Abstract
Cytoplasmic innate immune receptors are important therapeutic targets for diseases associated with overproduction of proinflammatory cytokines. One cytoplasmic receptor complex, the Nlrp3 inflammasome, responds to an extensive array of molecules associated with cellular stress. Under normal conditions, Nlrp3 is auto-repressed but in the presence of its ligands, it oligomerizes, recruits Asc, and triggers caspase 1 activation and the maturation of proinflammatory cytokines such as IL-1β and IL-18.
Since ischemic tissue injury provides a potential source for Nlrp3 ligands, our study compared and contrasted the effects of renal ischemia in wild-type mice and mice deficient in components of the Nlrp3 inflammasome (Nlrp3−/− and Asc−/− mice). To examine the role of the inflammasome in renal IRI we also tested its downstream targets caspase 1, IL-1 β and IL-18. Both Nlrp3 and Asc were highly expressed in renal tubular epithelium of humans and mice, and the absence of Nlrp3, but not Asc or the downstream inflammasome targets, dramatically protected from kidney ischemia reperfusion injury. We conclude that Nlrp3 contributes to renal ischemia reperfusion injury by a direct effect on renal tubular epithelium and that this effect is independent of inflammasome-induced proinflammatory cytokine production.
Introduction
Tremendous interest has evolved over the past decade in innate immune sensing receptors and their role in disease processes. Of the known innate immune receptors, the best described are the membrane-bound Toll-like receptors (TLRs); many recent discoveries have highlighted their importance in human diseases. Another family of intracellular innate sensors, called the nucleotide binding and oligomerization domain (NOD)-like receptors (NLRs), has attracted focused interest as potential therapeutic targets for diseases associated with the overproduction of proinflammatory cytokines. The NLRs are critical signaling molecules that contribute to formation of intracellular macromolecular complexes and regulate host immune responses to a variety of stimuli, including pathogens, molecules released from injured tissue, and a variety of non-specific molecules, including immune adjuvants (1).
The NLR family includes several different groups of intracellular molecules sharing a N-terminal pyrin domain (PYD), a central NACHT [Naip, CIITA, HET-E and telomerase-associated protein 1] domain and several leucine-rich repeat (LRRs) at the carboxy terminal end (2). One of the best-described members of the NLR family is Nlrp3 (also called cyropyrin, CIAS1, or Nalp3) (3). Nlrp3 is an essential component of the caspase 1 inflammasome, a multiprotein molecular scaffold necessary for caspase 1 activation (4). Upon ligand sensing, Nlrp3 recruits the adaptor protein Asc [apoptosis-associated speck-like protein containing a caspase recruitment domain (CARD) protein] through a PYD-PYD interaction. Asc then recruits inflammatory caspases (e.g., caspase 1) to the assembly complex through CARD-CARD interactions (5). The assembly complex brings into close proximity the inflammatory caspases, leading to their activation (6). Activation of caspase 1 is required for processing and release of active proinflammatory cytokines such as IL-1β and IL-18.
A large variety of structurally unrelated stimuli activate Nlrp3, such as microbial RNA and the imidazoquinoline compounds R837 and R848, MDP, poly (I-C), ATP, potassium efflux, asbestos, silica, aluminum hydroxide, amyloid β peptide, pore forming toxins, cellular components released into the extracellular milieu by distressed cells (including monosodium urate and calcium pyrophosphate dihydrate crystals found in gout and pseudogout) and cholesterol crystals (7–11). The fact that so many different stimuli trigger activation of Nlrp3, and subsequent inflammasome formation, suggests that Nlrp3 is a common hub for many different cellular triggers that lead to overproduction of proinflammatory cytokines.
Several human diseases have been linked to Nlpr3. For instance, mutations in the Nlrp3 gene cause familial cold autoinflammatory syndrome, Muckle-Wells syndrome, and neonatal-onset multisystem inflammatory disease, which are collectively known as cryopyrinopathies. (3, 12–14). More recently, inflammation associated with gout has been linked to Nlrp3 and overproduction of IL-1β (10). A central role for overproduction of IL-1β in the pathogenesis of Nlrp3-related diseases has been identified by the successful treatment of these diseases with IL-1 targeted therapies. The recombinant IL-1 receptor antagonist Anakinra has shown remarkable therapeutic efficacy for patients with cryopyrinopathies as well as gout (15–20).
Another of the disease processes linked to innate immune receptors is ischemic kidney injury. Ischemic kidney injury occurs commonly in hospitalized patients and is a complex pathophysiological process contributed to by both cell death and inflammation. While recent attention has highlighted the important role for TLRs in ischemic injury of the kidney (21, 22), as well as other organs (23–28), less is known about the role of the NLRs in ischemic organ injury (29).
Since Nlrp3 plays a central role in immune regulation associated with cellular injury, we investigated whether Nlrp3 plays a role in acute kidney injury. To mimic acute kidney injury, we used a well-characterized murine model of ischemia-reperfusion injury. We examined the dependence of kidney injury and cytokine/chemokine secretion on the Nlrp3 inflammasome using mice with targeted deletions in the inflammasome components, Nlrp3 and Asc. Since inflammasome formation activates caspase 1, we also asked whether targeted deletion of caspase 1 influenced acute kidney injury. The dependence of acute kidney injury on IL-1 was tested using an IL-1 receptor antagonist (ra) and also using IL-1 receptor knockout mice. The role of IL-18 was tested using IL-18 knockout mice. Our studies are the first to our knowledge to isolate an inflammasome-independent role of the Nlrp3 protein in renal epithelial cells, and to identify a new inflammasome independent function in vivo for Nlrp3.
Materials and Methods
Mice
Mice were housed in the vivariums at The Scripps Research Institute and University of California at San Diego and approved for use by the Laboratory Animal Care and Use Committee. Asc−/− and Nlrp3−/− mice were provided by Millenium pharmaceuticals. Animals were handled according to the standards of the Association for the Assessment and Accreditation of Laboratory Animal Care. C57BL/6, IL-1R−/−, and IL-18−/− mice were obtained from Jackson Laboratories (Bar Harbor, ME). Caspase 1−/− mice were obtained from R. Ulevitch (The Scripps Research Institute). All mice used in these experiments had been bred onto a C57BL/6 background by more than 10 generations.
Detection of Asc and Nlrp3 in WT mice and human cells
Asc and Nlrp3 mRNA were detected in renal tubular epithelium (RTE) or lymph node (LN) cells by semiquantitative PCR. To isolate and detect Asc and Nlrp3 from murine RTE, the same protocol was used as noted below (isolation of human RTE), except that collagenase D was used instead of collagenase A for murine RTE. Asc and Nlrp3 were also detected in pooled LN cells from dissected inguinal and axillary LNs. The first strand of cDNA of each sample was synthesized from 1 µg of total RNA using a QuantitectRT kit (Qiagen) according to the manufacturer's instructions. For reverse transcription (RT)-PCR, 1µg of total cellular RNA was reverse transcribed, and cDNA amplified. The expression of Asc and Nlrp3 mRNA in murine RTE was detected by semiquantitative PCR - with 5'-GCAGCGCATCGCCTTCTATC-3' as a forward primer and 5-GTCCATCACCAAGTAGGGATG-3' as a reverse primer for Asc mRNA and with 5'-GCAGCGCATCGCCTTCTATC-3' as a forward primer and 5'-CGGTGGTTGCTAGGAGATGG-3' as a reverse primer for Nlrp3 mRNA. The level of glyceraldehyde 3-phosphate dehydrogenase (GADPH) mRNA in each sample was also determined by PCR using 5'-GGTCTTACTCCTTGGAGGCCATGT-3' as a forward primer and 5'-GACCCCTTCATTGACCTCAACTACA-3' as a reverse primer. For detection of Asc in human RTE the forward primer was 5'-GCCGAGGAGCTCAAGAAGTT-3' and reverse was 5'-TCCTCCACCAGGTAGGACTG-3'. For detection of Nlrp3 in HEK293, Thp1 and human RTE cells the forward primer was 5'-AAAAGACTCATCCGTGTGCC-3' and reverse 5'-TTCCTGGCATATCACAGTGG-3'. The GADPH housekeeping gene was detected in the human cells by forward primer 5'-CACACCATCTTCCAGGAGC-3' and reverse - 5'CATGAGTCCTTCCACGATACC-3'. The PCR products were separated on a 1% agarose gel and digital photographs taken on a transilluminator.
Isolation of human RTE
Human kidney tissue was obtained from discarded nephrectomies for renal cell carcinoma (IRB:08-5054, Scripps Clinic and Green Hospital). Immediately after the nephrectomy, the renal pathologist removed a wedge section of normal tissue (distal from the site of tumor). After transport to the laboratory in sterile media, the renal capsule was removed and cortex dissected from the medulla. The cortex was then finely minced and placed in collagenase A (Sigma-Aldrich, St. Louis, MO) and incubated at 37°C for 30 min with frequent shaking. After incubation, the digested mixture was differentially sieved (200-50 um) and washed three times with fresh media. The sieved contents were then centrifuged, pelleted and layered over 30% Percoll (Sigma). After spinning the Percoll mixture at 21,500g for 30 minutes, four distinct bands were apparent as previously described (30, 31). The cells were collected from band 3 and washed three times with Hank's Buffered Salt Solution. The cells were then cultured in specialized tubular epithelial cell growth media [DMEM-Ham's-F-12 (Fischer Scientific, Pittsburgh, PA); Insulin (5mcg/ml), Transferrin (5mcg/ml), Selenium (50nmol/l) supplements, hydrocortisone (Sigma, (0.05 uM), epidermal growth factor (Sigma 10gn/ml) Tri-iodo thyronine (32 ng/ml) Penicillin/streptomycin 1ml, to promote growth of tubular epithelial cells but not other cell types. Within a few days a cobblestone morphology characteristic of cultured renal tubular epithelium was evident. Confirmation of renal tubular epithelium was made by positive staining for Lotus Tetragonolobus Lectin (32) (Vector Labs, Burlingame, CA).
Induction of in vivo ischemia/reperfusion injury
All experimental mice were matched for age (8–12 weeks) and only male mice were used. As previously published (21, 33), the following methods were used to induce non-lethal IRI. The mice were anesthetized with isofluorane and injected intraperitoneally with ketamine (100mg/kg)/xylazine (8mg/kg) in saline. Core body temperatures were maintained between 36°C and 37.5°C during surgery by continuous monitoring with a rectal thermometer and automatic heating blanket. Both kidneys were exposed with bilateral flank incisions and ischemia induced by clamping both renal arteries with nontraumatic microvessel clamps (S&T, Neuhausen, Switzerland) for 25 minutes. Renal veins remained unoccluded. Cessation of blood flow was documented by visual inspection. After 25 minutes of ischemia, the clamps were released and reflow verified by visual inspection of the kidneys. All mice received 200 microliters of saline dripped over the open flanks during surgery to keep the tissue moist and 30 microliters of saline per gram body weight injected subcutaneously after surgery to replenish for fluid loss.
Measurement of renal function
Measurement of renal function was conducted at indicated times following reperfusion. In all cases, the mice were anesthetized prior to sacrifice and blood was collected from the inferior vena cava into a syringe preloaded with 3.8% sodium citrate. Sham controls were also anesthetized prior to sacrifice and blood collected in an identical manner. Plasma was isolated by centrifugation at 4000×g for 10 min at 4°C. Renal function was assessed using the Sigma Diagnostics creatinine kit (Sigma-Aldrich, St. Louis, MO), running all samples in triplicates, and repeating measurements three times for each sample. Baseline (2 weeks before laparotomy) and terminal (at the time of sacrifice) plasma creatinines were measured in all animals.
Histological assessments
To assess renal histology, kidneys were harvested 24 hrs after kidney IR injury or sham surgery, fixed in a solution of zinc formalin and paraffin embedded. Sections (4 micron) were stained with Hematoxylin and Eosin or Periodic Acid Schiff stain. The tissue slides were blind labeled and reviewed by the renal pathologist who had no knowledge of the experimental groups. A histological scoring system, adapted from Kelly et al was used (34). The percentage of tubules in the outer medulla that showed epithelial cell necrosis was estimated and a numerical score assigned to represent degree of injury: 0 (no injury); 1 (0–10%); 2 (11–20%); 3 (21–40%); 4 (41–60%); 5 (61–75%); 6 (>75%) tubules injured. The scores represented the pathologist's impression of the severity of tubular injury (including loss of proximal tubule brush border, cell blebbing or vacuolization, and/or cell necrosis): the score ranges of 1–2 represented mild injury, 3–4 represented moderate injury and 5–6 represented severe injury. Infiltrating neutrophils were counted at a magnification of 400X. In the regions containing neutrophils, 10 fields were counted to derive the extent of neutrophil infiltration per field (0–1 represented little or no infiltration, 1–2 moderate infiltration, 3+ extensive infiltration).
Detection of cytokines
For cytokine/chemokine measurements, animals were sacrificed at indicated times after ischemic injury, a sample of blood was taken from the inferior vena cava and then kidneys harvested and snap-frozen in liquid nitrogen. The kidneys were homogenized in extraction buffer (10mM Na-phosphate, pH 7.5; 0.1Mm-amino caproic acid; 10 U/ml Heparin Na-salt; complete protease inhibitor tablet) for 30 seconds and incubated overnight at 4°C on a rotator. Supernatants were collected after centrifugation at 10,000g for 10 minutes at 4°C. Cytokine and chemokine levels were measured in tissue homogenates using commercial enzyme-linked immunosorbent assay (ELISA) kits (R&D Systems, Minneapolis, MN) according to manufacturer instructions. The detection limits in tissue were 16 pg/ml for IL-1β. Plasma concentrations of mouse IL-1β and IL-18 were measured using ELISA kits [limited to 16 pg/ml for IL-1 β and 26 pg/ml for IL-18]. To control for the ability to produce the cytokines, WT and Nlrp3−/− mice were injected intraperitoneally with lipopolysaccaride (LPS) from Salmonella minnesota R595 (Alexis Biochemicals, Enzo Life Sciences International, Inc, Plymouth Meeting, PA) at a concentration of 10mg/kg body weight. WT and Nlrp3−/− serum and kidneys were harvested at serial time points. Nonmanipulated controls were also sacrificed to compare baseline cytokine/chemokine levels.
Detection of active caspase 1 and mature IL-1β
To detect the Nlrp3 targets, caspase 1 and IL-1β, and to assess whether they were activated in WT and/or Nlrp3−/− mice after IRI, whole kidneys were harvested immediately following 25min bilateral renal artery clamping/24 hours reperfusion. The kidneys were then lysed in a buffer containing 60mM Tris, 10% Glycerol and 2% SDS and protease inhibitors. The lysis supernatants were then resolved by SDS-PAGE, transferred to nitrocellulose and immunoblotted with anti-caspase 1 antibody, anti-cleaved IL-1β antibody, or anti-hsp-90 loading control (all antibodies from Cell Signaling, Danvers, MA). The blots were then developed by the enhanced chemiluminescence (ECL) system (Amersham Corp, Louisville, CO).
Blockade of IL-1 and IL-18
The effect of IL-1 blockade on renal IRI was tested in two ways. The first employed the IL-1 receptor antagonist, (Anakinra, Kineret, Amgen, Thousand Oaks, CA). Anakinra (25mg/kg) was injected i.p. into WT mice at two intervals (upon induction of anesthesia, and at 6 hours post-operatively, following published dosing and interval recommendations (35, 36)). To assess the potential dose/interval–dependence, Anakinra was also given over a range doses from 1mg/kg to 150mg/kg and a range of administration times (from 6 hrs before surgery to 12 hrs after surgery). Higher/lower and/or more frequent Anakinra dosing did not show any different results from utilized regimen. The second method to test for the effect of IL-1 blockade was by inducing IRI in IL-1R−/− mice using methodology described above (induction of in vivo ischemia/reperfusion injury). IL-18−/− mice were used to test the effect of IL-18 deficiency in renal IRI.
Bone Marrow Transplantation
To evaluate the role of inflammation in kidney IR injury, Nlrp3−/− vs. WT bone marrow was transplanted into WT mice. Male WT mice were lethally irradiated with 2 doses of 5Gy, separated by 3 h, using a 137Cs Gammacell 40 Extractor irradiator (MDS Nordion, Ottawa, ON, Canada). The next day, bone marrow was collected from WT or Nlrp3−/− mice by flushing femurs and tibia with sterile 10K media [RPMI containing L-glutamine (2mM), fetal bovine serum (10%), penicillin (100U/ml), streptomycin (100ug/ml), 2-mercaptoethanol (0.05 mM), HEPES (10mM)]. The bone marrow cells were then washed with sterile PBS and 5 × 106 WT or Nlrp3−/− bone marrow cells in sterile PBS were injected into the tail vein of recipient irradiated mice. The mice were kept in microisolator cages for 6 weeks to complete engraftment with donor bone marrow and were given trimethoprim-sulfa enriched water until induction of IRI. Confirmation of Asc−/− or Nlrp3−/− engraftment after bone marrow transplantation was performed on bone marrow cells of chimeric WT mice engrafted with either Nlrp3−/− bone marrow or WT bone marrow. To detect the Nlrp3 mutation, the WT forward and reverse primers were 5'-GCTGTGCCCAGGTCCTAGC-3' and 5'-CAGCAGCAGCCCTTTCGAG-3' respectively and the KO allele forward and reverse primers were 5’-GCAGCGCATCGCCTTCTATC-3’ and 5’-CGGTGGTTGCTAGGAGATGG-3’ respectively. To detect the Asc mutation, the WT forward and reverse primers were 5’-GTGGACGGAGTGCTGGATG-3’ and 5’-GTCCATCACCAAGTAGGGATG-3’ respectively and the KO allele forward and reverse primers were 5’-GCAGCGCATCGCCTTCTATC-3’ and 5’-GTCCATCACCAAGTAGGGATG-3’ respectively.
Apoptosis
To evaluate for evidence of apoptosis in renal cortical tissue after renal IR injury, tissue cryosections (6 micron) were assayed with the TUNEL reaction, using the TdT-mediated dUTP nick-end labeling (TUNEL) assay as provided in the fluorescein FragEL™ DNA Fragmentation detection kit (Calbiochem, San Diego). Cryosections were fixed in 4% formaldehyde and permeabilized in proteinase K (in 10mM Tris, pH 8). The sections were then exposed to the TdT equilibration buffer and the free 3'- hydroxyl groups of DNA labeled with the fluorescein-conjugated deoxynucleotides. Nuclear staining was identified in cell nuclei with 4',6-diamidino-2-phenylindole (DAPI) and DNA breakage imaged by fluorescence microscopy. Eight random non-overlapping sections were viewed and counted under a grid at 200× magnification. All tissue sections were blind labeled and viewed without knowledge of experimental groups.
Results
Nlrp3 and Asc are expressed in murine and human kidneys
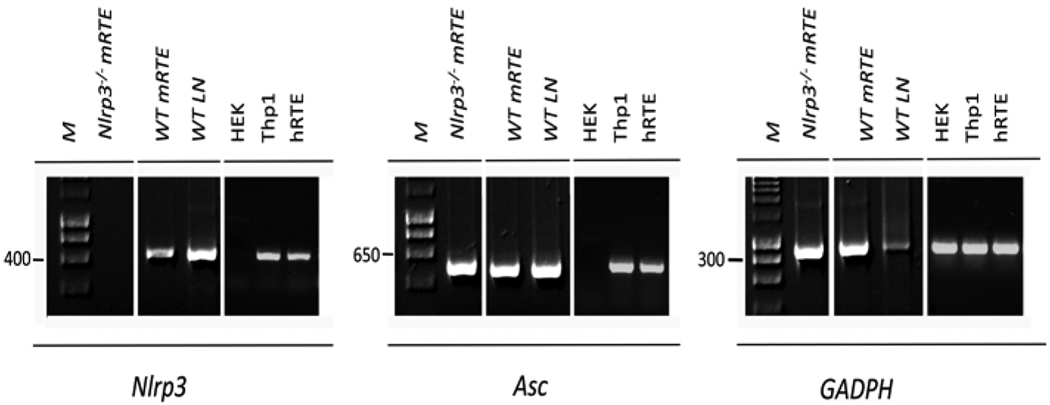
A pathognomonic finding of renal IRI is renal tubular epithelial injury (37, 38). To evaluate the role of Nlrp3 and Asc in kidney ischemia-reperfusion injury (IRI), we first asked whether the Nlrp3 and Asc genes were present in renal tubular epithelial cells of murine and human kidneys. As seen in Figure 1, using semiquantitative PCR, both Nlrp3 and Asc were well expressed in renal tubular epithelial cells in the two species. These genes were also expressed in murine lymphocytes and in the human monocytic cell line Thp1, but not in nontransfected HEK cells, as previously described (1, 5, 39, 40).
Figure 1. Nlrp3 and Asc in murine and human cells.
Figure 1 shows three panels depicting the Nlrp3, Asc or housekeeping GADPH genes. Each panel illustrates gene expression, detected by semiquantitative PCR in renal tubular epithelium of either Nlrp3−/− mice (Nlrp3−/− mRTE), wild type (WTmRTE) mice, lymph node cells from WT mice (WTLN), nontransfected HEK 293 cells (HEK), Thp1 cells (Thp1) or human renal tubular epithelial cells extracted from normal human kidneys (hRTE). The results are representative of 4 mice per group and 5 different human kidneys extracted for renal tubular cells with identical results.
Contribution of Nlrp3, Asc, and caspase 1 to kidney injury following ischemia and reperfusion
Since Nlrp3 and Asc were highly expressed in mouse and human renal tubular epithelial cells, the cells most susceptible to renal hypoxia, the participation of these inflammasome component proteins in responses to acute kidney injury were tested in a well-characterized model of murine kidney ischemia reperfusion injury (IRI). Using WT and mutant mice, bred for more than 10 generations to the same genetic background (C57BL/6), non-lethal renal IRI was induced in WT, Asc−/− and Nlrp3−/− mice using our previously well-characterized model (21). Upon ligand recognition, Nlrp3 and Asc form a multimolecular complex that is critical for triggering the activation of caspase 1 (41). Therefore, we tested whether a deficiency in caspase 1 influenced kidney IRI using caspase 1−/− mice.
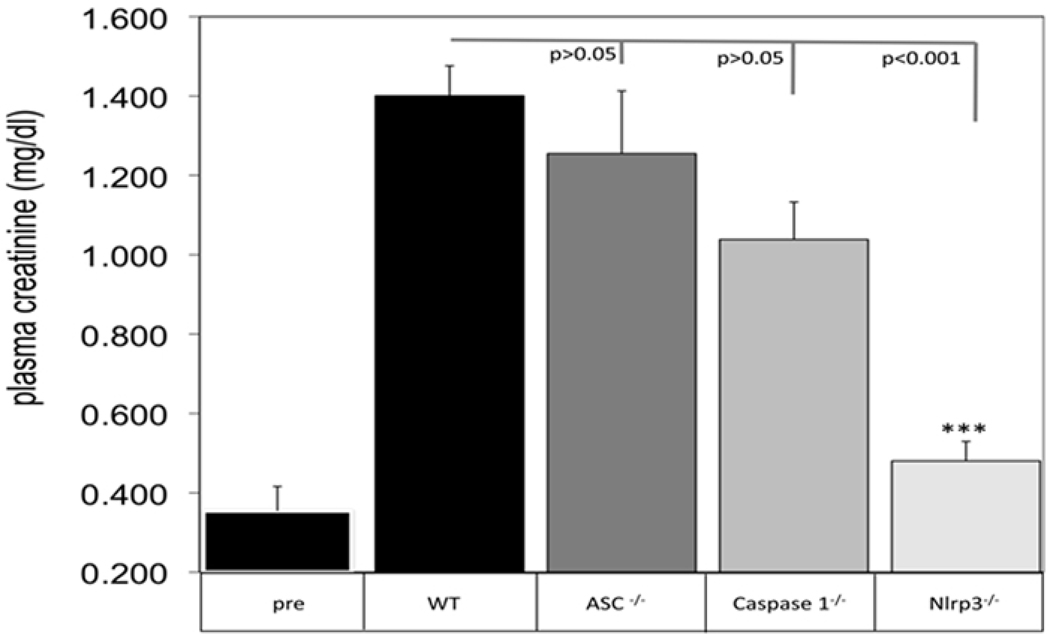
Figure 2 shows plasma creatinine levels two weeks before injury for WT mice and 24 hours after injury for each indicated group of mice. Pre injury and sham creatinines are listed in the figure legend for Asc−/−, caspase 1−/− and Nlrp3−/− mice; no differences were observed between any of the groups. As seen in Figure 2 there were no significant differences in post-injury creatinines between WT and Asc−/− mice (p<0.05) or between WT vs. caspase 1−/− mice (p<0.05). However, an extremely significant reduction in serum creatinine was noted in IR treated Nlrp3−/− mice (p<0.001); suggesting greater renal protection was afforded by a deficiency of Nlrp3 than by a deficiency in the protein Asc, which collaborates with Nlrp3 to form the inflammasome. Confirming that Nlrp3 can also signal independently of the inflammasome, there was no protection from renal IRI by deletion of caspase 1, the downstream signaling target of this inflammasome.
Figure 2. Kidney ischemia-reperfusion injury in WT, NLR and caspase-1 deficient mice.
WT, Asc−/−, caspase 1−/− or Nlrp3−/− mice were subjected to 25 min ischemia/24hr reperfusion and plasma obtained at 24 hrs to detect creatinine from injured WT, Asc−/−, caspase 1−/−, and Nlrp3−/− mice (n=6 mice per each group). Preinjury creatinines were obtained 2 weeks earlier on each of experimental mice; WT is shown in the figure (labeled, Pre); Asc−/− (0.42±0.01); caspase 1−/− (0.47±0.01); and Nlrp3−/− (0.48±0.04). Creatinines were also obtained from sham operated mice: WT (0.4±0.1); Asc−/− (0.3±0.1); Caspase 1−/− (0.4±0.2); and Nlrp3−/− (0.3±0.2). Error bars represent SD of creatinines and statistical significance was determined with a one-way ANOVA with Bonferroni’s multiple comparison test. The data represent one of five identical experiments with the same results.
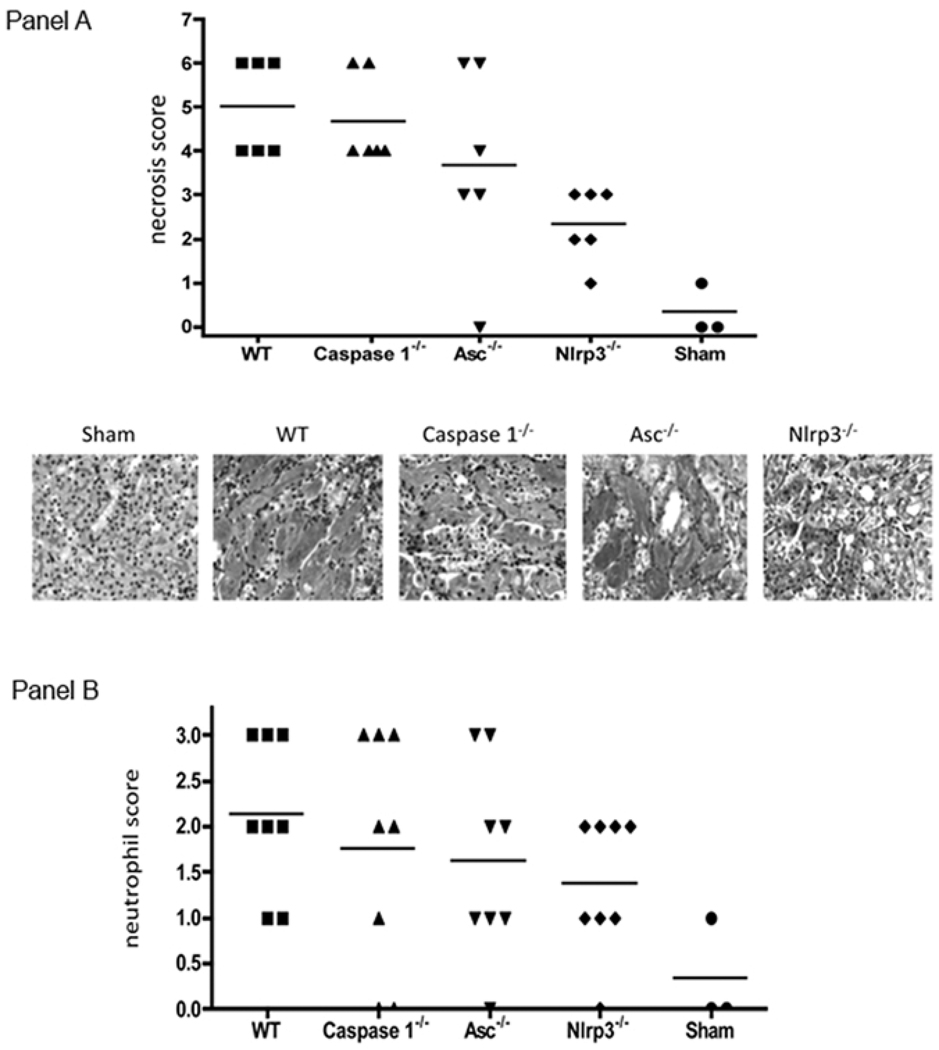
Acute tubular necrosis in each group of mice was evaluated by a pathologist blinded to the experimental groups (Figure 3, Panel A). Using a modified standard scoring system (21), necrosis was scored 24 hrs after the initial ischemic insult (Figure 3, Panel A). The means of each group are shown in the figure legend. As seen in Figure 3, top panel, there was no difference in necrosis between WT, caspase 1−/− (p>0.05) and Asc−/− mice (p>0.05), but a significant reduction in tubular necrosis was seen between WT mice and mice deficient in Nlrp3 (p<0.01). A representative photomicrograph is shown for each of the groups below Panel A. Neutrophil infiltration was also assessed in each group, in a blinded manner, by the pathologist (Figure 3, Panel B). There were no significant differences in neutrophil infiltration noted between any of the groups.
Figure 3. Histological renal injury after bilateral renal artery clamping.
Figure 3, Panel A shows blinded scoring of tubular necrosis from WT (n=6), caspase 1−/− (n=6), Asc−/− (n=6), Nlrp3−/− (n=6) and sham (n=3) operated mice 24 hrs after bilateral renal artery clamping (25 min ischemia/24hr reperfusion). The top panel shows the blinded necrosis score (see materials and methods for details) and the bottom panel shows a representative micrograph of each group of mice (PAS, 200X). Means of necrosis scores were as follows: WT (5.0±1.1); caspase 1−/− (4.7±1.0); Asc−/− (3.7±2.2); Nlrp3−/− (2.3±0.8). There were no statistical differences between WT vs. caspase 1−/− (p>0.50), or WT vs. Asc−/− (p>0.50); but significant differences in histological injury were observed between WT vs. Nlrp3−/− (p<0.01) mice. Panel B shows blinded scores of neutrophil infiltration on the same sections (see materials and methods). Means of neutrophil scores were: WT (2.1±0.8), caspase 1−/− (1.8±1.3), Asc−/− (1.6±1.1), Nlrp3−/− (1.4 ±0.7). No statistical differences in neutrophil infiltration were seen between the groups, WT vs. caspase 1−/− (p>0.05), vs. Asc−/− (p>0.05), or vs. Nlrp3−/− (p>0.05). Statistical significance was determined by a one-way ANOVA with Bonferroni’s multiple comparison test.
IL-18 and IL-1 β secretion in WT and Nlrp3−/− mice after kidney IRI
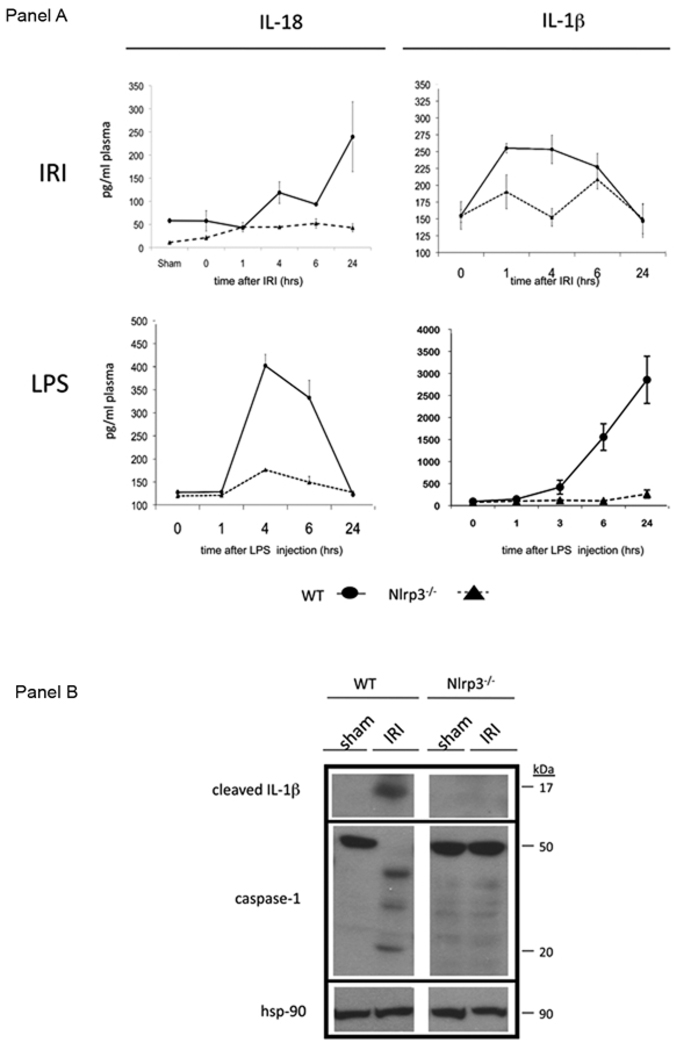
Protection from kidney injury following IRI was most prominent in mice lacking the innate sensor molecule Nlrp3. As such, post-injury IL-18 and IL-1β secretion was compared and contrasted between WT and Nlrp3−/− mice (Figure 4). Figure 4, Panel A shows there was significantly less IL-18 and IL-1β produced after kidney IRI in the Nlrp3−/− than WT mice. In Figure 4, Panel A, bottom panels, LPS treatment indicated that, as expected, mice deficient in Nlrp3 were unable to secrete the inflammasome-dependent cytokines IL-18 or IL-1β. Figure 4, Panel B shows that mature IL-1β and activated caspase 1 was detected in WT kidneys but not in Nlrp3−/− kidneys subjected to renal IRI. The fact that Nlrp3−/− mice were not able to activate caspase 1 or produce mature IL-1β following IRI confirms that Nlrp3 is necessary for inflammasome-mediated proinflammatory cytokine production in vivo. But, as seen below in Figure 5, the renal protection conferred by the deficiency in Nlrp3 is independent of its role in inflammasome-induced proinflammatory cytokine secretion.
Figure 4. Cytokine secretion after ischemia reperfusion or injection of LPS.
Panel A shows WT or Nlrp3−/− mice (n=6/gp) subjected to 25 min ischemia and indicated times of reperfusion. At the indicated time points plasma (for IL-18) or kidney homogenates (for IL-1 β) was assayed for the cytokines (top panels, IRI). Bottom panels show plasma cytokine secretion over time after LPS injection in WT (λ) or Nlrp3−/− (σ) mice (n=6/gp). The data are representative of 3 experiments with the same results. Error bars represent standard deviations. Panel B shows IL-1β and caspase 1 in WT vs. Nlrp3−/− kidneys from sham operated (sham) or IRI mice. The top panel shows mature IL-1β (mature IL-1β identified by the p17 fragment). The middle panel shows caspase 1 (active subunit p20) and the lower panel shows hsp-90 for a loading control. This represents one of 3 experiments with identical results.
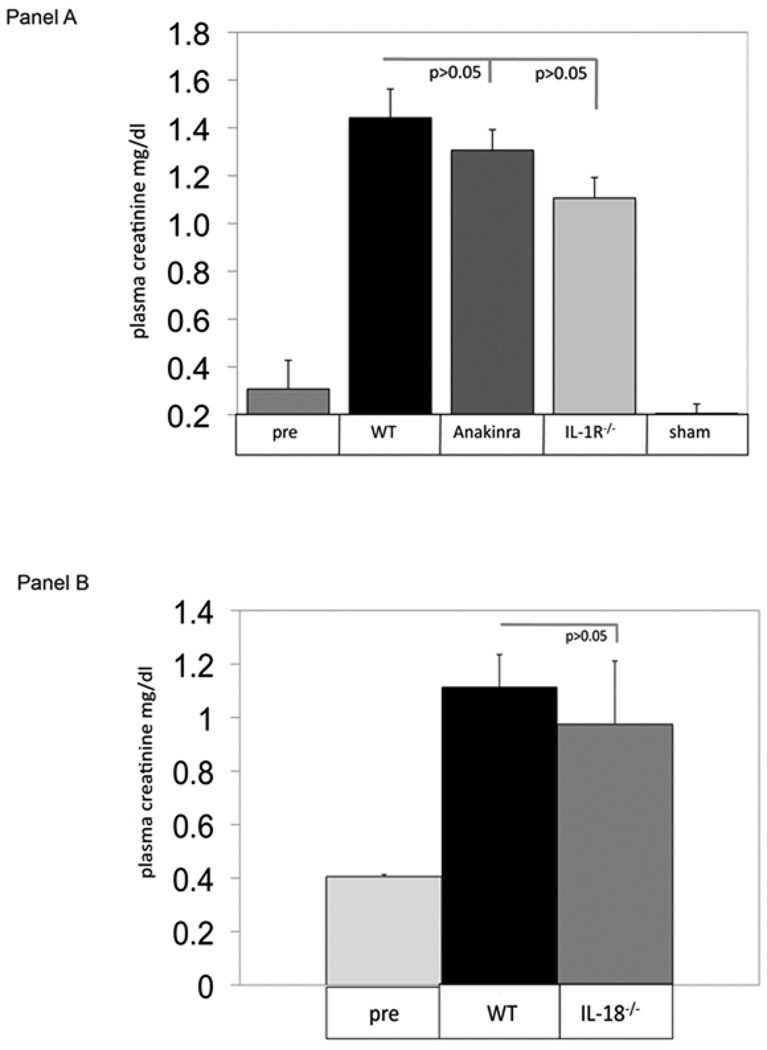
Figure 5. IL-1 and IL-18 blockade and kidney IRI.
Figure 5, Panel A shows WT (WT), WT mice treated with Anakinra (per materials and methods) (Anakinra), or IL-1R−/− (IL-1R−/−) mice that were treated with 25 min ischemia/24hr reperfusion followed by plasma creatinine determination at 24 hrs. Sham mice underwent laparotomy without bilateral renal artery clamping. These data represent 6 mice per group. There were no significant differences between WT vs. Anakinra (p>0.05), WT vs. IL-1R−/− (p>0.05) groups. Error bars represent SDs. Panel B shows blinded necrosis scores of the IR injured mice. The means of necrosis score were: WT (4.2±0.8), Anakinra (4.5±0.8), IL-1R−/− (4.0±0.6). There were no statistical differences in necrosis scores: Wt vs. Anakinra (p>0.05), vs. IL-1R−/− (p>0.05). The means of neutrophil infiltration were: WT (2.3±0.8), Anakinra (1.7±0.5), IL-1R−/− (2.0±0.6); and statistical differences – WT vs. Anakinra (p>0.05), vs. IL-1R−/− (p>0.05). Statistical significance was determined by a one-way ANOVA with Bonferroni’s multiple comparison test.
IL-18 and IL-1R blockade and kidney IRI
Since Nlrp3 deficient mice did not produce IL-18 or IL-1β, the experiments shown in Figure 5 were performed to determine whether protection afforded by the absence of Nlrp3 was mediated through these cytokines. In Panel A, WT mice were pre-treated with an interleukin-1 receptor antagonist (IL-1ra) prior to renal artery clamping. IL-1 targeted therapy is highly useful for treatment of several disorders associated with mutations in Nlrp3 (10, 15–20). Shown in Figure 5, Panel A there were no significant differences in creatinine levels after renal IRI in unmanipulated WT mice compared to WT mice treated with the IL-1Ra Anakinra (p=0.13). A wide range of Anakinra doses were compared and contrasted (see materials and methods) and there was no renal protection afforded by any of the tested doses of Anakinra (data not shown). In Panel B, a slight, but non-significant, decrease in renal injury in IL-1R−/− mice was noted compared to unmanipulated WT mice (p>0.05), but no differences were seen in histology score or neutrophil infiltrates (data not shown). In Panel C, there were no differences in creatinines of WT mice versus IL-18−/− mice (p>0.05) treated with bilateral renal artery clamping, consistent with prior reports of the ineffectiveness of IL-18 deficiency on renal IRI (42).
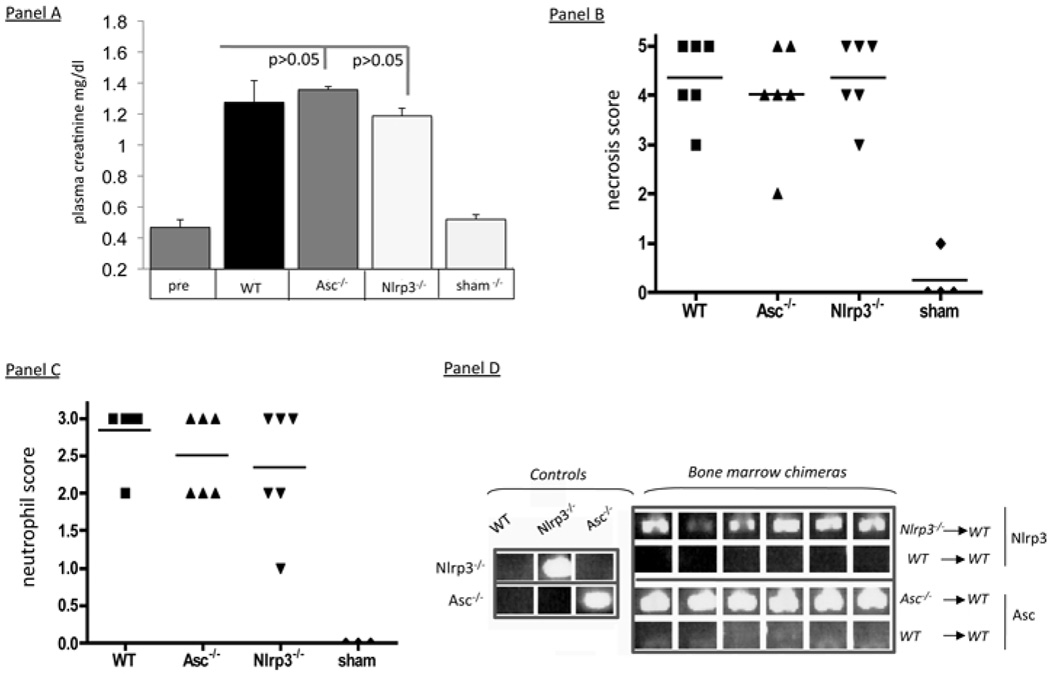
Inflammation in WT, Asc−/−, and Nlrp3−/− mice after renal IRI
To determine whether the absence of Nlrp3 protected kidneys from IRI by abrogating hematopoeitic cell mediated inflammation, WT mice were transplanted with bone marrow from either WT, Asc−/−, or Nlrp3−/− mice and renal IRI was induced (Figure 6). As shown in Figure 6, Panel A there were no differences in creatinine levels after IRI between the WT mice transplanted with WT vs. Asc−/− (p>0.05) or Nlrp3−/− (p>0.05) bone marrow. Confirming that there were no differences in tubular necrosis or inflammation between the two groups, blinded necrosis scores (Figure 6, Panel B) and neutrophil counts (Figure 6, Panel C) showed no differences between the WT and the chimeric mice (Figure 6, Panel B). Figure 6, Panel D confirms that the WT bone marrow was indeed replaced by the mutant marrow in the chimeric mice. Irradiated mutant mice were noted to have severe weight loss, and therefore reverse bone marrow transplants were not performed until further studies could determine the cause of the irradiation-induced weight loss in the mutant mice.
Figure 6. Bone marrow chimeric mice subjected to IRI.
Panel A shows WT mice that were irradiated and injected with either WT (n=6), Asc−/− (n=6) or Nlrp3−/− (n=6) bone marrow 6 weeks earlier. After engraftment the three groups of mice were treated with 25 min bilateral renal artery clamping followed by 24hrs reperfusion. Pre creatinine values were obtained 2 weeks before injury (pre). Sham creatinines were obtained from mice that underwent laparotomy without undergoing bilateral renal artery clamping (n=3). Error bars represent SDs. Panel B shows the necrosis score of the injured animals. The means of scores were: WT (4.3±0.8), Asc−/− (4.0±1.1), Nlrp3−/− (4.3±0.8) and statistical differences: Wt vs. Asc−/− (p>0.05), vs. Nlrp3−/− (p>0.05). Panel C shows the scores of neutrophil infiltration: WT (2.8±0.4), Asc−/− (2.5±0.5), Nlrp3−/− (2.3±0.8) and the statistical differences were: WT vs. Asc−/− (p>0.05), WT vs. Nlrp3−/− (p>0.05). Statistical significance was obtained by a one-way ANOVA with Bonferroni’s multiple comparison test. Panel D shows that chimeric bone marrow was engrafted in the indicated experimental groups. The control panels show the Nlrp3 knockout allele (indicating the Nlrp3 gene) was present in the Nlrp3−/− mice, but not in the WT or the Asc−/− mice (controls). The WT mice transplanted with the Nlrp3−/− bone marrow show that the Nlrp3 knockout allele was highly expressed (bone marrow chimeras, Nlrp3−/− ⇒ WT). Likewise the Asc knockout allele was expressed in Asc−/− controls, but not in the WT controls and also highly expressed in the mice transplanted with Asc−/− bone marrow (bone marrow chimeras, Asc−/− ⇒ WT).
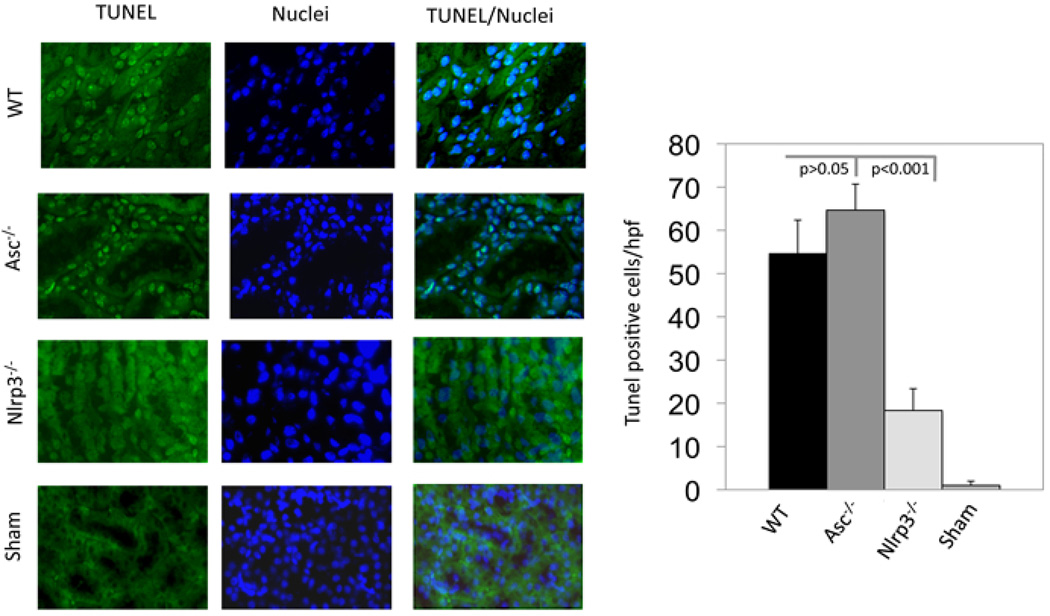
Apoptosis and renal IRI
An early histological finding of kidney ischemia/reperfusion injury is apoptosis of renal tubular cells; necrosis follows longer ischemic intervals (43). To determine whether Nlrp3 contributed to renal tubular apoptosis in our IRI model, kidney sections were examined for evidence of apoptosis in situ by the TUNEL assay. We have previously shown that maximal apoptosis occurs at 4 hours after injury in this model (29) and so focused on this interval, comparing results in WT vs. Asc−/− or Nlrp3−/− kidneys. As shown in Figure 7, there were significant differences in apoptosis between WT and Nlrp3−/− mice (p<0.001), whereas there were no differences between in IRI-treated WT and Asc−/− kidneys (p>0.05). These data suggest that in addition to the protection from necrosis, the absence of Nlrp3 also protected the kidney from renal tubular apoptosis in our model.
Figure 7. Apoptosis of renal tubular epithelial cells after renal IRI.
WT vs. Nlrp3−/−, Asc−/−, or sham mice were treated with 25 min of bilateral renal artery clamping followed by 4hr of reperfusion. The mice were sacrificed, their kidneys removed and placed into formalin for paraffin embedding and TUNEL assay. Panel A shows representative images of TUNEL and DAPI staining 4hrs after reperfusion. Panel B shows results of blinded counting of TUNEL-positive cells, 4hr after reperfusion, in nine random, non-overlapping, sections (n=3 mice per group). Data are expressed as means ± SD. Statistical significance was determined by a one-way ANOVA with Bonferroni’s multiple comparison test.
Discussion
Renal ischemia reperfusion injury (IRI) is a common clinical problem complicated by substantial morbidity and mortality; thus tremendous interest has evolved in putative triggers of the renal injury. The pathognomonic features of renal IRI include hypoxia-induced tubular epithelial damage followed by post-reperfusion inflammation. Multiple cell types and cell signals contribute to the syndrome, but tubular epithelial apoptosis and necrosis are predominant findings, particularly in the ischemic phases of injury.
Many recent studies have pointed to innate pattern recognition receptors (PRRs) as important triggers of tissue injury induced by ischemia (21, 29). Since apoptosis and inflammation are essential components of kidney IRI, our study focused on a recently identified intracellular innate immune receptor, Nlrp3, known to play a role in apoptosis and inflammatory responses to cellular injury.
Within the cytoplasm, Nlrp3 forms a complex with Asc and procaspase-1 called the Nlrp3 inflammasome. Recent studies have suggested that inflammasome components may signal death pathways independent from the inflammasome (44). We investigated the dependence of Nlrp3 on the intact inflammasome in vivo by testing the inflammasome components, Asc and Nlrp3, as well as the downstream targets caspase 1, IL-1β, and IL-18 in our well-characterized ischemic kidney injury model.
Examining murine and human renal tubular epithelial cells, we found that Nlrp3 and Asc were expressed in both species and, importantly, within tissue highly susceptible to renal IRI – renal tubular epithelium. These data are consistent with reports of innate immune receptor expression in many different cell types and in diverse species (45–52); suggesting these phylogenetically conserved proteins are involved in the response to endogenous stress.
To determine whether Nlrp3 plays an important role in tissue responses to renal ischemia, we compared and contrasted injury responses in WT and inflammasome deficient mice using a well-characterized model of renal IRI. Interestingly, despite the presence of both Nlrp3 and Asc in the cells most susceptible to IRI, only the Nlrp3 deficiency offered protection from tissue injury. Nlrp3 is well known to respond to a wide variety of structurally different ligands, positioning it as a key sensor for cellular injury (53). Our data showing that Nlrp3−/− mice, but not Asc−/− or capsase 1−/− mice were protected, suggest that Nlrp3 might be uncoupled from Asc, and from the inflammasome, in renal tubular epithelium. Consistent with our data Nlrp3−/− mice have been found to be protected from renal IRI in another model, but these investigators also found that Asc−/− mice were protected (54). The mice used in the study were backcrossed onto C57BL/6 mice for only 4 generations and therefore it is possible that the founder strain might account for the variance in findings. We have carefully confirmed that our mice are on a C57BL/6 background by absence of rejection of skin grafts from the mutant mice on the WT mice.
Since the absence of Nlrp3, but not Asc or caspase 1, protected from renal injury, our data strongly suggest an inflammasome-independent role for Nlrp3. The lack of protection from injury we observed in caspase 1 knockout mice is supported by studies of others using a similar model of renal ischemia (55). Activation of the Nlrp3 inflammasome is known to cause caspase 1 activation and cleavage of pro-IL-1β and pro-IL-18 into their active, mature forms (4, 6). Consistent with this, we found that a deficiency in Nlrp3 blocked IL-1β production, as well as IL-18 production. But, blockade of IL-1 and IL-18 (with either Anakinra or with IL-1R−/− or IL-18−/− mice) had no significant effect on renal injury responses, as previously reported (56). Others have reported that blockade of IL-18 provides either minimal (57) or no (42) protection from renal IRI. Therefore, Nlrp3 does not likely contribute to renal injury primarily through inflammasome mediated IL-1β or IL-18 production. Our data suggest that Nlrp3, rather than Asc, drives responses to tissue injury in this model, and suggests activation of Nlrp3 can induce inflammasome-independent responses in renal epithelial cells.
The pathogenesis of kidney IR is complex and to date many causative mechanisms have been proposed. These mechanisms generally involve direct induction of cell death pathways in tubular epithelia (58), glomerular injury and renal endothelial injury and expression of adhesion molecules (59), and leukocyte recruitment and activation (60). Nlrp3 has been detected in the cytosol of various immune cells, such as T cells, macrophages and dendritic cells (49), and we thought it possible that Nlrp3 might contribute to renal injury through inflammation initiated by hematopoeitic derived immune cells. However, WT mice engrafted with Nlrp3−/− bone marrow were not protected from injury. Although Nlrp3−/− mice do not produce IL-1b or IL-18 (neutrophil chemotaxins), neutrophils and still recruited to the injured tissue. Therefore, future studies will need to be conducted to completely exclude any role for Nlrp3 in activation of specific innate and adaptive inflammatory mediators to ischemic renal tissue in our model. A major role though for Nlrp3 mediated inflammation does not appear to be relevant from these data.
The most susceptible region of the kidney to ischemia appears to be the renal tubular epithelium located in the outer stripe of the medulla (37, 38). It is thought that ischemia-related reduction in microvascular blood flow to this region of the kidney coupled with a limited capacity of the proximal tubule cells to undergo anaerobic metabolism makes this region particularly susceptible. In fact, the most prominent histologic findings are the loss of the periodic acid-Schiff-positive brush border of the proximal tubular epithelium and scattered single cell necrosis or desquamation of proximal tubular cells with intact basement membranes (61). Interestingly, those proximal tubular epithelial cells that do not undergo apoptosis/necrosis (e.g. the surviving proximal tubular epithelial cells) divide and repopulate the tubular epithelium; thereby making kidney IRI a reversible disorder, unless all the epithelium is destroyed by the ischemia (62). Significantly less tubular necrosis was observed in Nlrp3−/− mice than in WT, Asc−/−, or caspase 1−/− mice following renal IRI, consistent with the known role for Nlrp3 as a mediator of necrosis in monocytes and macrophages (63). Interestingly, significantly less renal tubular apoptosis was also seen in the Nlrp3 deficient mice subjected to renal IRI, compared to renal IRI treated WT or Asc deficient mice. These data suggest that Nlrp3 might contribute to renal injury following ischemia/reperfusion by inducing apoptosis within a few hours of the ischemic insult. Future studies are ongoing in our laboratory to identify Nlrp3-dependent signaling events that contribute to renal tubular necrosis and apoptosis following IRI.
Our data point to a unique role for Nlrp3 in the kidney that is independent of the inflammasome. Future studies will need to focus on additional direct injury mechanisms that might be playing a role in Nlrp3-medated protection. Our study is the first to our knowledge to show that in renal epithelium Nlrp3 can signal injury responses independent of the inflammasome and independent of proinflammatory cytokines/chemokines.
Acknowledgements
We thank Susan Abel, RN for her assistance with the acquisition of human tissue for extraction of renal tubular epithelium and Terri Thinnes for her technical help with the caspase 1-deficient mice. We also thank John Bertin, Anthony Coyle, and Ethan Grant, formerly of Millenium pharmaceuticals, for providing the Nrlp3 and Asc knockout mice and Matthew McGeough and Carla Pena for mouse technical support.
Footnotes
This work was supported by a National Institutes of Health Grant (1R01DK60151) and a Scripps Translational Science Institute Pilot Grant (1UL1RR025774) award to DBM and a Renal Research Collaborative/Price Charities Grant awarded to A.J.K.
References
- 1.Geddes K, Magalhaes JG, Girardin SE. Unleashing the therapeutic potential of NOD-like receptors. Nat Rev Drug Discov. 2009;8:465–479. doi: 10.1038/nrd2783. [DOI] [PubMed] [Google Scholar]
- 2.Fritz JH, Ferrero RL, Philpott DJ, Girardin SE. Nod-like proteins in immunity, inflammation and disease. Nat Immunol. 2006;7:1250–1257. doi: 10.1038/ni1412. [DOI] [PubMed] [Google Scholar]
- 3.Hoffman HM, Mueller JL, Broide DH, Wanderer AA, Kolodner RD. Mutation of a new gene encoding a putative pyrin-like protein causes familial cold autoinflammatory syndrome and Muckle-Wells syndrome. Nat Genet. 2001;29:301–305. doi: 10.1038/ng756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agostini L, Martinon F, Burns K, McDermott MF, Hawkins PN, Tschopp J. NALP3 forms an IL-1beta-processing inflammasome with increased activity in Muckle-Wells autoinflammatory disorder. Immunity. 2004;20:319–325. doi: 10.1016/s1074-7613(04)00046-9. [DOI] [PubMed] [Google Scholar]
- 5.Stehlik C, Lee SH, Dorfleutner A, Stassinopoulos A, Sagara J, Reed JC. Apoptosis-associated speck-like protein containing a caspase recruitment domain is a regulator of procaspase-1 activation. J Immunol. 2003;171:6154–6163. doi: 10.4049/jimmunol.171.11.6154. [DOI] [PubMed] [Google Scholar]
- 6.Martinon F, Burns K, Tschopp J. The inflammasome: a molecular platform triggering activation of inflammatory caspases and processing of proIL-beta. Mol Cell. 2002;10:417–426. doi: 10.1016/s1097-2765(02)00599-3. [DOI] [PubMed] [Google Scholar]
- 7.Kanneganti TD, Body-Malapel M, Amer A, Park JH, Whitfield J, Franchi L, Taraporewala ZF, Miller D, Patton JT, Inohara N, Nunez G. Critical role for Cryopyrin/Nalp3 in activation of caspase-1 in response to viral infection and double-stranded RNA. J Biol Chem. 2006;281:36560–36568. doi: 10.1074/jbc.M607594200. [DOI] [PubMed] [Google Scholar]
- 8.Kanneganti TD, Ozoren N, Body-Malapel M, Amer A, Park JH, Franchi L, Whitfield J, Barchet W, Colonna M, Vandenabeele P, Bertin J, Coyle A, Grant EP, Akira S, Nunez G. Bacterial RNA and small antiviral compounds activate caspase-1 through cryopyrin/Nalp3. Nature. 2006;440:233–236. doi: 10.1038/nature04517. [DOI] [PubMed] [Google Scholar]
- 9.Petrilli V, Dostert C, Muruve DA, Tschopp J. The inflammasome: a danger sensing complex triggering innate immunity. Curr Opin Immunol. 2007;19:615–622. doi: 10.1016/j.coi.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 10.Martinon F, Petrilli V, Mayor A, Tardivel A, Tschopp J. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature. 2006;440:237–241. doi: 10.1038/nature04516. [DOI] [PubMed] [Google Scholar]
- 11.Chu J, Thomas LM, Watkins SC, Franchi L, Nunez G, Salter RD. Cholesterol-dependent cytolysins induce rapid release of mature IL-1beta from murine macrophages in a NLRP3 inflammasome and cathepsin B-dependent manner. J Leukoc Biol. 2009;86:1227–1238. doi: 10.1189/jlb.0309164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feldmann J, Prieur AM, Quartier P, Berquin P, Certain S, Cortis E, Teillac-Hamel D, Fischer A, de Saint Basile G. Chronic infantile neurological cutaneous and articular syndrome is caused by mutations in CIAS1, a gene highly expressed in polymorphonuclear cells and chondrocytes. Am J Hum Genet. 2002;71:198–203. doi: 10.1086/341357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aksentijevich I, Nowak M, Mallah M, Chae JJ, Watford WT, Hofmann SR, Stein L, Russo R, Goldsmith D, Dent P, Rosenberg HF, Austin F, Remmers EF, Balow JE, Jr, Rosenzweig S, Komarow H, Shoham NG, Wood G, Jones J, Mangra N, Carrero H, Adams BS, Moore TL, Schikler K, Hoffman H, Lovell DJ, Lipnick R, Barron K, O'Shea JJ, Kastner DL, Goldbach-Mansky R. De novo CIAS1 mutations, cytokine activation, and evidence for genetic heterogeneity in patients with neonatal-onset multisystem inflammatory disease (NOMID): a new member of the expanding family of pyrin-associated autoinflammatory diseases. Arthritis Rheum. 2002;46:3340–3348. doi: 10.1002/art.10688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hull KM, Shoham N, Chae JJ, Aksentijevich I, Kastner DL. The expanding spectrum of systemic autoinflammatory disorders and their rheumatic manifestations. Curr Opin Rheumatol. 2003;15:61–69. doi: 10.1097/00002281-200301000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Hawkins PN, Lachmann HJ, McDermott MF. Interleukin-1-receptor antagonist in the Muckle-Wells syndrome. N Engl J Med. 2003;348:2583–2584. doi: 10.1056/NEJM200306193482523. [DOI] [PubMed] [Google Scholar]
- 16.Yamazaki T, Masumoto J, Agematsu K, Sawai N, Kobayashi S, Shigemura T, Yasui K, Koike K. Anakinra improves sensory deafness in a Japanese patient with Muckle-Wells syndrome, possibly by inhibiting the cryopyrin inflammasome. Arthritis Rheum. 2008;58:864–868. doi: 10.1002/art.23261. [DOI] [PubMed] [Google Scholar]
- 17.Mirault T, Launay D, Cuisset L, Hachulla E, Lambert M, Queyrel V, Quemeneur T, Morell-Dubois S, Hatron PY. Recovery from deafness in a patient with Muckle-Wells syndrome treated with anakinra. Arthritis Rheum. 2006;54:1697–1700. doi: 10.1002/art.21807. [DOI] [PubMed] [Google Scholar]
- 18.Rynne M, Maclean C, Bybee A, McDermott MF, Emery P. Hearing improvement in a patient with variant Muckle-Wells syndrome in response to interleukin 1 receptor antagonism. Ann Rheum Dis. 2006;65:533–534. doi: 10.1136/ard.2005.038091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoffman HM, Rosengren S, Boyle DL, Cho JY, Nayar J, Mueller JL, Anderson JP, Wanderer AA, Firestein GS. Prevention of cold-associated acute inflammation in familial cold autoinflammatory syndrome by interleukin-1 receptor antagonist. Lancet. 2004;364:1779–1785. doi: 10.1016/S0140-6736(04)17401-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Granel B, Serratrice J, Disdier P, Weiller PJ. Dramatic improvement with anakinra in a case of chronic infantile neurological cutaneous and articular (CINCA) syndrome. Rheumatology (Oxford) 2005;44:689–690. doi: 10.1093/rheumatology/keh547. [DOI] [PubMed] [Google Scholar]
- 21.Shigeoka AA, Holscher TD, King AJ, Hall FW, Kiosses WB, Tobias PS, Mackman N, McKay DB. TLR2 is constitutively expressed within the kidney and participates in ischemic renal injury through both MyD88-dependent and -independent pathways. J Immunol. 2007;178:6252–6258. doi: 10.4049/jimmunol.178.10.6252. [DOI] [PubMed] [Google Scholar]
- 22.Shirali AC, Goldstein DR. Tracking the toll of kidney disease. J Am Soc Nephrol. 2008;19:1444–1450. doi: 10.1681/ASN.2008010123. [DOI] [PubMed] [Google Scholar]
- 23.Frantz S, Kelly RA, Bourcier T. Role of TLR-2 in the activation of nuclear factor kappaB by oxidative stress in cardiac myocytes. J Biol Chem. 2001;276:5197–5203. doi: 10.1074/jbc.M009160200. [DOI] [PubMed] [Google Scholar]
- 24.Shen XD, Ke B, Zhai Y, Gao F, Busuttil RW, Cheng G, Kupiec-Weglinski JW. Toll-like receptor and heme oxygenase-1 signaling in hepatic ischemia/reperfusion injury. Am J Transplant. 2005;5:1793–1800. doi: 10.1111/j.1600-6143.2005.00932.x. [DOI] [PubMed] [Google Scholar]
- 25.Chen LW, Chang WJ, Chen PH, Liu WC, Hsu CM. TLR ligand decreases mesenteric ischemia and reperfusion injury-induced gut damage through TNF-alpha signaling. Shock. 2008;30:563–570. doi: 10.1097/SHK.0b013e31816a3458. [DOI] [PubMed] [Google Scholar]
- 26.Kilic U, Kilic E, Matter CM, Bassetti CL, Hermann DM. TLR-4 deficiency protects against focal cerebral ischemia and axotomy-induced neurodegeneration. Neurobiol Dis. 2008;31:33–40. doi: 10.1016/j.nbd.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 27.Victoni T, Coelho FR, Soares AL, de Freitas A, Secher T, Guabiraba R, Erard F, de Oliveira-Filho RM, Vargaftig BB, Lauvaux G, Kamal MA, Ryffel B, Moser R, Tavares-de-Lima W. Local and remote tissue injury upon intestinal ischemia and reperfusion depends on the TLR/MyD88 signaling pathway. Med Microbiol Immunol. 2010;199:35–42. doi: 10.1007/s00430-009-0134-5. [DOI] [PubMed] [Google Scholar]
- 28.Hua F, Ha T, Ma J, Gao X, Kelley J, Williams DL, Browder IW, Kao RL, Li C. Blocking the MyD88-dependent pathway protects the myocardium from ischemia/reperfusion injury in rat hearts. Biochem Biophys Res Commun. 2005;338:1118–1125. doi: 10.1016/j.bbrc.2005.10.068. [DOI] [PubMed] [Google Scholar]
- 29.Shigeoka AA, Kambo A, Mathison JC, King AJ, Hall WF, da Silva Correia J, Ulevitch RJ, McKay DB. Nod1 and nod2 are expressed in human and murine renal tubular epithelial cells and participate in renal ischemia reperfusion injury. J Immunol. 2010;184:2297–2304. doi: 10.4049/jimmunol.0903065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Detrisac CJ, Sens MA, Garvin AJ, Spicer SS, Sens DA. Tissue culture of human kidney epithelial cells of proximal tubule origin. Kidney Int. 1984;25:383–390. doi: 10.1038/ki.1984.28. [DOI] [PubMed] [Google Scholar]
- 31.McLaren J, Whiting P, Simpson J, Hawksworth G. Isolation and characterisation of human proximal tubular cells derived from kidney cortical segments. Hum Exp Toxicol. 1995;14:916–922. doi: 10.1177/096032719501401110. [DOI] [PubMed] [Google Scholar]
- 32.Nadasdy T, Laszik Z, Blick KE, Johnson DL, Burst-Singer K, Nast C, Cohen AH, Ormos J, Silva FG. Human acute tubular necrosis: a lectin and immunohistochemical study. Hum Pathol. 1995;26:230–239. doi: 10.1016/0046-8177(95)90042-x. [DOI] [PubMed] [Google Scholar]
- 33.Frank RD, Schabbauer G, Holscher T, Sato Y, Tencati M, Pawlinski R, Mackman N. The synthetic pentasaccharide fondaparinux reduces coagulation, inflammation and neutrophil accumulation in kidney ischemia-reperfusion injury. J Thromb Haemost. 2005;3:531–540. doi: 10.1111/j.1538-7836.2005.01188.x. [DOI] [PubMed] [Google Scholar]
- 34.Kelly KJ, Williams WW, Jr, Colvin RB, Meehan SM, Springer TA, Gutierrez-Ramos JC, Bonventre JV. Intercellular adhesion molecule-1-deficient mice are protected against ischemic renal injury. J Clin Invest. 1996;97:1056–1063. doi: 10.1172/JCI118498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abbate A, Salloum FN, Vecile E, Das A, Hoke NN, Straino S, Biondi-Zoccai GG, Houser JE, Qureshi IZ, Ownby ED, Gustini E, Biasucci LM, Severino A, Capogrossi MC, Vetrovec GW, Crea F, Baldi A, Kukreja RC, Dobrina A. Anakinra, a recombinant human interleukin-1 receptor antagonist, inhibits apoptosis in experimental acute myocardial infarction. Circulation. 2008;117:2670–2683. doi: 10.1161/CIRCULATIONAHA.107.740233. [DOI] [PubMed] [Google Scholar]
- 36.Salloum FN, Chau V, Varma A, Hoke NN, Toldo S, Biondi-Zoccai GG, Crea F, Vetrovec GW, Abbate A. Anakinra in experimental acute myocardial infarction--does dosage or duration of treatment matter? Cardiovasc Drugs Ther. 2009;23:129–135. doi: 10.1007/s10557-008-6154-3. [DOI] [PubMed] [Google Scholar]
- 37.Donohoe JF, Venkatachalam MA, Bernard DB, Levinsky NG. Tubular leakage and obstruction after renal ischemia: structural-functional correlations. Kidney Int. 1978;13:208–222. doi: 10.1038/ki.1978.31. [DOI] [PubMed] [Google Scholar]
- 38.Reimer KA, Ganote CE, Jennings RB. Alterations in renal cortex following ischemic injury. 3. Ultrastructure of proximal tubules after ischemia or autolysis. Lab Invest. 1972;26:347–363. [PubMed] [Google Scholar]
- 39.Aggarwal BB. Nuclear factor-kappaB: the enemy within. Cancer Cell. 2004;6:203–208. doi: 10.1016/j.ccr.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 40.Hasegawa M, Imamura R, Motani K, Nishiuchi T, Matsumoto N, Kinoshita T, Suda T. Mechanism and repertoire of ASC-mediated gene expression. J Immunol. 2009;182:7655–7662. doi: 10.4049/jimmunol.0800448. [DOI] [PubMed] [Google Scholar]
- 41.Yu HB, Finlay BB. The caspase-1 inflammasome: a pilot of innate immune responses. Cell Host Microbe. 2008;4:198–208. doi: 10.1016/j.chom.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 42.Daemen MA, van't Veer C, Wolfs TG, Buurman WA. Ischemia/reperfusion-induced IFN-gamma up-regulation: involvement of IL-12 and IL-18. J Immunol. 1999;162:5506–5510. [PubMed] [Google Scholar]
- 43.Perl M, Chung CS, Ayala A. Apoptosis. Crit Care Med. 2005;33:S526–S529. doi: 10.1097/01.ccm.0000185499.28006.4c. [DOI] [PubMed] [Google Scholar]
- 44.Mariathasan S, Newton K, Monack DM, Vucic D, French DM, Lee WP, Roose-Girma M, Erickson S, Dixit VM. Differential activation of the inflammasome by caspase-1 adaptors ASC and Ipaf. Nature. 2004;430:213–218. doi: 10.1038/nature02664. [DOI] [PubMed] [Google Scholar]
- 45.Bostanci N, Emingil G, Saygan B, Turkoglu O, Atilla G, Curtis MA, Belibasakis GN. Expression and regulation of the NALP3 inflammasome complex in periodontal diseases. Clin Exp Immunol. 2009;157:415–422. doi: 10.1111/j.1365-2249.2009.03972.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lev-Sagie A, Prus D, Linhares IM, Lavy Y, Ledger WJ, Witkin SS. Polymorphism in a gene coding for the inflammasome component NALP3 and recurrent vulvovaginal candidiasis in women with vulvar vestibulitis syndrome. Am J Obstet Gynecol. 2009;200(303):e301–e306. doi: 10.1016/j.ajog.2008.10.039. [DOI] [PubMed] [Google Scholar]
- 47.Lee P, Lee DJ, Chan C, Chen SW, Ch'en I, Jamora C. Dynamic expression of epidermal caspase 8 simulates a wound healing response. Nature. 2009;458:519–523. doi: 10.1038/nature07687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McCall SH, Sahraei M, Young AB, Worley CS, Duncan JA, Ting JP, Marriott I. Osteoblasts express NLRP3, a nucleotide-binding domain and leucine-rich repeat region containing receptor implicated in bacterially induced cell death. J Bone Miner Res. 2008;23:30–40. doi: 10.1359/JBMR.071002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kummer JA, Broekhuizen R, Everett H, Agostini L, Kuijk L, Martinon F, van Bruggen R, Tschopp J. Inflammasome components NALP 1 and 3 show distinct but separate expression profiles in human tissues suggesting a site-specific role in the inflammatory response. J Histochem Cytochem. 2007;55:443–452. doi: 10.1369/jhc.6A7101.2006. [DOI] [PubMed] [Google Scholar]
- 50.Gonzalez-Benitez JF, Juarez-Verdayes MA, Rodriguez-Martinez S, Cancino-Diaz ME, Garcia-Vazquez F, Cancino-Diaz JC. The NALP3/Cryopyrin-inflammasome complex is expressed in LPS-induced ocular inflammation. Mediators Inflamm. 2008;2008:614345. doi: 10.1155/2008/614345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rosengren S, Hoffman HM, Bugbee W, Boyle DL. Expression and regulation of cryopyrin and related proteins in rheumatoid arthritis synovium. Ann Rheum Dis. 2005;64:708–714. doi: 10.1136/ard.2004.025577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Anderson JP, Mueller JL, Rosengren S, Boyle DL, Schaner P, Cannon SB, Goodyear CS, Hoffman HM. Structural, expression, and evolutionary analysis of mouse CIAS1. Gene. 2004;338:25–34. doi: 10.1016/j.gene.2004.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tschopp J, Schroder K. NLRP3 inflammasome activation: the convergence of multiple signalling pathways on ROS production? Nat Rev Immunol. 2010;10:210–215. doi: 10.1038/nri2725. [DOI] [PubMed] [Google Scholar]
- 54.Iyer SS, Pulskens WP, Sadler JJ, Butter LM, Teske GJ, Ulland TK, Eisenbarth SC, Florquin S, Flavell RA, Leemans JC, Sutterwala FS. Necrotic cells trigger a sterile inflammatory response through the Nlrp3 inflammasome. Proc Natl Acad Sci U S A. 2009;106:20388–20393. doi: 10.1073/pnas.0908698106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Daemen MA, Denecker G, van't Veer C, Wolfs TG, Vandenabeele P, Buurman WA. Activated caspase-1 is not a central mediator of inflammation in the course of ischemia-reperfusion. Transplantation. 2001;71:778–784. doi: 10.1097/00007890-200103270-00016. [DOI] [PubMed] [Google Scholar]
- 56.Haq M, Norman J, Saba SR, Ramirez G, Rabb H. Role of IL-1 in renal ischemic reperfusion injury. J Am Soc Nephrol. 1998;9:614–619. doi: 10.1681/ASN.V94614. [DOI] [PubMed] [Google Scholar]
- 57.Wu H, Craft ML, Wang P, Wyburn KR, Chen G, Ma J, Hambly B, Chadban SJ. IL-18 contributes to renal damage after ischemia-reperfusion. J Am Soc Nephrol. 2008;19:2331–2341. doi: 10.1681/ASN.2008020170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kaushal GP, Basnakian AG, Shah SV. Apoptotic pathways in ischemic acute renal failure. Kidney Int. 2004;66:500–506. doi: 10.1111/j.1523-1755.2004.761_6.x. [DOI] [PubMed] [Google Scholar]
- 59.Molitoris BA, Sutton TA. Endothelial injury and dysfunction: role in the extension phase of acute renal failure. Kidney Int. 2004;66:496–499. doi: 10.1111/j.1523-1755.2004.761_5.x. [DOI] [PubMed] [Google Scholar]
- 60.Bonventre JV, Zuk A. Ischemic acute renal failure: an inflammatory disease? Kidney Int. 2004;66:480–485. doi: 10.1111/j.1523-1755.2004.761_2.x. [DOI] [PubMed] [Google Scholar]
- 61.Olsen S. Acute Tubular Necrosis and Toxic Renal Injury. Philadelphia: J.B. Lippincott Co.; 1989. [Google Scholar]
- 62.Bonventre JV. Dedifferentiation and proliferation of surviving epithelial cells in acute renal failure. J Am Soc Nephrol. 2003;14 Suppl 1:S55–S61. doi: 10.1097/01.asn.0000067652.51441.21. [DOI] [PubMed] [Google Scholar]
- 63.Ting JP, Willingham SB, Bergstralh DT. NLRs at the intersection of cell death and immunity. Nat Rev Immunol. 2008;8:372–379. doi: 10.1038/nri2296. [DOI] [PubMed] [Google Scholar]