Abstract
A highly sensitive detection test for Rinderpest virus (RPV), based on a real-time reverse transcription-PCR (rRT-PCR)system, was developed. Five different RPV genomic targets were examined, and one was selected and optimized to detect viral RNA in infected tissue culture fluid with a level of detection ranging from 0.59 to 87.5 50% tissue culture infectious doses (TCID50) per reaction depending on the viral isolate. The strain sensitivity of the test was validated on 16 RPV strains belonging to all three phylogenetic branches described for RPV. No cross-reactivity was detected with closely related peste des petit ruminants or with symptomatically similar viruses, including all seven serotypes of foot-and-mouth disease virus, two serotypes of vesicular stomatitis virus, bluetongue virus, and bovine herpes virus type 2. In samples from experimentally infected cattle, our real-time RT-PCR test was significantly more sensitive than the gold standard test of virus isolation, allowing the detection of the disease 2 to 4 days prior to the appearance of clinical signs. The comparison of clinical samples with putative diagnostic value from live animals showed that conjunctival swabs and blood buffy coat were the samples of choice for epidemiological surveillance, while lymph nodes performed the best as postmortem specimens. This portable and rapid real-time RT-PCR has the capability of the preclinical detection of RPV and provides differential diagnosis from look-alike diseases of cattle. As RPV is declared globally eradicated, this test provides an important rapid virus detection tool that does not require the use of infectious virus and allows the processing of a large number of samples.
Rinderpest virus (RPV), a member of the Morbillivirus genus of the Paramyxoviridae family, causes an acute, highly contagious, and often fatal disease in cattle, buffaloes, and yaks (1, 4, 18). The disease affects the gastrointestinal and respiratory tracts of infected animals and is characterized by fever, nasal and ocular discharges, diarrhea, oral erosions, and lymphoid tissue necrosis (2). Like all morbilliviruses, RPV is an enveloped, single-stranded, nonsegmented, negative-sense RNA virus that is antigenically and genetically related to other member of the genus, such as measles virus (MV), peste des petits ruminants virus (PPRV), and canine distemper virus (CDV) (4, 15). The 15.8-kb viral genome contains six genes in the order 3′-N-P-M-F-H-L-5′ [each with their own start and poly(A) signals], an intergenic region between M and F genes, and two flanking untranslated regions (UTRs) at both ends of the genome (3, 8). Although the disease is expected to be declared eradicated in 2010 (http://www.fao.org/docs/eims/upload/258696/ak064e00.pdf), records indicate that field isolates during the last outbreaks were of low virulence and transmissibility and low mortality, opening the possibility that outbreaks will go undetected (5). The molecular bases for the differences in RPV pathogenicity are unknown, but the mild disease presentation seen lately (described as subacute infections) constitutes a problem for the early detection of RPV, as outbreaks involving large numbers of animals occur after the failure to recognize the index case in a population. RP also affects sheep, goats, certain breeds of pigs, and a wide range of wildlife species, but infection in these animals usually is subclinical (2) and sometimes indistinguishable from PPRV. Subacute infection in cattle is observed most often in countries where the disease remains enzootic (5). Therefore, the early preclinical detection of infected animals using a rapid diagnostic test capability for differentiation between RPV and PPRV would be very useful in the surveillance of suspected cases after eradication. In the case of suspected RPV activity, having a rapid and precise viral detection test in place will be critical for disease containment. The current diagnosis of RPV relies on a number of serologic methods, such as indirect enzyme-linked immunosorbent assay (ELISA), competitive ELISA, and seroneutralization (VN) tests, which are not ideal for outbreak detection and, in the case of VN, requires the use of live virus. RPV antibodies start to develop between 2 and 5 days after the onset of clinical disease in virulent infections and 6 to 10 days (up to 17 days) after infection with attenuated strains (5, 13, 16), which is between 2 and 4 weeks after infection. Therefore, serological approaches for diagnosis, although sensitive and specific, would allow the wide spread of the disease before an alert and the implementation of the appropriate control measures. Antigen detection historically has been carried out by virus isolation (VI) in monolayers of primary calf kidney (B95), a marmoset lymphoblastoid on African green monkey kidney (Vero) cells, and agar gel immunodifusion (AGID). Although these are reliable methods, they are available only in well-established laboratories and are not readily available for field use, for import/export purposes, and/or for animal movement regulation. These techniques do not perform well during outbreaks or acute investigations and lack the necessary speed and sensitivity required for outbreak control situations. Moreover, neither these tests nor clinical observation can differentiate between RPV and PPRV, requiring further differential diagnostics and further delay. Differential immunocapture ELISA is fast and specific but not sensitive enough for clinical samples. Finally, immunofluorescence, histopathology, and immunohistochemistry are very useful techniques for postmortem but not for in vivo diagnostics.
Conventional reverse transcription-PCRs (RT-PCRs) with viral RNA purified from postmortem samples (spleen, lymph node, and tonsil) or in vivo from peripheral blood lymphocytes (PBLs) or swabs from eye or mouth lesions have been used previously (10, 11). Conventional RT-PCR allows for fast turnaround times, but it is not portable and requires qualified instrumentation available only in centralized laboratory facilities. Real-time RT-PCR (rRT-PCR) has demonstrated superior sensitivity and specificity compared to that of the currently used antigen detection methods of virus isolation and conventional RT-PCR for many diseases of livestock, and it also has proved reliable in generating fast results in a portable format. In addition, it has the capability of preclinical diagnosis in the event of a potential disease outbreak (7, 22, 27). Here, we present the design and optimization of an rRT-PCR assay and its use for the early detection of RPV in samples from experimentally infected cattle.
MATERIALS AND METHODS
Virus isolates.
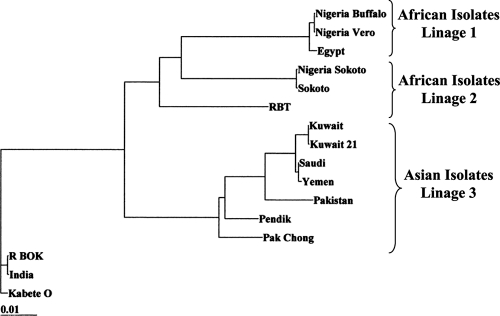
The viral isolates used in this study were obtained from FADDL-APHIS-USDA (Foreign Animal Diseases Diagnostic Laboratory of the Animal and Plant Health Inspection Service of the USDA) repository collection (Table 1). These isolates are representative of several geographic areas and include all RPV genetic lineages described to date (Fig. 1) (26).
TABLE 1.
RPV isolates used for nucleotide alignment to design the primers-probe sets
| Isolate | GenBank accession no. | Genomic data |
|---|---|---|
| Kabete Oa | To be determined | Complete genome |
| RBOKa | To be determined | Complete genome |
| Pak Chonga | To be determined | Complete genome |
| Pendika | To be determined | Complete genome |
| RBTa | To be determined | Complete genome |
| Saudia | To be determined | Complete genome |
| Kuwait 21a | To be determined | Complete genome |
| Nigeria Buffaloa | To be determined | Complete genome |
| Yemena | To be determined | Complete genome |
| Indiaa | To be determined | Complete genome |
| Nigeria Sokotoa | To be determined | Complete genome |
| Kuwaita | To be determined | Complete genome |
| Sokotoa | To be determined | Complete genome |
| Pakistana | To be determined | Complete genome |
| Nigeria veroa | To be determined | Complete genome |
| Egypta | To be determined | Complete genome |
| RBOK | Z30697 | N, P, C, M, F, H, and L |
| Kabete O | NC006296 | FL |
| LATC | AF515676 | N |
| RBOK | X68311, S54798 | N, P, V, and C |
| Kuwait 82/1 | Z34262 | N |
| Kabete O | U02679 | N |
| Kabete O | AY035887 | F |
| Kabete O Lapinized | M20870 | F |
| Kabete O | M21514 | F |
| Egypt/84 | Z31655 | F |
| RBOK | Z30700 | F |
| RBT1 | Z31656 | F |
| Kabete O | M21513 | H |
| LA | D82982 | H |
| Kabete O | AF132934 | H |
| Kabete O Lapinized | M17434 | H |
| RBOK | Z30699 | H |
| Kabete O | Y18816 | H |
| Kabete O | Z33634 | L |
| Kuwait 82/1 | Z33636 | L |
| Kabete O | X98291 | N, P, M, F, H, and L |
| RBOK | Z30698 | L |
The full lengths of these RPV isolates were sequenced previously (Carrillo et al., unpublished results).
FIG. 1.
Phylogenetic representation of the complete sequenced RPV isolates used for the design and optimization of rRT-PCR.
Virus isolation.
Tissue and swab samples from experimentally infected cattle were tested for VI in Vero cell cultures by following Office International des Epizooties (OIE) protocols (17). Briefly, approximately 0.2 g of tissue was homogenated in 1 ml Dulbecco's modified Eagle's medium (DMEM) and clarified by centrifugation, and 50 μl of supernatant was used to infect Vero cell monolayers in 96-well plates in quadruplicate, using three 10-fold dilutions (undiluted, 1:10, and 1:100). The presence of cytopathic effect (CPE) in the infected cell was monitored daily up to 7 days postinfection (dpi). Plates were frozen and thawed and used to infect fresh Vero cells. VI was determined by microscopic observation and crystal violet staining. Additionally, all wells corresponding to the same sample were pooled, and the total RNA was extracted and tested by conventional RT-PCR, as previously described (11), to confirm VI results.
Virus titrations.
Serial dilutions of viral suspension were inoculated in Vero cell monolayers with four replicates for each sample and observed for CPE, as described above. Titers were calculated according to Reed and Muench (21) and expressed as log10 50% tissue culture infectious doses (TCID50)/ml.
RNA extraction.
RNA was extracted from 140 μl of cell culture supernatant, culture media containing clinical swabs, or buffy coat samples. The RNeasy extraction kit (Qiagen, Stanford, CA) was used for RNA extraction from cell cultures and viral suspensions according to the manufacturer's specifications. Tissue samples obtained postmortem were homogenized and treated with QIAshredder (Qiagen, Stanford, CA) prior to RNA extraction. RNA was eluted in 40 μl of RNase-free water and stored at −70°C until the PCR test was performed.
rRT-PCR.
The assay was performed using ABI TaqMan RT-PCR core reagents (Applied Biosystems, product N8080232) with 5 mM Mn(OAc)2, 0.1 U rTth DNA polymerase, and 0.2 mM deoxynucleoside triphosphate mix (supplied as 10 mM dilution each and mixed 1:1:1:1 by volume) in a final 25-μl reaction mixture. Primer and probe sequences and their positions in the RPV genome are summarized in Table 2. Molarities for primers and probes were optimized individually and are detailed in Results. Real-time RT-PCR was done using a SmartCycler machine (Cepheid, Sunnyvale, CA). Reverse transcription was allowed to take place for 30 min at 60°C, followed by a 2-min denaturing step at 95°C and 45 amplification cycles of 95°C for 10 s and 55°C for 60 s.
TABLE 2.
Sequences and genomic position of the primer-probe sets
| Viral gene | Genome positiona | Oligonucleotide sense/function | 5′-3′ sense nucleotide sequence |
|---|---|---|---|
| H | 7315 | Forward primer | GAA CAC TCG GGT GGT TCT TAA TAA A |
| 7426 | Reverse primer | TGC GAT AGC TAA TAG CCC GAC | |
| Probe | ACG GTG TTG TTT GTC ATG T | ||
| F | 6956 | Forward primer | TGA TTG CAG TAG TGG GTA TCC TCA |
| 7092 | Reverse primer | TGA CCG TAC GTA GGA TTT GGA TG | |
| Probe | ACC TGT TGC TGT AGG AAG | ||
| N | 1020 | Forward primer | TGG GTG AAC TGG CTC C |
| 1120 | Reverse primer | CCC ATA GCA TAG CTC CA | |
| Probe | TTC AGT GCA GGA GCA | ||
| L9 | 9157 | Forward primer | GCAACATACAAACGGCTACCAA |
| 9303 | Reverse primer | TGGCAACCAGCTTGTTAGTCA | |
| Probe | CTG TAT TTC ACC ATG GAC TC | ||
| L10 | 10376 | Forward primer | RAT GAA AGG WCA TGC CAT ATT |
| 10450 | Reverse primer | GGT GGC CAG CTC C | |
| Probe | ATC ATC AAC GGG TAT CG |
Numbers indicate the 5′ nucleotide position of the primer-probe, counting from the 5′ end of the full-length genome sequence of RPV, according to Kabete O sequence NC006296.
Animal infections.
Six steers, weighing approximately 230 kg, were inoculated with 104 TCID50 of the Kabete O strain of RPV by intramuscular injection. Body temperature and clinical samples were taken daily from the infected animals. Clinical signs of infection included fever, conjunctivitis, emaciation, salivation, nasal discharge, respiratory distress, recumbence, mucopurulent discharge through eyes and nose, and complete prostration during the final stages of disease. Clinical samples were collected with Dacron swabs into tubes containing 500 μl of DMEM (Invitrogen, San Diego, CA), including nasal, oral, conjunctival, vaginal/preputial, and anal swabs (see Table 7). Blood samples were collected into BD Vacutainer cell preparation tubes with sodium heparin (BD, Franklin Lakes, NJ). Buffy coats were separated by centrifugation in a swinging rotor at 1,380 rpm (700 × g) on a Ficoll-Hypaque cushion, collected, and washed three times in phosphate-buffered saline (PBS) and resuspended in 1 ml DMEM. Approximately 7 days postinoculation, all animals were euthanized when found to be moribund. Tissue samples from tonsils, Peyer's patches, lymph nodes, spleen, abomasums, and other areas (see Table 7) were collected at necropsy and immediately frozen at −70°C until use.
RESULTS
Primer-probe design and assay optimization.
Genes N, F, H, and L, identified previously as the most conserved regions of the RPV genome (C. Carrillo, A. Vagnozzi, Z. Lu, G. F. Kutish, and D. L. Rock, unpublished data), were selected for the design of five primer-probe sets. Partial RPV sequences available in GenBank were added to the complete array of sequences we had generated in our laboratory (Table 1) and input into Primer Express software (Applied Biosystems, Foster City, CA) for primer-probe design. All of the putative primer-probe sets obtained were blasted against the NCBI nucleotide database and selected based on maximum RPV specificity and the minimum number of mismatches with the RPV sequences. Finally, the primers shown in Table 2 were selected.
Primer-probe sets initially were tested for their ability to detect RPV Kabete O RNA as the template at probe and primer concentrations ranging from 50 to 200 nM and 100 to 500 nM, respectively. Optimal primer-probe combinations (defined as those resulting in the lowest threshold cycle [CT] value and highest specific fluorescence) were 200 and 400 nM for H, N, and L9, and 100 and 500 nM for F and L10 (Table 3 ). Using these optimized conditions, primer-probe sets were tested for the detection of 16 RPV isolates representing the main genetic lineages described for RPV (Table 4). Only N and L10 primer-probe sets were able to detect all 16 RPV isolates.
TABLE 3.
CT and FAM values obtained during the primer/probe concentration optimization for every set using a 55°C annealing temperature and 55 cycles and Kabete O viral RNA template
| Probe and concn (nM) | Primer concn (25-μl reaction mix)a |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 100 nM |
200 nM |
300 nM |
400 nM |
500 nM |
||||||
| CT | ΔFAM | CT | ΔFAM | CT | ΔFAM | CT | ΔFAM | CT | ΔFAM | |
| H | ||||||||||
| 50 | 0.00 | 0 | 17.58 | 74 | 16.99 | 73 | 16.73 | 81 | 16.57 | 78 |
| 100 | 20.69 | 132 | 16.44 | 190 | 15.93 | 195 | 15.88 | 204 | 15.51 | 238 |
| 200 | 17.92 | 546 | 14.88 | 590 | 14.74 | 476 | 14.40 | 552 | 14.31 | 547 |
| N | ||||||||||
| 50 | 20.89 | 244 | 18.89 | 217 | 18.92 | 235 | 17.75 | 232 | 17.75 | 219 |
| 100 | 26.23 | 312 | 21.71 | 419 | 21.75 | 417 | 21.47 | 423 | 21.20 | 454 |
| 200 | 18.64 | 842 | 16.82 | 881 | 15.90 | 843 | 15.99 | 997 | 15.42 | 908 |
| F | ||||||||||
| 50 | 16.00 | 0 | 16.00 | 68 | 16.00 | 87 | 16.00 | 87 | 16.00 | 108 |
| 100 | 17.77 | 87 | 15.91 | 162 | 15.58 | 231 | 15.64 | 263 | 15.39 | 293 |
| 200 | 15.87 | 147 | 14.42 | 243 | 15.62 | 142 | 14.51 | 327 | 15.13 | 286 |
| L9 | ||||||||||
| 50 | 0.00 | 0 | 19.92 | 74 | 18.94 | 97 | 18.82 | 99 | 19.38 | 81 |
| 100 | 20.94 | 73 | 17.80 | 175 | 17.63 | 209 | 17.64 | 199 | 17.55 | 236 |
| 200 | 18.21 | 204 | 17.16 | 342 | 17.44 | 279 | 16.79 | 434 | 17.32 | 318 |
| L10 | ||||||||||
| 50 | 27.46 | 131 | 21.20 | 127 | 19.80 | 122 | 19.45 | 110 | 19.43 | 108 |
| 100 | 24.23 | 275 | 20.30 | 340 | 19.48 | 303 | 19.11 | 302 | 15.34 | 646 |
| 200 | 18.75 | 465 | 17.80 | 189 | 15.55 | 425 | 15.47 | 589 | 18.40 | 362 |
ΔFAM data represent increments of fluorescence. CT data represent threshold cycle values (the cycle numbers at which the increase in fluorescence is exponential and crosses the preassigned threshold). Boldface data represent the best CT values for each concentration and temperature combination.
TABLE 4.
RPV strains detected by rRT-PCR assay at 55°C annealing temperature and 55 cycles, with preoptimized concentrations of primer-probe for each set
| RPV isolate | Primer-probe set |
||||
|---|---|---|---|---|---|
| Ha | Nb | Fc | L9d | L10e | |
| K15 | 0 | 33.42 | 0 | 0 | 28.52 |
| Kabete O | 35.07 | 32.09 | 31.72 | 28.18 | 24.85 |
| Pakchong | 42.05 | 22.67 | 0 | 0 | 13.52 |
| NAK 3 | 44.58 | 30.25 | 0 | 0 | 23.31 |
| RBOK | 31.09 | 28.4 | 27.51 | 21.58 | 18.77 |
| RB Nigeria | 37.8 | 19.74 | 0 | 0 | 26.81 |
| Pakistan | 0 | 23.49 | 0 | 0 | 19.89 |
| Yemen | 0 | 25.47 | 0 | 0 | 19.22 |
| Pendik | 0 | 25.4 | 0 | 0 | 19.72 |
| Nigerian Buffalo | 46.2 | 22.7 | 0 | 0 | 21.09 |
| Kuwait | 0 | 25.75 | 0 | 0 | 18.89 |
| Saudi Arabia | 0 | 18.26 | 0 | 0 | 13.93 |
| RBT | 0 | 20.87 | 0 | 0 | 15.74 |
| India | 29.36 | 27.66 | 27.05 | 21.37 | 18.65 |
| Sokoto | 0 | 32.13 | 0 | 0 | 24.26 |
| Egypt | 37.8 | 24.31 | 0 | 0 | 22.99 |
Primer-probe set H (200 nM probe-400 nM primers).
Primer-probe set F (100 nM probe-500 nM primers).
Primer-probe set N (200 nM probe-400 nM primers).
Primer-probe set L9 (200 nM probe-400 nM primers).
Primer-probe set L10 (200 nM probe-400 nM primers).
Therefore, further optimization continued for these two primer-probe sets only. Annealing temperature optimization using 50, 55, and 60°C did not show significant differences in efficiency for the amplification of the RPV RNA (data not shown). A close RPV relative, PPRV, was used as a genetic near-neighbor RNA target to control for the specificity of the test at each temperature setting. Probe L10 specifically detected RPV at all annealing temperatures and did not detect PPRV at any annealing temperature (Table 5). The N system adequately recognized RPV at the three temperatures tested but showed the nonspecific amplification of PPRV at all annealing temperatures (Table 5). Therefore, no further testing was done with the N gene primer-probe set.
TABLE 5.
PPRV cross-detection with primer-probe sets L10 and N
| Primer-probe and virus | Annealing temp. | Avg FAM CTa |
|---|---|---|
| L10 | ||
| RPVb | 50 | 19.09 ± 0.27 |
| 55 | 18.79 ± 0.04 | |
| 60 | 21.26 ± 1.06 | |
| PPRc | 50 | 0.00 ± 0.00 |
| 55 | 0.00 ± 0.00 | |
| 60 | 0.00 ± 0.00 | |
| N | ||
| RPVb | 50 | 18.66 ± 0.34 |
| 55 | 18.33 ± 0.12 | |
| 60 | 18.54 ± 1.34 | |
| PPRc | 50 | 35.69 ± 2.45 |
| 55 | 31.48 ± 1.73 | |
| 60 | 36.88 ± 1.87 |
Results are expressed as average FAM CT values from two different isolates.
The RPV isolate was either Kabete O or India in two different experiments.
The PPRV isolate was either Burkina or Cote d'Ivoire in two different experiments.
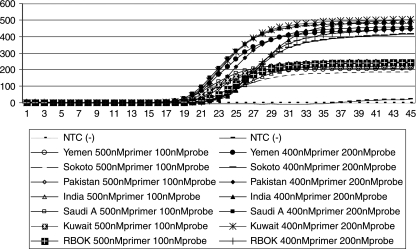
To determine the effect of annealing temperature in the sensitivity and/or specificity for detecting different RPV strains with the L10 rRT-PCR assay, conditions previously optimized for Kabete O were tested with all seven RPV strains, representatives of all known genetic lineages. The two highest annealing temperatures (55 and 60°C) with the two best primer-probe concentrations (500 and 100 nM and 400 and 200 nM) were tested. No significant differences were observed in relation to the annealing temperatures (data not shown); however, the 400 and 200 nM primer-probe concentration performed better and more consistently in detecting all seven reference isolates (Fig. 2).
FIG. 2.
Optimal concentration of the L10 primer-probe set for 45 cycles. Two combinations of L10 primer-probe sets (200 nM probe-400 nM primers and 100 nM probe-500 nM primer) were tested against different RPV isolates (Yemen, Sokoto, Pakistan, India, Saudi Arabia, Kuwait, and RBOK).
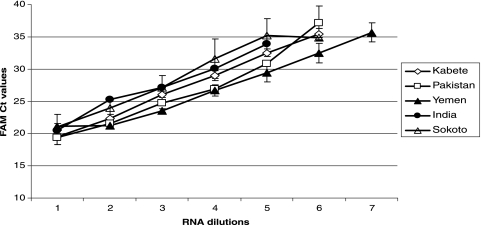
To assess the robustness of the selected conditions for the L10 rRT-PCR assay, 21 repetitions of the same RNA sample (Kabete O) were performed by three separate operators and on four different thermocycler units. No significant differences were observed between runs, indicating that the L10 rRT-PCR was highly reliable to detect RPV RNA within a range of ±2.0 FAM CT (the cycle number at which the fluorescent detector FAM [6-carboxyfluorescein] value increases exponentially and crosses the preassigned threshold) in 21 independent repetitions (data not shown). L10 rRT-PCR assay reproducibility also was analyzed by running 10-fold dilutions of RPV RNA from different RPV isolates: Kabete O (eight replicates), Pakistan (three replicates), Yemen (three replicates), India (two replicates), and Sokoto (five replicates). Results indicated a low degree of variability between runs and viral isolates (Fig. 3).
FIG. 3.
L10 primer-probe real-time RT-PCR assay reproducibility. Graphic representation of average and standard deviations from the FAM CT values obtained for 10-fold dilutions of RPV RNA from different isolates: Kabete O (eight replicates), Pakistan (three replicates), Yemen (three replicates), India (two replicates), and Sokoto (five replicates).
Specificity of amplification of L10 rRT-PCR.
The analytical specificity of the L10 rRT-PCR assay was tested against a collection of viruses that either show close genetic relationship with RPV (near neighbors) or cause a disease that can be difficult to differentiate clinically from RP (look-alikes). Near neighbors included 17 strains of PPRV from various geographical and temporal origins. Look-alike disease agents tested included bluetongue virus (BTV), bovine viral diarrhea virus (BVDV), bovine herpes virus 2 (BHV-2), seven serotypes of foot-and-mouth disease virus (FMDV), and vesicular stomatitis virus (VSV) serotypes Indiana and New Jersey. The L10 rRT-PCR assay showed no reactivity with any of the 25 non-RPV agents tested (see Table S1 in the supplemental material).
Analytical sensitivity and amplification efficiency of L10 rRT-PCR.
The analytical sensitivity was determined based on the ability of the assay to detect RNA extracted from different titrated RPV isolates. The RPV suspensions were serially diluted in log10 steps in DMEM in duplicate and RNA was extracted from each sample and tested by rRT-PCR to determine the limit of detection (LOD), defined as the smallest detectable amount of analyte. The assay was repeated for five RPV isolates (Kabete O, Pakistan, Yemen, India, and Sokoto) that encompassed all genetic variants (Fig. 1). For each isolate, a titration curve was generated with at least three independent RNA extractions from each virus supernatant. After adjustment for extraction (140 μl) and sample volume per reaction mix (2.5 μl), the LOD values of the five representative RPV isolates ranged from 0.59 to 87.5 TCID50 per reaction (Table 6). The amplification efficiency (AE) (an indicator of the linearity and efficiency of the amplification reaction [10(−1 slope)] that optimally should be around 2, indicating the doubling of the product in each cycle), ranged from 1.95 to 2.29 (average, 2.13) with an R2 from 0.992 to 0.999 (average, 0.993), and little variability was observed among the isolates tested (Table 6, Fig. 3).
TABLE 6.
Analytical sensitivity and amplification efficiency of L10 primer-probe rRT-PCR
| Isolate | TCID50/100 μl (log10) | FAM CT | LODa (TCID50/2.5-μl reaction mix) | Amplification efficiencyb | Amplification efficiency (R2) |
|---|---|---|---|---|---|
| Kabete O | 7.63 | 19.39 | |||
| 6.63 | 23.13 | ||||
| 5.63 | 25.89 | ||||
| 4.63 | 29.04 | ||||
| 3.63 | 32.40 | ||||
| 2.63 | 35.46 | 37.3 | 2.06 | 0.999 | |
| Pakistan | 4.83 | 21.93 | |||
| 3.83 | 24.81 | ||||
| 2.83 | 27.27 | ||||
| 1.83 | 30.37 | ||||
| 0.83c | 33.69 | 0.59 | 2.29 | 0.998 | |
| Yemen | 6.0 | 20.75 | |||
| 5.0 | 23.86 | ||||
| 4.0 | 27.24 | ||||
| 3.0 | 30.35 | ||||
| 2.0 | 33.59 | ||||
| 1.0 | 35.84 | 0.88 | 2.11 | 0.997 | |
| Sokoto | 5.0 | 21.49 | |||
| 4.0 | 25.08 | ||||
| 3.0 | 28.56 | ||||
| 2.0 | 32.77 | ||||
| 1.0 | 34.84 | 0.88 | 1.95 | 0.992 | |
| India | 6.0 | 25.26 | |||
| 5.0 | 27.17 | ||||
| 4.0 | 30.03 | ||||
| 3.0 | 33.91 | 87.5 | 2.22 | 0.977 | |
| Avg | 2.13 | 0.993 |
The limit-of-detection (LOD) calculation assumes 100% viral RNA extraction recovery. RNA was extracted from undiluted, titrated tissue culture supernatant, and 10-fold serial dilutions were made of the extracted RNA. The positive CT cutoff subsequently was set at ≤35.0.
The amplification efficiency (the measure of an assay's ability to double product after each cycle) was measured as described in Materials and Methods.
For RPV Pakistan, the LOD of 100.83 is theoretical, using CT < 40 as the cutoff.
Clinical sensitivity.
The ability of the L10 rRT-PCR assay to detect RPV RNA was evaluated in clinical samples collected from six steers inoculated intramuscularly with 104 TCID50 of the Kabete O strain of RPV. All animals developed the expected clinical signs of RP disease, including fever beginning at 4 dpi, followed by excessive salivation, dental pad lesions, and ocular and nasal discharges, starting at 5 dpi. This was followed by diarrhea, depression, emaciation and dehydration, mucopurulent nasal and conjunctival discharges, and prostration by 6 to 8 dpi. All animals were euthanized when found moribund by 6 to 8 dpi. At necropsy, no significant differences in the severity of the lesions were found between animals. Clinical samples were collected from 0 to 8 dpi and in postmortem examination at 8 dpi (Table 7).
TABLE 7.
L10 rRT-PCR sensitivity on clinical samples from Kabete O RPV experimentally infected cattlea
| Sample and time point | Days p.i. | VI | rRT-PCR |
|---|---|---|---|
| In vivo | |||
| Nasal swab | 3 | 0/4 | 1/4 |
| 4 | 0/4 | 4/4 | |
| 5 | 4/4 | 4/4 | |
| Conjunctival swab | 3 | 0/4 | 2/4 |
| 4 | 3/4 | 3/4 | |
| 5 | 4/4 | 4/4 | |
| Oral swab | 3 | 0/4 | 0/4 |
| 4 | 0/4 | 2/4 | |
| 5 | 1/4 | 4/4 | |
| Rectal swab | 3 | 0/4 | 1/4 |
| 4 | 1/4 | 2/4 | |
| 5 | 2/4 | 3/4 | |
| Preputial swab | 3 | 1/2 | 2/2 |
| 4 | 2/2 | 2/2 | |
| 5 | 2/2 | 2/2 | |
| Plasma | 3 | 0/2 | 0/2 |
| 4 | 0/2 | 0/2 | |
| 5 | 0/2 | 0/2 | |
| WBC | 3 | 0/2 | 2/2 |
| 4 | 0/2 | 2/2 | |
| 5 | 1/2 | 2/2 | |
| Whole blood | 3 | 0/2 | 1/2 |
| 4 | 0/2 | 2/2 | |
| 5 | 0/2 | 2/2 | |
| Postmortem | |||
| Spleen | 6 | 6/6 | 6/6 |
| LN | 6 | 16/17 | 17/17 |
| Abomasum | 6 | 4/4 | 4/4 |
| Lingual tonsil | 6 | 2/2 | 2/2 |
| Palatine tonsil | 6 | 2/2 | 2/2 |
| Third eyelid | 6 | 2/2 | 2/2 |
| Peyer's patches | 6 | 3/3 | 3/3 |
| Gallbladder | 6 | 1/1 | 1/1 |
Results are expressed as the number of RPV rRT-PCR-positive animals out of the total number of infected animals tested. WBC, whole blood cells; LN, lymph node; p.i., postinfection; VI, virus isolation confirmed by conventional RT-PCR.
In general, the L10 rRT-PCR demonstrated preclinical diagnostic value in several samples and better sensitivity than VI. The L10 rRT-PCR was able to detect RPV antigen in conjunctival and nasal swabs as early as 3 dpi (in two and one of four infected animals, respectively) and by 5 and 4 dpi in all four cattle, respectively (Table 7). This is as early as 3 days before clinical signs were observed. These samples remained positive until the day of euthanasia (8 dpi). Preputial swabs also were positive by 3 dpi, suggesting this as a good in vivo sample. Oral swabs and rectal swabs were late positives, indicating they are not the sample of choice. Buffy coat from heparin blood seemed to be as sensitive as conjunctival and nasal swabs, with positive results by rRT-PCR at 3 dpi, which makes it an excellent in vivo sample of choice for detecting RPV before clinical signs are observed. Blood samples also are obtained as part of surveillance programs for other diseases, providing a possible surveillance tool for RPV. Postmortem samples from infected animals, such as lymph nodes, spleen, Peyer's patches, tonsils, and others, were consistently positive by rRT-PCR.
The L10 rRT-PCR test was compared to the gold-standard method of virus isolation (VI). The results showed that rRT-PCR was able to identify RPV at least 1 or 2 days before VI-positive results, with the advantage that rRT-PCR results are obtained on the same day rather than a week later, as is the case for VI (Table 7). In some cases, CPE was difficult to identify, probably due to the presence of inhibitors or toxic substances for the cell cultures in the tissue homogenates, giving inconclusive VI results that required confirmation using a conventional RPV RT-PCR test (not shown). In none of the cases was VI more sensitive than L10 rRT-PCR (Table 7).
Determination of the cycle cutoff values.
The optimum cutoff value for L10 RPV rRT-PCR was determined using samples from experimentally infected and noninfected cattle or from tissue culture. A total number of 60 known positive and 85 known negative viral samples were tested by both L10 rRT-PCR and VI followed by a conventional RT-PCR confirmatory test, as described above. The mean CT value of the tissue culture samples known to be positive was 24.58 ± 3.87, while the mean CT value of clinical specimens that were known positives was 31.96 ± 2.67 (α ≤ 0.05, t test), indicating that even the weakly positive samples were crossing the fluorescence threshold before 35 cycles. No CT values of >0.00 were detected among the 85 known negative samples after 55 cycles (data not shown), indicating the absence of false positives in that range of cycles and threshold. The DESCRIBE program of the WINPEPI statistical package (www.brixtonhealth.com) was used to calculate the best cutoff point depending on weights given to false positives (FPs) and false negatives (FNs). The resulting optimum cutoff value was 30.89 cycles for equal weights, and amplification for up to 37 cycles resulted in a sensitivity of 100% without compromising the specificity for FNs. Therefore, based on our results of known positives and known negatives, we chose 40 cycles as the cutoff to ensure maximum sensitivity.
DISCUSSION
RP has long been recognized as one of the most devastating diseases of livestock. The Global Rinderpest Eradication Program (GREP) from the Food and Agriculture Organization of the United Nations (FAO), based on the intensive vaccination of susceptible animals, has been ongoing during the last decades. As a result, there has been a significant decrease of reported outbreaks, and there is the potential of a declaration of the total eradication of RPV by 2011 (12, 23). What remains to be done now is not only to ensure that the virus is not circulating in animal populations but also to ensure that it does not escape (either deliberately or accidentally) from storage virus repositories. RPV recently has been active in many developing countries, disaster zones, and war zones that would need some monitoring for a few more years. Hence, there is a new scientific challenge following the eradication of RP, which is to maintain large-scale surveillance to avoid the reemergence of the disease within a naïve, nonvaccinated, susceptible population. Several factors point out that RP still can pose a major risk, such as (i) the proven capability of the virus to reappear after long periods of absence, as happened in 1994 and 1996, and in 2001 with RPV lineage 2 in wildlife after a period of 30 years of silence (5, 9, 12, 14, 23, 25); (ii) the fact that the most recently circulating RPV field isolates had evolved to such mild pathology that they could escape veterinary attention in remote areas (5, 9); and (iii) the difficulties of distinguishing between infected and vaccinated animals by using serological tests, seriously compromising the efforts and achievements of the successful eradication program (www.fao.org). All of these premises lead to a real need for a highly sensitive and specific diagnostic tool based on clinical observation and in vivo samples instead of necropsy findings that can detect the presence of the virus in the absence of clinical signs.
Here, we described a highly sensitive one-step rRT-PCR that is able to detect RPV with high specificity and to provide a differential diagnosis with other look-alike diseases, PPRV, and other closely related viruses. The availability of this rRT-PCR test could aid in the timely and prompt diagnosis both in the laboratory and in the field. The rRT-PCR has been proven to be easily adaptable for the high-throughput monitoring of animals and also can be used in conjunction with a whole diagnostic panel for other diseases. It is accepted to be at least as sensitive and specific as VI, if not more so, and rRT-PCR assays have been widely demonstrated to be capable of early diagnosis in many other animal viral diseases (1, 20, 24, 25). In addition, test results can be obtained in 2 to 4 h after the arrival of the samples to the laboratory and also can be adapted to the field. We compared the performance of the rRT-PCR on a variety of clinical samples from experimentally infected natural hosts and showed the suitability of this test for the early detection of the RPV RNA in conjunctival or nasal swab and blood specimens before the appearance of clinical symptoms. Blood samples and buffy coat are ideal samples either for surveillance or during an investigation case, and they allow for the detection of the antigen 2 to 3 days before clinical detection. In cases where the bleeding of animals was not feasible, nasal, oral, and/or conjunctival swabs would be samples of choice for epidemiological surveillance and investigation, allowing RPV detection 1 to 2 days earlier than VI. Finally, we confirmed previous evidence indicating the usefulness of lymph nodes as postmortem samples for diagnosis.
The detection of infected animals 1 to 3 days before clinical signs are apparent will help in culling infected animals prior to the peak of viral shedding (6). Virus isolation is widely used as the gold standard for diagnosing RPV infection but can take more than 2 weeks to generate results, allowing ample time for the spread of RPV within a herd (5, 15, 16, 18, 19, 20). VI reading sometimes is affected by the presence of inhibitors or the toxicity of the tissue homogenates, the bad preservation of the samples, and contamination with other viral, bacterial, or fungal microorganisms.
Out of five different combinations of primer sets tested in this study, only two detected all of the isolates, and just one was specific enough to distinguish RPV from the genetically close relative PPRV. We believe that this difference is not related to the ratio of concentrations of the primer pairs or some other reaction conditions, since those were independently optimized for each primer-probe set. Like other members of the mononegavirales, RPV mRNA transcription is regulated by the order of the genes in the viral genome (3′-N-P/C/V-M-F-H-L-5′). Transcription proceeds in a stepwise pattern from a single promoter at the 3′ end of the genome. Therefore, there is a decrease in the abundance of mRNAs as the polymerase complex moves away from the single promoter at the 3′ end, resulting in L being the least-abundant transcript (3). Despite this differential expression, the L primer set demonstrated better sensitivity, suggesting that sequence conservation in the L gene may play a more important role in detection than differential mRNA expression.
The L10 rRT-PCR assay did not display cross-reactions with other viruses, such as PPRV, BHV-2, BTV, BVDV, FMDV, and VSV, indicating a high degree of specificity for RPV. Although the L10 test was based on a conserved genomic area, it is possible that new variants not detectable by the assay can emerge if RPV resurfaces. In that case, further field validation will be needed to ensure the validity of this test as a diagnostic tool. In summary, the one-step L10 rRT-PCR assay described in this report is a simple, sensitive, specific, and rapid method for the detection of RPV in field samples from live or dead animals.
Supplementary Material
Acknowledgments
We acknowledge the assistance of the Animal Care Unit of PIADC and the APHIS-FADDL school staff during the animal inoculations and sampling. We thank the RSV section of FADDL-APMIS for providing the RPV and PPRV isolates used in this study. We also thank Kaitlin Rainwater-Lovett for her help with the manuscript and Dan L. Rock for facilitating the RPV sequences used in the design of the test.
Footnotes
Published ahead of print on 15 September 2010.
Supplemental material for this article may be found at http://jcm.asm.org/.
REFERENCES
- 1.Agüero, M., E. San Miguel, A. Sánchez, C. Gómez-Tejedor, and M. A. Jiménez-Clavero. 2007. A fully automated procedure for the high-throughput detection of avian infuenza virus by real-time reverse transcription-polymerase chain reaction. Avian Dis. 51:35-41. [DOI] [PubMed] [Google Scholar]
- 2.Anderson, E. 1995. Morbillivirus infections in wildlife (in relation to their population biology and disease control in domestic animals). Vet. Microbiol. 44:319-332. [DOI] [PubMed] [Google Scholar]
- 3.Baron, M. D., and T. Barrett. 1995. The sequence of the N and L genes of rinderpest virus, and the 5′ and 3′ extragenic sequences: the completion of the genome sequence of the virus. Vet. Microbiol. 44:175-185. [DOI] [PubMed] [Google Scholar]
- 4.Barrett, T., S. Subbarao, G. Belsham, and B. Mahy. 1991. The molecular biology of the morbillivirus, p. 83-102. In D. Kingsbury (ed.), The paramyxoviruses. Plenum Press, New York, NY.
- 5.Barrett, T., and P. Rossiter. 1999. Rinderpest: the disease and its impact on humans and animals. Adv. Virus Res. 53:89-110. [DOI] [PubMed] [Google Scholar]
- 6.Blood, D., O. Radostits, J. Henderson, J. Arundel, and C. Gay. 1988. Rinderpest, p. 817-821. Veterinary Medicine, ed. 5a. Bailliere Tindal, London, United Kingdom.
- 7.Callahan, J., F. Brown, F. Osorio, J. Sur, E. Kramer, G. Long, J. Lubroth, S. Ellis, K. Shoulars, K. Gaffney, D. Rock, and W. Nelson. 2002. Use of a portable real-time reverse transcriptase-polymerase chain reaction assay for rapid detection of foot-and-mouth disease virus. J. Am. Vet. Med. Assoc. 220:1636-1642. [DOI] [PubMed] [Google Scholar]
- 8.Cattaneo, R., K. Kaelin, K. Baczko, and M. A. Billiter. 1989. Measles virus editing provides an additional cysteine-rich protein. Cell 56:759-764. [DOI] [PubMed] [Google Scholar]
- 9.Daszak, P., A. Cunningham, and A. Hyatt. 2000. Emerging infectious diseases of wildlife-threats to biodiversity and human health. Science 287:443-449. [DOI] [PubMed] [Google Scholar]
- 10.Forsyth, M., and T. Barrett. 1995. Evaluation of polymerase chain reaction for the detection and characterization of rinderpest and peste des petits ruminants viruses for epidemiological studies. Virus Res. 39:151-163. [DOI] [PubMed] [Google Scholar]
- 11.Forsyth, M., S. Parida, S. Alexandersen, G. Belsham, and T. Barret. 2003. Rinderpest virus lineage differentiation using RT-PCR and SNAP-ELISA. J. Virol. Methods 107:29-36. [DOI] [PubMed] [Google Scholar]
- 12.Kock, R. A., H. M. Wamwayi, P. B. Rossiter, G. Libeau, E. Wambwa, J. Okori, F. S. Shiferaw, and T. D. Mlengeya. 2006. Re-infection of wildlife populations with rinderpest virus on the periphery of the Somali ecosystem in east Africa. Prev. Vet. Med. 75:63-80. [DOI] [PubMed] [Google Scholar]
- 13.Lund, B., A. Tiwari, S. Galbraith, M. Baron, I. Morrison, and T. Barret. 2000. Vaccination of cattle with attenuated rinderpest virus stimulates CD4+ T cell responses with broad viral A antigen specificity. J. Gen. Virol. 81:2137-2146. [DOI] [PubMed] [Google Scholar]
- 14.Mariner, J. C., and P. L. Roeder. 2003. Use of participatory epidemiology in studies of the persistence of lineage 2 rinderpest virus in east Africa. Vet. Rec. 152:641-647. [DOI] [PubMed] [Google Scholar]
- 15.Norrby, E., H. Sheshberdaran, K. Mc Cullough, W. Carpeter, and C. Orvell. 1985. Is rinderpest virus the archevirus of the morbillivirus genus? Intervirology 23:228-232. [DOI] [PubMed] [Google Scholar]
- 16.Norrby, E. 1991. Immunobiology of paramyxoviruses, p 481-507. In D. Kingsbury (ed.), The paramyxoviruses. Plenum Press, New York, NY.
- 17.Office International des Epizooties/Global Rinderpest Eradication Program. 2007. Virus isolation and identification, p. 93-106, and Differential diagnosis, p. 113-118. In J. Anderson, T. Barret, and G. R. Scott (ed.), Manual on the diagnosis of rinderpest, 2nd ed. Food and Agriculture Organization of the United Nations, Rome, Italy.
- 18.Plowright, W. 1962. Rinderpest virus. Ann. N. Y. Acad. Sci. 101:548-563. [DOI] [PubMed] [Google Scholar]
- 19.Plowright, W., and R. Ferris. 1962. Studies with Rinderpest Virus in tissue culture. A technique for the detection and titration of virulent virus in cattle tissues. Res. Vet. Sci. 3:94-104. [Google Scholar]
- 20.Plowright, W., and R. Ferris. 1957. Cytopathogenicity of rinderpest virus in tissue culture. Nature 179:316. [DOI] [PubMed] [Google Scholar]
- 21.Reed, L., and H. Muench. 1938. Simple method of estimating fifty per cent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 22.Risatti, G., J. Callahan, W. Nelson, and M. Borca. 2003. Rapid detection of classical swine fever virus by a portable real time reverse transcriptase PCR assay. J. Clin. Microbiol. 41:500-505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roeder, P. L., J. Lubroth, and P. Taylor. 2004. Experience with eradicating rinderpest by vaccination. Dev. Biol. 119:73-91. [PubMed] [Google Scholar]
- 24.Shaw, A. E., S. M. Reid, K. Ebert, G. H. Hutchings, N. P. Ferris, and D. P. King. 2007. Implementation of a one-step real-time RT-PCR protocol for diagnosis of foot-and-mouth disease. J. Virol. Methods 143:81-85. [DOI] [PubMed] [Google Scholar]
- 25.Taylor, W. P., P. L. Roeder, M. M. Rweyemamu, J. N. Melewas, P. Majuva, R. T. Kimaro, J. N. Mollel, B. J. Mtei, P. Wambura, J. Anderson, P. B. Rossiter, R. Kock, T. Melengeya, and R. Van den Ende. 2002. The control of rinderpest in Tanzania between 1997 and 1998. Trop. Anim. Health Prod. 34:471-487. [DOI] [PubMed] [Google Scholar]
- 26.Wanwayi, H. M., M. Fleming, and T. Barret. 1995. Characterisation of African isolates of rinderpest virus. Vet. Microbiol. 44:151-163. [DOI] [PubMed] [Google Scholar]
- 27.Zsak, L., M. Borca, G. Risatti, A. Zsak, R. French, Z. Lu, G. Kutish, J. Neilan, J. Callahan, W. Nelson, and D. Rock. 2005. Preclinical diagnosis of African swine fever in contact-exposed swine by a real-time PCR assay. J. Clin. Microbiol. 43:112-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.