminders. Tools to improve population adherence to selected preventive services. J Fam Pract. 1991;32(1):82–90. [PubMed] [Google Scholar]
- 30.American Academy of Family Physicians (AAFP), American Academy of Pediatrics (AAP), American College of Physicians (ACP), American Osteopathic Association (AOA). Joint principles of the patient-centered medical home, March 2007. http://www.acponline.org/running_practice/pcmh/understanding/what.htm. Accessed August, 2010.
- 31.Fox SA, Stein JA. The effect of physician-patient communication on mammography utilization by different ethnic groups. Med Care. 1991;29(11):1065–82. doi: 10.1097/00005650-199111000-00001. [DOI] [PubMed] [Google Scholar]
- 32.Grady KE, Lemkau JP, McVay JM, et al. The importance of physician encouragement in breast cancer screening of older women. Prev Med. 1992;21(6):766–80. doi: 10.1016/0091-7435(92)90083-T. [DOI] [PubMed] [Google Scholar]
- 33.Jaen CR, Stange KC, Nutting PA. Competing demands of primary care: a model for the delivery of clinical preventive services. J Fam Pract. 1994;38(2):166–71. [PubMed] [Google Scholar]
- 34.Kottke TE, Brekke ML, Solberg LI. Making "time" for preventive services. Mayo Clin Proc. 1993;68(8):785–91. doi: 10.1016/s0025-6196(12)60638-7. [DOI] [PubMed] [Google Scholar]
- 35.Rosenthal MB. Beyond pay for performance–emerging models of provider-payment reform. N Engl J Med. 2008;359(12):1197–2000. doi: 10.1056/NEJMp0804658. [DOI] [PubMed] [Google Scholar]
- 36.Institute of Medicine (IOM). Crossing the quality chasm: A new health system for the 21st century. National Academy Press: Institute of Medicine. 2001. [PubMed]
- 37.Blumenthal D, DesRoches C, Donelan K, et al. Health information technology in the United States: the information base for progress. Robert Wood Johnson Foundation, 2006. http://www.rwjf.org/files/publications/other/EHRReport0609.pdf. Accessed August, 2010.
- 38.Jha AK, Ferris TG, Donelan K, et al. How common are electronic health records in the United States? A summary of the evidence. Health Aff (Millwood) 2006;25(6):496–507. doi: 10.1377/hlthaff.25.w496. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Below is the link to the electronic supplementary material.
Provider use of the population management Web page: A demonstration of how physicians and population managers accessed the informatics tool, reviewed their list of overdue patients, and used clinically relevant decision support information to initiate or defer the mammography screening process. File Format: .mov (MOV 9599 kb)
Practice delegate use of the population management Web page: A demonstration of how practice delegates accessed the informatics tool, reviewed their list of patients to contact, and directly used the radiology scheduling system for patients who wished to schedule a mammogram or documented deferral reasons for patients who did not. File Format: .mov (MOV 10152 kb)