Abstract
Rheumatoid arthritis (RA) is a chronic debilitating disease characterized by synovial inflammation, damage to cartilage and bone, and deformities of the joints. Several drugs possessing anti-inflammatory and immunomodulatory properties are being used in the conventional (allopathic) system of medicine to treat RA. However, the long-term use of these drugs is associated with harmful side effects. Therefore, newer drugs with low or no toxicity for the treatment of RA are actively being sought. Interestingly, several herbs demonstrate anti-inflammatory and anti-arthritic activity. In this review, we describe the role of the major biochemical and molecular mediators in the pathogenesis of RA, and highlight the sites of action of herbal medicinal products that have anti-arthritic activity. With the rapidly increasing use of CAM products by patients with RA and other inflammation-related disorders, our review presents timely information validating the scientific rationale for the use of natural therapeutic products.
Keywords: Complementary and alternative medicine (CAM), Herbal products, Inflammatory mediators, Rheumatoid arthritis (RA)
1. Introduction
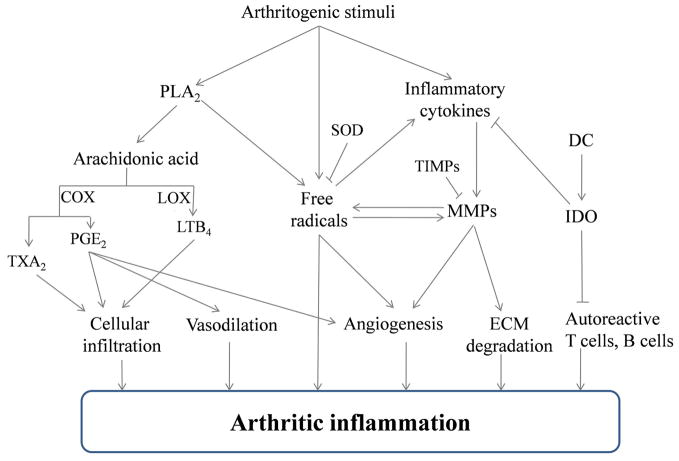
Rheumatoid arthritis (RA) is a chronic inflammatory disorder that mainly targets the joints 1. Both genetic and environmental factors are involved in the initiation and progression of the disease. Initiation of RA involves the activation of autoreactive T cells and the recruitment of these T cells along with other leukocytes into the joints. These leukocytes produce a variety of mediators of inflammation that induce synovial inflammation and eventually cause tissue damage in the joints (Fig. 1). Consequently, these mediators serve as potential targets for therapeutic agents for arthritis. The suppression of arthritis in experimental animal models using well-defined biochemical/pharmacological inhibitors has been reported 2, 3. Interestingly, many of these mediators also can be targeted by natural products, including herbal mixtures belonging to traditional or complementary and alternative medicine (CAM). In this review, we describe the role of various biochemical and molecular mediators of inflammation in the pathogenesis of RA (Table 1 and 2), as well as provide examples of plant medicinal products that target these mediators leading to the downmodulation of arthritis (Table 3–5).
Figure 1. Schematic representation of the initiation and propagation of autoimmune arthritis.
An arthritogenic stimulus (e.g., heat-killed M. tuberculosis H37Ra in adjuvant arthritis and Type II collagen in collagen-induced arthritis) initiates a series of pathogenic events that involve a variety of mediators of inflammation. Prominent among these mediators are arachidonic acid metabolites, pro-inflammatory cytokines, free radicals and matrix-degrading enzymes. These mediators modulate the processes relating to cellular migration into the joints as well as angiogenesis and degradation of the extracellular matrix within the joints leading to the arthritic inflammation. These mediators also are the targets of a variety of natural products. (COX- cyclooxygenase, LOX- lipooxygenase, TXA2- thromboxane A2, PGE2- prostaglandin E2, leukotriene B4 (LTB4), SOD- superoxide dismutase, MMP- matrix metalloprotease, TIMPS-tissue inhibitors of metalloproteases, ECM- extracellular matrix, DC- dendritic cells, and indoleamine 2,3-dioxygenase (IDO).)
Table 1.
Characteristics of the biochemical mediators of immune pathology in RA
| Enzyme | Isoforms | Substrate/Target | Product released/formed | Function | Reference |
|---|---|---|---|---|---|
| PLA2 | cPLA2, iPLA2, LpPLA2 and sPLA2 | Phospholipids containing arachidonic acid at sn-2 position | Arachidonic acid | Generation of precursor (arachidonic acid) for eicosanoid synthesis, release of free radicals | 28–30, 32, 33 |
| COX | COX-1 and COX-2 | Arachidonic acid | PGE2, TXA2 | Vasodilation, neutrophil infiltration, extracellular matrix degradation, angiogenesis, induction of pain and edema, platelet aggregation, smooth muscle contraction, endothelial cell migration | 43–45, 48 |
| LOX | 5-LOX, 12-LOX and15-LOX | Arachidonic acid | LTB4 | Leukocytes infiltration, expression of pathogenic TNF-α and IL-1β, activation of neutophils to release superoxides and MMPs | 50, 54 |
| MMPs | MMP-1, MMP-2, MMP-3, MMP-9, MMP-12, MMP-13 and MMP-14 | Collagen and proteoglycans | ------- | Degradation of cartilage and bone, osteoclast resorption, and angiogenesis | 68–70 |
| NOS | bNOS, ecNOS, iNOS | L-arginine | NO | Production of TNF-α, IL-1β, IFN-γ and MMPs | 93, 94 |
| IDO | ------- | Tryptophan | Kynurenine | Reduction in autoreactive T cells, and development of immune tolerance, induction of regulatory T cells, control of the accumulation of Th1 and Th17 pathogenic T cells | 100–103 |
The isoforms shown in bold font are the key enzymes in that group. bNOS- brain nitric oxide synthase, COX- cyclooxygenase, cPLA2- cytosolic phospolipase A2, ecNOS- endothelial cell nitric oxide synthase, IDO- indoleamine 2,3-dioxygenase, IL- interleukin, iNOS- inducible nitric oxide synthase, iPLA2- calcium independent phospolipase A2, LOX- lipooxgenase, LpPLA2- platelet activating factor acetyl hydrolase/oxidized lipid lipoprotein associated phospolipase A2, LTB4- leukotriene B4, MMPs- matrix metalloproteases, NO- nitric oxide, PGE2- prostaglandin E2, sPLA2- secreted phospolipase A2, TNF- tumor necrosis factor and TXA2- thromboxane A2.
Table 2.
Functions of the key molecular mediators associated with the pathogenesis of RA
| Molecular mediators | Function | Reference |
|---|---|---|
| Signaling molecules | ||
| ERK | Production of proinflammatory cytokines and MMPs, lymphocyte activation and differentiation | 117–119, 121, 122, 124, 125 |
| P38 | Release of proinflammatory cytokines, COX-2 and MMPs | 127, 128 |
| JNK | Expression of cytokines, growth factors, cell surface receptors, cell adhesion molecules and MMPs | 135 |
| Nuclear factors | ||
| NF-kB | Expression of cytokines (TNF-α, IL-1β, IL-6, IL-6, IL-17, IFN-γ, etc.), chemokines (MCP-1, MCP-4, CCL18, etc.), adhesion molecules (E-selectin, ICAM-1, VCAM-1, etc.), MMPs, VEGF, NOS and COX | 141 |
| AP-1 | Activation of cytokine production, T-cell differentiation, interaction with and trans-repression of the glucocorticoid receptor, and MMP expression | 149–151 |
COX- cyclooxygenase, ICAM- intracellular adhesion molecule, IFN- interferon, IL- interleukin, MCP- monocyte chemoattractant protein, MMPs- matrix metalloproteases, NOS- inducible nitric oxide synthase, TNF- tumor necrosis factor, VCAM- vascular cell adhesion molecule and VEGF- vascular endothelial growth factor.
Table 3.
Examples of herbs that target biochemical mediators of inflammation
| Herb | Origin | Active compound(s) | Reference |
|---|---|---|---|
| 1.1. Herbs targeting PLA2, COX-2, LOX, PGE2 and/or LTB4 | |||
| Allium cepa | Multiple | Quercetin | 6 |
| Aralia cordata | Korea | 7-oxosandaracopimaric acid | 164 |
| Boswellia serrata | India | Boswellic acid | 20, 165 |
| Camellia sinensis | China | Epigallocatechin-3-gallate | 166 |
| Curcuma longa | China/India | Curcumin | 10, 12 |
| Gentiana macrophylla | China | 19 | |
| Ocimum sanctum | India | Ursolic acid | 60 |
| Sinomenium acutum | China | Sinomenine | 167 |
| Tripterygium wilfordii | China | Triptolide, triptonide and celastrol | 8, 168, 169 |
| Turpinia arguta | China | Flavonoids | 7 |
| Vitis vinifera | Multiple | Resveratrol | 62, 170 |
| Zingiber officinale | China/India | Gingerol and Zingerone | 11 |
| 1.2. Herbs targeting MMPs and/or TIMPs | |||
| Achyranthes bidentata | China | Oleanolic acid | 171 |
| Camellia sinensis | China | Epigallocatechin-3-gallate | 13 |
| Cibotium barametz | Multiple | Cibotinoside, cyathenosin A | 172 |
| Magnolia officinalis | Asia | Magnolol | 173 |
| Ocimum sanctum | India | Ursolic acid | 4, 61 |
| Paeonia lactiflora | China | Paeoniflorin | 9 |
| Sinomenium acutum | China | Sinomenine | 174 |
| Triphala guggulu | India | Guggulsterone, Guggulsterol | 75 |
| 1.3. Herbs targeting NO, iNOS and/or SOD | |||
| Brassica sp. | Multiple | Indole-3-carbinol | 17 |
| Celastrus aculeatus | China | Celastrol | 18 |
| Cynodon dactylon | India | ----37 | 175 |
| Helenium microcephalum | Multiple | Bis(helenalinyl)glutarate | 176 |
| Sinomenium acutum | China | Sinomenine | 167 |
| Trewia polycarpa | India | -------- | 5 |
Herbs mentioned in bold font were studied in the adjuvant arthritis (AA) model. Active compound identified in each herbal extract is listed. Some of these compounds have been tested for their specific inhibitory activity.
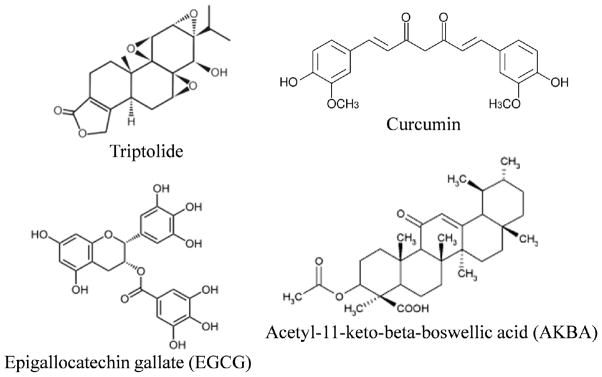
The natural plant products discussed in this article have been examined for their anti-inflammatory and anti-arthritic activity. The in vivo testing was performed using well-established experimental models of human RA (e.g., adjuvant-induced arthritis (AA) 4–7, collagen-induced arthritis (CIA) 8, 9 and streptococcal cell wall-induced arthritis 10–12), whereas the in vitro testing was based on cultures of defined cell types (e.g., macrophages, chondrocytes and fibroblasts) 13–16. For the in vivo studies, the plant products were tested either as an extract (e.g., water-extract and alcoholic extract) 5, 17–19 or as a purified bioactive compound (e.g., triptolide, curcumin, epigallocatechin-3-gallate (EGCG) and acetyl-11-keto-beta-boswellic acid (AKBA) 12, 13, 15, 20) (Fig. 2). Oral feeding and intraperitoneal injection represent the two major routes of administration employed for the in vivo testing. The readout for the efficacy of plant products in the arthritis models included assessment of the severity of arthritis using clinical criteria for grading or objective parameters such as paw volume, histopathological evaluation of tissue damage in the joints and bone mineral density 7, 9–12. For the in vitro models, specific compounds purified from the natural product were added to the cell culture in the presence of an inflammatory stimuli (e.g., interleukin-1 beta (IL-1β) and lipopolysaccharide; LPS) 15, 16. The cells tested were derived either from mice/rats (naïve or treated with the plant products) or from cell lines. The readouts of these cellular assays are comprised of various biochemical and molecular mediators of inflammation as discussed below in detail.
Figure 2. Chemical structures of four representative bioactive compounds isolated from natural plant extracts are shown.
Triptolide: a diterpene isolated from Tripterygium wilfordii, Curcumin: a polyphenol isolated from Curcuma longa, epigallocatechin-3-gallate (EGCG): a flavonoid from Camellia sinensis, and acetyl-11-keto-beta-boswellic acid (AKBA): an organic acid from Boswellia serrata. These natural compounds possess anti-inflammatory activity that can suppress autoimmune arthritis.
2. Biochemical mediators of inflammation and arthritis
Inflammation is physiological response of the organism to different stimuli such as trauma, infection or immune reactions 21. A variety of biochemical mediators act in concert to initiate and perpetuate the inflammatory reaction. We discuss below in detail the characteristics of these major biochemical mediators and also report the targeting of these mediators by synthetic and natural products leading to suppression of arthritis. The major biochemical mediators include phospholipase A2 (PLA2), cyclooxygenase (COX), lipoxgenase (LOX), matrix metalloproteases (MMPs), nitric oxide synthases (NOS), indoleamine 2,3-dioxygenase (IDO), tissue inhibitors of metalloproteases (TIMPs), prostaglandins (PG), leukotrienes (LT) and nitric oxide (NO). These mediators act via different interconnected pathways resulting in arthritic inflammation (Fig. 1). The functions of PLA2, COX, LOX, MMPs, NOS and IDO are summarized in Table 1.
2.1 Phospholipase A2 (PLA2)
PLA2 hydrolyzes the fatty acid from the sn-2 position of membrane phospholipids. Free fatty acids thus released can be metabolized to various lipid mediators of biological importance 22. The remaining lysophospholipids also serve important roles in biological processes 23, 24. There are more than 14 distinct groups of PLA2 enzymes 25, 26. Among the four main types of PLA2 are the secreted PLA2 (sPLA2), cytosolic PLA2 (cPLA2), calcium-independent PLA2 (iPLA2) and platelet activating factor (PAF) acetyl hydrolase/oxidized lipid lipoprotein-associated PLA2 (LpPLA2). cPLA2 is the predominant type synthesized at the site of inflammation 27 and it is the only PLA2 with a preference for arachidonic acid in the sn-2 position of phospholipids 28, 29. As arachidonic acid is the precursor of eicosanoids, cPLA2 represents the central enzyme involved in the generation of eicosanoids and hence, is the mediator of many inflammatory processes, including RA 30–33. In addition, cPLA2 upregulates nicotinamide adenine dinucleotide phosphate (NADPH) oxidase activity in neutrophils and monocytes, releasing superoxides during the inflammatory process 27, 34. sPLA2 can hydrolyze different fatty acids at the sn-2 position of the substrate phospholipid 35. Further, the role of the mammalian sPLA2 in eicosanoid generation is not clear. Different studies on this subject have yielded inconclusive results, and clinical trials of the efficacy of sPLA2 against arthritis and allergies revealed no significant therapeutic effects 36, 37.
2.2 Cyclooxygenase (COX) and prostaglandins (PG)
COX converts arachidonic acid into prostaglandin H2 (PGH2), which is further catalyzed by distinct synthases to 5 major bioactive prostaglandins (PGE2, PGI2, PGF2, PGD2, and thromboxane A2 (TXA2)) 38. There are two isoforms of COX that are designated as COX-1 and COX-2. COX-1 is constitutively expressed in most tissues, whereas COX-2 is induced by a range of mitogenic and inflammatory stimuli. Prostaglandin synthesis in inflammatory conditions is attributable largely to COX-2. However, COX-1 also is associated with the generation of proinflammatory prostaglandins 39. PGE2 and TXA2 are potent inflammatory mediators that contribute to the pathogenesis of RA 40–42. PGE2 causes vasodilatation and recruits neutrophils to the affected joints in RA. The latter effect is attributable both to the production of IL-23-induced IL-17 and the impaired production of IL-12 and IFN-γ production 43. Moreover, PGE2 mediates matrix degradation and cartilage destruction 44. PGE2 also plays a role in angiogenesis evoked by inflammation by stimulating the production of vascular endothelial growth factor (VEGF) 45. Moreover, PGE2 contributes to inflammatory pain by sensitizing to bradykinin as well as histamine-induced nociceptive stimuli, and to edema via plasma extravasation. In addition, the effects of IL-1, IL-6 and TNF-α on bone resorption have been shown to be PGE2 dependent 46. TXA2, the other product of COX, induces rapid irreversible aggregation of human platelets and it is a potent inducer of smooth muscle contraction 47. TXA2 also is a mediator of endothelial cell migration as well as angiogenesis 48. The role of inhibition of COX in inhibiting inflammation and arthritis is discussed below.
2.3 Lipoxgenase (LOX) and leukotrienes (LT)
LOX constitutes a group of non-heme iron-containing dioxygenases. So far, 5-LOX, 12-LOX, and 15-LOX have been identified, which stereospecifically integrate oxygen at carbon atom 5, 12 or 15, respectively of the substrate fatty acid 49. 5-LO catalyzes the synthesis of leukotriene B4 (LTB4) from arachidonic acid, and it is known to play an important role in the pathogenesis of RA 50. In contrast, 12- and 15-LOX represent major anti-inflammatory enzymes operative during the course of inflammatory joint disease 51. LTB4 is a chemoattractant and mediates the infiltration of leukocytes into the RA joint 50. There, these cells proliferate and form an invasive pannus, which leads to cartilage and bone destruction 52. Recent reports suggest that LTB4 increases the production of pathogenic TNF-α and IL-1β at both the mRNA and the protein level 53 LTB4 not only serves as a chemoattractant, but also activates neutrophils to release superoxides and proteolytic enzymes, which in turn cause matrix destruction 54. The release of inflammatory lipid mediators, particularly PGE2, TXA2 and LTB4 is regulated by a cascade of reactions starting from PLA2. Table 1 depicts the functions of PLA2, COX and LOX.
Selective inhibitors of LOX or COX display suppressive effect against inflammation in the joint 55, 56. However, dual inhibitors of LOX and COX are more effective than selective single-enzyme inhibitors in preventing arthritis in experimental models 57, 58. In comparison, the inhibition of over-expressed cPLA2 should simultaneously diminish the activity of multiple lipid mediators that facilitate the recruitment of neutrophils to the site of inflammation and the release of superoxides 27, 59.
Plant extracts and purified compounds derived from them can selectively inhibit COX, LOX or PLA2 and suppress arthritis (Table 3). For example, Bidens pilosa extract inhibits IL-1β-induced COX-2 expression and PGE2 production, and this effect is attributable to inhibition of mitogen activated protein kinase (MAPK), particularly p38 16. Similarly, total flavonoids derived from Turpinia Arguta reduce the production of IL-1β and PGE2 by peritoneal macrophages, and this effect correlates with their anti-arthritic activity observed in rats 7. A curcuminoid-containing turmeric extract that inhibits experimental arthritis in rats also inhibits the expression of COX-2 and reduces PGE2 levels in the joints in part via preventing the activation of nuclear factor-kB (NF-kB) 10. Another study highlights the anti-inflammatory activity of an extract of Gentiana macrophylla (Gentianaceae) in an experimental arthritis model, and that activity is associated with reduced PGE2 levels in the inflamed tissues 19. Ursolic acid inhibits sPLA2 60 and downregulates lipooxygenase and COX-2 owing to the inhibition of NF-kB activity 61. Resveratol, a phytoalexin, is a potent inhibitor of COX-2 production 62 as are Celastrol (from plants of Celastraceae family) 63 and Withanolides from Withania somnifera (Ashwagandha) 64. Similarly, phenolic gingerols from Zinziber officinale suppress COX-1 and COX-2 activity 11. A mechanism common to several of the herbal products described above involves inhibition of NF-kB activity, which in turn suppresses the activity of COX and other inflammation-related biomolecules.
2.4 Matrix metalloproteases (MMPs) and tissue inhibitors of metalloproteinases (TIMPs)
In arthritic conditions, inflammatory cytokines such as IL-1β and TNF-α stimulate the production of MMPs, enzymes that can irreversibly degrade components of extracellular matrix (ECM), including the articular cartilage and bone 65–67. Cartilage is made up of proteoglycans and type II collagen, while bone is composed primarily of type I collagen. The degradation of collagen by MMPs is the rate-limiting step in cartilage and bone damage. MMP-1 is produced primarily by the synovial cells that line the joints, while MMP-13 is a product of the chondrocytes that reside in the cartilage. MMP-13 degrades collagen as well as the proteoglycan molecule, aggrecan. The expression of other MMPs such as MMP-2, MMP-3, MMP-9, MMP-12, and MMP-14 is also elevated in arthritis 68. These enzymes degrade non-collagenous protein components of the matrix resulting in complete joint destruction. In addition, they play a critical role in angiogenesis 69, 70, which is one of the vital components of the pathogenic process in inflammatory arthritis. Summary of the functions of MMPs are given in Table 1. Inhibiting the activities of pathogenic MMPs can prevent or significantly reduce joint destruction, thereby benefiting arthritis patients with an improved quality of life. TIMPS 1–4 are the natural inhibitors of MMPs, and they also inhibit proinflammatory cytokines and tissue damage in the joint 71, 72. Significant effort has been invested in designing effective inhibitors of MMP activity and/or synthesis 73 that display anti-arthritic activity in experimental animal models 74. Moreover, a number of MMP inhibitors derived from herbal products have been shown to suppress arthritis (Table 3). For example, the anti-arthritic activity of total glucosides of paeony (TGP), a TCM product, in rats is attributable in part to the inhibition of the production of IL-1β and TNF-α by macrophage-like synoviocytes, and that of MMP-1 and MMP-3 by the fibroblast-like synoviocytes 9. Furthermore, this concurrent inhibition of different mediators of inflammation can be explained by the fact that IL-1β and TNF-α regulate the expression of MMP-1 and MMP-3. Similarly, in another study, Triphala guggulu, an Ayurvedic medicine, is shown to inhibit certain key enzymes involved in tissue damage in arthritis, including hyaluronidase, collagenase and MMPs 75. Ursolic acid suppresses the expression of MMP-9 61, one of the NF-kB-regulated genes. Celastrol (from Celastraceae family plants) 63, Ikarisoside (from Epimedium koreanum) 14, and AKBA (from Boswellia serrata, an Ayurvedic medicine) 20 inhibit the activity of MMP9, whereas green tea inhibits MMP1 and 13 13.
2.5 Free radicals
Free radicals are continually generated within metabolically active cells of aerobic organisms and they utilize molecular oxygen (dioxygen or O2). The major reactive oxygen species (ROS) generated are the superoxide anion radical (dioxide or O2−), the hydroxyl radical (OH) and the peroxynitrite anion (ONOO−). Free radicals are highly reactive 76 and they can be quite toxic and cause cellular dysfunction and even cell death 77. The harmful effects of free radicals are owing to their tendency to interact with and to damage macromolecules such as DNA, proteins, carbohydrates and lipids 77. Oxygen radical generation is relatively high in the RA joint 78, 79. In regard to RA pathogenesis, the effects of free radicals on connective tissue macromolecules (collagen, hyaluronic acid (HA), proteoglcans), intact tissues and immunoglobulins are of high relevance 80. The free radicals generated by polymorphonuclear cells (PMNs) alter IgG, which could in turn activate PMNs to generate additional superoxides 81. Free radicals themselves also activate PMNs 82. ROS might also perpetuate inflammation by facilitating the generation of chemotactic factors at the local site. Superoxide dismutase (SOD) is a ubiquitously distributed anti-oxidative enzyme that affords protection against free radical damage. In addition, anti-oxidants can scavenge the free radicals and limit damage. NO is a free radical that serves as an important messenger molecule in inflammatory conditions 83. The role of NO in the pathogenesis of RA is discussed below.
NO is synthesized from the guanidino group of L-arginine by a family of enzymes termed NO synthases (NOS), and this process involves the incorporation of molecular oxygen into L-arginine. Inducible macrophage type NOS (iNOS), endothelial cell NOS (ecNOS) and brain NOS (bNOS), represent different isoforms of NOS 84–86. A variety of immunological stimuli including pro-inflammatory cytokines induce the expression of iNOS in a number of non-hematopoietic cells, including fibroblasts 87. The induction of iNOS may have either a toxic or a protective effect 88–91. In arthritis, NO induces the production of pathogenic cytokines such as TNF-α, IL-1β and IFN-γ, as well as collagenase 92–96. NO also induces certain chemokines that contribute to the disease progression in arthritis. The functions of NOS are summarized in Table 1. Decreased production of NO via suppressing or inhibiting NOS reduces arthritic symptoms and affords protection against the loss of body weight 17, 97. Anti-oxidants that are present in a number of plant extracts scavenge NO and other free radicals. Plant-derived compounds also can suppress iNOS and increase SOD activity. Examples of herbal preparations and compounds isolated from them that can scavenge NO, suppress iNOS or increase SOD are given in Table 3. For example, oral feeding to rats of Quercetin, a flavonoid, ameliorates adjuvant arthritis (AA), and this effect is associated with reduced production of various mediators of inflammation, including NO by macrophages 6. In another study based on the AA model, treatment with Trewia polycarpa, an Ayurvedic medicine, revealed its free radical-scavenging property 5. The treatment led to an increase in the activity of SOD and glutathione peroxidase but a reduction in the level of lipid peroxide. Celastrus aculeatus Merr. (Celastrus) has anti-inflammatory and anti-arthritic activity as tested in the AA model 18. Celastrus-treated rats show a significant reduction in the levels of NO both in serum as well as in culture supernate of antigen-stimulated draining lymph node cells (LNC) 18. In another study, Celastrol, an active component of Celastrus and other Celastraceae family of plants, has been shown to modulate the expression of iNOS 63.
2.6 Indoleamine 2,3-dioxygenase (IDO)
Tryptophan is an essential amino acid that is critical for cell survival and proliferation98, 99. It can be catabolized by IDO yielding kynurenine, which can induce apoptosis of T cells. Furthermore, IDO-mediated deprivation of tryptophan inhibits T cell proliferation. IDO is expressed in dendritic cells (DC) and activated macrophages but not in T cells. IDO-positive DC play an important role in the induction and maintenance of peripheral tolerance via the depletion of self-reactive T cells 100 and the generation/activation of regulatory T cells 101, 102. It has been shown in the CIA model that the induction of IDO significantly reduces both the accumulation of pathogenic Th1 and Th17 cells in the arthritic joints 103 and the severity of the disease 104. However, it has also been reported that inhibiting IDO activity might attenuate rather than aggravate arthritis 105. The activity of IDO can be modulated by IFN-γ 106 as well as CD4+CD25+ regulatory T cells (Treg) 101. Furthermore, the cytoplasmic enzyme tryptophanyl-tRNA-synthetase (TTS) mediates the association of tryptophan with its specific tRNA 107, and this accumulation of tryptophan can antagonize the IDO-mediated deprivation of tryptophan 108, 109. It has been reported that autoreactive T cells in the rheumatoid joints resist IDO-mediated inhibition and persist during disease progression 110. This effect might be because of the enhanced expression of TTS in T cells by inflammatory cytokines such as IFN-γ and TNF-α 110. The role of IDO in the pathogenesis of RA is illustrated in Fig. 1. As of now, herbal preparations have not been studied much for their ability to modulate arthritis via altering IDO activity.
3. Molecular mediators of inflammation and arthritis
The initiation and progression of arthritic inflammation requires transduction of signals from the arthritogenic stimuli. Defined ligands bind to the appropriate receptors on the target cells, initiating a chain of reactions, including the activation of transcription factors. The generation of a variety of mediators (e.g., cytokines, chemokines, MMPs and other enzymes) of inflammation and tissue damage in RA are controlled at the transcriptional level 111. Hence, cell signaling pathways and transcription factors are important components of the effector pathways leading to arthritis. The roles of major signaling molecules and transcription factors are summarized in Table 2 and discussed below.
3.1 Cell signaling pathways
Mitogen-activated protein (MAP) kinases are central components of signal transduction pathways leading to the enhanced expression of mediators of inflammation that play a key role in the pathophysiology of RA and other inflammatory diseases 112, 113. Consequently, members of the MAP kinase pathways are potential therapeutic targets in RA. MAP kinases are proline-directed serine/threonine protein kinases. Nuclear translocation of activated MAP kinases facilitates the modulation of gene transcription via the induction and/or transactivation of transcription factors 114, 115. The 3 major mammalian MAP kinase pathways include the ERK pathway, the JNK/SAPK pathway, and the p38 pathway. The kinases in each pathway have multiple isoforms that may be differentially expressed in various tissues and play different roles. Summary of the functions of these pathways are given in Table 2 and discussed below.
3.1.1 Extracellular-signal-regulated kinase (ERK) pathway
The ERK pathway is activated by the MAP kinase kinases (also known as MAP kinase/ERK kinases (MEKs)). MEKs phosphorylate critical tyrosine and threonine residues of ERK 116. MEK/ERK pathway plays an important role in lymphocyte activation and differentiation 117–119, in the production of pro-inflammatory cytokines, such as IL-1β, TNF-α, and IL-6 120–123, in the production of MMPs 124, 125, and in the development of synovitis, pain, and tissue destruction in RA. Accordingly, MEK inhibitors are being exploited to inhibit diverse inflammatory pathways. For example, a selective MEK inhibitor demonstrates anti-arthritic activity 126. In this regard, medicinal plants being used in CAM might be an invaluable resource for novel MEK/ERK inhibitors. Examples of the herbs that target ERK are shown in Table 4.
Table 4.
Examples of herbs targeting molecular mediators of inflammation
| Herb | Origin | Active compound(s) | Reference |
|---|---|---|---|
| 2.1. Herbs targeting cell signaling molecules (ERK, p38 MAP kinase and/or JNK) | |||
| Aralia cordata | Korea | 7-oxosandaracopimaric acid | 164 |
| Bidens pilosa | Taiwan | Phenylheptatriyne, linolic acid and linolenic acid | 16 |
| Curcuma longa | China/India | Curcumin | 177 |
| Epimedium koreanum | Korea | Ikarisoside A | 14 |
| Tanacetum parthenium | Europe | Parthenolide | 178 |
| Zingerber officinale | China/India | Zingerone | 140 |
| 2.2. Herbs targeting nuclear factors (NF-kB and/or AP-1) | |||
| Aralia cordata | Oriental region | 7-oxosandaracopimaric acid | 164 |
| Commiphora mukul | India | Guggulsterone, cembranoids | 61 |
| Dictamnus dasycarpus | Korea | Dictamnine, obacunone and fraxinellone | 179 |
| Epimedium koreanum | Korea | Ikarisoside A | 14 |
| Magnolia officinalis | Asia | Magnolol | 173 |
| Sinomenium acutum | China | Sinomenine | 167 |
| Tripterygium wilfordii | China | Triptolide, triptonide and celastrol | 15, 63, 180 |
| Withania somnifera | India | Withanolides | 64 |
Herbs mentioned in bold font were studied in the adjuvant arthritis (AA) model. Active compound identified in each herbal extract is listed. Some of these compounds have been tested for their specific inhibitory activity.
3.1.2 P38 MAP kinase pathway
The p38 MAP kinase has many isoforms (p38α, β, γ and δ), and p38α is believed to be a critical regulator of the inflammatory response, including the release of cytokines by immune competent cells and the functional response of neutrophils to inflammatory stimuli 127, 128. p38 MAP kinase phosphorylates several transcription factors, including signal transducer and activator of transcription (STAT), nuclear factor of activated T cells (NFAT), and downstream kinases 129. In addition, it regulates a variety of genes involved in inflammation, such as TNF-α, IL-1β, IL-6, IL-8, COX-2, and MMPs 128. The p38 pathway also mediates cellular functions, including cell migration, cell survival and cell death 130–132. Inhibition of p38 MAPK suppresses paw swelling, joint damage and the production of inflammatory cytokines 133, 134. The herbal extracts that target p38 MAP kinase in experimental models of arthritis are shown in Table 4. For example, Bidens pilosa (BP) extract has been shown to possess anti-inflammatory activity 16. One of the molecular mediators targeted here is MAPK. The phoshorylation of MAPK is inhibited by BP, with a predominant effect on p38.
3.1.3 c-Jun N-terminal kinase (JNK) pathway
JNKs phosphorylate and activate transcription factors and other cellular factors which regulate the expression of many genes encoding cytokines (TNF-α, IL-2), growth factors, cell surface receptors, cell adhesion molecules (E-selectin) and degradative enzymes (MMPs) 135. Activated JNK can be detected in synovial fibroblasts and chondrocytes from the joints of arthritic patients but not from normal controls, and it has been implicated in chondrocyte injury and cartilage degeneration 136, 137. Furthermore, the disease-suppressive effect of a JNK inhibitor in an animal model of arthritis has been reported 138. Inhibitors of JNK can be found in a certain Chinese herbs that are used in CAM for the treatment of several inflammatory disorders including RA 139 (Table 4). For example, Ikarisoside, a purified compound from Epimedium koreanum, has inhibitory effects on JNK and Akt (besides NF-kB) when tested for its effects on osteoclastogenesis using monocyte/macrophage RAW 267.7 cells 14. The molecules targeted here are involved in abnormal bone lysis in RA. In another study, 6-dehydrogingerdione, a compound purified from ginger, was shown to enhance the activity of JNK without much effect on ERK and p38, resulting in the induction of apoptosis in the target cells 140.
3.2 Transcription factors
3.2.1 Nuclear factor-kB (NF-kB)
The transcription factor NF-kB regulates the expression of a wide variety of genes. RelA, RelB, c-Rel, NF-kB1 and NF-kB2 are members of NF-kB family. These members activate characteristic sets of genes in a cell-type and stimulus-type manner, thus regulating the transcription of genes 141–145. NF-kB remains in an inactive form by binding to the inhibitor of NF-kB proteins (IkB), but cellular stimuli including cytokines, mitogens and stress activate IkB via activating NF-kB kinase (IkB kinase (IKK) complex) and subsequent degradation of IkB 146, 147. The activated NF-kB translocates to the nucleus and stimulates the transcription of genes containing the consensus kB sequence 5′-GGGPuNNPyPyCC-3′ (where Pu denotes a purine and Py denotes a pyrimidine). Such genes include those encoding certain cytokines and chemokines, adhesion molecules, MMPs, VEGF, iNOS, COX-2, etc. Most of these genes have been reported to have important role in the pathogenesis of RA 141. VEGF as well as a few other molecules involved in angiogenesis are attractive targets for therapeutic agents against RA 148.
3.2.2 Activator protein-1 (AP-1)
AP-1 is another transcription factor that transduces extracellular signals in immune cells. AP-1 gets activated in response to a variety of inflammatory stimuli. Activated AP-1 interacts with the binding site(s) in their promoter/enhancer regions resulting in the expression of specific target genes enciding MMPs and pro-inflammatory cytokines 149–151. AP-1-mediated cytokine production is in cooperation with transcription factors of the nuclear factor of activated T cells (NFAT) family 152, wherein AP-1 and NFAT form stable ternary complexes on DNA-binding sites. AP-1-mediated activation of NFAT and integration of the signals via the receptor activator for nuclear factor kB ligand (RANKL) and macrophage colony-stimulating factor (M-CSF) are required for osteoclast differentiation 153. AP-1 also regulates the differentiation of naïve T cells into T helper 1 (Th1) or T helper 2 cells (Th2), and it interacts with and trans-represses the glucocorticoid receptor 154, 155. All these mechanisms affect the severity of arthritic inflammation.
3.2.3 Other transcription factors
Signal transducer and activator of transcription (STAT) family of proteins, interferon regulatory factors (IRFs), forkhead (Fox) family proteins, T-box transcription factor 21 (TBX21)/T-box expressed in T cells (T-bet), the (cytidine-cytidine-adenosine-adenosine-thymidine) CCAAT-enhancer binding protein family and the E-twenty six (Ets) transcription factor family represent other transcription factors implicated in the pathogenesis of RA 156. Furthermore, single nucleotide polymorphisms in the Runt-related transcription factor 1 (Runx1)-binding site of the SLC22A4 gene, the major histocompatibility complex class II transactivator (CIITA) gene, and the STAT4 gene are associated with RA 157–160. Modulation of the synthesis and/activity of transcription factors represents an alternative therapeutic strategy for RA. Specific inhibitors for NF-kB and NFAT have already been reported 161–163. However, the inhibition of such transcription factors that regulate a variety of pathways might induce unexpected side effects in vivo.
Numerous examples of herbs that target NF-kB and other transcription factors are shown in Table 4. For example, the anti-arthritic activity of a turmeric extract containing curcuminoid as an active ingredient, was associated with a reduction in the local activation of NF-kB and thereby modulation of the expression of various inflammation-related genes controlled by NF-kB 10. Similarly, a component of Epimedium koreanum, Ikarisoside, has an inhibitory effect on NF-kB signaling pathways, which in turn influences the osteoclastogenic activity associated with arthritis 14. Using an in vitro model of inflammation, triptolide, a bioactive compound isolated from Tripterygium wilfordii, was shown to inhibit NF-kB-regulated reporter transcription in LPS-stimulated macrophages 15. Celastrol has been shown to modulate both inducible as well as constitutive NF-kB activity 63. Specifically, Celastrol inhibits the TNF-α-induced activation, phosphorylation and degradation of IkBα; nuclear transport and phosphorylation of p65; and TAK-1-induced NF-kB activation 63. Similar effects on NF-kB were observed with withanolides isolated from Withania somnifera, an Ayurvedic medicine 64. Ursolic acid inhibits both the DNA binding of NF-kB and the IkBα kinase activity, as well as phosphorylation and nuclear transport of p65 61. Resveratol is a potent inhibitor of NF-kB activation 62, and AKBA was shown to inhibit NF-kB-regulated gene expression induced by IL-1β, TNF-α or LPS, but the binding of NF-kB to DNA was unaffected 20. However, AKBA inhibits the activation of IkBα kinase (IKK) and the phosphorylation, ubiquitination and degradation of IkBα, as well as phosphorylation and nuclear transport of p65 20. The effect of AKBA on IkBα is mediated through inhibition of Akt. EGCG showed a dose-dependent inhibition of NF-kB and AP-1, providing insights into the anti-inflammatory effects of this flavonoid 13.
4. Concluding remarks
It is clear from the above description that herbal medicinal products target specific defined mediators of inflammation and arthritis. The major benefit of using herbs and other natural products lies in their limited or no undesirable side effects. Therefore, the interdisciplinary efforts of researchers aimed at identifying new herbal products and defining their mechanisms of action should be reinforced. This would facilitate the discovery and development of safe and effective natural products for the treatment of RA and other immune-mediated disorders.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Choi Y, Arron JR, Townsend MJ. Nat Rev Rheumatol. 2009;5:543. doi: 10.1038/nrrheum.2009.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khanna D, Sethi G, Ahn KS, Pandey MK, Kunnumakkara AB, Sung B, Aggarwal A, Aggarwal BB. Curr Opin Pharmacol. 2007;7:344. doi: 10.1016/j.coph.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 3.Manning AM, Davis RJ. Nat Rev Drug Discov. 2003;2:554. doi: 10.1038/nrd1132. [DOI] [PubMed] [Google Scholar]
- 4.Ahmad SF, Khan B, Bani S, Suri KA, Satti NK, Qazi GN. Pharmacol Res. 2006;53:233. doi: 10.1016/j.phrs.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 5.Chamundeeswari D, Vasantha J, Gopalakrishnan S, Sukumar E. J Ethnopharmacol. 2003;88:51. doi: 10.1016/s0378-8741(03)00143-0. [DOI] [PubMed] [Google Scholar]
- 6.Mamani-Matsuda M, Kauss T, Al-Kharrat A, Rambert J, Fawaz F, Thiolat D, Moynet D, Coves S, Malvy D, Mossalayi MD. Biochem Pharmacol. 2006;72:1304. doi: 10.1016/j.bcp.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 7.Zhang L, Li J, Yu SC, Jin Y, Lv XW, Zou YH, Li Y. J Ethnopharmacol. 2008;116:167. doi: 10.1016/j.jep.2007.11.027. [DOI] [PubMed] [Google Scholar]
- 8.Wang Y, Jia L, Wu CY. Scand J Immunol. 2008;68:383. doi: 10.1111/j.1365-3083.2008.02147.x. [DOI] [PubMed] [Google Scholar]
- 9.Zhu L, Wei W, Zheng YQ, Jia XY. Inflamm Res. 2005;54:211. doi: 10.1007/s00011-005-1345-x. [DOI] [PubMed] [Google Scholar]
- 10.Funk JL, Frye JB, Oyarzo JN, Kuscuoglu N, Wilson J, McCaffrey G, Stafford G, Chen G, Lantz RC, Jolad SD, Solyom AM, Kiela PR, Timmermann BN. Arthritis Rheum. 2006;54:3452. doi: 10.1002/art.22180. [DOI] [PubMed] [Google Scholar]
- 11.Funk JL, Frye JB, Oyarzo JN, Timmermann BN. J Nat Prod. 2009;72:403. doi: 10.1021/np8006183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Funk JL, Oyarzo JN, Frye JB, Chen G, Lantz RC, Jolad SD, Solyom AM, Timmermann BN. J Nat Prod. 2006;69:351. doi: 10.1021/np050327j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahmed S, Wang N, Lalonde M, Goldberg VM, Haqqi TM. J Pharmacol Exp Ther. 2004;308:767. doi: 10.1124/jpet.103.059220. [DOI] [PubMed] [Google Scholar]
- 14.Choi HJ, Park YR, Nepal M, Choi BY, Cho NP, Choi SH, Heo SR, Kim HS, Yang MS, Soh Y. Eur J Pharmacol. 2010;636:28. doi: 10.1016/j.ejphar.2010.03.023. [DOI] [PubMed] [Google Scholar]
- 15.Matta R, Wang X, Ge H, Ray W, Nelin LD, Liu Y. Am J Transl Res. 2009;1:267. [PMC free article] [PubMed] [Google Scholar]
- 16.Yoshida N, Kanekura T, Higashi Y, Kanzaki T. J Dermatol. 2006;33:676. doi: 10.1111/j.1346-8138.2006.00158.x. [DOI] [PubMed] [Google Scholar]
- 17.Rostoka E, Baumane L, Isajevs S, Line A, Dzintare M, Svirina D, Sharipova J, Silina K, Kalvinsh I, Sjakste N. Basic Clin Pharmacol Toxicol. 2010;106:461. doi: 10.1111/j.1742-7843.2009.00526.x. [DOI] [PubMed] [Google Scholar]
- 18.Tong L, Moudgil KD. Arthritis Res Ther. 2007;9:R70. doi: 10.1186/ar2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yu F, Yu F, Li R, Wang R. J Ethnopharmacol. 2004;95:77. doi: 10.1016/j.jep.2004.06.025. [DOI] [PubMed] [Google Scholar]
- 20.Takada Y, Ichikawa H, Badmaev V, Aggarwal BB. J Immunol. 2006;176:3127. doi: 10.4049/jimmunol.176.5.3127. [DOI] [PubMed] [Google Scholar]
- 21.Henrotin Y, de Leval X, Mathy-Hartet M, Mouithys-Mickalad A, Deby-Dupont G, Dogne JM, Delarge J, Reginster JY. Inflamm Res. 2001;50:391. doi: 10.1007/PL00000261. [DOI] [PubMed] [Google Scholar]
- 22.Funk CD. Science. 2001;294:1871. doi: 10.1126/science.294.5548.1871. [DOI] [PubMed] [Google Scholar]
- 23.Rivera R, Chun J. Rev Physiol Biochem Pharmacol. 2008;160:25. doi: 10.1007/112_0507. [DOI] [PubMed] [Google Scholar]
- 24.Xu Y, Xiao YJ, Zhu K, Baudhuin LM, Lu J, Hong G, Kim KS, Cristina KL, Song L, Elson FSWP, Markman M, Belinson J. Curr Drug Targets Immune Endocr Metabol Disord. 2003;3:23. [PubMed] [Google Scholar]
- 25.Burke JE, Dennis EA. J Lipid Res. 2009;50 (Suppl):S237. doi: 10.1194/jlr.R800033-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schaloske RH, Dennis EA. Biochim Biophys Acta. 2006;1761:1246. doi: 10.1016/j.bbalip.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 27.Raichel L, Berger S, Hadad N, Kachko L, Karter M, Szaingurten-Solodkin I, Williams RO, Feldmann M, Levy R. Eur J Immunol. 2008;38:2905. doi: 10.1002/eji.200838545. [DOI] [PubMed] [Google Scholar]
- 28.Clark JD, Lin LL, Kriz RW, Ramesha CS, Sultzman LA, Lin AY, Milona N, Knopf JL. Cell. 1991;65:1043. doi: 10.1016/0092-8674(91)90556-e. [DOI] [PubMed] [Google Scholar]
- 29.Ghosh M, Tucker DE, Burchett SA, Leslie CC. Prog Lipid Res. 2006;45:487. doi: 10.1016/j.plipres.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 30.Bonventre JV, Huang Z, Taheri MR, O'Leary E, Li E, Moskowitz MA, Sapirstein A. Nature. 1997;390:622. doi: 10.1038/37635. [DOI] [PubMed] [Google Scholar]
- 31.Niknami M, Patel M, Witting PK, Dong Q. Int J Biochem Cell Biol. 2009;41:994. doi: 10.1016/j.biocel.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 32.Uozumi N, Kume K, Nagase T, Nakatani N, Ishii S, Tashiro F, Komagata Y, Maki K, Ikuta K, Ouchi Y, Miyazaki J, Shimizu T. Nature. 1997;390:618. doi: 10.1038/37622. [DOI] [PubMed] [Google Scholar]
- 33.Uozumi N, Shimizu T. Prostaglandins Other Lipid Mediat. 2002;68–69:59. doi: 10.1016/s0090-6980(02)00021-7. [DOI] [PubMed] [Google Scholar]
- 34.Riesenberg K, Levy R, Katz A, Galkop S, Schlaeffer F. Eur J Clin Invest. 1997;27:398. doi: 10.1046/j.1365-2362.1997.1270667.x. [DOI] [PubMed] [Google Scholar]
- 35.Singer AG, Ghomashchi F, Le Calvez C, Bollinger J, Bezzine S, Rouault M, Sadilek M, Nguyen E, Lazdunski M, Lambeau G, Gelb MH. J Biol Chem. 2002;277:48535. doi: 10.1074/jbc.M205855200. [DOI] [PubMed] [Google Scholar]
- 36.Lambeau G, Gelb MH. Annu Rev Biochem. 2008;77:495. doi: 10.1146/annurev.biochem.76.062405.154007. [DOI] [PubMed] [Google Scholar]
- 37.Schevitz RW, Bach NJ, Carlson DG, Chirgadze NY, Clawson DK, Dillard RD, Draheim SE, Hartley LW, Jones ND, Mihelich ED, et al. Nat Struct Biol. 1995;2:458. doi: 10.1038/nsb0695-458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Narumiya S, Sugimoto Y, Ushikubi F. Physiol Rev. 1999;79:1193. doi: 10.1152/physrev.1999.79.4.1193. [DOI] [PubMed] [Google Scholar]
- 39.Chen M, Boilard E, Nigrovic PA, Clark P, Xu D, Fitzgerald GA, Audoly LP, Lee DM. Arthritis Rheum. 2008;58:1354. doi: 10.1002/art.23453. [DOI] [PubMed] [Google Scholar]
- 40.Honda T, Segi-Nishida E, Miyachi Y, Narumiya S. J Exp Med. 2006;203:325. doi: 10.1084/jem.20051310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Trebino CE, Stock JL, Gibbons CP, Naiman BM, Wachtmann TS, Umland JP, Pandher K, Lapointe JM, Saha S, Roach ML, Carter D, Thomas NA, Durtschi BA, McNeish JD, Hambor JE, Jakobsson PJ, Carty TJ, Perez JR, Audoly LP. Proc Natl Acad Sci U S A. 2003;100:9044. doi: 10.1073/pnas.1332766100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Weissmann G, Korchak H. Inflammation. 1984;8 (Suppl):S3. doi: 10.1007/BF00915708. [DOI] [PubMed] [Google Scholar]
- 43.Lemos HP, Grespan R, Vieira SM, Cunha TM, Verri WA, Jr, Fernandes KS, Souto FO, McInnes IB, Ferreira SH, Liew FY, Cunha FQ. Proc Natl Acad Sci U S A. 2009;106:5954. doi: 10.1073/pnas.0812782106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Miwa M, Saura R, Hirata S, Hayashi Y, Mizuno K, Itoh H. Osteoarthritis Cartilage. 2000;8:17. doi: 10.1053/joca.1999.0266. [DOI] [PubMed] [Google Scholar]
- 45.Akaogi J, Nozaki T, Satoh M, Yamada H. Endocr Metab Immune Disord Drug Targets. 2006;6:383. doi: 10.2174/187153006779025711. [DOI] [PubMed] [Google Scholar]
- 46.Yano K, Nakagawa N, Yasuda H, Tsuda E, Higashio K. J Bone Miner Metab. 2001;19:365. doi: 10.1007/s007740170006. [DOI] [PubMed] [Google Scholar]
- 47.Dogne JM, de Leval X, Neven P, Rolin S, Wauters J, David JL, Delarge J, Massereel B. Prostaglandins Leukot Essent Fatty Acids. 2000;62:311. doi: 10.1054/plef.2000.0160. [DOI] [PubMed] [Google Scholar]
- 48.Daniel TO, Liu H, Morrow JD, Crews BC, Marnett LJ. Cancer Res. 1999;59:4574. [PubMed] [Google Scholar]
- 49.Hagmann W. Pathol Oncol Res. 1997;3:83. doi: 10.1007/BF02907800. [DOI] [PubMed] [Google Scholar]
- 50.Mathis S, Jala VR, Haribabu B. Autoimmun Rev. 2007;7:12. doi: 10.1016/j.autrev.2007.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kronke G, Uderhardt S, Katzenbeisser J, Schett G. Autoimmunity. 2009;42:383. doi: 10.1080/08916930902832488. [DOI] [PubMed] [Google Scholar]
- 52.Chen ZK, Lv HS. Beijing Da Xue Xue Bao. 2006;38:533. [PubMed] [Google Scholar]
- 53.Xu S, Lu H, Lin J, Chen Z, Jiang D. Rheumatol Int. 30:1183. doi: 10.1007/s00296-009-1125-y. [DOI] [PubMed] [Google Scholar]
- 54.Wipke BT, Allen PM. J Immunol. 2001;167:1601. doi: 10.4049/jimmunol.167.3.1601. [DOI] [PubMed] [Google Scholar]
- 55.Anderson GD, Hauser SD, McGarity KL, Bremer ME, Isakson PC, Gregory SA. J Clin Invest. 1996;97:2672. doi: 10.1172/JCI118717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cortes-Burgos LA, Zweifel BS, Settle SL, Pufahl RA, Anderson GD, Hardy MM, Weir DE, Hu G, Happa FA, Stewart Z, Muthian S, Graneto MJ, Masferrer JL. Eur J Pharmacol. 2009;617:59. doi: 10.1016/j.ejphar.2009.06.058. [DOI] [PubMed] [Google Scholar]
- 57.Araico A, Terencio MC, Alcaraz MJ, Dominguez JN, Leon C, Ferrandiz ML. Life Sci. 2007;80:2108. doi: 10.1016/j.lfs.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 58.Martel-Pelletier J, Lajeunesse D, Reboul P, Pelletier JP. Ann Rheum Dis. 2003;62:501. doi: 10.1136/ard.62.6.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Magrioti V, Kokotos G. Expert Opin Ther Pat. 20:1. doi: 10.1517/13543770903463905. [DOI] [PubMed] [Google Scholar]
- 60.Nataraju A, Raghavendra Gowda CD, Rajesh R, Vishwanath BS. Curr Top Med Chem. 2007;7:801. doi: 10.2174/156802607780487696. [DOI] [PubMed] [Google Scholar]
- 61.Shishodia S, Majumdar S, Banerjee S, Aggarwal BB. Cancer Res. 2003;63:4375. [PubMed] [Google Scholar]
- 62.Elmali N, Esenkaya I, Harma A, Ertem K, Turkoz Y, Mizrak B. Inflamm Res. 2005;54:158. doi: 10.1007/s00011-004-1341-6. [DOI] [PubMed] [Google Scholar]
- 63.Sethi G, Ahn KS, Pandey MK, Aggarwal BB. Blood. 2007;109:2727. doi: 10.1182/blood-2006-10-050807. [DOI] [PubMed] [Google Scholar]
- 64.Ichikawa H, Takada Y, Shishodia S, Jayaprakasam B, Nair MG, Aggarwal BB. Mol Cancer Ther. 2006;5:1434. doi: 10.1158/1535-7163.MCT-06-0096. [DOI] [PubMed] [Google Scholar]
- 65.Burrage PS, Mix KS, Brinckerhoff CE. Front Biosci. 2006;11:529. doi: 10.2741/1817. [DOI] [PubMed] [Google Scholar]
- 66.Kevorkian L, Young DA, Darrah C, Donell ST, Shepstone L, Porter S, Brockbank SM, Edwards DR, Parker AE, Clark IM. Arthritis Rheum. 2004;50:131. doi: 10.1002/art.11433. [DOI] [PubMed] [Google Scholar]
- 67.Poole AR, Nelson F, Dahlberg L, Tchetina E, Kobayashi M, Yasuda T, Laverty S, Squires G, Kojima T, Wu W, Billinghurst RC. Biochem Soc Symp. 2003:115. doi: 10.1042/bss0700115. [DOI] [PubMed] [Google Scholar]
- 68.Andersen TL, del Carmen Ovejero M, Kirkegaard T, Lenhard T, Foged NT, Delaisse JM. Bone. 2004;35:1107. doi: 10.1016/j.bone.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 69.Moses MA. Stem Cells. 1997;15:180. doi: 10.1002/stem.150180. [DOI] [PubMed] [Google Scholar]
- 70.Raza SL, Cornelius LA. J Investig Dermatol Symp Proc. 2000;5:47. doi: 10.1046/j.1087-0024.2000.00004.x. [DOI] [PubMed] [Google Scholar]
- 71.Carmichael DF, Stricklin GP, Stuart JM. Agents Actions. 1989;27:378. doi: 10.1007/BF01972827. [DOI] [PubMed] [Google Scholar]
- 72.Mohammed FF, Smookler DS, Khokha R. Ann Rheum Dis. 2003;62 (Suppl 2):ii43. doi: 10.1136/ard.62.suppl_2.ii43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.van der Laan WH, Quax PH, Seemayer CA, Huisman LG, Pieterman EJ, Grimbergen JM, Verheijen JH, Breedveld FC, Gay RE, Gay S, Huizinga TW, Pap T. Gene Ther. 2003;10:234. doi: 10.1038/sj.gt.3301871. [DOI] [PubMed] [Google Scholar]
- 74.Shaw T, Nixon JS, Bottomley KM. Expert Opin Investig Drugs. 2000;9:1469. doi: 10.1517/13543784.9.7.1469. [DOI] [PubMed] [Google Scholar]
- 75.Sumantran VN, Kulkarni AA, Harsulkar A, Wele A, Koppikar SJ, Chandwaskar R, Gaire V, Dalvi M, Wagh UV. J Biosci. 2007;32:755. doi: 10.1007/s12038-007-0075-3. [DOI] [PubMed] [Google Scholar]
- 76.de Groot H. Hepatogastroenterology. 1994;41:328. [Google Scholar]
- 77.Kehrer JP. Crit Rev Toxicol. 1993;23:21. doi: 10.3109/10408449309104073. [DOI] [PubMed] [Google Scholar]
- 78.Merry P, Winyard PG, Morris CJ, Grootveld M, Blake DR. Ann Rheum Dis. 1989;48:864. doi: 10.1136/ard.48.10.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Woodruff T, Blake DR, Freeman J, Andrews FJ, Salt P, Lunec J. Ann Rheum Dis. 1986;45:608. doi: 10.1136/ard.45.7.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Cuzzocrea S. Curr Pharm Des. 2006;12:3551. doi: 10.2174/138161206778343082. [DOI] [PubMed] [Google Scholar]
- 81.Zlabinger GJ, Rosenkranz AR, Schmaldienst S, Stuhlmeier K, Bohmig G, Stockl J, Pohanka E, Kovarik J. Eur J Immunol. 1993;23:977. doi: 10.1002/eji.1830230434. [DOI] [PubMed] [Google Scholar]
- 82.Weiss SJ, Peppin G, Ortiz X, Ragsdale C, Test ST. Science. 1985;227:747. doi: 10.1126/science.2982211. [DOI] [PubMed] [Google Scholar]
- 83.Kerwin JF, Jr, Heller M. Med Res Rev. 1994;14:23. doi: 10.1002/med.2610140103. [DOI] [PubMed] [Google Scholar]
- 84.Geller DA, Billiar TR. Cancer Metastasis Rev. 1998;17:7. doi: 10.1023/a:1005940202801. [DOI] [PubMed] [Google Scholar]
- 85.Marletta MA. J Biol Chem. 1993;268:12231. [PubMed] [Google Scholar]
- 86.Stuehr DJ. Annu Rev Pharmacol Toxicol. 1997;37:339. doi: 10.1146/annurev.pharmtox.37.1.339. [DOI] [PubMed] [Google Scholar]
- 87.Nathan C. Faseb J. 1992;6:3051. [PubMed] [Google Scholar]
- 88.Kim YM, de Vera ME, Watkins SC, Billiar TR. J Biol Chem. 1997;272:1402. doi: 10.1074/jbc.272.2.1402. [DOI] [PubMed] [Google Scholar]
- 89.Palmer RM, Bridge L, Foxwell NA, Moncada S. Br J Pharmacol. 1992;105:11. doi: 10.1111/j.1476-5381.1992.tb14202.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Salzman AL. New Horiz. 1995;3:352. [PubMed] [Google Scholar]
- 91.Szabo C, Thiemermann C. Shock. 1994;2:145. [PubMed] [Google Scholar]
- 92.Ajuebor MN, Virag L, Flower RJ, Perretti M, Szabo C. Immunology. 1998;95:625. doi: 10.1046/j.1365-2567.1998.00644.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Brenner T, Brocke S, Szafer F, Sobel RA, Parkinson JF, Perez DH, Steinman L. J Immunol. 1997;158:2940. [PubMed] [Google Scholar]
- 94.Diefenbach A, Schindler H, Donhauser N, Lorenz E, Laskay T, MacMicking J, Rollinghoff M, Gresser I, Bogdan C. Immunity. 1998;8:77. doi: 10.1016/s1074-7613(00)80460-4. [DOI] [PubMed] [Google Scholar]
- 95.Hierholzer C, Harbrecht B, Menezes JM, Kane J, MacMicking J, Nathan CF, Peitzman AB, Billiar TR, Tweardy DJ. J Exp Med. 1998;187:917. doi: 10.1084/jem.187.6.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.McInnes IB, Leung B, Wei XQ, Gemmell CC, Liew FY. J Immunol. 1998;160:308. [PubMed] [Google Scholar]
- 97.McCartney-Francis N, Allen JB, Mizel DE, Albina JE, Xie QW, Nathan CF, Wahl SM. J Exp Med. 1993;178:749. doi: 10.1084/jem.178.2.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mellor AL, Keskin DB, Johnson T, Chandler P, Munn DH. J Immunol. 2002;168:3771. doi: 10.4049/jimmunol.168.8.3771. [DOI] [PubMed] [Google Scholar]
- 99.Munn DH, Shafizadeh E, Attwood JT, Bondarev I, Pashine A, Mellor AL. J Exp Med. 1999;189:1363. doi: 10.1084/jem.189.9.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Szanto S, Koreny T, Mikecz K, Glant TT, Szekanecz Z, Varga J. Arthritis Res Ther. 2007;9:R50. doi: 10.1186/ar2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Fallarino F, Grohmann U, Hwang KW, Orabona C, Vacca C, Bianchi R, Belladonna ML, Fioretti MC, Alegre ML, Puccetti P. Nat Immunol. 2003;4:1206. doi: 10.1038/ni1003. [DOI] [PubMed] [Google Scholar]
- 102.Hayashi T, Beck L, Rossetto C, Gong X, Takikawa O, Takabayashi K, Broide DH, Carson DA, Raz E. J Clin Invest. 2004;114:270. doi: 10.1172/JCI21275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Criado G, Simelyte E, Inglis JJ, Essex D, Williams RO. Arthritis Rheum. 2009;60:1342. doi: 10.1002/art.24446. [DOI] [PubMed] [Google Scholar]
- 104.Bianco NR, Kim SH, Ruffner MA, Robbins PD. Arthritis Rheum. 2009;60:380. doi: 10.1002/art.24229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Scott GN, DuHadaway J, Pigott E, Ridge N, Prendergast GC, Muller AJ, Mandik-Nayak L. J Immunol. 2009;182:7509. doi: 10.4049/jimmunol.0804328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hassanain HH, Chon SY, Gupta SL. J Biol Chem. 1993;268:5077. [PubMed] [Google Scholar]
- 107.Fleckner J, Martensen PM, Tolstrup AB, Kjeldgaard NO, Justesen J. Cytokine. 1995;7:70. doi: 10.1006/cyto.1995.1009. [DOI] [PubMed] [Google Scholar]
- 108.Boasso A, Herbeuval JP, Hardy AW, Winkler C, Shearer GM. Blood. 2005;105:1574. doi: 10.1182/blood-2004-06-2089. [DOI] [PubMed] [Google Scholar]
- 109.Murray MF. Lancet Infect Dis. 2003;3:644. doi: 10.1016/s1473-3099(03)00773-4. [DOI] [PubMed] [Google Scholar]
- 110.Zhu L, Ji F, Wang Y, Zhang Y, Liu Q, Zhang JZ, Matsushima K, Cao Q, Zhang Y. J Immunol. 2006;177:8226. doi: 10.4049/jimmunol.177.11.8226. [DOI] [PubMed] [Google Scholar]
- 111.Okamoto H, Cujec TP, Yamanaka H, Kamatani N. FEBS J. 2008;275:4463. doi: 10.1111/j.1742-4658.2008.06582.x. [DOI] [PubMed] [Google Scholar]
- 112.Karin M. Ann Rheum Dis. 2004;63 (Suppl 2):ii62. doi: 10.1136/ard.2004.028274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Sweeney SE, Firestein GS. Curr Opin Rheumatol. 2004;16:231. doi: 10.1097/00002281-200405000-00011. [DOI] [PubMed] [Google Scholar]
- 114.Chang L, Karin M. Nature. 2001;410:37. doi: 10.1038/35065000. [DOI] [PubMed] [Google Scholar]
- 115.Robinson MJ, Cobb MH. Curr Opin Cell Biol. 1997;9:180. doi: 10.1016/s0955-0674(97)80061-0. [DOI] [PubMed] [Google Scholar]
- 116.Cobb MH. Prog Biophys Mol Biol. 1999;71:479. doi: 10.1016/s0079-6107(98)00056-x. [DOI] [PubMed] [Google Scholar]
- 117.Chen D, Heath V, O'Garra A, Johnston J, McMahon M. J Immunol. 1999;163:5796. [PubMed] [Google Scholar]
- 118.DeSilva DR, Jones EA, Favata MF, Jaffee BD, Magolda RL, Trzaskos JM, Scherle PA. J Immunol. 1998;160:4175. [PubMed] [Google Scholar]
- 119.Pages G, Guerin S, Grall D, Bonino F, Smith A, Anjuere F, Auberger P, Pouyssegur J. Science. 1999;286:1374. doi: 10.1126/science.286.5443.1374. [DOI] [PubMed] [Google Scholar]
- 120.Dumitru CD, Ceci JD, Tsatsanis C, Kontoyiannis D, Stamatakis K, Lin JH, Patriotis C, Jenkins NA, Copeland NG, Kollias G, Tsichlis PN. Cell. 2000;103:1071. doi: 10.1016/s0092-8674(00)00210-5. [DOI] [PubMed] [Google Scholar]
- 121.Scherle PA, Jones EA, Favata MF, Daulerio AJ, Covington MB, Nurnberg SA, Magolda RL, Trzaskos JM. J Immunol. 1998;161:5681. [PubMed] [Google Scholar]
- 122.Schett G, Tohidast-Akrad M, Smolen JS, Schmid BJ, Steiner CW, Bitzan P, Zenz P, Redlich K, Xu Q, Steiner G. Arthritis Rheum. 2000;43:2501. doi: 10.1002/1529-0131(200011)43:11<2501::AID-ANR18>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 123.Tuyt LM, Dokter WH, Birkenkamp K, Koopmans SB, Lummen C, Kruijer W, Vellenga E. J Immunol. 1999;162:4893. [PubMed] [Google Scholar]
- 124.Brauchle M, Gluck D, Di Padova F, Han J, Gram H. Exp Cell Res. 2000;258:135. doi: 10.1006/excr.2000.4913. [DOI] [PubMed] [Google Scholar]
- 125.Brogley MA, Cruz M, Cheung HS. J Cell Physiol. 1999;180:215. doi: 10.1002/(SICI)1097-4652(199908)180:2<215::AID-JCP9>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 126.Thiel MJ, Schaefer CJ, Lesch ME, Mobley JL, Dudley DT, Tecle H, Barrett SD, Schrier DJ, Flory CM. Arthritis Rheum. 2007;56:3347. doi: 10.1002/art.22869. [DOI] [PubMed] [Google Scholar]
- 127.Herlaar E, Brown Z. Mol Med Today. 1999;5:439. doi: 10.1016/s1357-4310(99)01544-0. [DOI] [PubMed] [Google Scholar]
- 128.Ono K, Han J. Cell Signal. 2000;12:1. doi: 10.1016/s0898-6568(99)00071-6. [DOI] [PubMed] [Google Scholar]
- 129.Shi Y, Gaestel M. Biol Chem. 2002;383:1519. doi: 10.1515/BC.2002.173. [DOI] [PubMed] [Google Scholar]
- 130.Hannigan MO, Zhan L, Ai Y, Kotlyarov A, Gaestel M, Huang CK. J Immunol. 2001;167:3953. doi: 10.4049/jimmunol.167.7.3953. [DOI] [PubMed] [Google Scholar]
- 131.Kotlyarov A, Yannoni Y, Fritz S, Laass K, Telliez JB, Pitman D, Lin LL, Gaestel M. Mol Cell Biol. 2002;22:4827. doi: 10.1128/MCB.22.13.4827-4835.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kontoyiannis D, Boulougouris G, Manoloukos M, Armaka M, Apostolaki M, Pizarro T, Kotlyarov A, Forster I, Flavell R, Gaestel M, Tsichlis P, Cominelli F, Kollias G. J Exp Med. 2002;196:1563. doi: 10.1084/jem.20020281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Adams JL, Badger AM, Kumar S, Lee JC. Prog Med Chem. 2001;38:1. doi: 10.1016/s0079-6468(08)70091-2. [DOI] [PubMed] [Google Scholar]
- 134.Badger AM, Bradbeer JN, Votta B, Lee JC, Adams JL, Griswold DE. J Pharmacol Exp Ther. 1996;279:1453. [PubMed] [Google Scholar]
- 135.Manning AM, Mercurio F. Expert Opin Investig Drugs. 1997;6:555. doi: 10.1517/13543784.6.5.555. [DOI] [PubMed] [Google Scholar]
- 136.Clancy R, Rediske J, Koehne C, Stoyanovsky D, Amin A, Attur M, Iyama K, Abramson SB. Osteoarthritis Cartilage. 2001;9:294. doi: 10.1053/joca.2000.0388. [DOI] [PubMed] [Google Scholar]
- 137.Han Z, Boyle DL, Chang L, Bennett B, Karin M, Yang L, Manning AM, Firestein GS. J Clin Invest. 2001;108:73. doi: 10.1172/JCI12466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Gaillard P, Jeanclaude-Etter I, Ardissone V, Arkinstall S, Cambet Y, Camps M, Chabert C, Church D, Cirillo R, Gretener D, Halazy S, Nichols A, Szyndralewiez C, Vitte PA, Gotteland JP. J Med Chem. 2005;48:4596. doi: 10.1021/jm0310986. [DOI] [PubMed] [Google Scholar]
- 139.Ehrman TM, Barlow DJ, Hylands PJ. Bioorg Med Chem. 2010;18:2204. doi: 10.1016/j.bmc.2010.01.070. [DOI] [PubMed] [Google Scholar]
- 140.Hsu YL, Chen CY, Hou MF, Tsai EM, Jong YJ, Hung CH, Kuo PL. Mol Nutr Food Res. 2010;54:1307. doi: 10.1002/mnfr.200900125. [DOI] [PubMed] [Google Scholar]
- 141.Li Q, Verma IM. Nat Rev Immunol. 2002;2:725. doi: 10.1038/nri910. [DOI] [PubMed] [Google Scholar]
- 142.Dejardin E, Droin NM, Delhase M, Haas E, Cao Y, Makris C, Li ZW, Karin M, Ware CF, Green DR. Immunity. 2002;17:525. doi: 10.1016/s1074-7613(02)00423-5. [DOI] [PubMed] [Google Scholar]
- 143.Ghosh S, Karin M. Cell. 2002;109 (Suppl):S81. doi: 10.1016/s0092-8674(02)00703-1. [DOI] [PubMed] [Google Scholar]
- 144.Silverman N, Maniatis T. Genes Dev. 2001;15:2321. doi: 10.1101/gad.909001. [DOI] [PubMed] [Google Scholar]
- 145.Udalova IA, Mott R, Field D, Kwiatkowski D. Proc Natl Acad Sci U S A. 2002;99:8167. doi: 10.1073/pnas.102674699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Mullan RH, Bresnihan B, Golden-Mason L, Markham T, O'Hara R, FitzGerald O, Veale DJ, Fearon U. Arthritis Rheum. 2006;54:105. doi: 10.1002/art.21518. [DOI] [PubMed] [Google Scholar]
- 147.Uhlar CM, Whitehead AS. Eur J Biochem. 1999;265:501. doi: 10.1046/j.1432-1327.1999.00657.x. [DOI] [PubMed] [Google Scholar]
- 148.Lainer-Carr D, Brahn E. Nat Clin Pract Rheumatol. 2007;3:434. doi: 10.1038/ncprheum0559. [DOI] [PubMed] [Google Scholar]
- 149.Benbow U, Brinckerhoff CE. Matrix Biol. 1997;15:519. doi: 10.1016/s0945-053x(97)90026-3. [DOI] [PubMed] [Google Scholar]
- 150.Foster LC, Wiesel P, Huggins GS, Panares R, Chin MT, Pellacani A, Perrella MA. Faseb J. 2000;14:368. doi: 10.1096/fasebj.14.2.368. [DOI] [PubMed] [Google Scholar]
- 151.Harrison LM, van Haaften WC, Tesh VL. Infect Immun. 2004;72:2618. doi: 10.1128/IAI.72.5.2618-2627.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Rooney JW, Sun YL, Glimcher LH, Hoey T. Mol Cell Biol. 1995;15:6299. doi: 10.1128/mcb.15.11.6299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Takayanagi H. J Mol Med. 2005;83:170. doi: 10.1007/s00109-004-0612-6. [DOI] [PubMed] [Google Scholar]
- 154.Brogan IJ, Murray IA, Cerillo G, Needham M, White A, Davis JR. Mol Cell Endocrinol. 1999;157:95. doi: 10.1016/s0303-7207(99)00156-2. [DOI] [PubMed] [Google Scholar]
- 155.Rincon M, Derijard B, Chow CW, Davis RJ, Flavell RA. Genes Funct. 1997;1:51. doi: 10.1046/j.1365-4624.1997.00007.x. [DOI] [PubMed] [Google Scholar]
- 156.Aud D, Peng SL. Nat Clin Pract Rheumatol. 2006;2:434. doi: 10.1038/ncprheum0222. [DOI] [PubMed] [Google Scholar]
- 157.Iikuni N, Ikari K, Momohara S, Tomatsu T, Hara M, Yamanaka H, Okamoto H, Kamatani N. Ann Rheum Dis. 2007;66:274. doi: 10.1136/ard.2006.063347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Kobayashi S, Ikari K, Kaneko H, Kochi Y, Yamamoto K, Shimane K, Nakamura Y, Toyama Y, Mochizuki T, Tsukahara S, Kawaguchi Y, Terai C, Hara M, Tomatsu T, Yamanaka H, Horiuchi T, Tao K, Yasutomo K, Hamada D, Yasui N, Inoue H, Itakura M, Okamoto H, Kamatani N, Momohara S. Arthritis Rheum. 2008;58:1940. doi: 10.1002/art.23494. [DOI] [PubMed] [Google Scholar]
- 159.Remmers EF, Plenge RM, Lee AT, Graham RR, Hom G, Behrens TW, de Bakker PI, Le JM, Lee HS, Batliwalla F, Li W, Masters SL, Booty MG, Carulli JP, Padyukov L, Alfredsson L, Klareskog L, Chen WV, Amos CI, Criswell LA, Seldin MF, Kastner DL, Gregersen PK. N Engl J Med. 2007;357:977. doi: 10.1056/NEJMoa073003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Tokuhiro S, Yamada R, Chang X, Suzuki A, Kochi Y, Sawada T, Suzuki M, Nagasaki M, Ohtsuki M, Ono M, Furukawa H, Nagashima M, Yoshino S, Mabuchi A, Sekine A, Saito S, Takahashi A, Tsunoda T, Nakamura Y, Yamamoto K. Nat Genet. 2003;35:341. doi: 10.1038/ng1267. [DOI] [PubMed] [Google Scholar]
- 161.Kiani A, Rao A, Aramburu J. Immunity. 2000;12:359. doi: 10.1016/s1074-7613(00)80188-0. [DOI] [PubMed] [Google Scholar]
- 162.Morishita R, Tomita N, Kaneda Y, Ogihara T. Curr Opin Pharmacol. 2004;4:139. doi: 10.1016/j.coph.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 163.Muller P, Kuttenkeuler D, Gesellchen V, Zeidler MP, Boutros M. Nature. 2005;436:871. doi: 10.1038/nature03869. [DOI] [PubMed] [Google Scholar]
- 164.Kim TD, Lee JY, Cho BJ, Park TW, Kim CJ. Arch Pharm Res. 33:509. doi: 10.1007/s12272-010-0403-2. [DOI] [PubMed] [Google Scholar]
- 165.Kimmatkar N, Thawani V, Hingorani L, Khiyani R. Phytomedicine. 2003;10:3. doi: 10.1078/094471103321648593. [DOI] [PubMed] [Google Scholar]
- 166.Adcocks C, Collin P, Buttle DJ. J Nutr. 2002;132:341. doi: 10.1093/jn/132.3.341. [DOI] [PubMed] [Google Scholar]
- 167.Yang DS, Liu F, Zeng FD, Chen H. Zhongguo Zhong Yao Za Zhi. 2005;30:1361. [PubMed] [Google Scholar]
- 168.Ramgolam V, Ang SG, Lai YH, Loh CS, Yap HK. Ann Acad Med Singapore. 2000;29:11. [PubMed] [Google Scholar]
- 169.Setty AR, Sigal LH. Semin Arthritis Rheum. 2005;34:773. doi: 10.1016/j.semarthrit.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 170.Aggarwal BB, Bhardwaj A, Aggarwal RS, Seeram NP, Shishodia S, Takada Y. Anticancer Res. 2004;24:2783. [PubMed] [Google Scholar]
- 171.Sun B, Lv L, Lu ZX, Yang SY. Zhongguo Zhong Yao Za Zhi. 2008;33:2946. [PubMed] [Google Scholar]
- 172.Li J, Wang ZH, Wang CT, Cao CX, Dong QF, Jia TZ. Zhongguo Zhong Yao Za Zhi. 2008;33:2170. [PubMed] [Google Scholar]
- 173.Hwang ES, Park KK. Biosci Biotechnol Biochem. 2010;74:961. doi: 10.1271/bbb.90785. [DOI] [PubMed] [Google Scholar]
- 174.Ou Y, Li W, Li X, Lin Z, Li M. Rheumatol Int. 2010 (Ahead of print) [Google Scholar]
- 175.Sindhu G, Ratheesh M, Shyni GL, Helen A. Immunopharmacol Immunotoxicol. 2009;31:647. doi: 10.3109/08923970902947325. [DOI] [PubMed] [Google Scholar]
- 176.Konkimalla VB, Blunder M, Bauer R, Efferth T. Biochem Pharmacol. 2010;79:1573. doi: 10.1016/j.bcp.2010.01.020. [DOI] [PubMed] [Google Scholar]
- 177.Yu S, Zheng W, Xin N, Chi ZH, Wang NQ, Nie YX, Feng WY, Wang ZY. Rejuvenation Res. 2010;13:55. doi: 10.1089/rej.2009.0908. [DOI] [PubMed] [Google Scholar]
- 178.Koprowska K, Czyz M. Postepy Hig Med Dosw (Online) 2010;64:100. [PubMed] [Google Scholar]
- 179.Yang X, Liu Y, Bao Z, Jiang Y, Tu P. Zhongguo Zhong Yao Za Zhi. 2010;35:187. [PubMed] [Google Scholar]
- 180.Li H, Jia YF, Pan Y, Pan DJ, Li D, Zhang LX. Zhongguo Yao Li Xue Bao. 1997;18:270. [PubMed] [Google Scholar]