Abstract
In the Netherlands, there is an ongoing and unparalleled outbreak of Q fever. Rapid and reliable methods to identify patients infected with Coxiella burnetii, the causative agent of Q fever, are urgently needed. We evaluated the performance of different DNA extraction methods and real-time PCR assays that are in use in seven diagnostic or reference laboratories in the Netherlands. A low degree of variation in the sensitivities of most of the developed real-time PCR assays was observed. However, PCR assays amplifying short DNA fragments yielded better results than those producing large DNA fragments. With regard to DNA extraction, the automated MagNA Pure Compact system and the manual QIAamp DNA mini kit consistently yielded better results than either the MagNA Pure LC system and NucliSens EasyMag (both automated) or the High Pure viral nucleic acid kit (manual). The present study shows that multiple combinations of DNA extraction kits and real-time PCR assays offer equivalent solutions to detect C. burnetii DNA in serum samples from patients suspected to have Q fever.
Q fever is a worldwide zoonosis caused by Coxiella burnetii, an obligate intracellular bacterium (11). Whereas animals such as sheep and goats are generally asymptomatic carriers, infection with C. burnetii in these animals may become manifest by abortion. Although asymptomatic in ∼60% of infected persons, C. burnetii can cause serious illness in humans. Q fever can cause acute or chronic infection depending on the patient's condition or immune status. Acute Q fever may present as a self-limiting flu-like atypical pneumonia accompanied by severe headache and sometimes hepatitis. Approximately 5% of all Q fever cases may progress in a chronic infection leading to life-threatening endocarditis (1, 3, 5, 7-9). C. burnetii is highly infectious and can survive for long periods in the environment. Human outbreaks have been associated with farms, slaughterhouses, and wind dispersion from farms where infected animals were kept. Ticks and pets, including cats and dogs, have also been demonstrated to be potential sources of Q fever (1, 4, 10).
Laboratory diagnosis of Q fever is usually performed by serological methods such as the indirect immunofluorescence assay (IFA), complement fixation test (CFT), or enzyme-linked immunosorbent assay (ELISA), but these tests are of limited use in the early phase of the disease, as it may take up to 2 weeks for a detectable immune response to develop. Several PCR-based diagnostic methods, such as conventional PCR, nested PCR, or real-time PCR, have successfully been applied for the direct detection of C. burnetii DNA in clinical samples. The sequences targeted by these tests varied from plasmids (QpH1 or QpRS) to chromosomal genes, such as the isocitrate dehydrogenase gene (NADP) or the transposase gene of the C. burnetii IS1111a insertion element (3, 4, 14-16). The multicopy IS1111a insertion element is present in 20 copies in the genome of the C. burnetii Nine Mile RSA493 strain. Copy numbers per isolate vary and can reach up to ∼100 copies per genome (7). Due to the multicopy nature of this DNA element, it provides a highly sensitive target for detection of C. burnetii DNA in serum samples. Furthermore, real-time PCR can be useful for diagnosis of chronic Q fever, since in these patients C. burnetii DNA can be detected in serum over long periods of time (3).
In the Netherlands, as of 2007, there is an unprecedented and ongoing outbreak of Q fever (12, 17). At present, more than 3,000 cases have been reported in the Netherlands. In order to improve diagnosis for Q fever, medical microbiology laboratories have implemented molecular methods to close the diagnostic gap between onset of the disease and the presence of specific antibodies in serum. The aim of this study was to compare the performances of different DNA extraction methods and real-time PCR assays, all targeting the C. burnetii IS1111a insertion element, that are being used in seven diagnostic or public health laboratories in the Netherlands.
MATERIALS AND METHODS
Study design.
The study was set up to separately assess the performances of the DNA extraction methods and of the real-time PCR assays. The analytical sensitivities of the different PCR methods were determined using a dilution series of genomic DNA extracted from the Nine Mile strain (RSA493). The concentration of the DNA was determined by UV measurements and adjusted to approximately 50 fg/μl. Three-fold serial dilutions (nine steps) were prepared in duplicate. Each DNA sample was tested in duplicate, and thus four PCR results were obtained per sample. Based on a genome size of 2 Mbp and the presence of 20 IS1111a copies per Nine Mile genome, the starting dilution (9-fold) contains approximately 50 target copies/μl DNA. The samples were blinded. All laboratories used a fixed amount of 5 μl DNA in their PCRs according the procedure of each individual laboratory (Table 1).
TABLE 1.
Overview of equipment and protocols used by the participating laboratories
| Laboratory | DNA extraction platform | DNA isolation kit | PCR platform | PCR reagents | Reaction vol (μl) | Cycling parameterse |
|---|---|---|---|---|---|---|
| A | Manual | High Pure viral nucleic acid kita | LightCycler 480a | LightCycler 480 Probe Mastera | 20 | 95°C, 1 s; 60°C, 12 s (50×) |
| B | NucliSens EasyMagb | NucliSens magnetic extraction reagentsb | ABI Prism 7500c | In-house master mix | 25 | 95°C, 15 s; 60°C, 1 min (45×) |
| C | MagNA Pure Compact systema | MagNA Pure Compact nucleic acid isolation kit Ia | ABI Prism 7500 | ABI Universal Master mixc | 25 | 50°C, 2 min; 95°C, 15 s; 60°C, 1 min (45×) |
| D | MagNA Pure Compact system | MagNA Pure Compact nucleic Acid isolation kit I | ABI Prism 7500 | ABI Universal Master mix | 25 | 50°C, 2 min; 95°C, 15 s; 60°C, 1 min (45×) |
| MagNA Pure LC Systema | MagNA Pure LC total nucleic acid isolation kita | |||||
| E | Manual | QIAamp DNA mini kitd | ABI Prism 7500 | ABI Universal Master mix | 30 | 50°C, 2 min; 95°C, 15 s; 60°C, 1 min (45×) |
| F | MagNA Pure Compact system | MagNA Pure Compact nucleic acid isolation kit I | LightCycler 480 | LightCycler 480 Probe Master | 50 | 95°C, 15 s; 60°C, 1 min (45×) |
| MagNA Pure LC system | MagNA Pure LC total nucleic acid isolation kit | |||||
| G | Manual | QIAamp DNA mini kit | LightCycler 480 | LightCycler FastStart DNA Master HybProbea | 20 | 95°C, 10 s; 60°C, 20 s; 72°C, 15 s (45×) |
Roche Diagnostics, Almere, Netherlands.
bioMerieux, Boxtel, Netherlands.
Applied Biosystems, Nieuwekerk a/d IJssel, Netherlands.
Qiagen, Venlo, Netherlands.
Excluding any initial denaturation or final extension and/or cooling step.
Furthermore, all laboratories received three serum samples to compare the relative efficiencies of the different DNA extraction methods. Two Q fever-positive clinical samples were actual clinical samples from patients suffering from acute Q fever. The clinical samples were qualified based on the threshold cycle (CT) value that was obtained during initial screening of the samples. Sample A represents a strong positive sample, and sample B is on the lower end of the normal range for positive samples and repeatedly tested positive. The third sample (C) was a negative control.
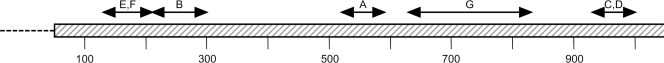
All samples were provided in duplicate and blinded such that the person handling the samples had no prior knowledge of the contents. According to the protocol, each laboratory was instructed to isolate DNA from 200 μl of each serum sample, using their routine DNA extraction method. Details of the DNA extraction procedures and amplification protocols are described in Table 1. DNA was eluted in 100 μl of elution buffer, supplemented with 5 μl of bovine serum albumin (New England Biolabs, Ipswich, MA) to a final concentration of 0.1 mg/ml, and stored at −20°C until further use. All DNA samples were subsequently collected by a central laboratory and redistributed among the participating laboratories for PCR analysis. Each real-time PCR mixture contained 5 μl of DNA extract. PCR analysis of each DNA extract was performed in duplicate, and thus four PCR results were obtained per original sample. The locations of the primers and probe combinations used by the participating laboratories are shown in Fig. 1 and described in Table 2.
FIG. 1.
Location of amplicon with PCR primers and probes from each laboratory (A to G) on the IS1111a insertion element.
TABLE 2.
Nucleotide sequences of amplification primers and detection probes used in this study.
| Laboratory(ies) | Formata | Primer or probe | Concn (μM) | Sequence (5′ → 3′) | Locationb | Amplicon size (bp) | Reference |
|---|---|---|---|---|---|---|---|
| A | TM | QKF3 | 0.5 | GTGGTGCCAAGCGATTTTAT | 7216-7235 | 78 | This study |
| QKR3 | 0.5 | GTTTCATCCGCGGTGTTAAT | 7293-7274 | ||||
| QKP3 | 0.2 | FAM-TTTAGCGAGCGAAGCGGTGG-TAMRA | 7253-7272 | ||||
| B | TM | QFw | 0.9 | TGATGGAAGCGTGTGGAGG | 6910-6928 | 87 | This study |
| QRv | 0.9 | CGTGCTGCGGACTGATCAAC | 6996-6977 | ||||
| QProbe | 0.2 | VIC-GCGAACCATTGGTATCGGACGTTT-TAMRA | 6951-6974 | ||||
| C, D | TM | 456 | 0.5 | AAAACGGATAAAAAGAGTCTGTGGTT | 7635-7660 | 70 | 13 |
| 457 | 0.5 | CCACACAAGCGCGATTCAT | 7704-7686 | ||||
| Coxbur | 0.15 | FAM-AAAGCACTCATTGAGCGCCGCG-TAMRA | 7661-7683 | ||||
| E, F | TM | IS FW | 0.5 | AAAGTGATCTACACGAGACGGGTTA | 6834-6858 | 75 | This study |
| IS REV | 0.5 | CACGCAGCCCACCTTAAGAC | 6908-6889 | ||||
| PIS | 0.2 | FAM-CGTGCTCAGTATGTATC-MGB | 6861-6877 | ||||
| G | HP | CbISF-2 | 0.5 | GGACGAAGCGATTGGTGATTAC | 7331-7352 | 202 | This study |
| CbISR-2 | 0.5 | ACTCGAATGTTGTCGAGGG | 7532-7514 | ||||
| CbIS1111aFL | 0.2 | GCGTGGGTGACATTCATCAATTTCATCG-Flu | 7453-7480 | ||||
| CbIS1111aCT635 | 0.2 | CFRed635-CCCGGCAGTTGTCGGCGTTTA-PO4 | 7483-7503 |
TM, TaqMan/hydrolysis probe; HP, hybridization probe.
Location in positions 6684 to 7778 of the whole genome sequence of C. burnetii RSA493 (GenBank accession number AE016828), encoding the transposase gene of the C. burnetii-specific IS1111a insertion element.
All samples were shipped on dry ice using an overnight delivery service. Laboratories were instructed to keep the samples frozen until they were processed.
RESULTS
In the first experiment, the analytical sensitivities of the different real-time PCR procedures were evaluated using nine samples of 3-fold serial dilutions of DNA extracted from the Nine Mile strain (RSA493). From each DNA dilution, four PCR results were obtained per laboratory. A minimum difference in PCR assay sensitivity was observed between the laboratories when evaluated on a dilution series of genomic DNA (Table 3). All laboratories were able to demonstrate the presence of C. burnetii DNA in four out of four replicates in the first two dilutions. Five laboratories were able to demonstrate the presence of C. burnetii DNA in at least two out of four replicates in the fourth dilution step. One laboratory was able to demonstrate the presence of C. burnetii DNA in three out of four replicates in the fifth dilution step. Incidentally, a single positive PCR result was obtained with some of the higher DNA dilutions, while a lower dilution remained PCR negative. We believe that this is the result of the stochastic distribution of the DNA molecules over these high dilutions.
TABLE 3.
Number of positive PCRs using a 3-fold serial dilution series of Nine Mile DNA tested with four replicates
| Dilution (fold) | Approximate copy no. per DNA sample (5 μl) | No. of positive PCRs in laboratory: |
||||||
|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | ||
| 9 | 250 | 4 | 4 | 4 | 4 | 4 | 4 | 4 |
| 27 | 83 | 4 | 4 | 4 | 4 | 4 | 4 | 4 |
| 81 | 28 | 4 | 4 | 2 | 4 | 3 | 4 | 1 |
| 243 | 9.3 | 2 | 1 | 3 | 2 | 2 | 2 | 1 |
| 729 | 3.1 | 3 | 1 | 0 | 0 | 0 | 1 | 0 |
| 2,187 | 1.0 | 1 | 0 | 1 | 0 | 0 | 1 | 1 |
| 6,561 | 0.34 | 0 | 1 | 0 | 0 | 1 | 0 | 0 |
| 19,683 | 0.11 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 59,049 | 0.04 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
By the design of the study, we were able to assess the relative efficiencies of the DNA extraction methods that were used as well as the sensitivities of the PCR assays being used. These were evaluated with clinical samples from Q fever patients. The results are shown in Table 4. For sample A, the percentages of positive PCRs were similar, indicating that all extraction methods performed equally well on this sample (71 to 89%). All but one of the laboratories were able to produce at least three out of four positive PCR results. With one exception, a positive PCR result was obtained in 89 to 97% of samples across all DNA extraction methods. More variation in the results was seen with sample B. Depending on the DNA extraction method used, a positive PCR result was obtained in 25 to 64% across all real-time PCR assays. A positive PCR result was obtained in 3 to 78% of samples across all DNA extraction methods. Apparently, the sensitivity of one of the PCR assays was much lower for both samples on DNA extracted from clinical samples than those of the other assays (laboratory G). The PCR assay that was used by laboratories C and D showed the highest overall sensitivity on DNA extracted from serum. With one exception (laboratory G), none of the laboratories obtained a positive PCR result on the negative-control sample (sample C) (data not shown).
TABLE 4.
Efficiency of DNA extraction methods and sensitivity of real-time PCR assays (tested in quadruplicate)
| Sample | DNA extraction method (laboratory) | No. of positive results out of 4 PCRs in laboratory: |
Total % positive | ||||||
|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | |||
| Aa | High Pure viral nucleic acid kit (A) | 3 | 4 | 3 | 4 | 3 | 3 | 0 | 71 |
| QIAamp DNA mini kit (E) | 4 | 4 | 4 | 4 | 4 | 4 | 1 | 89 | |
| QIAamp DNA mini kit (G) | 4 | 4 | 4 | 4 | 4 | 4 | 0 | 86 | |
| NucliSens EasyMag (B) | 3 | 3 | 4 | 3 | 4 | 3 | 0 | 71 | |
| MagNA Pure Compact (C) | 4 | 4 | 4 | 4 | 4 | 4 | 1 | 89 | |
| MagNA Pure Compact (D) | 4 | 3 | 4 | 4 | 4 | 4 | 0 | 82 | |
| MagNA Pure Compact (F) | 3 | 4 | 4 | 4 | 4 | 4 | 0 | 82 | |
| MagNA Pure LC system (D) | 4 | 3 | 4 | 4 | 3 | 3 | 0 | 75 | |
| MagNA Pure LC system (F) | 4 | 3 | 4 | 4 | 4 | 4 | 0 | 82 | |
| Total % positive | 92 | 89 | 97 | 97 | 94 | 92 | 6 | ||
| Bb | High Pure viral nucleic acid kit (A) | 2 | 1 | 2 | 3 | 1 | 0 | 0 | 32 |
| QIAamp DNA mini kit (E) | 2 | 1 | 3 | 4 | 3 | 4 | 0 | 61 | |
| QIAamp DNA mini kit (G) | 1 | 2 | 3 | 4 | 4 | 2 | 0 | 57 | |
| NucliSens EasyMag (B) | 1 | 1 | 2 | 0 | 2 | 1 | 0 | 25 | |
| MagNA Pure Compact (C) | 3 | 1 | 4 | 4 | 2 | 4 | 0 | 64 | |
| MagNA Pure Compact (D) | 1 | 0 | 4 | 3 | 2 | 3 | 1 | 50 | |
| MagNA Pure Compact (F) | 2 | 1 | 2 | 4 | 4 | 3 | 0 | 57 | |
| MagNA Pure LC system (D) | 0 | 1 | 1 | 2 | 4 | 1 | 0 | 32 | |
| MagNA Pure LC system (F) | 1 | 0 | 2 | 4 | 0 | 2 | 0 | 32 | |
| Total % positive | 36 | 22 | 64 | 78 | 61 | 56 | 3 | ||
Clinical positive sample with a relatively high DNA load.
Clinical positive sample with a relatively low DNA load.
All PCR primers and probes were designed using various primer and probe design programs targeting the DNA sequence of the IS1111a insertion element from the genome of the Nine Mile strain RSA493 (GenBank accession number AE016828). More recently, the genomic sequences of four additional C. burnetii strains, i.e., Dugway (accession number CP000733), RSA331 (CP000890), CbuG Q212 (CP001019), and Cbuk Q154 (CP001020), have become available from the National Center for Biotechnology Information (NCBI) nucleotide database (http://www.ncbi.nlm.nih.gov). The insertion elements of these strains may contain polymorphisms that have not been taken into account in development of the PCR primers and probes. Since any mismatch between the primer or probe sequence and the target sequence may lead to less efficient or less sensitive PCR assays, the suitability of the developed primers and probes was reassessed in silico using these additionally available genomic sequences. As it turns out, certain primer and probe combinations contain mismatches in the target sequences that may affect the performance of the PCR assays (Table 5) .
TABLE 5.
Numbers of IS1111a insertion elements with exact matches to the primer and probe sequences in the genomes of five different C. burnetii isolates
| Laboratory(ies) | No. of elements in strain (IS1111a copy no.): |
||||
|---|---|---|---|---|---|
| RSA493 (20) | Dugway (12) | RSA331 (47) | CbuG Q212 (28) | CbuK Q154 (48) | |
| A | 20 | 12 | 43b | 28 | 48 |
| B | 20 | 12 | 47 | 28 | 48 |
| C, D | 20 | 12 | 47 | 28 | 40e |
| E, F | 20 | 0a | 47 | 28 | 46f |
| G | 20 | 12 | 46c | 0d | 8g |
This involves a single nucleotide mismatch at the 5′ end of the forward primer.
This involves various mismatches in both forward and reverse primers in 4 of the 47 copies of the IS1111a insertion element.
This involves six mismatches in the reverse primer in 1 of the 47 copies of the IS1111a insertion element.
This involves a single nucleotide mismatch at a central position of the 28-base CbIS1111aFL probe.
This involves a single nucleotide mismatch at the second position of the forward primer in 8 of the 48 copies of the IS1111a insertion element.
This involves a single nucleotide mismatch and a double nucleotide mismatch in the reverse primer, both in 1 of the 48 copies of the IS1111a insertion element.
This involves a single nucleotide mismatch at the 5′ end of the reverse primer in 29 of the 48 copies of the IS1111a insertion element and various mismatches in the reverse primers in another 10 of the 48 copies of the IS1111a insertion element.
DISCUSSION
Reliable detection of C. burnetii DNA in serum requires highly efficient DNA extraction procedures and sensitive PCR methods. In this study we compared the analytical procedures that were developed by diagnostic laboratories in the Netherlands to aid in identification of patients with Q fever. All PCR assays targeted the C. burnetii IS1111a element, a multicopy element that has been reported to be specific for Coxiella burnetii (2, 7, 16). By the design of this study, we were able to separately analyze the performance of the DNA extraction procedure and of the PCR assays. In this study, we used actual clinical serum samples containing different loads of C. burnetii (DNA) instead of serum samples that were spiked with high-molecular-weight genomic DNA from C. burnetii DNA to get a more representative measure of the efficiency of the DNA extraction methods used. Manual extraction procedures performed equally as well as some automated extraction platforms. Despite the fact that most commercial DNA extraction kits are based on the similar chemistries, the automated MagNA Pure Compact system and the manual QIAamp DNA mini kit consistently yielded better results than either the MagNA Pure LC system and the NucliSens EasyMag (both automated) or the High Pure viral nucleic acid kit (manual). Less variation was observed in the sensitivity of the different PCR assays, with one major exception: the PCR that was in use in laboratory G was much less sensitive than the other PCR assays. This PCR performed similarly to the other assays on a dilution series of high-molecular-weight genomic DNA from the Nine Mile strain but was less sensitive on DNA extracted from clinical samples. Unfortunately, insufficient material was left to confirm these findings. However, there appears to be a very plausible explanation for these results: the lack in sensitivity may possibly be explained by the significantly larger PCR product that is targeted by laboratory G (202 bp, versus 70 to 87 bp in the other laboratories). In general cell-free DNA in serum is very likely to be degraded to a certain extent. Therefore, short sequences are likely to represent better targets than larger sequences. The highest overall sensitivity on DNA extracted from serum was obtained by the PCR assay that was in use in laboratories C and D. Notably, although the differences from most other PCR assays were relatively small, this assay targeted the shortest DNA fragment (70 bp). Another explanation for this difference may reside in sequence polymorphisms in the target sequences. All PCR assays were developed using the IS1111a sequence from the Nine Mile RSA493 strain. Analysis of IS1111a sequences from various other C. burnetii genomes shows the presence of multiple nucleotide polymorphisms that may affect PCR performance. Certain PCR amplification primers or detection probes do not match the target sequences of certain genomes equally well (Table 5). Depending on the location of the present mismatch(es), this may have had a detrimental effect on the performance of the PCR, especially for those near the 3′ end of the primers or near the 5′end of a hydrolysis probe. It has been shown that C. burnetii genotypes from the Netherlands display a considerable degree of homogeneity, indicating a clonal origin (6). Therefore, DNA sequence polymorphisms in the IS1111a elements in this Dutch clone may also affect the different PCR assays studied here and may also explain the poor performance of the PCR used by laboratory G. Whether or not this is a likely explanation remains to be established. Obviously, in samples with a very low target concentration, sampling variation may explain part of the heterogeneity seen in the results from the dilution series of genomic DNA from the Nine Mile strain (Table 3). For the evaluation of the performance of the DNA extraction methods, all participating laboratories analyzed all of the extracted DNA samples, and any effect of sampling variation on the interpretation of the results would be minimized. Two different real-time PCR platforms were used by the participating laboratories (LightCycler 480 or ABI Prism 7500). Although this could have contributed to differences in sensitivities for the various assays, in the context of the results presented in Table 3 and the alternative explanations for the lower sensitivity of the assay used by laboratory G, this appears unlikely to be a contributing factor.
In conclusion, we show that multiple combinations of DNA extraction kits and real-time PCR assays offer equivalent solutions for the screening of patients suspected to have Q fever.
Acknowledgments
We thank Elise Kraan and Linda Poort for technical assistance.
Footnotes
Published ahead of print on 8 September 2010.
REFERENCES
- 1.Arricau-Bouvery, N., Y. Hauck, A. Bejaoui, D. Frangoulidis, C. C. Bodier, A. Souriau, H. Meyer, H. Neubauer, A. Rodolakis, and G. Vergnaud. 2006. Molecular characterization of Coxiella burnetii isolates by infrequent restriction site-PCR and MLVA typing. BMC Microbiol. 6:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Denison, A. M., H. A. Thompson, and R. F. Massung. 2007. IS1111 insertion sequences of Coxiella burnetii: characterization and use for repetitive element PCR-based differentiation of Coxiella burnetii isolates. BMC Microbiol. 7:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fenollar, F., P. E. Fournier, and D. Raoult. 2004. Molecular detection of Coxiella burnetii in the sera of patients with Q fever endocarditis or vascular infection. J. Clin. Microbiol. 42:4919-4924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fournier, P. E., and D. Raoult. 2003. Comparison of PCR and serology assays for early diagnosis of acute Q fever. J. Clin. Microbiol. 41:5094-5098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Glazunova, O., V. Roux, O. Freylikman, Z. Sekeyova, G. Fournous, J. Tyczka, N. Tokarevich, E. Kovacava, T. J. Marrie, and D. Raoult. 2005. Coxiella burnetii genotyping. Emerg. Infect. Dis. 11:1211-1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klaassen, C. H., M. H. Nabuurs-Franssen, J. J. Tilburg, M. A. Hamans, and A. M. Horrevorts. 2009. Multigenotype Q fever outbreak, The Netherlands. Emerg. Infect. Dis. 15:613-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klee, S. R., J. Tyczka, H. Ellerbrok, T. Franz, S. Linke, G. Baljer, and B. Appel. 2006. Highly sensitive real-time PCR for specific detection and quantification of Coxiella burnetii. BMC Microbiol. 6:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McQuiston, J. H., J. E. Childs, and H. A. Thompson. 2002. Q fever. J. Am. Vet. Med. Assoc. 221:796-799. [DOI] [PubMed] [Google Scholar]
- 9.Musso, D., and D. Raoult. 1995. Coxiella burnetii blood cultures from acute and chronic Q-fever patients. J. Clin. Microbiol. 33:3129-3132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nelder, M. P., J. E. Lloyd, A. D. Loftis, and W. K. Reeves. 2008. Coxiella burnetii in wild-caught filth flies. Emerg. Infect. Dis. 14:1002-1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raoult, D., T. Marrie, and J. Mege. 2005. Natural history and pathophysiology of Q fever. Lancet Infect. Dis. 5:219-226. [DOI] [PubMed] [Google Scholar]
- 12.Schimmer, B., G. Morroy, F. Dijkstra, P. M. Schneeberger, G. Weers-Pothoff, A. Timen, C. Wijkmans, and W. van der Hoek. 2008. Large ongoing Q fever outbreak in the south of The Netherlands, 2008. Euro Surveill 13:18939. [PubMed] [Google Scholar]
- 13.Schneeberger, P. M., M. H. A. Hermans, E. J. van Hannen, J. J. A. Schellekens, A. C. A. P. Leenders, and P. C. Wever. 2010. Real-time PCR on serum samples is indispensable for early diagnosis of acute Q fever. Clin. Vaccine Immunol. 17:286-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spyridaki, I., A. Gikas, D. Kofteridis, A. Psaroulaki, and Y. Tselentis. 1998. Q fever in the Greek island of Crete: detection, isolation, and molecular identification of eight strains of Coxiella burnetii from clinical samples. J. Clin. Microbiol. 36:2063-2067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Turra, M., G. Chang, D. Whybrow, G. Higgins, and M. Qiao. 2006. Diagnosis of acute Q fever by PCR on sera during a recent outbreak in rural south Australia. Ann. N. Y. Acad. Sci. 1078:566-569. [DOI] [PubMed] [Google Scholar]
- 16.Vaidya, V. M., S. V. Malik, S. Kaur, S. Kumar, and S. B. Barbuddhe. 2008. Comparison of PCR, immunofluorescence assay, and pathogen isolation for diagnosis of Q fever in humans with spontaneous abortions. J. Clin. Microbiol. 46:2038-2044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van Steenbergen, J. E., G. Morroy, C. A. Groot, F. G. Ruikes, J. H. Marcelis, and P. Speelman. 2007. An outbreak of Q fever in The Netherlands—possible link to goats. Ned. Tijdschr. Geneeskd. 151:1998-2003. [PubMed] [Google Scholar]