Abstract
Objective
Coping with the physical and mental side effects of diagnosis and treatment for advanced prostate cancer (APC) is a challenge for both survivors and their spousal caregivers. There is a gap in our current understanding of the dyadic adjustment process on marital satisfaction in this population. The current study sought to: 1) document levels of physical and mental health, and marital satisfaction and 2) evaluate the relationship between physical and mental health with marital satisfaction in this understudied population.
Methods
APC survivors who had undergone hormonal therapy within the past year and their spousal caregiver participated in the study (N=29 dyads). Physical and mental health was assessed using the MOS SF-36 Health Survey and marital satisfaction was evaluated using the Dyadic Adjustment Scale.
Results
The Actor-Partner Interdependence Model revealed strong relations between physical and mental health with marital satisfaction for both survivor and caregiver (actor effects). Furthermore, caregiver physical and mental health was related with the survivor's marital satisfaction (partner effect).
Conclusions
Levels of mental health and marital satisfaction were comparable to community-based or prostate cancer samples, while physical health was higher. Marital satisfaction between APC survivors and their spousal caregivers may be influenced by both physical and mental health functioning. In particular, APC survivor functioning may affect both his marital satisfaction as well as his spousal caregiver's. This has implications for psychosocial interventions for APC dyads. Further evaluation of the complex nature of survivor/caregiver dyadic adjustment in dealing with APC is necessary.
Keywords: Cancer, Oncology, Physical and mental health, Marital satisfaction, prostate cancer patient-caregiver dyad
Introduction
Quality of Life (QoL) Among Advanced Prostate Cancer (APC) Survivors and Their Spouses
Prostate cancer (PC) is the most common non-skin cancer for men in the United States with over 2.2 million current survivors and an estimated 192,000 new diagnoses in 2009 [1]. Although improved screening practices have increased the proportion of men diagnosed with localized disease, approximately 15% of PC survivors still experience the spread of the cancer outside of the prostate gland, indicative of APC [1]. Those diagnosed with APC typically receive androgen deprivation therapy (ADT) which is associated with physical side effects of treatment such as fatigue, weight gain, nausea, hot flashes, pain, constipation, and urinary and sexual dysfunction [2]. Mental health is also compromised as APC survivors who received ADT report greater levels of psychological distress up to 12 months post-treatment when compared to those who did not [3]. The physical and psychological challenges of an advanced cancer diagnosis, ADT related side effects and survival rates of only approximately 30% are difficult to manage, and make APC survivors distinct population among those affected by PC.
PC not only affects the survivors but also their spouses, who are typically the primary caregivers [4]. The physical health of cancer caregivers has been reported as poorer than age-matched controls [5]. Additionally, the caregivers' levels of psychological distress can be equal to, or greater than, that of the survivors. Spousal caregivers of APC survivors showed clinical levels of anxiety and depression that were two times higher than the population norm and slightly higher than that of APC survivors [6].
Marital Satisfaction Among Couples Dealing with Advanced Prostate Cancer
The challenges brought about by PC appear not only to affect the individual's QoL but also strain the quality of the relationship between married survivors and their spousal caregivers [8,7]. Decrements in marital satisfaction may be a greater concern for PC survivor-caregiver dyads as female cancer caregivers appear to be at greater risk for decreases in marital satisfaction than male caregivers [8]. Research suggests that being in a satisfying marital relationship may be an important correlate of positive adjustment [9] and has been related with longer median survival times in PC survivors [10].
Current Study
There has been limited work examining the dyadic effects of physical and mental health on marital satisfaction within APC populations. Furthermore, much of the existing literature has assessed the QoL of the survivor and caregiver independently of one another without capturing the interplay between the partners in the dyad. The extent to which mental and physical health of APC survivors who have undergone ADT and their spousal caregiver relates to the marital relationship of each individual in the dyad, however, remains unknown. This is a salient gap in PC survivorship research, which has long been considered a ‘couple's disease.’ The current study addressed these gaps in the literature by (a) documenting levels of mental and physical health, and marital satisfaction within the understudied populations of APC survivors who have experienced ADT and their spousal caregivers, and (b) examining the extent to which each individual's physical and mental health relates to marital satisfaction in a dyadic context.
Methods
Participants and Procedures
APC survivors were recruited through a larger project that evaluated the efficacy of a psychosocial intervention on QoL and health functioning in men with APC [11]. They were recruited from urology clinics and a state-wide cancer registry. Men were required to be at least 50 years of age, have Stage III/IV PC, and have received ADT (or experienced physical side effects associated with ADT) within the prior 12 months. Once recruited, participants were asked if they had a spouse willing to participate in the present study. Any participant (APC survivor or spouse) reporting psychosis, suicidal ideation or substance use/dependence, was excluded as this would interfere with their ability to participate in the study. The survivors and spouses who agreed to participate signed independent informed consent forms, both approved by a university IRB. APC survivors were administered a comprehensive psychosocial assessment battery in an interview format. Spouses completed a psychosocial assessment packet at home, and returned the completed packet by mail.
A total of 65 APC survivors were approached for participation, and 31 participants and spouses ultimately agreed to be in the study. Primary reasons for exclusion for the 34 non-participants were: lack of a spouse (N=16), not wanting to involve the spouse (N=2) and inability to contact spouse (N=7). Two spouses did not complete their assessment packet and researchers were unable to contact the spouse after repeated attempts over a 6-month period, resulting in a final sample of 29 survivor-caregiver dyads.
Measures
Physical & Mental Health
Participant's physical and mental health were assessed over the previous 4-week period using a 10-item physical health subscale and a 5-item mental health subscales of the MOS SF-36 Health Survey [12], respectively. The physical health subscale assesses the individual's self-reported ability to perform certain activities, such as walking a mile or being able to climb several flights of stairs. The mental health subscale assesses the amount of time that they report feeling nervous, down in the dumps, peaceful, blue/sad and happy. Higher scores indicate better physical or mental health. In the current study, both subscales had acceptable internal consistency for both APC survivors and their spousal caregivers (αs>.65).
Marital Satisfaction
The extent to which each individual was satisfied with their marital relationship was measured using a 10-item dyadic satisfaction subscale from the Dyadic Adjustment Scale (DAS) [13]. The dyadic satisfaction subscale assessed thoughts and behaviors related to quarrelling and displaying affection within the dyad. In the current study, the subscale had acceptable internal consistency for both APC survivors and their spousal caregivers (αs>.65).
Demographics & Medical Variables
A broad range of demographic and medical information was collected as potential covariates of marital satisfaction: self-reported age, ethnicity, years of education, household income and number of medical co-morbidities [14]. Time since diagnosis and time since treatment completion were obtained only from the survivor.
Analytic Strategies
Preliminary analyses showed that none of the demographic or medical variables studied were significantly associated with the marital satisfaction. However, because age has been shown to be directly related to marital satisfaction (e.g., [15]) as well as mental and physical health, we included it as a covariate in subsequent analyses.
Mean differences between the survivor's and spousal caregiver's physical health, mental health and relationship satisfaction were evaluated using paired samples t-tests. Furthermore, the extent to which the survivor and his spousal caregiver were similar on physical health, mental health and relationship satisfaction was examined using Pearson zero-order correlation coefficients. The differences in mental and physical health between the current sample and the US population were evaluated with independent samples t-tests. These analyses were conducted using PASW (SPSS) Statistics 17.0.
The primary research questions for the current study were evaluated guided by the Actor Partner Interdependence Model (APIM) [16] using structural equation modeling (Amos 7.0). In the APIM, the effect of an individual's own characteristics (e.g., physical health) on their own outcomes (i.e., marital satisfaction) is considered an actor effect, while the effect of an individual's own characteristics on their partner's outcomes is considered a partner effect. Two indices were used to evaluate model fit: a confirmatory fit index (CFI) value above .95 and a root mean square error of approximation (RMSEA) value less than .05 were considered to be indicative of good model fit.
Results
Comparison of Levels of Study Variables
Table 1 presents demographic information for the current study. The participants were diverse, primarily older, well-educated and affluent. Our survivors reported higher physical health scores (77.4 versus 62.3) and comparable mental health scores of our sample (77.2 versus 78.9) when compared to APC norms [17]. Marital satisfaction scores of both the survivors and their spouses were similar to that of a community-based sample [13] and a mixed sample of PC survivors (primarily localized disease) [18]. As shown in Table 1, the levels of physical health, mental health, and marital satisfaction of survivors were comparable with those of caregivers. The survivor's scores were not significantly correlated with their caregiver's scores (ps>.10).
Table 1. Descriptives of study variables, paired sample t-tests and Pearson correlation coefficients between APC survivor and spousal caregiver (N=29 dyads).
| Survivors | Caregivers | t | r | |
|---|---|---|---|---|
| Age (years) | 71.9 (SD=8.9) | 67.4 (SD=9.5) | 3.7* | |
| Education (years) | 15.5 (SD=3.2) | 14.6 (SD=2.4) | 2.5* | |
| Household Income ($) | 59,200 (SD=28,400) |
-- | ||
| Months since diagnosis | 31.1 (SD=8.8) | -- | ||
| Months since treatment | 11.8 (SD=9.6) | -- | ||
|
Other completed treatments (% of sample) |
||||
| Radical prostatectomy | 50% | |||
| Radiation therapy | 33% | |||
| Ethnicity | ||||
| Non Hispanic White | 62% | 76% | ||
| Hispanic | 17% | 10% | ||
| African-American | 21% | 14% | ||
| Mental health | 77.2 (SD=17.4) | 73.7 (SD=20.3) | .62 | -.07 |
| Physical health | 77.4 (SD=17.1) | 73.8 (SD=24.1) | .56 | -.05 |
| Marital satisfaction | 40.0 (SD=5.1) | 38.7 (SD=5.3) | .98 | .25 |
p<.05
Relationship Between Mental Health and Marital Satisfaction
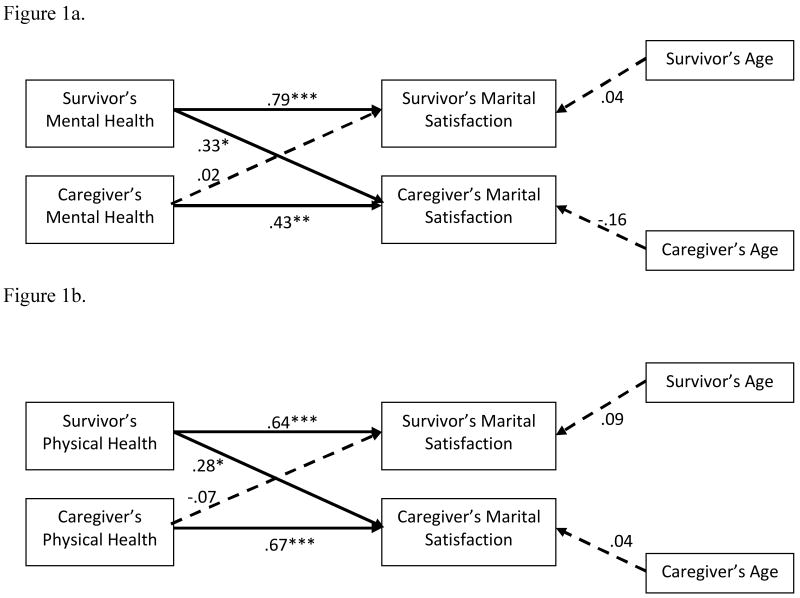
As shown in Figure 1a (CFI=.983; RMSEA=.035), both the survivors' mental health and the caregivers' mental health were positively related to their marital satisfaction, supporting actor effects. In addition, the survivor's mental health was positively related to their caregiver's marital satisfaction, supporting a partner effect. However, the caregivers' mental health was not significantly related to the survivor's marital satisfaction. Age was not significantly related to marital satisfaction scores.
Figure 1.
Relationships between mental and physical health and marital satisfaction in a sample of APC survivors and their spousal caregivers.
Note: Standardized regression coefficients shown, with solid lines represent statistically significant relationships (*p<.05, **p<.01, ***p<.001). The survivor's and spousal caregiver's age were correlated with one another. Measurement errors between the survivor's mental and physical health, with the caregiver's mental and physical health, and between the survivor's and spousal caregiver's marital satisfaction scores were allowed to be correlated with each other.
Relationship Between Physical Health and Marital Satisfaction
The same actor effects and a partner effect were found in the relationship between physical health and marital satisfaction (Figure 1b; CFI=.977; RMSEA=.041): For survivors and caregivers, physical health was positively related to their own marital satisfaction, supporting actor effects. The only significant partner effect was identified between the caregiver's physical health and survivor's marital satisfaction.
Discussion
Despite the fact that PC is often considered a ‘couple's disease,’ PC survivors and their spousal caregivers are an understudied group. In particular, APC survivors who have undergone ADT are a population that face challenges unique from even localized PC survivors. These men are not only faced with a lengthy list of physical side effects from treatment, but also with psychological challenges associated with issues including adjusting to those side effects as well as their high risk of mortality. Additionally, their spouses must find ways to adjust to the tremendous impact APC can have on their lives as well. Our primary aim was to document levels of physical health, mental health and marital satisfaction within this understudied population. The physical health score for the survivors from this sample was higher than that of other APC samples, while the mental health and marital satisfaction scores were comparable [13, 17-18]. Thus, despite the challenges associated with a diagnosis of APC, and subsequent ADT treatment, it appears that participants in our study have found effective ways of coping with their disease.
Our secondary aim was to examine the individual and dyadic health factors affecting marital satisfaction. We conclude that individual's physical and mental health are positively related with their marital satisfaction, and this is consistent with existing literature in localized PC, which has identified similar actor effects of the PC survivor's mental health functioning on marital satisfaction [19]. Furthermore, evidence from this study suggests that there are partner effects of the survivor's physical and mental health on their spouse's level of marital satisfaction, concurring with existing literature which has found that a PC survivor's physical and mental health were associated with lower QoL and greater distress in their caregivers [19]. This study did not provide any evidence of a partner effect on the survivor's level of marital satisfaction. We speculate that there may not have been a partner effect on the survivor's marital satisfaction for several reasons. First, the survivor may be too focused on his own disease management process to be concerned about marital satisfaction. Second, it is possible that subtle cues of physical or mental dysfunction in the caregiver may not be noticed by the survivor, as existing literature has supported the idea that men are less likely to be attentive to the emotional needs of other individuals in their life [20].
Our novel findings emphasize the important role of physical and mental health on marital satisfaction in APC dyads. Furthermore, we identify the APC survivor's functioning as having a notable role in how satisfied his spouse is with the relationship. These findings provide several clinical implications that should be further evaluated. First, one area in which marital satisfaction in the dyad can be improved is by finding ways to enhance physical and mental health of individuals. Second, it is important to educate the spousal caregivers as to the effects of their husband's physical and mental health on their relationship satisfaction. This may help to identify any mis-attributions the spousal caregiver has of problems in the marriage, and to provide a foundation from which to improve the state of that relationship.
Several limitations from this study should be noted. First, our findings are based on cross-sectional data, which precludes causal interpretations. A model with reversed directionality was evaluated, and demonstrated acceptable model fit. In the future, it will be important to replicate the current findings to longitudinally evaluate the survivor and caregiver dyad during their cancer adjustment experience. Second, we had a limited sample size that prevented more complex analyses of possible mediators in the relationship between physical and mental health with marital satisfaction, such as coping styles or illness perceptions [3]. Finally, the study sample was relatively well adjusted and may not be fully representative of all APC survivors and their spousal caregivers.
Despite these limitations, these findings contribute to a growing area of study that identifies the spousal caregiver as an under-studied, but very important, part of any PC survivor's cancer experience. In particular, for APC survivors, it appears that the impact of the disease is not limited just to their own functioning, but also has implications in their spouse's satisfaction with their marriage.
Acknowledgments
We are thankful for the time of all of the participants of this study as well as for the help of many students and staff members who helped make this study possible. This research was funded by NCI Grant #R21-CA102761-01A2.
References
- 1.American Cancer Society. Cancer Facts and Figures 2009. American Cancer Society; Atlanta: 2009. [Google Scholar]
- 2.Potosky AL, Reeve BB, Clegg LX, et al. Quality of life following localized prostate cancer treated initially with androgen deprivation therapy or no therapy. Journal of the National Cancer Institute. 2002;94:430–437. doi: 10.1093/jnci/94.6.430. [DOI] [PubMed] [Google Scholar]
- 3.Northouse LL, Mood DW, Montie JE, et al. Living with prostate cancer: Patients' and spouses' psychosocial status and quality of life. Journal of Clinical Oncology. 2007;25:1–7. doi: 10.1200/JCO.2006.09.6503. [DOI] [PubMed] [Google Scholar]
- 4.Nijboer C, Tempelaar R, Sanderman R, Triemstra M, Sprujt RJ, van den Bos GA. Cancer and caregiving: The impact on the caregiver's health. Psycho-Oncology. 1998;7:3–13. doi: 10.1002/(SICI)1099-1611(199801/02)7:1<3::AID-PON320>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 5.Haley WE, LaMonde LA, Han B, Narramore S, Schonwetter R. Family caregiving in hospice: Effects on psychological and health functioning among spousal caregivers of hospice patients with lung cancer or dementia. Hospice Journal. 2001;15:1–18. doi: 10.1080/0742-969x.2000.11882959. [DOI] [PubMed] [Google Scholar]
- 6.Couper JW, Bloch S, Love A, Duchesne G, Macvean M, Kissane DW. The psychosocial impact of prostate cancer on patients and their partners. The Medical Journal of Australia. 2006;185:428–432. doi: 10.5694/j.1326-5377.2006.tb00640.x. [DOI] [PubMed] [Google Scholar]
- 7.Couper J, Bloch S, Love A, Macvean M, Duchesne GM, Kissane D. Psychosocial adjustment of female partners of men with prostate cancer: A review of the literature. Psycho-Oncology. 2006;15:937–953. doi: 10.1002/pon.1031. [DOI] [PubMed] [Google Scholar]
- 8.Langer S, Abrams J, Syrjala K. Caregiver and patient marital satisfaction and affect following hematopoietic stem cell transplantation: A prospective, longitudinal investigation. Psycho-Oncology. 2003;12:239–253. doi: 10.1002/pon.633. [DOI] [PubMed] [Google Scholar]
- 9.Weihs K, Enright T, Howe G, Siemens S. Marital satisfaction and emotional adjustment after breast cancer. Journal of Psychosocial Oncology. 1999;17:33–49. [Google Scholar]
- 10.Krongrad A, Lai H, Burke MA, Goodkin K, Lai S. Marriage and mortality in prostate cancer. The Journal of Urology. 1996;156:1696–1700. doi: 10.1016/S0022-5347(01)65485-5. [DOI] [PubMed] [Google Scholar]
- 11.Penedo FJ, Benedict C, Zhou ES, Kava B, Soloway M, Antoni M, Schneiderman N. Telephone based cognitive behavioral stress management intervention improves coping, quality of life, and cortisol regulation in men undergoing hormonal treatment (HT) for advanced prostate cancer (APC) International Journal of Behavioral Medicine. 2010;17:S23. [Google Scholar]
- 12.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36) Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 13.Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and Family. 1976;38:15–28. [Google Scholar]
- 14.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 15.Levenson RW, Carstensen LL, Gottman JM. Long-term marriage: Age, gender and satisfaction. Psychology and Aging. 1993;8:301–313. doi: 10.1037/0882-7974.8.2.301. [DOI] [PubMed] [Google Scholar]
- 16.Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. Guilford Press; New York: 2006. [Google Scholar]
- 17.Albertsen PC, Aaronson NK, Muller MJ, Keller SD, Ware JE. Health-related quality of life among patients with metastatic prostate cancer. Urology. 1997;49:207–217. doi: 10.1016/S0090-4295(96)00485-2. [DOI] [PubMed] [Google Scholar]
- 18.Banthia R, Malcarne VL, Varni JW, Ko CM, Sadler GR, Greenbergs HL. The effects of dyadic strength and coping styles on psychological distress in couples faced with prostate cancer. Journal of Behavioral Medicine. 2003;26:31–52. doi: 10.1023/A:1021743005541. [DOI] [PubMed] [Google Scholar]
- 19.Kornblith AB, Herr HW, Ofman US, Scher HI, Holland JC. Quality of life of patients with prostate cancer and their spouses The value of a data base in clinical care. Cancer. 1994;73:2791–2802. doi: 10.1002/1097-0142(19940601)73:11<2791::aid-cncr2820731123>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 20.Lutzky SM, Knight BG. Explaining gender differences in caregiver distress: The roles of emotional attentiveness and coping styles. Psychology and Aging. 1994;9:513–519. doi: 10.1037/0882-7974.9.4.513. [DOI] [PubMed] [Google Scholar]