Abstract
Objectives. We examined the influence of tobacco outlet density and residential proximity to tobacco outlets on continuous smoking abstinence 6 months after a quit attempt.
Methods. We used continuation ratio logit models to examine the relationships of tobacco outlet density and tobacco outlet proximity with biochemically verified continuous abstinence across weeks 1, 2, 4, and 26 after quitting among 414 adult smokers from Houston, Texas (33% non-Latino White, 34% non-Latino Black, and 33% Latino). Analyses controlled for age, race/ethnicity, partner status, education, gender, employment status, prequit smoking rate, and the number of years smoked.
Results. Residential proximity to tobacco outlets, but not tobacco outlet density, provided unique information in the prediction of long-term, continuous abstinence from smoking during a specific quit attempt. Participants residing less than 250 meters (P = .01) or less than 500 meters (P = .04) from the closest tobacco outlet were less likely to be abstinent than were those living 250 meters or farther or 500 meters or farther, respectively, from outlets.
Conclusions. Because residential proximity to tobacco outlets influences smoking cessation, zoning restrictions to limit tobacco sales in residential areas may complement existing efforts to reduce tobacco use.
Although the prevalence of smoking has decreased substantially over the past few decades, smoking remains the leading cause of preventable death and disability among adults in the United States.1 A key public health strategy to reduce the deleterious health effects of tobacco use is to decrease the prevalence of smoking by increasing smoking cessation rates.2 Previous public health and policy approaches to affect smoking prevalence have included restrictions on tobacco advertising, counter-advertising campaigns, bans on smoking in public places, increases in federal and state cigarette excise taxes, and increases in the availability of treatment programs. The effectiveness of these approaches in increasing smoking cessation rates has been supported by the literature.3–5 However, additional tobacco control strategies are needed to achieve national public health goals.2
One potential area of expansion for tobacco control policies is the regulation of tobacco retail outlets. Regulation strategies are designed to facilitate behavior change by altering structural aspects of the community context in which problematic behavior occurs.6 An analogous area in which regulation strategies have been applied is alcohol beverage retail outlets. In this case, regulation strategies have included the implementation of zoning restrictions to reduce the density of alcohol outlets and the proximity of alcohol outlets to residential areas. It was hypothesized that such regulations would affect problematic alcohol use at a community level by decreasing residents’ access to alcohol, reducing exposure to on-site product marketing, and changing social norms about alcohol use.7 Ultimately, research supported the success of these policies in reducing problematic alcohol use and alcohol-related injury, crimes, and violence.7–9 In contrast to the alcohol arena, little attention has been paid thus far to the potential utility of tobacco outlet regulation strategies as a supplement to existing tobacco control policies.
The Family Smoking Prevention and Tobacco Control Act, signed into law in June 2009, greatly expands the federal government's ability to enact new public health policies related to tobacco sales in the United States. If one considers the success of alcohol outlet regulation strategies on curbing alcohol use, an increased understanding of the effects of tobacco retail outlets on smoking behaviors may provide direction to emerging tobacco control policies. Thus far, studies largely support associations between tobacco retail outlets and smoking behaviors. For example, the density of tobacco retail outlets around schools has been linked to adolescent smoking initiation10 and purchasing habits.11 Similarly, the density of tobacco outlets around the home, as well as the proximity of tobacco outlets to the home, has been associated with the number of cigarettes consumed per day among adult smokers.12 In another study, greater smoker sensitivity to point-of-sale advertising at tobacco outlets predicted a reduced likelihood of having quit smoking 18 months later.13 However, no previous studies have directly examined the effects of tobacco outlet density and proximity on smoking cessation during a specific quit attempt.
The purpose of our study was to examine the effect of tobacco retail outlet density and proximity on smoking cessation among a racially/ethnically diverse group of smokers undergoing a specific quit attempt. We had two hypotheses. The first was that greater density of tobacco outlets around participants’ homes would be associated with lower odds of cessation. The second was that close residential proximity to a tobacco retail outlet would be associated with lower odds of cessation. All analyses controlled for participant demographics and tobacco-related variables. To our knowledge, this is the first study to examine the effects of tobacco retail outlets on a smoking quit attempt using a prospective, longitudinal design and biochemically verified smoking abstinence.
METHODS
We collected data as part of a longitudinal cohort study, conducted in the Houston, Texas, metropolitan area, designed to examine social disparities in smoking cessation.14 Participants were recruited via local print and radio advertisements and were required to be aged at least 21 years, to have smoked at least 5 cigarettes per day for the past year, to have a home address and functioning telephone number, to demonstrate proficiency in English at a 6th grade level or higher, and to be motivated to quit smoking in the next 30 days. Potential participants were excluded if the nicotine patch was contraindicated, if they reported use of tobacco products other than cigarettes, or if they reported participation in a smoking cessation program within the past 90 days. The original cohort sample consisted of 424 adult smokers who were enrolled from April 2005 through April 2007. All participants received standard smoking cessation treatment as part of the larger cohort study, which consisted of 6 weeks of nicotine patch therapy, 6 brief smoking cessation counseling sessions based on the Treating Tobacco Use and Dependence Clinical Practice Guideline,15 and self-help materials.
Measures
Participant demographics and tobacco-related variables.
We collected demographic and tobacco-related variables at baseline and included these as covariates in the analysis. These variables included age, race/ethnicity, partner status, education, gender, employment status, prequit smoking rate, and the number of years smoked. Although we collected income data, we did not use income as a covariate in the current study because 47 participants declined to provide this information.
Participant smoking abstinence outcomes.
Continuous abstinence from smoking through 26 weeks after quitting was the outcome of interest. We defined continuous abstinence as a self-report of no cigarettes smoked since the quit date (not even a puff) and an expired carbon monoxide level of 10 ppm or less. Smoking status was assessed at weeks 1, 2, 4, and 26 after quitting. Because the focus was on continuous abstinence, relapse at any postquit week resulted in classification as relapsed from that point forward. An intention-to-treat procedure was followed, whereby participants with missing abstinence outcomes were considered not abstinent (i.e., relapsed). The percentage of participants with missing smoking status at these timepoints ranged from 15% (week 26) to 18% (week 1).
Participant residential locations.
We geocoded participants’ residential addresses so that the density of tobacco outlets and the distance to closest tobacco outlet could be measured. We obtained participants’ (N = 424) residential addresses from baseline data. Using Environmental Systems Research Institute's ArcGIS software version 9.3.1 (ESRI, Redlands CA), we created an address locator to set parameters for batch geocoding of the participant addresses using address points from Centerpoint Energy's Houston metropolitan area address database. The majority of the participants’ residential addresses were successfully geocoded using the address locator, but about one quarter required manual geocoding. Only 10 participants from the original cohort could not be geocoded (6 participants gave a PO box as their address and 4 participants gave addresses that could not be found). Therefore, the current study included 414 adult smokers from the original cohort.
Tobacco outlet locations.
We obtained tobacco outlet addresses from the Texas Comptroller of Public Accounts, who keeps a record of all the facilities licensed to sell tobacco in Houston and surrounding areas. We used tobacco outlet records from 2006 (the midpoint of our enrollment) in the current study. We geocoded tobacco outlet locations (N = 7183) using the same procedures used for geocoding participant residential locations. The majority of tobacco outlets were geocoded with the address locator, but 7% required manual geocoding.
Tobacco outlet density.
The measurement of tobacco outlet density was a 3-step process. First, 3 road network buffers were created around each participant's home by using the New Service Area tool in the ArcGIS Network Analyst based on travel distances of 500 meters, 1 kilometer, and 3 kilometers, respectively. These distances are commonly used in accessibility studies.16–18 Defining a neighborhood based on distance traveled along the street network is preferable to defining a neighborhood with a circular buffer based on straight-line distance from the home, as distance traveled along the street network more closely approximates the actual travel effort required to access goods and services.16 Second, the geocoded tobacco outlets were overlaid with the road network neighborhood buffer areas, and a count of outlets within each buffer was obtained using the Spatial Join tool within ArcGIS, which joins the polygons (buffers) to points (outlets). Finally, the count of outlets was divided by the actual geographic coverage area of each buffer area to obtain the tobacco outlet density variables. This procedure resulted in 3 predictor variables that were unique to each participant: the density of tobacco outlets within 500 meters, 1 kilometer, and 3 kilometers of the participant's residence.
Tobacco outlet proximity.
To measure the proximity of each participant's home to the closest tobacco outlet we used the New Closest Facility tool in ArcGIS Network Analyst, which calculates the shortest travel distance in meters along the street network from the home to the closest outlet. We dichotomized tobacco outlet proximity based on the 25th and 50th percentile values, respectively, for analyses. This procedure resulted in 2 binary predictor variables: the closest tobacco outlet was less than 250 meters from the home (yes or no) and the closest tobacco outlet was less than 500 meters from the home (yes or no).
Data Analysis
Because continuous abstinence was the outcome of interest, we used continuation ratio (CR) logit models (PROC GENMOD19–21) to examine the influence of tobacco outlets on abstinence across weeks 1, 2, 4, and 26 after quitting. Continuation ratio logit models are appropriate when ordered categories (e.g., relapsed at week 1, abstinent at week 1 but relapsed at week 2, abstinent at week 2 but relapsed at week 4, abstinent at week 4 but relapsed at week 26, and abstinent through week 26) represent a progression through stages.19–21 The CR logit models operate by modeling the conditional probability of being abstinent at the current assessment point given that a participant has been abstinent through the most recent assessment point. Because all data in this study were compiled at the individual level, error related to the modifiable areal unit problem was minimized and no statistical adjustment for nesting structures was necessary. We performed all analyses with SAS version 9.1 (SAS Institute, Cary, NC).
First, we ran respective CR logit models to assess the relationship of tobacco outlet density within (1) 500 meters, (2) 1 kilometer, and (3) 3 kilometers of the participant's residence with continuous abstinence. Next, we ran respective CR logit models to assess the relationship of tobacco outlet proximity within: (1) 250 meters and (2) 500 meters of the participant's residence with continuous abstinence. We adjusted all analyses for time and age, race/ethnicity, partner status, education, gender, employment status, prequit smoking rate, and the number of years smoked to isolate the effect of tobacco outlet density and proximity on abstinence.
RESULTS
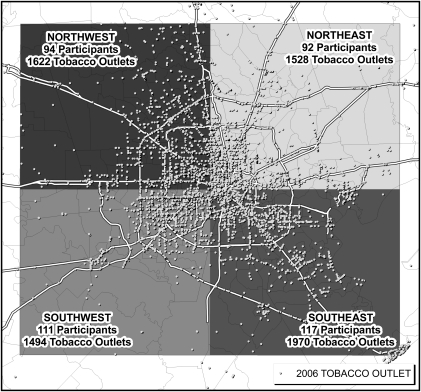
Participants were 414 racially/ethnically diverse adult smokers (approximately 33% were non-Latino White, 34% non-Latino Black, and 33% Latino. Forty-seven percent of participants were male. As a group, they were primarily low income (37% of responders reported less than $20 000 yearly household income). See Table 1 for participant characteristics. Participants were spread throughout the Houston metropolitan area, with at least 1 participant in each of 337 Census block group areas and 280 Census tracts. Figure 1 shows the mean center of participants’ residences (average longitude, average latitude), which was slightly east of downtown, and indicates the number of participants in each quadrant of a grid superimposed on this origin. Of the 7183 tobacco outlets geocoded, 6614 outlets were located within the 4-quadrant grid and were relevant to the generation of the outlet density and proximity variables. Figure 1 shows the number of tobacco outlets in each quadrant. On average, there were 1.5 (±2.1) tobacco outlets within the 500-meter buffers (range = 0–14), 6.6 (±6.6) outlets within the 1-kilometer buffers (range = 0–38), and 50.5 (±38.5) outlets within the 3-kilometer buffers (range = 0–244) around participants’ residences. The proximity of the closest cigarette outlet to participants’ homes ranged from 16 meters to 5315 meters, with a median distance of 492 meters and an average distance of 654.7 meters (±606.8). Participants living in areas with higher tobacco outlet densities were more likely to be unemployed and without a partner than were those living in areas with lower tobacco outlet densities (both P ≤ .05). Participants living in closer proximity to a tobacco outlet (< 250 m) were more likely to be without a partner and to have smoked for more years than were those living farther from the closest outlet (≥ 250 m; both P < .001).
TABLE 1.
Participant Characteristics (n = 414): Adult Smokers in Houston, TX, April 2005–April 2007
| Demographics and Tobacco-Related Variables | % or Mean (SD) |
| Age, y | 41.4 (11.2) |
| Race/ethnicity, % | |
| Non-Latino White | 32.9 |
| Non-Latino Black | 34.3 |
| Latino | 32.9 |
| Gender, % male | 47.0 |
| Married or living with partner, % | 34.8 |
| Annual household income <$ 20 000, % | 37.0 |
| Education, % | |
| < High school/GED | 13.8 |
| High school/GED | 28.3 |
| Some college | 30.4 |
| College degree | 26.6 |
| Not employed, % | 41.3 |
| Prequit smoking ratea | 21.2 (10.3) |
| No. of y smoked | 21.6 (11.1) |
Note. GED = general equivalency diploma.
The prequit smoking rate was defined as the number of cigarettes per day smoked before the participant began their latest quit attempt.
FIGURE 1.
Tobacco outlet locations in the Houston, TX, metropolitan area, 2006.
Note. Census tracts and major highways displayed.
Tobacco Outlet Density
The density of tobacco outlets around participants’ residences was not a significant predictor of smoking abstinence in any analysis (for 500 m: b = −0.03; SE = 0.02; χ2 [1] = 2.40; P = .12; for 1 km: b = −0.01; SE = 0.02; χ2 [1] = 0.28; P = .6; for 3 km: b = −0.03; SE = 0.04; χ2 [1] = 0.49; P = .48).
Tobacco Outlet Proximity
The proximity of residence to the closest tobacco outlet was a significant predictor of smoking abstinence in both analyses (for < 250 m vs ≥ 250 m: b = −0.62; SE = 0.25; χ2[1] = 6.46; odds ratio [OR] = 0.54; 95% confidence interval [CI] = 0.33, 0.87; P = .01; for < 500 m vs ≥ 500 m: b = −0.39; SE = 0.20; χ2[1] = 4.04; OR = 0.68; 95% CI = 0.46, 0.99; P = .04). The tobacco outlet proximity by time interaction was not significant in either analysis, indicating that the effect of outlet proximity on smoking abstinence did not vary across postquit weeks (for < 250 m vs ≥ 250 m: χ2[3] = 2.70; P = .44; for < 500 m vs ≥ 500 m: χ2[3] = 0.21; P = .98).
DISCUSSION
To our knowledge, this is the first longitudinal study assessing the influence of tobacco retail outlet density and proximity on smoking abstinence during a specific quit attempt. Results indicated that residential proximity to the closest tobacco retail outlet predicted smoking cessation among racially/ethnically diverse, adult daily smokers. In this sample, participants living within a short walking distance (< 500 m) of the closest tobacco retail outlet were less likely to maintain continuous abstinence from smoking 6 months following a quit attempt than were those who lived farther from the closest tobacco retail outlet. The strength of this relationship increased with decreased distance (i.e., < 250 m) to the closest outlet. These results add to a growing body of literature supporting the influence of tobacco outlets on smoking behavior10–12 and extend that literature to smoking cessation.
This study had a number of strengths, including the longitudinal design, biochemical verification of smoking status, and adjustment for a number of covariates known to affect smoking cessation (e.g., age, race/ethnicity, partner status, education, gender, employment status, prequit smoking rate, and the number of years smoked). However, other potential confounders might exist that were not accounted for in our analyses. For example, income was not among the covariates in the models because these data were not provided by 11% of participants. Posthoc analyses conducted among those providing income data, however, indicated that the inclusion of income as an additional covariate did not change the pattern of results. It is also possible that the relationship between tobacco outlet proximity and smoking cessation might be attenuated when one is adjusting for relevant neighborhood-level characteristics. For example, a previous study found that smokers living in more economically deprived areas were less likely to quit smoking over a 6-year period than were those residing in areas with greater economic resources.22 Posthoc analyses of our data indicated that further adjusting models for neighborhood (i.e., Census tract) unemployment, poverty, and low levels of education, respectively, did not alter our pattern of results.
Close residential proximity to tobacco outlets could reduce the likelihood of maintaining smoking abstinence during a quit attempt in several ways. For example, a large body of evidence supports that smoking cues can provoke subjective and autonomic responses among smokers, including increases in self-reported cravings to smoke.23 It may be that a tobacco outlet close to the home represents a cue for smoking that is difficult to avoid when one is walking or driving in the neighborhood, which might increase the risk of relapse. Previous research also supports that the ready availability of cigarettes is a risk factor for relapse.24 Thus, the close proximity of a tobacco retail outlet may increase the likelihood of relapse by offering easy access to cigarettes when an urge to smoke strikes. Another study found that greater smoker sensitivity to point-of-sale advertising at tobacco outlets predicted a reduced likelihood of having quit smoking 18 months later.13 Thus, it may be that the closer proximity of retail outlets results in greater exposure to point-of-sale tobacco advertising, which may derail a quit attempt. These ideas are speculative, however, and require additional research.
The passage of the Family Smoking Prevention and Tobacco Control Act represents an unprecedented legislative opportunity to affect smoking prevalence and smoking cessation rates in the United States. Results suggest that if tobacco outlets were less accessible to quitting smokers (i.e., located farther from their homes) the likelihood of maintaining abstinence during a quit attempt might increase. Therefore, exerting greater control over the locations of tobacco outlets through zoning regulations may reduce access to cigarettes, and ultimately decrease smoking prevalence.25 Similar regulation policies have been applied to alcohol beverage retail outlets and have been successful in reducing problematic alcohol use and alcohol-related injury, crimes, and violence.7–9 Zoning restrictions on tobacco licensing have been implemented around school zones in some areas10 to prevent adolescent smoking, and such restrictions might also be helpful in promoting cessation among established adult smokers undergoing a quit attempt.
In this study, the density of tobacco retail outlets around the home was not associated with smoking abstinence during a quit attempt. Previous studies have established an association between tobacco outlet density and smoking rate among adult smokers,12 smoking initiation among adolescents,10 and cigarette purchasing behavior among underage smokers.11 These, and other studies on tobacco outlet density,26–28 have engendered recommendations to limit the availability of tobacco retail sale licenses within prescribed areas or require a certain distance between retail outlets to better restrict the sale of tobacco.29 Results of this study, however, indicate that the presence of even a single tobacco outlet in close proximity to the home was enough to affect smoking abstinence during a quit attempt. This may be because only a single retail outlet is needed to purchase cigarettes, and the closer that cigarette outlet is to home, the lower the cost in effort (time and distance traveled) expended to obtain the product. It may also be that having to travel farther to obtain cigarettes may result in the natural dissipation of cravings, or may allow participants greater opportunity to employ other strategies to cope with the urge to smoke. These suppositions require more research. Although the density of tobacco outlets did not affect smoking cessation in this sample, results might be sample- or area-specific and should be replicated in future research. Moreover, the absence of significant effects in this study does not preclude the importance of tobacco outlet density on smoking initiation10 or other smoking behaviors.12
Limitations
Participants in this study were self-selected, treatment-seeking smokers who may differ from smokers who attempt to quit without treatment in important ways, and the influence of tobacco outlets on cessation among the latter group remains unknown. This study did not assess car ownership, the density or proximity of tobacco outlets around participants’ workplaces, their usual travel routes, or proportion of time spent in the neighborhood to determine the effect of these factors on smoking cessation. Future studies might explore these areas.
Another limitation includes the use of tobacco outlet data from a single point in time (i.e., 2006), despite a rolling enrollment period for participants that spanned 2005 through 2007. However, although opening or closing of tobacco outlets may have occurred before or after we obtained tobacco licensing data, it is unlikely that substantial changes would have taken place if one considers the absence of major external economic factors during this time span (e.g., a local or national economic crisis). Also, because analyses were conducted in 2009, tobacco outlet locations in 2006 could not be confirmed by direct observation. Instead, we relied on the accuracy of licensing data provided by the comptroller. Results may not generalize to other metropolitan areas in the United States, and studies like this should be replicated in other cities. More research is needed to assess relationships between tobacco retail outlets and smoking cessation in rural areas, which may differ from metropolitan areas in important ways. Finally, although analyses adjusted for several potential confounders, the presence of unknown and unmeasured confounders might have influenced these results.
Conclusions
Results indicated that close residential proximity to a tobacco outlet was associated with lower odds of maintaining smoking abstinence during a smoking quit attempt, even after controlling for participant age, race/ethnicity, partner status, education, gender, employment status, prequit smoking rate, and the number of years smoked. Because residential proximity to tobacco outlets affects smoking cessation, results suggest that zoning laws restricting the licensing of tobacco retail outlets around residential areas might be an important complement to existing policy efforts to reduce tobacco use.
Acknowledgments
This article was supported by grants from the National Institute of Drug Abuse (R01DA014818 to D. W. W.) and the Centers for Disease Control and Prevention (K01DP001120 to L. R. R.), and the National Cancer Institute through MD Anderson's Cancer Center Support Grant (CA016672).
We are grateful for the contributions of the following research team members, who were integral in the data collection, database design, and counseling provision on the parent project: Jamie Barnes, Shanna Barnett, Matiko Bivens, Barrett Blackmon, Vantrese Camiso, Aprill Dawson, Alex de la Torre, Mark Evans, Patricia Figueroa, Linda Kong, Tracy Kottwitz, Debbie Lew, Devin Olivares-Reed, Heather Pool, Krystal Robinson, Nikita Robinson, Paul Rowan, Maribel Sifuentes, and Rebecca Steinbach.
Note. Authors have no conflicts of interest pertaining to this research, but would like to report that P. M. Cinciripini has served on the scientific advisory board of Pfizer Pharmaceuticals and has conducted educational talks sponsored by Pfizer on smoking cessation for physicians within the past 3 years.
Human Participant Protection
The University of Texas MD Anderson Cancer Center institutional review board approved this study.
References
- 1.Ries LAG, Eisner MP, Kosary CL, et al. , SEER Cancer Statistics Review, 1975-2001. Bethesda, MD: National Cancer Institute; 2004 [Google Scholar]
- 2.Healthy People 2010. Washington, DC: US Dept of Health and Human Services; 2001 [Google Scholar]
- 3.Frieden TR, Mostashari F, Kerker BD, Miller N, Hajat A, Frankel M. Adult tobacco use levels after intensive tobacco control measures: New York City, 2002-2003 Am J Public Health; 2005;95(6):1016–1023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Longo DR, Johnson JC, Kruse RL, Brownson RC, Hewett JE. A prospective investigation of the impact of smoking bans on tobacco cessation and relapse. Tob Control. 2001;10(3):267–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Netemeyer RG, Andrews CJ, Burton S. Effects of anti-smoking advertising-based beliefs on adult smokers’ consideration of quitting. Am J Public Health. 2005;95(6):1062–1066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holder HD. Community prevention of alcohol problems. Addict Behav. 2000;25(6):843–859 [DOI] [PubMed] [Google Scholar]
- 7.Campbell CA, Hahn RA, Elder R, et al. The effectiveness of limiting alcohol outlet density as a means of reducing excessive alcohol consumption and alcohol-related harms. Am J Prev Med. 2009;37(6):556–569 [DOI] [PubMed] [Google Scholar]
- 8.Reynolds RI, Holder HD, Gruenewald PJ. Community prevention and alcohol retail access. Addiction. 1997;92(Suppl 2):S261–S272 [PubMed] [Google Scholar]
- 9.Holder HD, Gruenewald PJ, Ponicki WR, et al. Effect of community-based interventions on high-risk drinking and alcohol-related injuries. JAMA. 2000;284(18):2341–2347 [DOI] [PubMed] [Google Scholar]
- 10.McCarthy WJ, Mistry R, Lu Y, Patel M, Zheng H, Dietsch B. Density of tobacco retailers near schools: effects on tobacco use among students. Am J Public Health. 2009;99(11):2006–2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leatherdale ST, Strath JM. Tobacco retailer density surrounding schools and cigarette access behaviors among underage smoking students. Ann Behav Med. 2007;33(1):105–111 [DOI] [PubMed] [Google Scholar]
- 12.Chuang YC, Cubbin C, Ahn D, Winkleby MA. Effects of neighbourhood socioeconomic status and convenience store concentration on individual level smoking. J Epidemiol Community Health. 2005;59(7):568–573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Germain D, McCarthy M, Wakefield M. Smoker sensitivity to retail outlet displays and quitting: a cohort study. Addiction. 2010;105(1):159–163 [DOI] [PubMed] [Google Scholar]
- 14.Businelle MS, Kendzor DE, Reitzel LR, et al. Mechanisms linking socioeconomic status to smoking cessation: a structural equation modeling approach. Health Psychol. 2010;29(3):262–273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fiore M, Bailey WC, Cohen SJ, et al. Treating Tobacco Use and Dependence. Clinical Practice Guidelines. Rockville, MD: US Dept of Health and Human Services, Public Health Service; 2000 [Google Scholar]
- 16.Frank LD, Schmid TL, Sallis JF, Chapman J, Saelens BE. Linking objectively measured physical activity with objectively measured urban form: findings from SMARTRAQ. Am J Prev Med. 2005;28(2 Suppl 2):117–125 [DOI] [PubMed] [Google Scholar]
- 17.Tucker P, Irwin JD, Gilliland J, He M, Larsen K, Hess P. Environmental influences on physical activity levels in youth. Health Place. 2009;15(1):357–363 [DOI] [PubMed] [Google Scholar]
- 18.Berke EM, Gottlieb LM, Moudon AV, Larson EB. Protective association between neighborhood walkability and depression in older men. J Am Geriatr Soc. 2007;55(4):526–533 [DOI] [PubMed] [Google Scholar]
- 19.Agresti A. Categorical Data Analysis. 2nd ed. Hoboken, NJ: John Wiley & Sons Inc; 2002 [Google Scholar]
- 20.Bender R, Benner A. Calculating Ordinal Regression Models in SAS and S-Plus. Biometrical J. 2000;42:677–699 [Google Scholar]
- 21.McGowan MJ. Ordinal outcomes with the continuation ratio model. In: Proceedings of the Northeast SAS Users Group Conference. 2000. Available at: http://www.nesug.org/Proceedings/nesug00/ps/ps7015.pdf. Accessed October 29, 2010
- 22.Giskes K, van Lenthe FJ, Turrell G, Brug J, Mackenbach JP. Smokers living in deprived areas are less likely to quit: a longitudinal follow-up. Tob Control. 2006;15(6):485–488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carter BL, Tiffany ST. Meta-analysis of cue-reactivity in addiction research. Addiction. 1999;94(3):327–340 [PubMed] [Google Scholar]
- 24.Fiore M, Jaen C, Baker T. Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guidelines. Rockville, MD: US Dept of Health and Human Services, Public Health Service; 2008 [Google Scholar]
- 25.Bonnie RJ, Stratton K, Wallace RB. Ending the Tobacco Problem: A Blueprint for the Nation. Washington, DC: National Academy Press; 2007 [Google Scholar]
- 26.Novak SP, Reardon SF, Raudenbush SW, Buka SL. Retail tobacco outlet density and youth cigarette smoking: a propensity-modeling approach. Am J Public Health. 2006;96(4):670–676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peterson NA, Lowe JB, Reid RJ. Tobacco outlet density, cigarette smoking prevalence, and demographics at the county level of analysis. Subst Use Misuse. 2005;40(11):1627–1635 [DOI] [PubMed] [Google Scholar]
- 28.Schneider JE, Reid RJ, Peterson NA, Lowe JB, Hughey J. Tobacco outlet density and demographics at the tract level of analysis in Iowa: implications for environmentally based prevention initiatives. Prev Sci. 2005;6(4):319–325 [DOI] [PubMed] [Google Scholar]
- 29.Cohen JE, Anglin L. Outlet density: a new frontier for tobacco control. Addiction. 2009;104(1):2–3 [DOI] [PubMed] [Google Scholar]