Abstract
Objectives
Biliary injuries are frequently accompanied by vascular injuries, which may worsen the bile duct injury and cause liver ischemia. We performed an analytical review with the aim of defining vasculobiliary injury and setting out the important issues in this area.
Methods
A literature search of relevant terms was peformed using OvidSP. Bibliographies of papers were also searched to obtain older literature.
Results
Vasculobiliary injury was defined as: an injury to both a bile duct and a hepatic artery and/or portal vein; the bile duct injury may be caused by operative trauma, be ischaemic in origin or both, and may or may not be accompanied by various degrees of hepatic ischaemia. Right hepatic artery (RHA) vasculobiliary injury (VBI) is the most common variant. Injury to the RHA likely extends the biliary injury to a higher level than the gross observed mechanical injury. VBI results in slow hepatic infarction in about 10% of patients. Repair of the artery is rarely possible and the overall benefit unclear. Injuries involving the portal vein or common or proper hepatic arteries are much less common, but have more serious effects including rapid infarction of the liver.
Conclusions
Routine arteriography is recommended in patients with a biliary injury if early repair is contemplated. Consideration should be given to delaying repair of a biliary injury in patients with occlusion of the RHA. Patients with injuries to the portal vein or proper or common hepatic should be emergently referred to tertiary care centers.
Keywords: cholecystectomy, vasculobiliary injury, bileduct injury, biliary injury, hepatic infarction, liver abscess
Introduction
Biliary injury is the most common severe complication of cholecystectomy. Iatrogenic bile duct injury had been well recognized by 19201 and the introduction of laparoscopic cholecystectomy led to a sharp rise in its incidence.2 Biliary injuries are commonly associated with vascular injuries, especially arterial injuries.3 In 1948, Shapiro and Robillard theorized that arterial injury might induce biliary ischaemia and thereby worsen a biliary injury.4 The first actual description of an arterial injury leading to the failure of a biliary repair was provided by Brittain et al.5 In 1994, Madariaga et al. described a patient in whom the biliary injury seemed to potentiate hepatic ischaemia induced by an arterial injury.6 Thus, a second concept began to emerge: namely, that a biliary injury, which disrupted collateral arteries running along the biliary tree, could exacerbate hepatic ischaemia caused by an arterial injury.
Although biliary and vascular injuries frequently occur together, there has been no overview of this subject in the literature and important issues remain unresolved. These include the effect of vascular injuries on the outcome of biliary repairs, and the advisability and timing of vascular and biliary repairs when there is a vasculobiliary injury (VBI). The current study represents an analytical review of the subject with the aim of providing a stable definition and categorization of the problem. The relative frequencies of VBIs, their causes, their effects on the viability of the bile ducts and liver, the clinical implications of such injuries, and their management are examined.
Materials and methods
A literature search was performed in OvidSP from 1966 to February 2009 using multiple title terms that relate biliary injuries to concomitant arterial or portal venous injuries, as well as terms that link biliary injury to liver or bile duct infarction or atrophy. Cross-referenced terms included: ‘biliary’ or ‘bile duct’; ‘hepatic’ and ‘liver’; ‘artery’, ‘vein’, ‘vessel’ and their adjectives; ‘pseudoaneurysm’ and ‘blood supply’; ‘cholecystectomy’ and ‘gallbladder’, and ‘injury’, ‘repair’ and ‘reconstruction’. The term ‘vasculobiliary’ was also used. Articles that referred to VBI as defined below were included. For the section regarding pseudoaneurysms, papers that referred to pseudoaneurysms were included whether or not they reported a VBI. A further literature search was performed using terms related to the vascular anatomy of the bile ducts and terms that link biliary injury or bile duct obstruction to alterations in hepatic blood flow. All bibliographies were searched for pertinent articles that might have been missed in the primary search. All reports of vascular injury accompanying a biliary injury were incorporated, including case reports.
Results
Background
Three types of studies provide valuable background to understanding of the aetiology and pathophysiology of VBIs. These are: cadaveric studies of the blood supply of human bile ducts; radiological studies on the effect of selective arterial occlusion of hepatic arteries in living humans, and investigations into the consequences of bile duct obstruction on portal venous blood flow in animals.
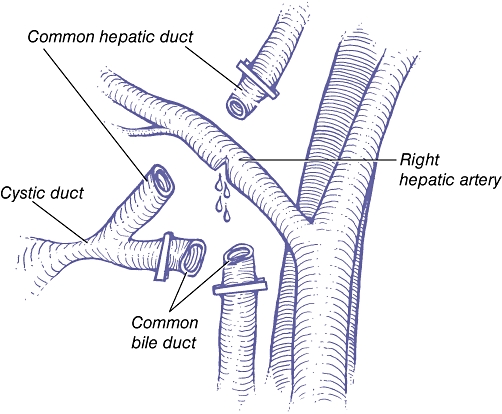
Studies of blood supply to the bile ducts in cadavers
Many studies, dating back to the 19th century, have examined the blood supply of the extrahepatic bile ducts in cadaveric specimens.1,4,7–13 Based on these studies, the blood supply to the ducts can be thought of as having three elements: afferent vessels; marginal arteries, and an epicholedochal plexus. These are illustrated in Figs 1–3. Unlike the liver, bile ducts are supplied only by arteries.13 The marginal artery, labelled the ‘transverse hilar marginal artery’ in Fig. 2, has been called the ‘caudate arcade’14 or ‘communicating arcade’.10 It can function as an arterial shunt between the two sides of the liver and is of great importance in understanding how high biliary injuries contribute to hepatic ischaemia. Branches of the epicholedochal plexus (Fig. 3) pierce the bile duct and supply it through two deeper and finer intracholedochal plexuses within the wall of the bile duct.7
Figure 1.
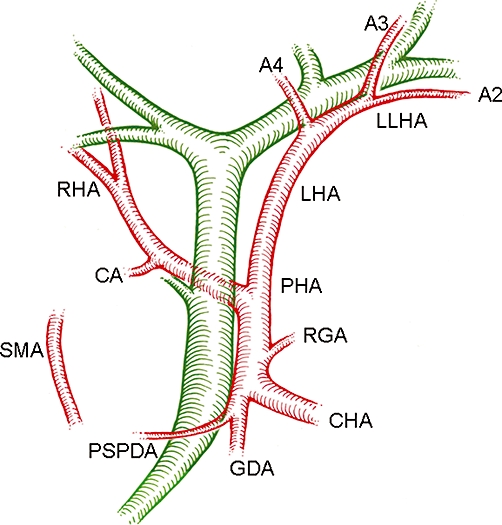
Blood supply to the bile ducts. Element 1: the supplying arteries. The arteries shown can all twig to the marginal arteries or, in some cases, directly supply the epicholedochal plexus. SMA, superior mesenteric artery; PSPDA, posterior superior pancreatoduodenal artery (the most important and constant artery); CHA, common hepatic artery; PHA, proper hepatic artery; RGA, right gastric artery; GDA, gastroduodenal artery; RHA, right hepatic artery; LHA, left hepatic artery; CA, cystic artery; LLHA, left lateral hepatic artery; A2, A3, A4, arteries to segments 2, 3 and 4. Replaced arteries can also supply the bile ducts
Figure 3.
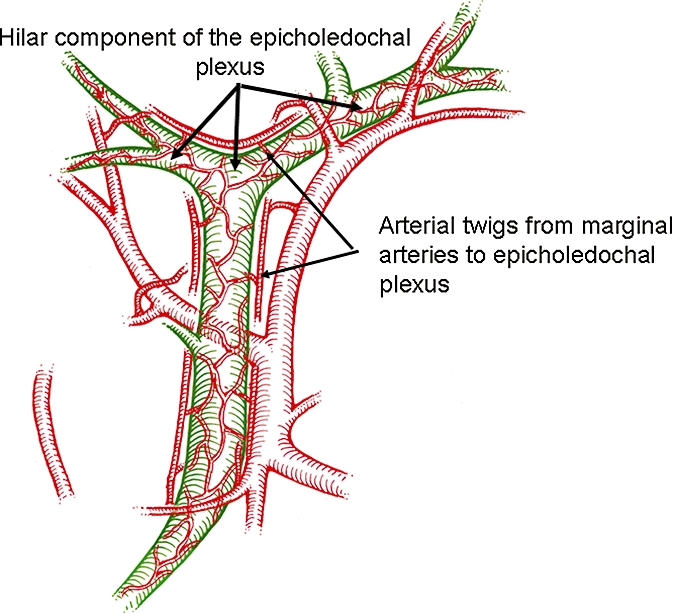
Blood supply to the bile ducts. Element 3: the epicholedochal plexus. The epicholedochal plexus is supplied by the marginal arteries and sometimes directly by the supplying arteries. The part of the network around the confluence of the right and left hepatic ducts has been termed the ‘hilar plexus’. However, it is continuous with the plexus that surrounds the common duct and is probably best considered as the hilar component of the epicholedochal plexus
Figure 2.
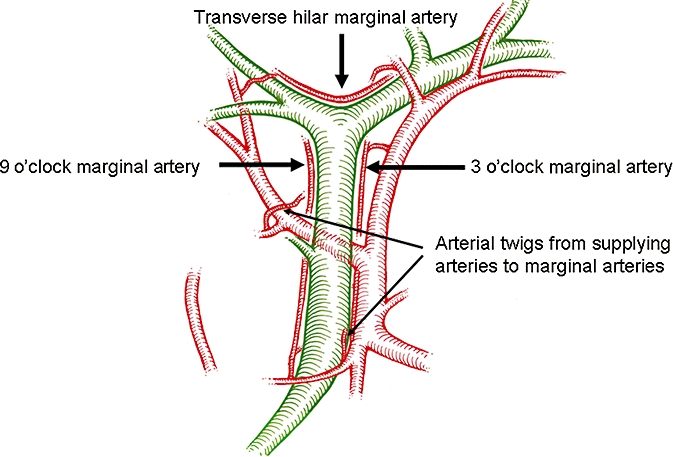
Blood supply to the bile ducts. Element 2: the marginal arteries. Marginal arteries are disposed at 3, 9 and, rarely, 12 o'clock (not shown) on the common bile duct/common hepatic duct. The hilar marginal artery runs across the top of the confluence of the right and left hepatic ducts
The advantage of this complex three-element system is that it provides backup in the form of continuing arterial inflow to the bile ducts when some supplying vessels are disrupted. This redundancy was demonstrated by Vellar,9 who occluded the right hepatic artery (RHA) and the common hepatic duct of cadaveric livers and injected colorized gelatin intra-arterially below the level of occlusion. The entire epicholedochal plexus became perfused, including that on the right hepatic duct. The implication of this finding was that the backup system was adequate to prevent ischaemia, even when a biliary and a vascular injury were combined. However, the perfusing fluids and pressures used in such studies were not physiological and therefore we cannot conclude that sufficient blood flow to maintain the viability of the ducts will occur when the same stress is applied in a living person. In fact, evidence will be provided that this is often not the case.
Arteriographic studies on the effects of selective occlusion of hepatic arteries on blood flow to the liver in humans
The effects of acute selective arterial occlusion on hepatic arterial blood flow in angiographic studies depend upon the level of arterial occlusion and the presence or absence of replaced (aberrant) hepatic arteries.15–17 Reflow after occlusion of the right or left hepatic artery occurs from the unaffected side through the hilar marginal artery and hilar plexus, which function as a preformed collateral arterial route.15–17 Injury to the confluence of the right and left hepatic ducts has the potential to disrupt the hilar shunt, preventing reflow from the left hepatic artery in the case of an RHA injury, thus aggravating hepatic ischaemia induced by the arterial injury. Reflow after occlusion of the proper hepatic artery occurs from proximal portions of the occluded proper hepatic artery, the common hepatic artery, the gastroduodenal artery, the pancreatoduodenal arteries, the intercostal arteries and the phrenic arteries. This collateral flow is present at 10 h and total hepatic arterial flow approaches normal levels by 4 days.17 These routes are not preformed and therefore reperfusion of the liver is delayed under these circumstances. Reflow after occlusion of the common hepatic artery (i.e. proximal to the gastroduodenal artery take-off) occurs from the superior mesenteric artery via the pancreaticoduodenal and gastroduodenal arteries (i.e. via another preformed arterial collateral route). When replaced arteries from the superior mesenteric or left gastric arteries are present, they can also function as preformed arterial collaterals even when the proper hepatic artery is occluded.
Arterial reflow observed in radiographic studies is not readily quantifiable. Therefore, although preformed shunts may open immediately, it is unknown how long it takes for these shunts to attain maximum flow or whether normal flow rates are ever attained. Scintigraphic studies carried out by Mays and Wheeler17 suggest it may take days for flow to recover when a hepatic artery is occluded.
Reduction of portal venous blood flow induced by biliary obstruction in animals
If biliary obstruction impairs portal venous blood flow, this will represent a second mechanism by which a VBI might reduce hepatic blood flow more than an arterial injury alone. Studies examining this possibility have been performed in animals only.18–21
The most convincing studies were performed by Kandaet al. in conscious dogs using electromagnetic flowmeters.21 Biliary obstruction caused an acute decrease in portal venous flow, which persisted for 2 weeks.21 Hepatic arterial flow increased in response, but total liver blood flow was still decreased. Decompression of biliary obstruction reversed these trends.21 The proposed pathogenesis of the drop in portal venous flow is that high biliary pressures increase portal venous resistance, thereby reducing portal venous flow. This, in turn, normally induces an increase in hepatic arterial blood flow.21 However, in the case of an arterial injury the presence of concomitant biliary obstruction could aggravate the hepatic ischaemia induced by the arterial injury alone. In support of this concept, Soares et al. showed that ligation of both the hepatic artery and the bile duct, but not of the artery alone, caused hepatic necrosis in the rat.22 Doppman et al. made similar findings.23
Definition of vasculobiliary injury
According to our search, the first use of the term ‘vasculobiliary injury’ appears in a paper on the arterial supply of the bile duct by Vellar.9 Other authors, including one of the present writers (SMS),24 have subsequently used the term, but it has not been clearly or precisely defined. We have established the following definition after considering the patients presented in this literature.
A vasculobiliary injury is an injury to both a bile duct and a hepatic artery and/or portal vein; the bile duct injury may be caused by operative trauma, be ischaemic in origin or both, and may or may not be accompanied by various degrees of hepatic ischaemia.
Right hepatic artery VBI
Right hepatic artery VBI is by far the most common VBI. In combination, the papers reviewed for this article describe about 225 patients, 92% of whom had a VBI involving the RHA.3,5,6,25–50 The remainder involved other arteries, the portal vein alone or the portal vein in combination with arteries, and sometimes included the RHA.
Right hepatic artery injury during cholecystectomy without concomitant bile duct injury
Key to understanding the consequences of combined injury to the RHA and a bile duct is an understanding of the consequences of an injury to the RHA alone. It seems that occlusion of the RHA without a concomitant biliary or portal vein injury rarely results in clinically significant ischaemia to the liver or bile ducts. This is suggested by two lines of evidence. First, Halasz showed that injury to the RHA or its branches was present in 7% (5/71) of cadavers that had undergone cholecystectomy in life, yet there was no abnormality of the liver or bile ducts.51 The second line of evidence is related to the striking difference in the literature between the ratio of RHA occlusion to pseudoaneurysm in patients with and without associated biliary injury. When there is an associated biliary injury, reports of arterial occlusions are far more common than pseudoaneurysms, but in the absence of a biliary injury, reports of pseudoaneurysms predominate. For instance, a large study by Stewart et al. on combined RHA and bile duct injury refers to seven pseudoaneurysms compared with 77 RHA occlusions.41 Thirteen other papers on the same subject accumulated for this review showed similar results, describing a total of six pseudoaneurysms and 78 instances of RHA occlusion.5,6,31,32,34–39,44 However, we found many reports of the negative consequences of pseudoaneurysms in the absence of a concomitant biliary injury, 52–69 but only two reports on the consequences of occlusion.25,48 It is unlikely that concomitant biliary injury greatly influences whether a pseudoaneurysm or an arterial occlusion results when the artery is injured during a cholecystectomy. Pseudoaneurysms differ from occlusions in that they can present as arterial problems (i.e. bleeding) and it is unlikely that a concomitant biliary injury would reduce the chance that a pseudoaneurysm might become symptomatic. Occlusion is manifested secondarily through its effect on blood flow to the liver or bile ducts, an action that may be magnified by a bile duct injury. Therefore, the best explanation for these observations is that isolated right hepatic occlusions probably occur rather frequently during cholecystectomy and the difference in the ratio in the literature reflects the fact that occlusion of the RHA without a biliary injury rarely produces clinical symptoms. The important corollary is that bile duct injury aggravates the effect of arterial occlusion by some of the mechanisms discussed in the previous sections and makes it much more likely that a clinically significant problem will result.
Right hepatic artery injury associated with a bile duct injury
Incidence
The exact incidence of RHA injury in patients with biliary injuries is unknown. In a large survey, Deziel et al. found that 12% of bile duct injuries were accompanied by an RHA injury, but arteriography was not performed routinely in this population.70 Two centres have reported results of routine arteriography in patients with bile duct injuries. Right hepatic artery injury was detected in 41% of patients in one study39 and 61% of patients in the other.33 Not unexpectedly, these values are higher than in the many case series from centres that have selectively employed arteriography. However, case series of patients undergoing routine arteriography in tertiary centres cannot establish the true incidence of arterial injuries, because patients with VBIs are more likely to be referred to tertiary centres than patients with less serious biliary injuries. One reason for this is that RHA VBIs are usually high and complex.33,36,41 Furthermore, as we will discuss below, anastomotic stricture following biliary reconstruction appears to occur more commonly when an RHA injury has also occurred and patients in whom a biliary reconstruction has failed are also more likely to be referred to tertiary centres. Notably, in one of the studies that used routine arteriography, all of the patients were being treated for recurrent stricture.33 Therefore, the 61% incidence observed in this study should be regarded as indicative of the incidence in this particular population (i.e. patients with strictures after repair of a bile duct injury) as opposed to a population that includes all patients with bile duct injuries. Determination of the true incidence of RHA injury associated with biliary injury would require population studies of biliary injuries in which there was routine assessment of the artery. Consequently, it is likely that the true incidence of RHA injury is probably below the 41% and 61% values reported from tertiary centres and above the 12% found in the large survey by Deziel et al.70 An estimate of 25% would not be unreasonable.
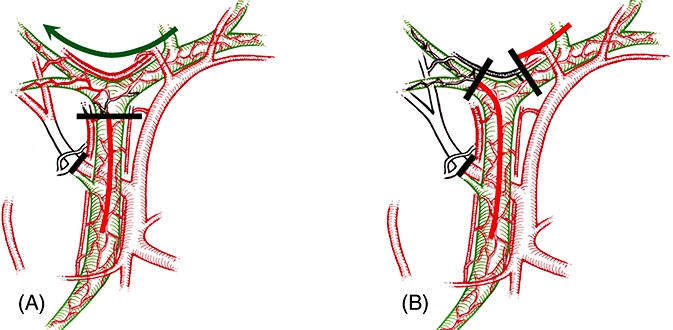
Pathogenesis of RHA VBI
It is highly likely that the reason why the RHA is injured much more commonly than other arteries in association with a biliary injury is simply because it lies in closer proximity to the common hepatic duct.3,5 Davidoff et al. described the following sequence, which they referred to as the ‘classical’ injury3 (Fig. 4). Firstly, the common bile duct is mistaken as the cystic duct and is divided. The cause of the misidentification is frequently a combination of adverse operative conditions and less than optimal techniques of identification, such as the infundibular technique.71 Next, the surgeon, who thinks that the common bile duct is the cystic duct, which has been divided, carries the dissection along the left side of the common hepatic duct in the belief that the dissection is proceeding along the underside of the gallbladder toward the liver. Finally, in order to actually reach the liver bed (i.e. the cystic plate on which the gallbladder rests), the common hepatic duct must be divided. This step is often described in operative notes as dividing a second cystic duct or an accessory duct because of the surgeon's tendency to persist in the anatomic frame of reference in which he or she believes the dissection is to the right of the bile duct when it is actually to the left.72,73 The point at which the common hepatic duct is divided is often exactly where the RHA passes under it and the artery is injured either by direct mechanical or thermal trauma,3 or is clipped on the assumption that it is the cystic artery (Fig. 5). Not surprisingly, a number of authors have noted that a history of brisk bleeding at the time of cholecystectomy is often associated with the intraoperative or postoperative diagnosis of an RHA injury.3,26,27,29,41,45,46,52
Figure 4.
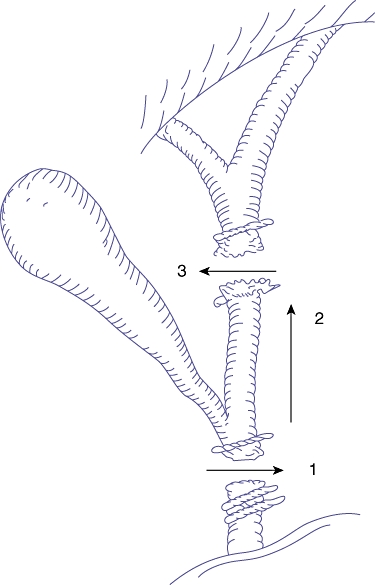
Pathogenesis of the ‘classical’ injury. 1. The common bile duct is mistaken as the cystic duct and is clipped and divided. 2. The dissection is carried up along the left side of the common hepatic duct in the belief that this is the underside of the gallbladder. 3. The common hepatic duct is transected as the surgeon tries to dissect what he or she believes is the gallbladder from the liver bed. If the structure is recognized as a bile duct at this point, it is often thought to be a second cystic duct or an accessory duct. As the common hepatic duct is divided, the right hepatic artery is often injured (see Fig. 6)
Figure 5.
The final stage of the ‘classical’ injury. The hepatic duct has been divided. The right hepatic artery, which lies immediately behind the common hepatic duct, is injured. (Redrawn from Davidoff et al.3)
Effect of RHA injury on outcome of an accompanying biliary injury
There is disagreement regarding whether RHA injury worsens the outcome of a biliary injury. Koffron et al. concluded that it was a key factor because 61% of patients with restricture after biliary–enteric anastomosis had an associated injury to the artery.33 Schmidt et al. found that RHA injury was a significant predictor of poor longterm patency of biliary reconstruction in a multivariate analysis of 54 biliary injuries.38 Brittain et al.5 and Madariagaet al.6 describe frank early necrosis of an anastomosis of the bile duct itself in the presence of an RHA injury. Additionally, several other series have reported that stricture formation after biliary reconstruction is more common in patients with an accompanying RHA injury than in those without vascular injury.34,35,37,44 By contrast, Stewart et al.41 and Alves et al.39 found no effect of RHA injury on longterm outcome after biliary reconstruction and, in a review of this literature, Tzovaras and Dervenis concluded that there was no strong evidence implicating RHA injury in later anastomotic stricture.74
The explanation for this difference in conclusions almost certainly relates to referral patterns and the timing of the biliary repair. Restricture seems to be much more common when repair is undertaken within days of injury34,35,37,38,42,43 and, when restricture occurs after early repair, it is much more likely to involve patients who suffered an RHA injury.34,35,37,38,42,43 This has also been our experience. In a study involving 113 patients with bile duct injuries we reported 12 patients who were known to have suffered an RHA injury, two of whom had early repairs and 10 of whom had late repairs.50 Both patients with early repairs developed biliary restricture, whereas none of the other 10 patients did.50 No other identifiable differences between the patients with early and late repairs, such as extent of injury or level of injury, were found to account for this difference. Twenty other patients not diagnosed with arterial injury underwent early repairs and none developed strictures.50 Series that report low rates of anastomotic problems in the presence of an RHA injury come from centres that have usually performed the repairs late. The series reported by Alves et al.39 and Stewart et al.41 and most of the patients in our series50 fall into this category. Note also that although Koffron et al. implicate RHA injury as pathogenetic in stricture formation after biliary reconstruction, there were no failures among their late repairs,33 although RHA occlusion was present in 61% of patients.
The cause of the difference in results between early and late repairs in the presence of an RHA injury probably lies in the fact that bile duct necrosis can progress after biliary injury and may not reach a stable state for about 3 months.75 Therefore, performing a bile duct reconstruction soon after injury in the presence of an RHA injury risks repairing to a location on the bile duct which may appear viable, but is in fact destined to become fibrotic. Finally, the current review of the literature provides further support to the argument that biliary ischaemia is an important outcome of RHA injury. As the RHA lies at the level of the mid common hepatic duct, we might expect biliary injuries that occur in association with RHA injury to be at that level (E1–E2). Indeed, the videotapes available to Davidoff et al. clearly indicated that the mechanical injury in the ‘classical’ injury occurs at the mid common hepatic duct level.3 However, as reported by several authors, when patients with RHA VBIs are actually seen at tertiary centres, the bile duct injuries tend to be higher in the biliary tree, at the level of the confluence (i.e. E3 and E4 injuries).33,36,41 Therefore, it seems very likely that ischaemia contributes to the final level of a biliary injury when the RHA is also injured. Put another way, the level of a bile duct injury associated with an RHA injury is probably determined in many situations not only by the site of the mechanical injury, but also by the accompanying induced biliary ischaemia.
The important inference of these observations on practice is that assessment of the hepatic arteries should be part of the investigation of all major biliary injuries. Additionally, in the face of an RHA occlusion, consideration should be given to delaying repair unless the artery is repairable (see below). A stronger recommendation is not possible at this time because this conclusion is mainly based on a review of case series. If an early repair is made, the anastomosis should be at a high level, as advocated by Alves et al.39 Although there is no properly defined length of wait to ensure that blood supply is well preserved to the injured duct, most authors with substantial experience in biliary reconstruction wait at least 3 months. During this waiting period, biliary decompression can be achieved by percutaneous transhepatic drainage or by placing percutaneous drains into a subhepatic location in order to collect hepatic bile flow.50
Effect of bile duct injury on collateral blood flow to the right hemiliver in the presence of an RHA injury
As we have noted, RHA injury without a biliary injury rarely results in clinically important hepatic ischaemia because preformed arterial hilar shunts supply enough blood to the right liver to avoid infarction. This shunt, by which blood flows from the left hepatic artery via the hilar marginal artery to a point on the RHA beyond an arterial occlusion, has been demonstrated in several studies15,39,44,49 (Figs 6 and 7A, B). Theoretically, a second shunt, which we will refer to as the ‘longitudinal shunt’, might exist along the 3 o'clock and 9 o'clock marginal arteries. This shunt should carry blood from the gastroduodenal and proper hepatic arteries through the marginal arteries to a point on the RHA beyond the occlusion (Fig. 7C). Figure 8(A) schematically shows the effect of an E1–3 injury (i.e. an injury that results in occlusion or transection of the common hepatic duct below or at the confluence). In such an injury, the longitudinal shunt would be obstructed, but the hilar shunt would remain open and visible on arteriography. However, when the bile duct confluence is injured, such as in an E4 injury, there is potential for the disruption of the hilar shunt. Figure 8(B) shows the effect of an E4 injury, which might obstruct both the longitudinal and hilar shunts.
Figure 6.
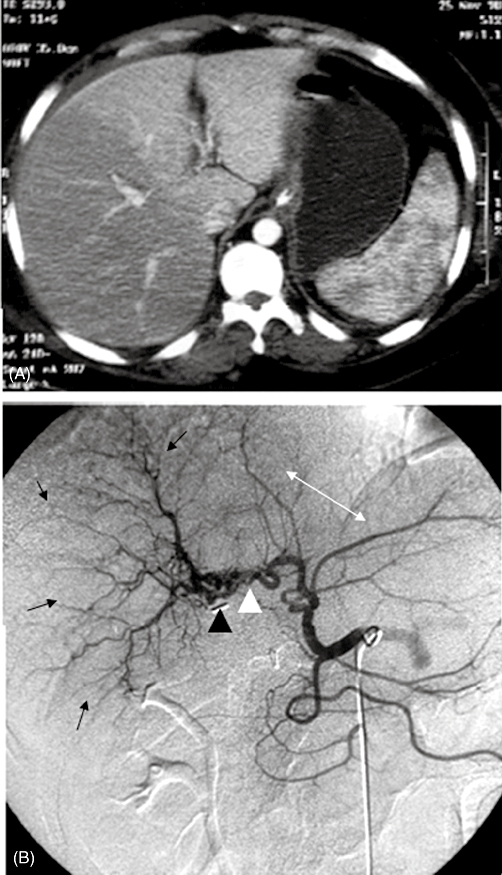
Right hepatic artery (RHA) vasculobiliary injury with collateral flow from left hepatic artery and atrophy of right liver. (A) Computed tomography scan of liver shortly after injury. The arterial phase shows no filling of right liver. (B) Arteriogram performed 2 years later. Abundant arterial collaterals extend from the left hepatic artery to the RHA along the hilar plexus (white arrowhead). The clip which occluded the RHA is also seen (black arrowhead). The arterial pattern of the right liver shows crowding (black arrows) indicative of atrophy of the right liver, whereas the arterial pattern of the left liver shows elongation and spreading characteristic of hypertrophy of the left liver. (Reproduction of original photographs from Mathisen et al.44 by permission)
Figure 7.
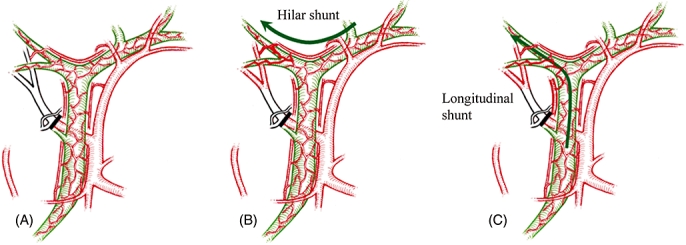
Effect on hepatic blood flow of an injury to the right hepatic artery (RHA) without biliary injury. (A) Occlusion of the RHA results in ischaemia of the right liver, but (B, C) flow is restored by preformed collateral arterial shunts
Figure 8.
Vasculobiliary injury involving the right hepatic artery (RHA). (A) E1–3 injuries leave the hilar shunt open but obstruct the longitudinal shunt and may induce greater hepatic ischaemia than RHA occlusion only. (B) E4 injuries induce greater ischaemia than right hepatic injuries alone by obstructing the important hilar shunt and the longitudinal shunt
The best explanation for the increase in liver ischaemia seen in an RHA injury associated with a bile duct injury as opposed to an RHA injury alone is that bile duct injury eliminates compensatory collateral flow through marginal arteries when the RHA is occluded. Theoretically, E4 injuries which disrupt the hilar shunt would produce more severe injuries than lower injuries which do not. However, whether or not this is so is not determinable from the literature because few studies link the site of bile duct injury to the type and extent of an accompanying liver injury. Another contributing factor to hepatic ischaemia when the bile duct injury leads to bile duct obstruction may be reduction in portal vein blood flow.21 However, it should be remembered that it has not yet been shown that obstructing the bile duct reduces portal vein flow in humans.
Hepatic infarction and ischaemic hepatic atrophy in RHA VBI
There are multiple reports of liver ischaemia of the right hemiliver in patients with an RHA VBI,6,31,34,36,41,43,47,48,76,77 some of which involve multiple patients. These patients either developed a type of slow infarction of the right liver that is associated with the formation of ‘abscesses’ over 1–3 weeks following the injury or they developed ischaemic atrophy. The ‘abscesses’ are probably zones of infarction that have become superinfected. There are no reports of rapid complete infarction requiring emergency right hepatectomy, as is sometimes required when the portal vein is also injured (see below). The incidence of infarction in RHA VBI is probably exaggerated by the tendency to report more serious outcomes as case reports.47,48,77 Based on only those papers that are not case reports,6,34,36,41,43 we might estimate the incidence of right liver infarction in RHA VBI to be about 10% (11/117 cases). Thomsonet al.78 reported four patients with RHA VBIs who underwent right hepatectomy, three in the context of a left hepaticojejunostomy. These procedures were performed 6–95 months after injury and so were clearly not performed for rapid infarction of the right liver, but whether they were carried out for slow infarction, atrophy or because of the effects of recurrent stricture on the right liver is unclear.
Most patients who develop infarction are treated by right hepatectomy6,34,36,41,43 or partial right hepatectomy.41 Death has been reported after right hepatectomy48 or after failed RHA reconstruction43 for this condition. A complete evaluation of the extent of the problem, management strategies, and outcomes is not possible because key details such as times of referral are not provided on a case-by-case basis. Consequently, it is sometimes difficult to determine from the literature whether liver resection for a liver damaged by abscesses was performed at 2 weeks, when the likely cause was ischaemia, or at 2 years, when the abscesses were probably caused by recurrent biliary stricture and resulting cholangitis.
The issue of ‘ischaemic atrophy’ induced by RHA VBI is rarely mentioned in the literature, probably because patients who develop it are asymptomatic44 (Fig. 6). Biliary strictures may also induce atrophy and therefore it is difficult to assess the cause of the atrophy from the available literature. It is also unclear whether intrahepatic abscess secondary to recurrent stricture of a biliary enteric anastomosis is more likely to occur when ischaemic atrophy is also present.
Repair of the RHA in RHA VBI
Immediate repair of the RHA has been undertaken in a number of centres, either by end-to-end anastomosis or with a graft usually taken from the inferior mesenteric vein.6,31,38,42,43 The results have been good in tertiary centres, judged by the non-occurrence of liver infarction and the fact that patients have generally done well in follow-up.6,31,38,42,43 Whether the patients would have done as well without arterial reconstruction is unclear because only about 10% of patients with RHA VBI develop clinically relevant hepatic ischaemia. In addition, the actual number of repairs reported is very low, totalling about a dozen, five of which were reported from one centre.42,43 Opportunities for repair are limited, both because the procedure must be performed within a short time of the occurrence of the injury, ideally within hours, and because the injury is frequently too severe to repair. Several centres with large patient series involving biliary injuries have never performed arterial repairs, either because of the lack of opportunity or because they have adopted a strategy which involves delaying repairs.39,41,50 The risk in not repairing the artery is that slow infarction of the liver will occur. Thus, the conventional recommendation is that early repair of the artery should be performed when the opportunity arises. However, if only 10% of patients with an RHA/bile duct injury develop clinically important hepatic ischaemia, this implies that the majority of patients will do just as well without reconstruction of the artery. The alternative strategy of allowing slow infarction to take place in a minority of patients and treating it by resection, if necessary, may result in better overall outcomes than early operation and reconstruction of all early presentations of RHA VBI. This is an open question for which no clear answer is apparent at this time.
Vasculobiliary injuries involving the portal vein
The portal vein is much less vulnerable to injury at cholecystectomy than the RHA; consequently there are few reports of portal vein injury associated with a major biliary injury. Furthermore, as a result of its rarity, the pathogenesis of this type of injury is not clear. Sixteen such injuries were identified in the current literature review (Table 1). Thirteen were also associated with injury to a major hepatic artery. Seven of the 16 patients developed rapid necrosis of the right liver and required an emergency right hepatectomy 1–16 days after the cholecystectomy (Fig. 9) and three of these patients died of postoperative complications (sepsis or liver failure). Another patient required a liver transplant at day 4 for a combined portal vein and RHA injury, and subsequently died.78 Thus there was a 50% (4/8 cases) mortality rate in patients who developed rapid infarction (Table 1). The value of magnetic resonance imaging (MRI) in obtaining a rapid diagnosis was stressed by Ragozzino et al.79 As noted above, rapid necrosis has not been described in an RHA VBI, but of course we would expect to see a more severe effect when both the artery and vein are occluded. Three patients developed slow necrosis with abscess formation, which required liver resection at 1–12 months after the cholecystectomy (Table 1). One patient, described by de Santibanes et al., underwent a transection of the right portal pedicle, but the portal vein was immediately repaired.49 The patient received an orthotopic liver transplant (OLT) at 2 years, when the right liver was atrophied, but the OLT was required because of the consequences of the biliary injury as opposed to infarction of the right liver. Similarly, in two patients described by Laurent et al., in whom injury occurred to the right portal vein but not to an artery, subsequent resection was required years later because of cholangitis and biliary cirrhosis and not for hepatic infarction76 (Table 1). The series reported by Thomsonet al.78 included four patients with portal vein injuries, three of which were associated with RHA injuries and one with an injury to the common hepatic artery. One patient, who had rapid decompensation and required a transplant on day 4, is mentioned above. Of the other three patients, one underwent a right hepatectomy and survived, one underwent a liver transplant at 4 months and died of hepatic failure and sepsis and the third died at 126 months while waiting for a transplant. Note that patients such as those of Usal et al., who died as the result of a portal vein injury80 but did not have an accompanying biliary injury, are not included in this discussion.
Table 1.
Vasculobiliary injuries involving the portal veina
| Authors | Portal vein injury | Arterial injury | Type of hepatic ischaemia | Type of liver resection | Timing of resection after laparoscopic cholecystectomy | Outcome |
|---|---|---|---|---|---|---|
| Felekouras et al.45 | Main portal vein | Right hepatic artery | Rapid | Right hepatectomy | 1 day | Died on day 16 of sepsis |
| Frilling et al.42 | Main portal vein and superior mesenteric veind | Right hepatic artery | Rapid | Right hepatectomy | 16 days | Died on day 28 of sepsis and multisystem organ failure |
| Madariaga et al.6 | Main portal vein | Right hepatic artery | Rapid | Right hepatectomy | 5 days | Survived |
| Laurent et al.76 patient 2 | Right portal vein | Right hepatic artery | Rapid | Right hepatectomy | 7 days | Survived |
| Strasberg24 | Right portal vein | Right hepatic artery | Rapid | Right hepatectomy | 1 day | Survived |
| Ragozzino et al.79 (patient 1) | Right portal vein | Right hepatic artery | Rapid | Right hepatectomy | 1 day | Died day 15 |
| Ragozzino et al.79 (patient 2) | Right portal vein | Right hepatic artery | Rapid | Right hepatectomy | 1 day | Survived |
| Nishio et al.28 | Right anterior portal vein | Right hepatic artery | Slow with abscess formation | Right hepatectomy | 4 months | Survived |
| Robertson et al.29 | Left portal vein | Proper hepatic arteryc | Slow with abscess formation | Porto-enterostomy, orthotopic liver transplant | 5 months 1 year | Survived |
| de Santibanes et al.49 | Right portal vein (immediate repair) | Right hepatic artery | Atrophy | Orthotopic liver transplantb | 2 years | Survived |
| Laurent et al.76 (patient 7) | Right portal vein | None | None | Right hepatectomyb | 8 years | Survived |
| Laurent et al.76 (patient 8) | Right portal vein | None | None | Right hepatectomyb | 2.5 years | Survived |
| Thomson et al.78 (patient 3) | Right portal vein | None | Not stated | Right hepatectomy | Not stated | Survived |
| Thomson et al.78 (patient 12) | Right portal vein | Right hepatic artery | Not stated | Awaiting liver transplant | Died at 10.5 years | |
| Thomson et al.78 (patient 13) | Left portal vein | Common hepatic artery | Not stated | Orthotopic liver transplant | 4 months | Died |
All patients had an accompanying major biliary injury
The primary reason for orthotopic liver transplant and resection in these patients referred to the consequences of the biliary injury (i.e. cholangitis and biliary cirrhosis), not hepatic ischaemia
Personal communication from the senior author
The portal vein and superior mesenteric vein thrombosis were thought to be secondary to bile peritonitis by the authors
Figure 9.
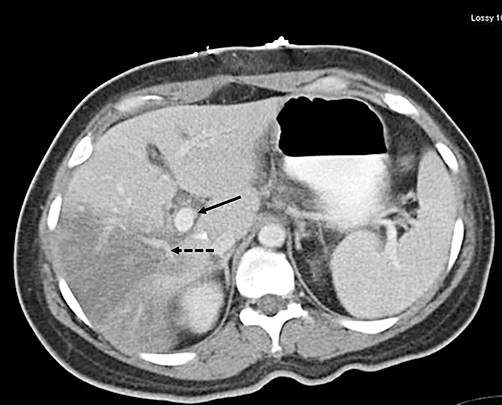
Computed tomography scan showing infarction of right liver resulting from injury to the right hepatic artery and right portal vein. The scan was performed within hours of the cholecystectomy. The right liver shows almost no perfusion. Note the gap between the main portal vein (solid arrow) and the sectional branches (dashed arrow) where the right portal vein would normally be filled with contrast. The sectional veins show some filling through collaterals. (Modified from Strasberg et al.24)
It is highly likely that injuries leading to rapid infarction are under-reported as a result of rapid patient deterioration and death prior to referral to a tertiary centre. It is also unlikely that a patient who died as a consequence of an iatrogenic biliary injury in a community hospital setting would be reported in the literature. Other causes of under-reporting may be that few of these injuries are seen at any one tertiary centre and thus it is difficult to mount an institutional case series, and reluctance to report poor outcome.
Vasculobiliary injuries involving the proper or common hepatic arteries
Nine patients with injury to the proper hepatic artery or common hepatic artery without concomitant portal vein injury32,36,42,47 were identified. Two of these suffered a concomitant portal vein injury29,78 (see Table 1). The detail available in the papers describing these injuries is variable and in some cases additional information was supplied by the authors (Table 2). The serious nature of these injuries may be judged by the fact that several of the patients died. Another patient developed superior mesenteric artery thrombosis of uncertain origin and also died (Table 2). The pathogenesis of the injuries to the common and proper hepatic arteries remains unclear from the available reports. Our previous comments regarding under-reporting also apply to this type of injury.
Table 2.
Vasculobiliary injuries involving major arteries other than the right hepatic artery
| Authors | Arterial injury | Type of hepatic ischaemia | Treatment | Timing of treatment after laparoscopic cholecystectomy | Outcome |
|---|---|---|---|---|---|
| Frilling et al.42a | PHA | None apparent | End-to-end reconstruction of PHA | 1 day | Recovered |
| Frilling et al.42 | PHA | Left liver and CHDb | Reconstruction using saphenous vein | 17 days | Died of MSOF on day 37 |
| Buell et al.36a | CHA | Intrahepatic bilateral bile duct necrosis | Orthotopic liver transplant | 2 years | Recovered |
| Buell et al.36a | CHA | Rapid infarction | Extended right hepatectomy | 5 days | Died of MSOF on day 8 |
| Buell et al.36 | CHA | NA | Supportive | Died | |
| Yan et al.47 | PHA | NA | Orthotopic liver transplantc | NA | Recovered |
| Wudel et al.32 | CHA | NA | NA | NA | NA |
| Wudel et al.32 | CHA | NA | NA | NA | NA |
| Salmen et al.46 | PHA | Liver abscesses | 1. Drainage of abscess | 1.3 months | Recovered |
| 2. Bile duct reconstruction | 2.5 months | ||||
| Mathisen et al.44a | SMA | None; small bowel infarction | Laparotomy | 3 days | Died on day 4 |
Additional details regarding this case were kindly supplied by the authors
This is another example of frank infarction of the bile duct. (See also Madariaga et al.6)
This patient developed biliary cirrhosis and the timing of the transplant is not given. Therefore, it is unclear what role the arterial injury played in the outcome
CHA, common hepatic artery; PHA, proper hepatic artery; SMA, superior mesenteric artery; NA, not available; CHD, common hepatic duct; MSOF, multisystem organ failure
Summary of vasculobiliary injuries
Vasculobiliary injuries may lead to biliary, arterial or hepatic problems and the type and extent of these problems depend on the level of the biliary injury and the vessel(s) injured. A summary of these possibilities is provided in Table 3.
Table 3.
Vasculobiliary injuries: spectrum of clinical effects and time of onset
| 1 Artery |
|---|
| 1.1 Pseudoaneurysm with intraperitoneal or intrabiliary haemorrhage (haematobilia) (presentation: hours to weeks) |
| 2 Bile duct |
|---|
| 2.1 Necrosis of bile duct with generalized peritonitis. When an anastomosis has been performed, this will be manifested as an early breakdown of the anastomosis with fistula, intraperitoneal abscess or generalized peritonitis (presentation: days) |
| 2.2 Stenosis of the bile duct or of an anastomosis to the bile duct leading to hepatic atrophy or cholangitis with or without hepatic abscess (presentation: weeks to years) |
| 2.3 Untreated or unsuccessfully treated stenosis leading to recurrent cholangitis, intrahepatic stones and secondary biliary stenosis (presentation: months to years) |
| 3 Liver |
|---|
| 3.1 Rapid hepatic necrosis with haemodynamic instability (presentation: hours) |
| 3.2 Slow hepatic necrosis with abscess formation (presentation: days to weeks) |
| 3.3 Hepatic atrophy (presentation: months to years; usually asymptomatic) |
Future studies
Future efforts in this area should, of course, focus on prevention. Unfortunately, basic statistics, such as the population incidence of VBI, are lacking because of the lack of mandatory requirements to report surgical complications. The magnitude of the problem(s) caused by VBI is therefore not known. Because the incidence of the more serious types of VBI is low, it is probably necessary that data be pooled if we are to understand the pathogenesis of these injuries, as no single centre will see enough cases to detect a pattern. A registry would be an ideal mechanism. Summation of small case series or even case reports of VBIs may provide valuable insight, especially if standardized reporting methods are adopted. Therefore, a standard method of reporting cases in the literature, especially of the more severe injuries involving the portal vein or proper and common hepatic arteries, should be encouraged. The criteria for judging whether or not a vascular injury has actually occurred need to be formalized. According to our search findings, the only paper to definitively approach the subject was that by Stewart et al.41Table 4 shows and adds to these authors’ criteria for assessing injury to a vascular structure.
Table 4.
Criteria for judging injury to a vascular structure
| 1 Intraoperative identification |
|---|
| 1.1 Ligation or clipping noted during the initial cholecystectomy |
| 1.2 Ligation or clipping noted during a subsequent operation other than bile duct repair |
| 1.3 Ligation or clipping noted during a bile duct repair |
| 2 Photographic identification |
|---|
| 2.1 Ligation or clipping identified on a videotape |
| 2.2 Ligation or clipping identified on intraoperative photographs |
| 3 Radiological identification |
|---|
| 3.1 Hepatic angiography: occlusion, narrowing, intraluminal thrombus or pseudoaneurysm |
| 3.2 Magnetic resonance angiography: occlusion, narrowing, intraluminal thrombus or pseudoaneurysm |
| 3.3 Computed tomographic angiography: occlusion, narrowing, intraluminal thrombus or pseudoaneurysm |
| 3.4 Non-enhancement of a portion of the liver on any of the preceding radiological methods compatible with ischaemia to that portion of the liver |
| 4 Postmortem identification |
|---|
| 4.1 Iatrogenic vascular injury noted during postmortem |
In summary, an analytical review of VBIs revealed the following several findings. Right hepatic artery VBI is the most common variant. This injury is most likely to occur when the common hepatic duct is divided as described in the ‘classical’ injury during laparoscopic cholecystectomy. Injury to the RHA very likely extends the biliary injury to a higher level than the gross observed mechanical injury. Failures of bile duct reconstructions are more common when the bile duct is repaired in the early period after an RHA VBI has occurred because the bile duct is often ischaemic. Therefore, routine evaluation of the hepatic arteries is recommended in all patients with a biliary injury if early repair is contemplated. Consideration should be given to delaying repair of a biliary injury in patients with occlusion of the RHA. Right hepatic artery VBI results in slow hepatic infarction in about 10% of patients. Repair of the artery is rarely possible and the benefit of doing so has not been clearly demonstrated. Injuries involving the portal vein or common or proper hepatic arteries are much less common, but have more serious effects. Rapid infarction of the liver is common in such injuries and patients should be emergently referred to tertiary centres where hepatopancreatobiliary expertise is available. The pathogenesis of such injuries is unclear. Pooling of data and standardized reporting of injuries should help to further delineate the consequences of injuries and, we hope, provide insights into their prevention.
Acknowledgments
The authors are indebted to the following surgeons who provided substantial unpublished data and follow-up information regarding patients in their reports: Joseph Buell (Louisville, KY); Jacques Belghiti (Paris); Andrea Frilling (Essen), and Eduardo de Santibanes (Buenos Aires).
Conflicts of interest
None declared.
References
- 1.Eisendrath DN. Operative injury of the common and hepatic bile ducts. Surg Gynecol Obstet. 1920;31:1–18. [Google Scholar]
- 2.Anonymous. A prospective analysis of 1518 laparoscopic cholecystectomies. The Southern Surgeons Club. N Engl J Med. 1991;325:1517–1518. doi: 10.1056/NEJM199104183241601. [DOI] [PubMed] [Google Scholar]
- 3.Davidoff AM, Pappas TN, Murray EA, Hillern DJ, Johnson RD, Baker ME, et al. Mechanisms of major biliary injury during laparoscopic cholecystectomy. Ann Surg. 1992;215:196–202. doi: 10.1097/00000658-199203000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shapiro AL, Robillard GL. The arterial blood supply of the common and hepatic bile ducts with reference to the problems of common duct injury and repair; based on a series of 23 dissections. Surgery. 1948;23:1–11. [PubMed] [Google Scholar]
- 5.Brittain RS, Marchioro TL, Hermann G, Wadell WR, Strarzl TE. Accidental hepatic artery ligation in humans. Am J Surg. 1964;107:822–832. doi: 10.1016/0002-9610(64)90169-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Madariaga JR, Dodson SF, Selby R, Todo S, Iwatsuki S, Starzl TE. Corrective treatment and anatomic considerations for laparoscopic cholecystectomy injuries. J Am Coll Surg. 1994;179:321–325. [PMC free article] [PubMed] [Google Scholar]
- 7.Parke WW, Michels NA, Ghosh GM. Blood supply of the common bile duct. Surg Gynecol Obstet. 1963;117:47–55. [PubMed] [Google Scholar]
- 8.Nery JR, Frasson E, Rilo HL, Purceli E, Barros MFA, Neto JB, et al. Surgical anatomy and blood supply of the left biliary tree pertaining to partial liver grafts from living donors. Transplant Proc. 1990;22:1492–1496. [PubMed] [Google Scholar]
- 9.Vellar ID. The blood supply of the biliary ductal system and its relevance to vasculobiliary injuries following cholecystectomy. Aust N Z J Surg. 1999;69:816–820. doi: 10.1046/j.1440-1622.1999.01702.x. [DOI] [PubMed] [Google Scholar]
- 10.Gunji H, Cho A, Tohma T, Okazumi S, Makino H, Shuto K, et al. The blood supply of the hilar bile duct and its relationship to the communicating arcade located between the right and left hepatic arteries. Am J Surg. 2006;192:276–280. doi: 10.1016/j.amjsurg.2006.01.046. [DOI] [PubMed] [Google Scholar]
- 11.Northover JMA, Terblanche J. A new look at the arterial supply of the bile duct in man and its surgical implications. Brit J Surg. 1979;66:379–384. doi: 10.1002/bjs.1800660603. [DOI] [PubMed] [Google Scholar]
- 12.Stapleton GN, Hickman R, Terblanche J. Blood supply of the right and left hepatic ducts. Brit J Surg. 1998;85:202–207. doi: 10.1046/j.1365-2168.1998.00511.x. [DOI] [PubMed] [Google Scholar]
- 13.Rappaport AM, Kawamura T, Knoblauch M, Cowan JS, Ohira S, Kalnins A, et al. Effects of arterial or portal ischaemia on survival and metabolism of partially and totally depancreatized dogs. Z Exp Chir. 1975;8:326–342. [PubMed] [Google Scholar]
- 14.Stapleton GN, Hickman R, Terblanche J. Blood supply of the right and left hepatic ducts. Br J Surg. 1998;85:202–207. doi: 10.1046/j.1365-2168.1998.00511.x. [DOI] [PubMed] [Google Scholar]
- 15.Redman HC, Reuter SR. Arterial collaterals in the liver hilus. Radiology. 1970;94:575–579. doi: 10.1148/94.3.575. [DOI] [PubMed] [Google Scholar]
- 16.Bengmark S, Rosengren K. Angiographic study of the collateral circulation to the liver after ligation of the hepatic artery in man. Am J Surg. 1970;119:620–624. doi: 10.1016/0002-9610(70)90228-x. [DOI] [PubMed] [Google Scholar]
- 17.Mays ER, Wheeler CS. Demonstration of collateral arterial flow after interruption of hepatic arteries in man. N Engl J Med. 1974;290:993–996. doi: 10.1056/NEJM197405022901804. [DOI] [PubMed] [Google Scholar]
- 18.Yoshidome H, Miyazaki M, Shimizu H, Ito H, Nakagawa K, Ambiru S, et al. Obstructive jaundice impairs hepatic sinusoidal endothelial cell function and renders liver susceptible to hepatic ischaemia/reperfusion. J Hepatol. 2000;33:59–67. doi: 10.1016/s0168-8278(00)80160-9. [DOI] [PubMed] [Google Scholar]
- 19.Aronsen KF, Nylander G, Ohlsson EG. Liver blood flow studies during and after various periods of total biliary obstruction in the dog. Acta Chir Scand. 1969;135:55–59. [PubMed] [Google Scholar]
- 20.Ohlsson EG, Rutherford RB, Haalebos MM, Wagner HN, Jr, Zuidema GD. The effect of biliary obstruction on hepatosplanchnic blood flow in dogs. J Surg Res. 1970;10:201–208. doi: 10.1016/0022-4804(70)90032-6. [DOI] [PubMed] [Google Scholar]
- 21.Kanda H, Nimura Y, Yasui A, Uematsu T, Kamiya S, Machiki Y, et al. Hepatic blood flow after acute biliary obstruction and drainage in conscious dogs. Hepatogastroenterology. 1996;43:235–240. [PubMed] [Google Scholar]
- 22.Soares AF, Castro e Silva Junior O, Ceneviva R, Roselino JE, Zucoloto S. Biochemical and morphological changes in the liver after hepatic artery ligation in the presence or absence of extrahepatic cholestasis. Int J Exp Pathol. 1993;74:367–370. [PMC free article] [PubMed] [Google Scholar]
- 23.Doppman JL, Girton M, Vermess M. The risk of hepatic artery embolization in the presence of obstructive jaundice. Radiology. 1982;143:37–43. doi: 10.1148/radiology.143.1.7063748. [DOI] [PubMed] [Google Scholar]
- 24.Strasberg SM. Error traps and vasculobiliary injury in laparoscopic and open cholecystectomy. J Hepatobiliary Pancreat Surg. 2008;15:284–292. doi: 10.1007/s00534-007-1267-9. [DOI] [PubMed] [Google Scholar]
- 25.Bacha EA, Stieber AC, Galloway JR, Hunter JG. Non-biliary complication of laparoscopic cholecystectomy. Lancet. 1994;344:896–897. [PubMed] [Google Scholar]
- 26.Balsara KP, Dubash C, Shah CR. Pseudoaneurysm of the hepatic artery along with common bile duct injury following laparoscopic cholecystectomy. A report of two cases. Surg Endosc. 1998;12:276–277. doi: 10.1007/s004649900651. [DOI] [PubMed] [Google Scholar]
- 27.Gupta N, Solomon H, Fairchild R, Kaminski DL. Management and outcome of patients with combined bile duct and hepatic artery injuries. Arch Surg. 1998;133:176–181. doi: 10.1001/archsurg.133.2.176. [DOI] [PubMed] [Google Scholar]
- 28.Nishio H, Kamiya J, Nagino M, Uesaka K, Kanai M, Sano T, et al. Right hepatic lobectomy for bile duct injury associated with major vascular occlusion after laparoscopic cholecystectomy. J Hepatobiliary Pancreat Surg. 1999;6:427–430. doi: 10.1007/s005340050145. [DOI] [PubMed] [Google Scholar]
- 29.Robertson AJ, Rela M, Karani J, Steger AC, Benjamin IS, Heaton ND. Laparoscopic cholecystectomy injury: an unusual indication for liver transplantation. Transpl Int. 1998;11:449–451. doi: 10.1007/s001470050173. [DOI] [PubMed] [Google Scholar]
- 30.Uenishi T, Hirohashi K, Tanaka H, Fujio N, Kubo S, Kinoshita H. Right hepatic lobectomy for recurrent cholangitis after bile duct and hepatic artery injury during laparoscopic cholecystectomy: report of a case. Hepatogastroenterology. 1999;46:2296–2298. [PubMed] [Google Scholar]
- 31.Bachellier P, Nakano H, Weber JC, Lemarque P, Oussoultzoglou E, Candou C, et al. Surgical repair after bile duct and vascular injuries during laparoscopic cholecystectomy: when and how? World J Surg. 2001;25:1335–1345. doi: 10.1007/s00268-001-0120-6. [DOI] [PubMed] [Google Scholar]
- 32.Wudel LJ, Jr, Wright JK, Pinson CW, Herline A, Debelak J, Seidel S, et al. Bile duct injury following laparoscopic cholecystectomy: a cause for continued concern. Am Surg. 2001;67:557–563. [PubMed] [Google Scholar]
- 33.Koffron A, Ferrario M, Parsons W, Nemcek A, Saker M, Abecassis M. Failed primary management of iatrogenic biliary injury: incidence and significance of concomitant hepatic arterial disruption. Surgery. 2001;130:722–728. doi: 10.1067/msy.2001.116682. [DOI] [PubMed] [Google Scholar]
- 34.Slater K, Strong RW, Wall DR, Lynch SV. Iatrogenic bile duct injury: the scourge of laparoscopic cholecystectomy. Aust N Z J Surg. 2002;72:83–88. doi: 10.1046/j.1445-2197.2002.02315.x. [DOI] [PubMed] [Google Scholar]
- 35.Silva MA, Coldham C, Mayer AD, Bramhall SR, Buckels JA, Mirza DF, et al. Specialist outreach service for on-table repair of iatrogenic bile duct injuries – a new kind of ‘travelling surgeon’. Ann R Coll Surg Engl. 2008;90:243–246. doi: 10.1308/003588408X261663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buell JF, Cronin DC, Funaki B, Koffron A, Yoshida A, Lo A, et al. Devastating and fatal complications associated with combined vascular and bile duct injuries during cholecystectomy. Arch Surg. 2002;137:703–708. doi: 10.1001/archsurg.137.6.703. [DOI] [PubMed] [Google Scholar]
- 37.Al-Sebayel MI. High bile duct injury following laparoscopic cholecystectomy. Saudi Med J. 2003;24:971–973. [PubMed] [Google Scholar]
- 38.Schmidt SC, Langrehr JM, Hintze RE, Neuhaus P. Longterm results and risk factors influencing outcome of major bile duct injuries following cholecystectomy. Br J Surg. 2005;92:76–82. doi: 10.1002/bjs.4775. [DOI] [PubMed] [Google Scholar]
- 39.Alves A, Farges O, Nicolet J, Watrin T, Sauvanet A, Belghiti J, et al. Incidence and consequence of an hepatic artery injury in patients with postcholecystectomy bile duct strictures. Ann Surg. 2003;238:93–96. doi: 10.1097/01.sla.0000074983.39297.c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Heinrich S, Seifert H, Krahenbuhl L, Fellbaum C, Lorenz M. Right hemihepatectomy for bile duct injury following laparoscopic cholecystectomy. Surg Endosc. 2003;17:1494–1495. doi: 10.1007/s00464-002-4278-2. [DOI] [PubMed] [Google Scholar]
- 41.Stewart L, Robinson TN, Lee CM, Liu K, Whang K, Way LW, et al. Right hepatic artery injury associated with laparoscopic bile duct injury: incidence, mechanism, and consequences. J Gastrointest Surg. 2004;8:523–530. doi: 10.1016/j.gassur.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 42.Frilling A, Li J, Weber F, Weber F, Fruhauf NR, Engel J, et al. Major bile duct injuries after laparoscopic cholecystectomy: a tertiary centre experience. J Gastrointest Surg. 2004;8:679–685. doi: 10.1016/j.gassur.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 43.Li J, Frilling A, Nadalin S, Paul A, Malago M, Broelsch CE. Management of concomitant hepatic artery injury in patients with iatrogenic major bile duct injury after laparoscopic cholecystectomy. Br J Surg. 2008;95:460–465. doi: 10.1002/bjs.6022. [DOI] [PubMed] [Google Scholar]
- 44.Mathisen O, Soreide O, Bergan A. Laparoscopic cholecystectomy: bile duct and vascular injuries: management and outcome. Scand J Gastroenterol. 2002;37:476–481. doi: 10.1080/003655202317316123. [DOI] [PubMed] [Google Scholar]
- 45.Felekouras E, Megas T, Michail OP, Megas T, Michail OP, Papaconstantinou I, et al. Emergency liver resection for combined biliary and vascular injury following laparoscopic cholecystectomy: case report and review of the literature. South Med J. 2007;100:317–320. doi: 10.1097/01.smj.0000242793.15923.1a. [DOI] [PubMed] [Google Scholar]
- 46.Salmen B, Akyurek N, Onal B, Cindoruk M. Combined proper hepatic artery and common hepatic duct injury in open cholecystectomy: case report and review of the literature. Adv Ther. 2007;24:639–647. doi: 10.1007/BF02848789. [DOI] [PubMed] [Google Scholar]
- 47.Yan JQ, Peng CH, Ding JZ, Yang WP, Zhou GW, Chen YJ, et al. Surgical management in biliary restricture after Roux-en-Y hepaticojejunostomy for bile duct injury. World J Gastroenterol. 2007;13:6598–6602. doi: 10.3748/wjg.v13.i48.6598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kayaalp C, Nessar G, Kaman S, Akoglu M. Right liver necrosis: complication of laparoscopic cholecystectomy. Hepatogastroenterology. 2001;48:1727–1729. [PubMed] [Google Scholar]
- 49.de Santibanes E, Palavecino M, Ardiles V, Pekolj J. Bile duct injuries: management of late complications. Surg Endosc. 2006;20:1648–1653. doi: 10.1007/s00464-006-0491-8. [DOI] [PubMed] [Google Scholar]
- 50.Winslow ER, Fialkowski EA, Linehan DC, Hawkins WG, Picus DD, Strasberg SM, et al. ‘Sideways’: results of repair of biliary injuries using a policy of side-to-side hepatico-jejunostomy. Ann Surg. 2009;249:426–434. doi: 10.1097/SLA.0b013e31819a6b2e. [DOI] [PubMed] [Google Scholar]
- 51.Halasz NA. Cholecystectomy and hepatic artery injuries. Arch Surg. 1991;126:137–138. doi: 10.1001/archsurg.1991.01410260021002. [DOI] [PubMed] [Google Scholar]
- 52.Anderson PT. Traumatic false aneurysm of the right hepatic artery: an unusual complication of cholecystectomy. Aust N Z J Surg. 1971;40:273–277. doi: 10.1111/j.1445-2197.1971.tb04072.x. [DOI] [PubMed] [Google Scholar]
- 53.Dean TE. False aneurysm of the right hepatic artery complicating cholecystectomy: a report of two cases. J R Coll Surg Edinb. 1986;31:95–97. [PubMed] [Google Scholar]
- 54.Iannelli A, Karimdjee BS, Fabiani P, Benizri EI, Converset S, Medjoubi SA, et al. [Haemobilia due to pseudoaneurysm of the right hepatic artery following laparoscopic cholecystectomy.] Gastroenterol Clin Biol. 2003;27:341–343. [PubMed] [Google Scholar]
- 55.Ibrarullah M, Singh B, Mehrotra P, Kaushik SP. Right hepatic artery pseudoaneurysm after laparoscopic cholecystectomy. Am J Gastroenterol. 1997;92:528–529. [PubMed] [Google Scholar]
- 56.Journe S, De Simone P, Laureys M, Le Moine O, Gelin M, Closset J. Right hepatic artery pseudoaneurysm and cystic duct leak after laparoscopic cholecystectomy. Surg Endosc. 2004;18:554–556. doi: 10.1007/s00464-003-4262-5. [DOI] [PubMed] [Google Scholar]
- 57.Yahchouchy-Chouillard E, Limot O, Ghiles E, Etienne JC, De Baer T, Picone O, et al. Embolization for right hepatic artery pseudoaneurysm following laparoscopic cholecystectomy. Aust N Z J Surg. 2003;73:82–84. doi: 10.1046/j.1445-2197.2003.02625.x. [DOI] [PubMed] [Google Scholar]
- 58.Keddie N, Metcalfe-Gibson C. Secondary haemorrhage from the right hepatic artery. Arch Surg. 1979;114:550. doi: 10.1001/archsurg.1979.01370280204039. [DOI] [PubMed] [Google Scholar]
- 59.Bulut T, Yamaner S, Bugra D, Akyuz A, Acarli K, Poyanli A. False aneurysm of the hepatic artery after laparoscopic cholecystectomy. Acta Chir Belg. 2002;102:459–463. doi: 10.1080/00015458.2002.11679352. [DOI] [PubMed] [Google Scholar]
- 60.Stewart BT, Abraham RJ, Thomson KR, Collier NA. Post-cholecystectomy haemobilia: enjoying a renaissance in the laparoscopic era? Aust N Z J Surg. 1995;65:185–188. doi: 10.1111/j.1445-2197.1995.tb00604.x. [DOI] [PubMed] [Google Scholar]
- 61.Chigot V, Lallier M, Alvarez F, Dubois J, Chigot V, Lallier M, et al. Hepatic artery pseudoaneurysm following laparoscopic cholecystectomy. Pediatr Radiol. 2003;33:24–26. doi: 10.1007/s00247-002-0772-x. [DOI] [PubMed] [Google Scholar]
- 62.Clements WD, Wilson RH, Crothers JG, McIlrath EM, Johnston GW. Pseudoaneurysm of the cystic artery following cholecystectomy. J R Coll Surg Edinb. 1993;38:348–349. [PubMed] [Google Scholar]
- 63.Genyk YS, Keller FS, Halpern NB. Hepatic artery pseudoaneurysm and haemobilia following laser laparoscopic cholecystectomy. A case report. Surg Endosc. 1994;8:201–204. doi: 10.1007/BF00591830. [DOI] [PubMed] [Google Scholar]
- 64.Kapoor R, Agarwal S, Calton R, Pawar G. Hepatic artery pseudoaneurysm and haemobilia following laparoscopic cholecystectomy. Indian J Gastroenterol. 1997;16:32–33. [PubMed] [Google Scholar]
- 65.Ribeiro A, Williams H, May G, Fulmer JT, Spivey JR. Haemobilia due to hepatic artery pseudoaneurysm 13 months after laparoscopic cholecystectomy. J Clin Gastroenterol. 1998;26:50–53. doi: 10.1097/00004836-199801000-00013. [Erratum in J Clin Gastroenterol 1998;26 (4):359] [DOI] [PubMed] [Google Scholar]
- 66.Rivitz SM, Waltman AC, Kelsey PB. Embolization of an hepatic artery pseudoaneurysm following laparoscopic cholecystectomy. Cardiovasc Intervent Radiol. 1996;19:43–46. doi: 10.1007/BF02560147. [DOI] [PubMed] [Google Scholar]
- 67.Schwarzmannova K, Poch T, Simsa J, Vidim T, Chudomel P, Volsansky P, et al. Pseudoaneurysm of the hepatic artery presenting with haemobilia – a complication of laparoscopic cholecystectomy. Rozhl Chir. 2008;87:360–363. [PubMed] [Google Scholar]
- 68.Siablis D, Tepetes K, Vasiou K, Karnabatidis D, Perifanos S, Tzorakoleftherakis E. Hepatic artery pseudoaneurysm following laparoscopic cholecystectomy: transcatheter intra-arterial embolization. Hepatogastroenterology. 1996;43:1343–1346. [PubMed] [Google Scholar]
- 69.Srivastava DN, Chakravarti AL, Gupta RK, Gujral RB. Gastrointestinal bleeding from a false aneurysm of the hepatic artery after cholecystectomy. Am J Gastroenterol. 1996;91:395–397. [PubMed] [Google Scholar]
- 70.Deziel DJ, Millikan KW, Economou SG, Doolas A, Ko ST, Airan MC. Complications of laparoscopic cholecystectomy: a national survey of 4292 hospitals and an analysis of 77 604 cases. Am J Surg. 1993;165:9–14. doi: 10.1016/s0002-9610(05)80397-6. [DOI] [PubMed] [Google Scholar]
- 71.Strasberg SM, Eagon CJ, Drebin JA. The ‘hidden cystic duct’ syndrome and the infundibular technique of laparoscopic cholecystectomy – the danger of the false infundibulum. J Am Coll Surg. 2000;191:661–667. doi: 10.1016/s1072-7515(00)00717-1. [DOI] [PubMed] [Google Scholar]
- 72.Hugh TB. New strategies to prevent laparoscopic bile duct injury – surgeons can learn from pilots. Surgery. 2002;132:826–835. doi: 10.1067/msy.2002.127681. [DOI] [PubMed] [Google Scholar]
- 73.Way LW, Stewart L, Gantert W, Liu K, Lee CM, Whang K, et al. Causes and prevention of laparoscopic bile duct injuries: analysis of 252 cases from a human factors and cognitive psychology perspective. Ann Surg. 2003;237:460–469. doi: 10.1097/01.SLA.0000060680.92690.E9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tzovaras G, Dervenis C. Vascular injuries in laparoscopic cholecystectomy: an underestimated problem. Dig Surg. 2006;23:370–374. doi: 10.1159/000097951. [DOI] [PubMed] [Google Scholar]
- 75.Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101–125. [PubMed] [Google Scholar]
- 76.Laurent A, Sauvanet A, Farges O, Watrin T, Rivkine E, Belghiti J, et al. Major hepatectomy for the treatment of complex bile duct injury. Ann Surg. 2008;248:77–83. doi: 10.1097/SLA.0b013e31817b65f2. [DOI] [PubMed] [Google Scholar]
- 77.Wachsberg RH, Cho KC, Raina S. Liver infarction following unrecognized right hepatic artery ligation at laparoscopic cholecystectomy. Abdom Imaging. 1994;19:53–54. doi: 10.1007/BF02165862. [DOI] [PubMed] [Google Scholar]
- 78.Thomson BN, Parks RW, Madhavan KK, Garden OJ. Liver resection and transplantation in the management of iatrogenic biliary injury. World J Surg. 2007;31:2363–2369. doi: 10.1007/s00268-007-9234-9. [DOI] [PubMed] [Google Scholar]
- 79.Ragozzino A, Lassandro F, De Ritis R, Imbriaco M. Value of MRI in three patients with major vascular injuries after laparoscopic cholecystectomy. Emerg Radiol. 2007;14:443–447. doi: 10.1007/s10140-007-0617-x. [DOI] [PubMed] [Google Scholar]
- 80.Usal H, Sayad P, Hayek N, Hallak A, Huie F, Ferzli G. Major vascular injuries during laparoscopic cholecystectomy. An institutional review of experience with 2589 procedures and literature review. Surg Endosc. 1998;12:960–962. doi: 10.1007/s004649900756. [DOI] [PubMed] [Google Scholar]


