Abstract
In temperate regions of the world, influenza epidemics follow a highly regular seasonal pattern, in which activity peaks in midwinter. Consistently with this epidemiology, we have shown previously that the aerosol transmission of a seasonal H3N2 influenza virus is most efficient under cold, dry conditions. With the 2009 H1N1 pandemic, an exception to the standard seasonality of influenza developed: during 2009 in the Northern Hemisphere, an unusually high level of influenza virus activity over the spring and summer months was followed by a widespread epidemic which peaked in late October, approximately 2.5 months earlier than usual. Herein we show that aerosol transmission of a 2009 pandemic strain shows a dependence on relative humidity and temperature very similar to that of a seasonal H3N2 influenza virus. Our data indicate that the observed differences in the timings of outbreaks with regard to the seasons are most likely not due to intrinsic differences in transmission between the pandemic H1N1 and seasonal H3N2 influenza viruses.
In temperate regions of the world, influenza epidemics occur with a very regular seasonal pattern: influenza activity exceeding the epidemic threshold is generally seen only in the winter, with peak activity observed in January or February in the North and in June or July in the South (7; http://www.cdc.gov/flu/about/season/flu-season.htm). In 2009, circulation of the swine origin, pandemic H1N1 strain in the Northern Hemisphere exhibited very different timing with regard to the seasons. The pandemic virus was initially detected in Mexico and the United States in late April, and it continued to spread in the Northern Hemisphere at low levels throughout the summer months. A sharp increase in influenza activity occurred early in September, and the peak of the fall wave of the pandemic was observed in mid-October, much earlier than is normally seen with epidemic strains (1). The unusual timing of the spread of pandemic H1N1 influenza virus through the temperate regions of the Northern Hemisphere led us to ask whether the transmission of this virus might differ from that of a seasonal strain in its sensitivity to relative humidity (RH) and temperature. We showed previously that, in the guinea pig model, aerosol transmission of influenza A/Panama/2007/1999 (H3N2) (Pan/99) virus is highly dependent on both of these environmental conditions, with a cold, dry environment (5°C and 20% or 35% RH) being the most favorable and either warm (30°C) or humid (80% RH) conditions being unfavorable for spread (5). To test the relative effects of humidity and temperature on the transmission of the pandemic H1N1 influenza virus, we set up a series of aerosol transmission experiments using the guinea pig model, in which we compared Pan/99 virus to the pandemic isolate influenza A/Netherlands/602/2009 (H1N1) (NL/09) under a number of different environmental conditions.
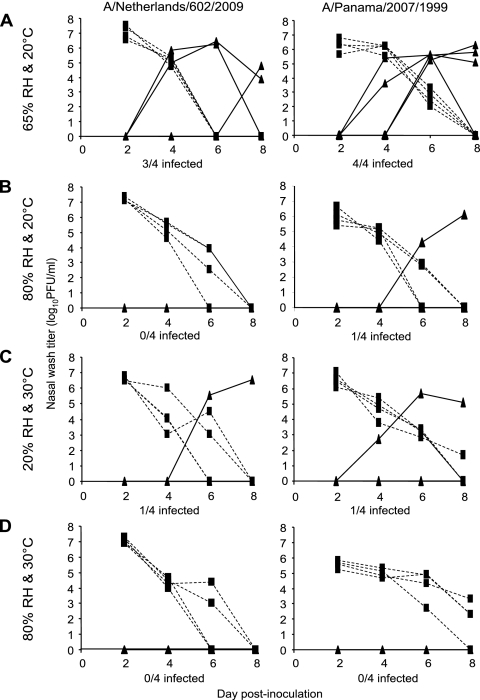
Aerosol transmission experiments were performed as described previously (5, 12), with Hartley strain guinea pigs (Charles River Laboratories) housed individually in open cages within an environmental test chamber (Caron model 6030). For each experiment, four animals were infected intranasally with 103 PFU of Pan/99 or NL/09 virus and, starting 24 h after inoculation, four naïve guinea pigs were exposed to the infected animals by being placed within the same environmental chamber. The use of two separate chambers allowed experiments with Pan/99 and NL/09 viruses to be performed in parallel. We have previously reported the transmission efficiencies of Pan/99 and NL/09 under the standard conditions that we routinely use for aerosol transmission experiments; at 20°C and 20% RH, both of these viruses spread to all four exposed animals (12). We now report the results obtained under four additional environmental conditions: 20°C and 65% RH, 20°C and 80% RH, 30°C and 20% RH, and 30°C and 80% RH. At 20°C and 65% RH, transmission of Pan/99 virus was seen previously to proceed with an efficiency ratio of 75% (5). In the present study, Pan/99 virus infection was contracted by all four exposed animals, while NL/09 virus spread to three-quarters of the exposed guinea pigs under the same conditions (Fig. 1A). Thus, good transmission of both viruses was observed at 20°C and 65% RH. When more humid conditions (80% RH) were tested at 20°C, NL/09 virus did not transmit, while Pan/99 virus spread to one of four exposed animals (Fig. 1B). When increased temperature was tested under dry conditions (30°C and 20% RH), transmission was again markedly reduced relative to that at 20°C and 20% RH, with one-quarter of the exposed guinea pigs becoming infected with each virus (Fig. 1C). Again, both the seasonal H3N2 and the pandemic H1N1 strain exhibited the same phenotype, although this result differed slightly from that reported previously for Pan/99 virus (6). Finally, at an elevated temperature and humidity (30°C and 80% RH), previously observed to block Pan/99 virus transmission, no transmission was observed with either the Pan/99 or NL/09 virus (Fig. 1D). Thus, overall, the aerosol transmission of pandemic strain NL/09 exhibited a sensitivity to humidity and temperature similar to that of the seasonal Pan/99 virus (Table 1).
FIG. 1.
NL/09 virus transmitted as an aerosol exhibits a sensitivity to RH and temperature similar to that of Pan/99 virus. Viral titers in nasal washes are plotted as a function of day postinoculation. Titers from inoculated animals are represented by dashed lines with squares, and titers from exposed animals are shown with solid lines and triangles. The environmental conditions under which each experiment was conducted are stated at the left, and the result in terms of number of exposed animals which contracted infection over the 7-day exposure period is indicated underneath each graph. Results obtained with the pandemic strain NL/09 virus are shown on the left, while results obtained with the seasonal strain Pan/99 virus are shown on the right. Experiments shown in panel B were performed at different times; experiments shown in panels A, C, and D were done in parallel.
TABLE 1.
Efficiency of aerosol transmission under various conditions of humidity and temperature
| RH (%) | Temp (°C) | Transmission efficiency (%) of influenza strain (reference)a: |
|||
|---|---|---|---|---|---|
| NL/09 | Pan/99 |
||||
| Replicate 1 | Replicate 2 | Replicate 3 | |||
| 20 | 20 | 100 (12) | 100 (12) | 100 (5) | 75 (5) |
| 65 | 20 | 75 | 100 | 75 (5) | 75 (5) |
| 80 | 20 | 0 | 25 | 0 (5) | 0 (5) |
| 20 | 30 | 25 | 25 | 0 (6) | ND |
| 80 | 30 | 0 | 0 | 0 (6) | ND |
Transmission efficiency is reported as a percentage of exposed animals that contracted infection, and references are given in parentheses for data reported in previous publications. ND, not done.
Our results suggest that the unusual seasonality exhibited to date by the swine origin pandemic virus is not due to an intrinsic property of this virus that would allow it to spread more efficiently at increased temperature or humidity. Instead, it seems likely that this virus was able to circulate among humans during the summer and early autumn months due to a relative lack of preexisting immunity in the population. Indeed, a spring wave of influenza activity has also been seen in previous pandemics (2-4, 11). The well-established susceptible-, infected-, recovered-population (SIR) epidemiological model dictates that the availability of susceptible hosts is a key factor in determining whether or not spread will occur in a population (8); our data suggest that humidity and temperature conditions also impact the effective transmissibility of influenza virus. Thus, perhaps in the absence of widespread immunity, the humidity and temperature requirements needed to achieve sustained transmission of influenza virus become less stringent.
Reanalysis of our previous data by other groups has been used to suggest that aerosol transmission of influenza virus shows a direct dependence on absolute humidity, rather than varying with both relative humidity and temperature (9, 10). While an inverse correlation between the log10 of specific humidity or vapor pressure (both of which are measures of absolute humidity) and transmission was found to be statistically significant, several outlying data points indicate that absolute humidity alone cannot account for our data. Of particular note is the high ratio of transmission seen among guinea pigs housed at 20°C and 65% RH: either 75% or 100% efficiency in four independent experiments (Table 1). If the transmission ratio were a simple logarithmic function of specific humidity, approximately 25% transmission would be expected. Thus, although the viability of influenza viruses in an aerosol is strongly correlated to specific humidity (9), it appears that the relationship between aerosol transmission and ambient humidity and temperature conditions may be more complex. Perhaps two or more mechanisms, including virion stability in an aerosol, are required to explain the observed effects of humidity and temperature on influenza virus transmission.
Acknowledgments
We thank the Centers for Disease Control and Prevention for providing the Pan/99 isolate and Ron Fouchier for providing the NL/09 virus.
This research was supported by the Center for Research on Influenza Pathogenesis (NIAID contract HHSN266200700010C) and the W. M. Keck Foundation (grant to P.P.). John Steel is supported by a Career Development Fellowship from the Northeast Biodefense Center (U54-AI057158-Lipkin).
Footnotes
Published ahead of print on 17 November 2010.
REFERENCES
- 1.Centers for Disease Control and Prevention. April-May 2010. FluView: a weekly influenza surveillance report prepared by the influenza division. Centers for Disease Control and Prevention, Atlanta, GA. http://www.cdc.gov/flu/weekly/. Accessed 25 September 2010.
- 2.Chowell, G., C. Viboud, L. Simonsen, M. A. Miller, and R. Acuna-Soto. 2010. Mortality patterns associated with the 1918 influenza pandemic in Mexico: evidence for a spring herald wave and lack of preexisting immunity in older populations. J. Infect. Dis. 202:567-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Housworth, J., and A. D. Langmuir. 1974. Excess mortality from epidemic influenza, 1957-1966. Am. J. Epidemiol. 100:40-48. [DOI] [PubMed] [Google Scholar]
- 4.Kilbourne, E. D. 2006. Influenza pandemics of the 20th century. Emerg. Infect. Dis. 12:9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lowen, A. C., S. Mubareka, J. Steel, and P. Palese. 2007. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog. 3:1470-1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lowen, A. C., J. Steel, S. Mubareka, and P. Palese. 2008. High temperature (30°C) blocks aerosol but not contact transmission of influenza virus. J. Virol. 82:5650-5652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nelson, M. I., and E. C. Holmes. 2007. The evolution of epidemic influenza. Nat. Rev. Genet. 8:196-205. [DOI] [PubMed] [Google Scholar]
- 8.Nokes, D. J., and R. M. Anderson. 1988. The use of mathematical models in the epidemiological study of infectious diseases and in the design of mass immunization programmes. Epidemiol. Infect. 101:1-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shaman, J., and M. Kohn. 2009. Absolute humidity modulates influenza survival, transmission, and seasonality. Proc. Natl. Acad. Sci. U. S. A. 106:3243-3248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shaman, J., V. E. Pitzer, C. Viboud, B. T. Grenfell, and M. Lipsitch. 2010. Absolute humidity and the seasonal onset of influenza in the continental United States. PLoS Biol. 8:e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steel, J., and P. Palese. 2008. The 1918 influenza pandemic: lessons from the past raise questions for the future, p. 272-286. In H. D. Klenk, M. N. Matrosovich, and J. Stech (ed.), Avian influenza, vol. 27. Karger, Basel, Switzerland. [Google Scholar]
- 12.Steel, J., et al. 2010. Transmission of pandemic H1N1 influenza virus and impact of prior exposure to seasonal strains or interferon treatment. J. Virol. 84:21-26. [DOI] [PMC free article] [PubMed] [Google Scholar]