Abstract
OBJECTIVE:
To evaluate the effects of short‐term exercise detraining on the functional fitness of older women after a 12‐week water‐based exercise (WE) program.
METHODS:
Healthy older women (trained (TR) group) were submitted to 12 weeks WE (three 45 min sessions per week) followed by a 6‐week detraining period. A group of aged‐matched women without any exercise training (UN group) were evaluated during the same period. The aerobic power, measured by VO2max and 800 meters performance, and the neuromuscular fitness and quality of life were evaluated. All assessments were made at baseline, after 12 weeks of training and after 4 and 6 weeks of detraining.
RESULTS:
No changes were found for the UN group during the follow‐up study, but WE induced significant improvement in aerobic capacity, neuromuscular fitness and quality of life score. However, the upper and lower body strength, agility, flexibility, and body balance returned to UN levels (p>0.05) after 6 weeks of detraining.
CONCLUSIONS:
The results confirmed that 12 weeks of WE improves the functional fitness parameters and quality of life of older women. However, after a short detraining period of 4–6 weeks, the neuromuscular parameters and the quality of life score returns to baseline or untrained subject levels.
Keywords: Older women, Water‐based exercise, Functional fitness, Detraining
INTRODUCTION
Ageing often leads to a loss of functional fitness in older people, reducing their ability to perform daily tasks.1 Moreover, fall‐related injuries are serious problems in old age, as they often lead to prolonged, or even permanent, disability. Thus, maintenance of functional fitness and prevention of the associated injuries should reduce disability, improve the quality of life, and reduce the costs of health care.
Exercise training has been shown to be an effective non‐pharmacological way of reducing physical difficulties in older people. Recently, we demonstrated that exercise training contributes significantly to the maintenance of functional fitness in older healthy people2 and those with cardiac disease.3 Furthermore, exercise is generally accepted as effective in preventing falls in old age. A review of randomized controlled trials has demonstrated that exercise reduces the risk of falls in elderly people, and reduction in the incidence of fall‐related injuries is related to lower healthcare costs.4
Water‐based exercise (WE) has been widely promoted as the optimal type of exercise for older people as it reduces weight‐bearing stresses on the skeletal joints and provides therapeutic benefits for orthopedic conditions.5,6 In addition, WE‐associated benefits3,6 are in agreement with current recommendations stating that aerobic power, muscle strength, and body flexibility are important factors in maintaining functional independence in older people.7,8
The health benefits of any exercise depend on its regularity, but older people commonly have different chronic diseases, side effects of drugs, hospitalization, and disability, which may be compelling reasons to abandon exercise programs.9 Most studies of detraining in older people have evaluated the effects after stopping land‐based resistance training of low to high intensity10-12 or multicomponent programs.9,13 To the best of our knowledge, few studies have reported the effects of detraining after a WE program, and they have evaluated functional ability only in people with neuromuscular and cardiovascular illness.12,14
Despite some evidence of physiological decline after short detraining periods,9,15,16 there are insufficient data on functional fitness and quality‐of‐life changes in healthy older women when a WE program is stopped. Therefore, this study was designed to determine the effects of 12‐weeks of WE training followed by a 6‐week detraining period on the functional fitness of older healthy women.
MATERIAL AND METHODS
Participants
This study included 50 women aged >62 years. All participants underwent a clinical examination and answered questionnaires about their medical history; the exclusion and inclusion criteria have been described in detail elsewhere.2,3 All participants read and signed the terms of consent before inclusion in the study in accordance with the Declaration of Helsinki.
The women were randomized into a trained (TR; n = 30) or untrained group (UN; n = 20). The TR group was directed to follow a WE program, and the UN group comprised women who could not undergo frequent training sessions. Subjects from both groups continued with their daily activities, and the TR group underwent no other physical training besides WE.
Training and Detraining Protocols
A detailed description of the training process can be found in a recent study published by our laboratory.2 Briefly, the WE program consisted of 60‐min sessions, three times a week, over 12 weeks. Training was performed on three different days, with a 1‐day rest between sessions. Each training session included a 10‐min warm‐up stretching period (stage 1); 45‐min endurance training (stage 2); and a 5‐min cool‐down/relaxation period with slow walking and stretching (stage 3). This training protocol is in agreement with the exercise guidelines recommended by the American College of Sports Medicine for healthy adults and the elderly.7 To detrain, the WE group were instructed to give details of any new prescribed medication, to not participate in any other type of physical activity, and finally, to continue only with their usual daily activities.
Measurements
Both groups were assessed by the same researcher at four time points as follows: before training (baseline), after 12 weeks of training, and after 4 and 6 weeks of detraining. Five sets of evaluations were obtained on different days to improve knowledge of the methods and robustness of the test technique.
Body mass index (BMI)
Height and body mass were measured using a stadiometer and balance weighing scales. Body mass index was calculated by the equation: BMI = body mass (kg)/height2 (m2).
Aerobic fitness
A Bruce treadmill protocol was carried out to determine the VO2max as previously described.2 A 1‐min warm‐up without treadmill inclination at 1.0 mph preceded the Bruce treadmill protocol. The Borg scale with scores of between 6 and 20 was used for determination of subjective exertion level. The test was considered a success if participants reached their age‐predicted maximum heart rate—that is, 220 – age, with the result in beats per minute).
For the functional aerobic test, we used the 800 meters test standardized for the Brazilian population17 and previously used by Bocalini et al.3 Subjects were instructed to run or walk a distance of 800 meters as quickly as possible.
Neuromuscular fitness
The “arm curl” test assessed upper body strength and was scored as the total number of hand weight curls through the full range of motion in 30 seconds. The “chair stand” test assessed lower body strength and was scored as the number of stands executed correctly within 30 seconds. Agility was assessed by the shortest time for the “8‐foot up and go” test—that is, rising from a seated position, walking 8 feet, returning to the seated position. The chair “sit and reach” test assessed lower body flexibility and was scored as the best distance achieved between the extended fingers and the tip of the toe. Static balance was assessed by asking subjects to stand on one leg for a maximum of 30 seconds on each side18 and was scored as the longest time of quiet standing, allowing only minimal fluctuations of ankle position or obvious toe clawing, and no hopping or arm movement. The test was stopped after 30 seconds or whenever the raised foot touched the floor or contacted the other leg/foot, the ankle movement was excessive, or hopping occurred.
Quality of life
Quality of life was evaluated by a shortened WHO quality‐of‐life questionnaire as previously used by Bocalini et al.3 The questionnaire comprised 25 questions about several aspects of quality of life, including: Physical Domain, which concerns pain or discomfort, energy or fatigue, sleep, rest, mobility, daily activities, medicine dependency, and job performance; Psychological Domain, which includes feelings, learning, memory and attention, self‐esteem, aspect, spirituality, religiousness, and positive or negative thinking; Social Domain, which deals with personal relationships, social support and sexuality; Environmental Domain, which includes physical security, home environment, financial security, opportunity for information assessment, social or cultural event participation, and activities undertaken during spare time. Each domain was scored from 0 to 100 points, and higher scores represented improvement.
Statistical analysis
Data (means ± SEM) were analyzed using the GraphPad Prism software (version 4.0, San Diego, CA, USA). Two‐way analysis of variance for repeated‐measures analysis was used to examine differences within and between groups over time, and the Tukey post hoc test was used when appropriate. The significance level was set at p<0.05.
RESULTS
During the research period, three women from the TR group left the study and two women from the UN group could not be traced at the end of the study for the re‐evaluation. Therefore, our data are based on the following subjects: UN (n = 18) and TR (n = 27).
There were no differences between the groups at baseline for age or body mass index (Table 1), or for aerobic capacity (Figure 1), neuromuscular fitness (Table 2) and quality of life (Figure 2). Furthermore, all outcomes for the UN group remained unchanged throughout the follow‐up. After the 12‐week WE program, the body mass index was similar between the groups, and nor were any differences found between the groups after 4‐ and 6‐weeks of detraining (Table 1).
Table 1.
Changes of biometric parameters after training and detraining.
| 12‐week WE program | Detraining | |||||||
| Baseline | After WE | 4 Weeks | 6 Weeks | |||||
| TR | UN | TR | UN | TR | UN | TR | UN | |
| Body weight (kg) | 78 ± 2 | 79 ± 2 | 75 ± 2 | 78 ± 2 | 76 ± 2 | 79 ± 2 | 77 ± 2 | 79 ± 2 |
| Height (m) | 1.61 ± 2.32 | 1.62 ± 2.21 | 1.61 ± 2.35 | 1.61 ± 2.23 | 1.62 ± 2.34 | 1.61 ± 2.00 | 1.62 ± 2.45 | 1.61 ± 2.00 |
| BMI (kg/m2) | 29 ± 1 | 30 ± 1 | 29 ± 1 | 30 ± 1 | 29 ± 0.78 | 30 ± 1 | 29 ± 1 | 31 ± 1 |
Results are expressed at mean ± SEM for water‐based exercise trained (TR) and untrained (UN) groups.
No statistical differences were found between groups, condition or time of analysis.
BMI, body mass index; WE, water‐based exercise.
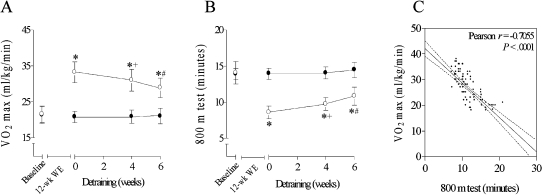
Figure 1.
Aerobic fitness assessed by VO2max (A) and 800 m walking test (B) at baseline, after 12‐week water‐based exercise (WE) program and, with 4 and 6 weeks of detraining. (C) Correlation between these functional capacity evaluations. Open circles shows the trained group; closed circles shows the untrained group. Two‐way analysis of variance followed by a Tukey post hoc test was applied for comparisons. *p<0.05 vs. baseline and group without any exercise training; +p<0.05 vs. 12 weeks of WE; #p<0.05 vs. 4 weeks of detraining.
Table 2.
Changes in functional fitness after training and detraining.
| Strength | Agility | Flexibility | Balance | ||
| Test S1 | Test S2 | Test A1 | Test F1 | Test B1 | |
| Baseline | |||||
| TR | 17.9 ± 0.6 | 23.7 ± 0.3 | 15.4 ± 0.6 | 12.9 ± 0.7 | 14.6 ± 0.3 |
| UN | 17.9 ± 1.0 | 23.6 ± 0.5 | 14.3 ± 0.7 | 13.0 ± 0.9 | 14.3 ± 0.5 |
| After 12 weeks of WE | |||||
| TR | 25.0 ± 0.5*# | 33.6 ± 0.5*# | 9.8 ± 0.6*# | 18.9 ± 0.9 *# | 23.0 ± 0.8*# |
| UN | 18.1 ± 0.9 | 23.7 ± 0.5 | 14.4 ± 0.7 | 13.1 ± 1.0 | 14.6 ± 0.6 |
| 4 Weeks of detraining | |||||
| TR | 20.8 ± 0.5*+ | 28.2 ± 0.3*#+ | 11.1 ± 0.6*+ | 14.9 ± 0.8*+ | 17.4 ±0.3*#+ |
| UN | 18.4 ± 0.8 | 23.9 ± 0.5 | 15.0 ± 0.5 | 13.3 ± 0.9 | 14.9 ± 0.8 |
| 6 Weeks of detraining | |||||
| TR | 18.9 ± 0.5+ | 26.0 ± 0.2 *+ | 13.9 ± 0.6*+ | 13.3 ± 0.7+ | 17.1± 0.1*+ |
| UN | 18.9 ± 0.9 | 24.3 ± 0.7 | 15.5 ± 0.5 | 13.8 ± 0.9 | 15.6 ± 0.9 |
Data are expressed at mean ± SEM for water‐based exercise (WE) trained (TR) and untrained (UN) groups. Two‐way ANOVA followed by Tukey post hoc test was applied for comparisons.
p<0.05 vs. baseline.;
p< 0.05 vs. 12 weeks of WE;
p<0.05 vs. UN group.
Fitness tests for strength: arm curl repetitions in 30 s (test S1) and chair stand repetitions in 30 s (test S2); agility: time in seconds to 8‐feet up and go (test A1); flexibility: distance in centimeters obtained on sit and reach test (test F1); and static balance: time in seconds of quiet standing up on just one leg without hopping (test B1).
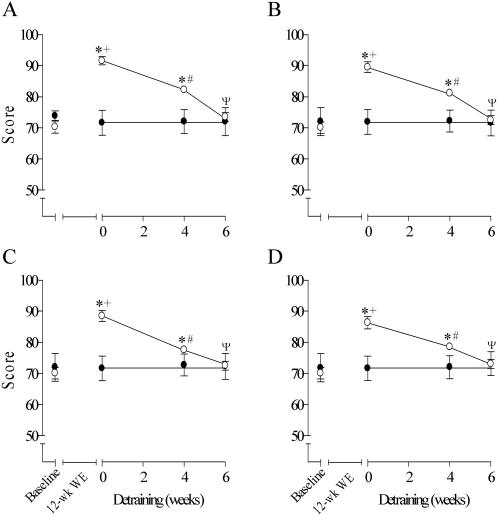
Figure 2.
Quality of life evaluated by the multiple domain questionnaires in baseline, after 12‐week water‐based exercise (WE) program and with 4 and 6 weeks of detraining (Panel A: physical domain; Panel B: psychological domain; Panel C: social domain and Panel D: environmental domain). Open circles shows the trained group; closed circles shows the untrained group. Two‐way ANOVA followed by Tukey post hoc test was applied for comparisons. *p<0.05 vs. baseline; +p<0.05 vs. group without any training; #p<0.05 vs. 12 weeks of WE; Ψp<0.05 vs. 4 weeks of detraining.
The aerobic fitness of the TR group was enhanced significantly after training, but with detraining, this group showed a progressive impairment with decreasing VO2max (Figure 1A) and increase in the time for the 800 m test (Figure 1B). However, even after 6 weeks of detraining, the scores of the TN group remained better than at baseline and better than those of the UN group (Figure 1A and B). In addition, a significant high correlation was found between VO2max and the 800 m test (Figure 1C).
Table 2 shows the results for the neuromuscular fitness assessment. After 12‐weeks of training, there was significant improvement of 28% and 29% in upper and lower body strength as evaluated by the arm curl and chair stand tests, respectively. Moreover, there were improvements of 36% for the 8‐foot up and go test, 31% for the chair sit and reach test and 36% for static balance, showing an enhancement of the agility, flexibility and balance, respectively. However, the neuromuscular fitness became progressively impaired when training was discontinued, and after just 4 weeks of detraining all scores were significantly lower than after 12 weeks of WE training. Only lower body strength and static balance remained significantly higher than those of the UN group at this time.
Table 2 shows that a greater decline in the functional fitness scores occurred after 6 weeks of detraining, and all the analyzed parameters were similar in the TN and UN groups. The most pronounced effect of detraining was seen in the arm curl and sit and reach tests, which returned to their baseline level.
WE training resulted in a significant general improvement in all the domains of quality of life (Figure 2), but there was a progressive return to baseline levels after as early as 4 weeks of detraining, matching completely the UN group and baseline levels at 6 weeks of detraining.
DISCUSSION
The major finding of this study was that after 6 weeks of detraining, the improvement of functional fitness of older healthy women, achieved with 12 weeks of WE training, was lost. Not only body strength and agility, but also flexibility and static balance, and quality of life had returned to pre‐training conditions. Aerobic fitness was least affected by detraining, since the VO2max values and performance on 800 m test remained higher than those of the UN group and of the pre‐training values.
Our results show that the 12‐week WE program improved several components of functional fitness in older women, was well tolerated, and no adverse events, such as fall‐related injuries or adverse cardiovascular effects, were seen in any subject during the exercise program, suggesting that the protocol is safe. These indications corroborate previous studies reporting that regular participation in a structured exercise program is a safe and effective intervention for healthy older people, improving their aerobic capacity, body strength, flexibility, agility and range of motion.3,6 To evaluate whether physical exercise practice can improve social and personal wellbeing and quality of life, we used a validated questionnaire and noted a significant enhancement in the quality‐of‐life scores of the trained group, including physical, psychological, social and environmental domains. These findings also agree with those of other investigators5 and are important, since studies have demonstrated a strong association between psychosocial problems such as depression, anxiety or social isolation, and chronic diseases.19
The improvement in the TN group on both the VO2max and 800 m tests owing to the 12‐week WE program was significantly lost after 6 weeks of detraining, although their scores remained better than those of matched UN subjects and the baseline values. An explanation for this reduction in aerobic fitness with detraining remains unclear. It is well known that improvement in aerobic capacity with training is influenced by cardiovascular and musculoskeletal adaptations.20,21 Thus, the decline in cardiac output, arteriovenous difference, oxidative enzymes, hemoglobin concentration, myocytic mitochondria density, and muscle capillarization, which occur with detraining, may contribute to the decrease in aerobic fitness.22-24
Although the lower body strength did not return to the baseline levels when exercise was stopped, our results are similar to those of others using a different exercise modality in an older people13,16,25,26 and indicate that lower body strength scores decrease significantly and are similar to UN scores after detraining. Our subjects had a decrease in upper body strength as early as after 4 weeks of detraining, and returned to baseline at the sixth week of detraining. A plausible explanation for these divergences between upper and lower body strength may be the greater adaptable response to exercise of the lower limbs. Other possible conflicting factors are the variable adjustments to different frequency, type duration and intensity of training and detraining, as well as the age‐related particular daily activity routines during the detraining period that may affect upper and lower limbs differently.25-28
Agility/balance has an essential role in routine activities in old age. Some authors have demonstrated that the agility/balance gain is lost 6 weeks after exercise cessation,9 but other studies have found the gain to be maintained even after 313 or 12 months of detraining.8 The agility/balance improvement in the cases that use land‐based exercise is probably due to a gain in strength, as described for a multicomponent exercise program.10,29,30 Thus, we believe that for the WE program also, the agility/balance changes should be directly correlated with improvement and impairment of both the balance and strength during training and detraining, respectively, as also proposed by Ryushi et al.30
In agreement with previous multicomponent training studies in older women,9,13 flexibility was significantly affected by detraining. After only 6 weeks of detraining the improvement in flexibility achieved with the WE program had reverted to baseline level. Owing to its importance for physical autonomy and fall/injury prevention,4 the maintenance of flexibility should be evaluated with caution during detraining in older adults.
Finally, a significant worsening of quality of life was associated with detraining, with the benefits of the WE program being almost completely lost in just 4 weeks. Moreover, the worsening in all domains of the quality of life (physical, psychological, social, and environment) matched closely reductions in aerobic capacity, body strength, agility, flexibility, and static balance, thus reinforcing scientific evidence that directly correlates regular physical exercise with psychosocial well‐being and quality of life in older people.2,31
This is a relatively small sample and short‐term study, with no information about long‐term outcomes. Nevertheless, for future public health strategies, this work reinforces the message of the importance of the frequency and regularity of this exercise modality. In addition, there may be some inaccuracy in estimating maximum aerobic fitness (indirect estimate of VO2max) by measuring cardiopulmonary gas exchange. Nevertheless this drawback was common to both the UN and TR groups and for all evaluations during follow‐up, thus reducing inaccuracy. Despite this significant induction of positive changes in the functional fitness of older women with the WE program, more studies are needed to examine WE practices and the effect of education, training and detraining on older men and women.
CONCLUSION
This study demonstrated that short term WE training improves cardiorespiratory and neuromuscular fitness. As a result, the ability to carry out tasks of daily living is enhanced with WE training, leading to independence, psychosocial well‐being and better quality of life in older women. However, regularity of the exercise had a key role, as after a short period of detraining, most neuromuscular fitness parameters and quality‐of‐life scores returned to baseline levels.
ACKNOWLEDGEMENTS
Special acknowledgment is given to Planet Sport Academia for all assistance.
REFERENCES
- 1. Chu KS, Eng JJ, Dawson AS, Harris A. Water‐based exercise for cardiovascular fitness in people with chronic stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2004;85:870–4. doi: 10.1016/j.apmr.2003.11.001. 10.1016/j.apmr.2003.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bocalini DS, Serra AJ, Levy RF, Murad N. Water‐ vs walking land‐based exercise effects on the physical fitness in older women. Geriatr Gerontol Int. 2008;8:265–71. doi: 10.1111/j.1447-0594.2008.00485.x. 10.1111/j.1447‐0594.2008.00485.x [DOI] [PubMed] [Google Scholar]
- 3. Bocalini DS, Serra A, dos Santos L. Physical exercise improves functional capacity and quality of life in patients with heart failure. Clinics. 2008;63:437–42. doi: 10.1590/S1807-59322008000400005. 10.1590/S1807‐59322008000400005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gardner MM, Robertson MC, Campbell AJ. Exercise in preventing falls and fall related injuries in older people: a review of randomized controlled trials. Br J Sports Med. 2000;34:7–17. doi: 10.1136/bjsm.34.1.7. 10.1136/bjsm.34.1.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Carral JMC, Pérez CA. Effects of high‐intensity combined training on women over 65. Gerontology. 2007;53:340–6. doi: 10.1159/000104098. 10.1159/000104098 [DOI] [PubMed] [Google Scholar]
- 6. Takeshima N, Rogers ME, Watanabe E. Water based exercise improves health‐related aspects of fitness in older women. Med Sci Sports Exerc. 2002;33:544–51. doi: 10.1097/00005768-200203000-00024. [DOI] [PubMed] [Google Scholar]
- 7. American College of Sports Medicine. Exercise and physical activity for older adults. Med Sci Sports Exerc. 1998;30:992–1008. 10.1097/00005768‐199806000‐00033 [PubMed] [Google Scholar]
- 8. McDermott AY, Mernitz H. Exercise and older patients: prescribing guidelines. Am Fam Physician. 2006;74:437–44. [PubMed] [Google Scholar]
- 9. Toraman NF, Erman A, Agyar E. Effects of multicomponent training on functional fitness in older adults. J Aging Phys Act. 2004;2:538–53. doi: 10.1123/japa.12.4.538. [DOI] [PubMed] [Google Scholar]
- 10. Fatouros IG, Kambas A, Katrabasas I. Strength training and detraining effects on muscular strength, anaerobic power, and mobility of inactive older men are intensity dependent. Br J Sports Med. 2005;39:776–80. doi: 10.1136/bjsm.2005.019117. 10.1136/bjsm.2005.019117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Slentz CA, Houmard JA, Johnson JL. Inactivity, exercise training and detraining, and plasma lipoproteins. STRRIDE: a randomized, controlled study of exercise intensity and amount. J Appl Physiol. 2007;103:432–42. doi: 10.1152/japplphysiol.01314.2006. 10.1152/japplphysiol.01314.2006 [DOI] [PubMed] [Google Scholar]
- 12. Tokmakidis SP, Spassis AT, Volaklis KA. Training, detraining and retraining effects after a water‐based exercise program in patients with coronary artery disease. Cardiology. 2008;111:257–64. doi: 10.1159/000127737. 10.1159/000127737 [DOI] [PubMed] [Google Scholar]
- 13. Carvalho MJ, Marques E, Mota J. Training and detraining effects on functional fitness after a multicomponent training in older women. Gerontology. 2008;55:41–8. doi: 10.1159/000140681. 10.1159/000140681 [DOI] [PubMed] [Google Scholar]
- 14. Tomas‐Carus P, Häkkinen A, Gusi N. Aquatic training and detraining on fitness and quality of life in fibromyalgia. Med Sci Sports Exerc. 2007;39:1044–50. doi: 10.1249/01.mss.0b0138059aec4. 10.1249/01.mss.0b0138059aec4 [DOI] [PubMed] [Google Scholar]
- 15. Sforzo GA, Macmanis BG, Black D. Resilience to exercise detraining in healthy older adults. J Am Geriatr Soc. 1995;43:209–15. doi: 10.1111/j.1532-5415.1995.tb07324.x. [DOI] [PubMed] [Google Scholar]
- 16. Toraman NF, Ayceman N. Effects of six weeks of detraining on retention of functional fitness of old people after nine weeks of multicomponent training. Br J Sports Med. 2005;39:565–8. doi: 10.1136/bjsm.2004.015586. 10.1136/bjsm.2004.015586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Andreotti RA, Okuma SS. Validação de uma Bateria de Testes de Atividade da Vida Diária para Idosos Fisicamente Independentes. Revista Paulista de Educação Física. 1999;13:46–66. [Google Scholar]
- 18. Villareal DT, Banks M, Siener C. Physical frailty and body composition in obese elderly men and women. Obes Res. 2004;12:913–20. doi: 10.1038/oby.2004.111. 10.1038/oby.2004.111 [DOI] [PubMed] [Google Scholar]
- 19. Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99:2192–217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 20. Hoppeler H, Howald H, Conley K. Endurance training in humans: aerobic capacity and structure of skeletal muscle. J Appl Physiol. 1985;59:320–7. doi: 10.1152/jappl.1985.59.2.320. [DOI] [PubMed] [Google Scholar]
- 21. Ookawara T, Suzuki K, Haga S. Transcription regulation of gene expression in human skeletal muscle in response to endurance training. Research communications in Molecular Pathol Pharmacol. 2002;111:41–54. [PubMed] [Google Scholar]
- 22. Convertino VA, Bisson R, Bates D. Effects of antiorthostatic bed rest on the cardiorespiratory responses to exercise. Aviation Space Enviromental Medicine. 1981;52:251–5. [PubMed] [Google Scholar]
- 23. Coyle EF, Martin WH, Sinacore DR. Time course of loss of adaptations after stopping prolonged intense endurance training. J Appl Physiol. 1984;57:1857–67. doi: 10.1152/jappl.1984.57.6.1857. [DOI] [PubMed] [Google Scholar]
- 24. Madsen K, Pedersen PK, Djurhuus MS. Effects of detraining on endurance capacity and metabolic changes during prolonged exhaustive exercise. J Appl Physiol. 1993;75:444–51. doi: 10.1152/jappl.1993.75.4.1444. [DOI] [PubMed] [Google Scholar]
- 25. Raso V, Matsudo SMM, Matsudo VKR. A força muscular de mulheres idosas decresce principalmente após oito semanas de interrupção de um programa de exercícios com pesos livres. Rev Bras Med Esporte. 2001;7:177–86. [Google Scholar]
- 26. Michelin E, Coelho CF, Burini RC. Efeito de um mês de destreinamento sobre a aptidão física relacionada à saúde em programa de mudança de estilo de vida. Rev Bras Med Esporte. 2008;14:192–6. 10.1590/S1517‐86922008000300006 [Google Scholar]
- 27. Fatouros IG, Kambas A, Katrabasas I, Nikolaidis K, Chatzinikolaou A, et al. Strength training and detraining effects on muscular strength, anaerobic power, and mobility of inactive older men are intensity dependent. Br J Sports Med. 2005;39:776–80. doi: 10.1136/bjsm.2005.019117. 10.1136/bjsm.2005.019117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fatouros IG, Kambas A, Katrabasas I, Leontsini D, Chatzinikolaou A, Jamurtas AZ, et al. Resistance training and detraining effects on flexibility performance in the elderly are intensity‐dependent. J Strength Cond Research. 2006;20:634–642. doi: 10.1519/R-17615.1. [DOI] [PubMed] [Google Scholar]
- 29. Nelson ME, Layne JE, Bernstein MJ. The effects of multidimensional home‐based exercise on functional performance in elderly people. Journals of Gerontology. Series A, Biol Sci Med Sci. 2004;59:154–60. doi: 10.1093/gerona/59.2.m154. [DOI] [PubMed] [Google Scholar]
- 30. Ryushi T, Kumagai K, Hayase H. Effect of resistive knee extension training on postural control measures in middle aged and elderly persons. J Physiol Anthropol Appl Human Sci. 2000;19:143–9. doi: 10.2114/jpa.19.143. 10.2114/jpa.19.143 [DOI] [PubMed] [Google Scholar]
- 31. Yoshikawa TT. New and evolving concepts in geriatrics and gerontology. Geriatr Gerontol Int. 2004;4:S26. 10.1111/j.1447‐0594.2004.00140.x [Google Scholar]