Abstract
Context
Little is known about how health insurance status affects decisions to seek care during emergency medical conditions like acute myocardial infarction (AMI).
Objective
To examine the association between lack of health insurance and financial concerns about accessing care among those with health insurance, and the time from symptom onset to hospital presentation (prehospital delays) during AMI.
Design, Setting and Patients
Multicenter, prospective registry of 3721 AMI patients enrolled between April, 2005 and December, 2008 from 24 U.S. hospitals. Health insurance status was categorized as uninsured, insured with financial concerns about accessing care, and insured without financial concerns. Insurance information was determined from medical records while financial concerns among those with health insurance were determined from structured interviews.
Main Outcome Measure
Prehospital delay times (≤2 hours, >2 to 6 hours, >6 hours), adjusted for demographic, clinical, social and psychological factors using hierarchical ordinal regression models.
Results
Of 3,721 patients, 738 (19.8%) were uninsured, and 689 (18.5%) were insured with financial concerns, and 2294 (61.7%) were insured without financial concerns. Uninsured and insured patients with financial concerns were more likely to delay seeking care during AMI, with prehospital delays >6 hours among 48.6% of uninsured patients, 44.6% of insured patients with financial concerns, and 39.3% of insured patients without financial concerns, as compared with prehospital delays of <2 hours among 27.5%, 33.5%, and 36.6% of those who were uninsured, insured with financial concerns, and insured without financial concerns, respectively (P <.001). After adjusting for potential confounders, both insurance with financial concerns and lack of insurance were associated with prehospital delays: insurance without financial concerns (reference); insurance with financial concerns, adjusted odds ratio [OR)], 1.21; 95% confidence interval [CI]: 1.05-1.41, P=.01; no insurance, adjusted OR 1.38, 95% CI: 1.17-1.63, P <.001.
Conclusions
Lack of health insurance and financial concerns about accessing care among those with health insurance were each associated with delays in seeking emergency care for AMI.
BACKGROUND
Over 45 million Americans are without health care insurance1 and another 25 million avoid care because of financial concerns related to underinsurance.2 Although insurance status has been shown to affect use of preventive screening and chronic care,3, 4 little is known about how health care insurance affects decisions to seek care during an emergency medical condition, such as an acute myocardial infarction (AMI). While current public policy measures, such as the U.S. Emergency Medical Treatment and Active Labor Act (EMTALA), assure the provision of care during emergency medical conditions irrespective of insurance coverage, there is no guarantee that patients with health care insurance can afford such treatment.5 As a result, patients may still delay seeking care for acute, life-threatening conditions because of the potential financial costs of care.
AMI is a clinical condition for which delays in seeking care can have significant, adverse consequences on patients’ outcomes.6-9 AMI is common, affecting almost 1 million Americans each year,10 and the benefits of early treatment are clear and substantial.11, 12 Prior studies of prehospital delays for AMI have focused primarily on non-modifiable patient factors, such as age, race, and sex, and education-based community interventions to date have not been shown to reduce prehospital delays.13,14 However, studies have not examined whether financial concerns about accessing medical care, as assessed from the patient’s perspective, in those with health care insurance is associated with prehospital delays. Prior studies have defined patients with difficulty affording health care services or treatment despite having some form of health insurance as the ‘underinsured’. 15-17 Because prehospital delays are associated with higher AMI morbidity and mortality,6-9 demonstrating that patients with no insurance or those with insurance but reporting financial concerns are at higher risk for prehospital delays is important, as it would suggest that reducing financial barriers to care – perhaps through expansion of benefits or health insurance coverage – could reduce delays and improve care.
To address this current gap in knowledge, we examined the association between lack of health insurance and financial concerns about accessing care among those with health insurance, and the time from symptom onset to hospital presentation (prehospital delays) during AMI in the contemporary, multicenter Translational Research Investigating Underlying disparities in acute Myocardial infarction Patients’ Health Status (TRIUMPH) study. Given the growing number of uninsured and insured Americans with financial concerns about accessing care, an understanding of the effect of health care insurance, including the patient’s perspective, on decisions to seek prompt medical attention for AMI may have important implications in the current debate on American health care reform.
METHODS
Participants and Study Design
Participants were consecutively enrolled between April 11, 2005 and December 31, 2008 from 24 U.S. urban hospitals as part of TRIUMPH—a multi-site, prospective AMI registry focused upon specific gaps in knowledge about racial differences in AMI care. Participating hospitals within TRIUMPH were geographically diverse and included both academic and non-academic institutions (See Appendix 1 for list of sites). Patients were eligible for inclusion if they were aged ≥18 years, had elevated cardiac enzymes (troponin-I or creatinine kinase-MB) within 24 hours of hospital admission and supporting evidence suggestive of AMI, including either prolonged ischemic symptoms or electrocardiographic ST-changes. Exclusion criteria included patients who were incarcerated, refused participation, were unable to provide consent, did not speak English or Spanish, were transferred to the participating hospital from another facility >24 hours after initial admission, or expired or were discharged prior to being contacted by the investigators.
Of the 6163 patients that met eligibility criteria, 1823 patients refused to participate in the study. Compared with patients that consented, patients who refused participation were more likely to be white (74% vs. 67%, P<.001), of older age (62±14 vs. 59±12 years, P<.001), and have health insurance (85% vs. 80%, P<.001), although no difference in sex was noted (66% males vs. 67% males, P=.42). Among the 4340 patients who provided consent and were enrolled into TRIUMPH, we excluded patients with missing information on insurance status (n=63 [2%]) or in whom prehospital delay time was not documented (n= 534 [12%]) or could not be determined because they did not experience ischemic symptoms prior to hospital arrival (n=22 [0.5%]). The final study cohort consisted of 3721 patients.
Demographic, social, clinical, health status, and psychological data for patients were collected from chart abstraction and baseline interviews by trained staff within 24 to 72 hours of the index AMI admission. All participants provided written informed consent and the study protocol was approved by the institutional review board at each participating center.
Insurance Status
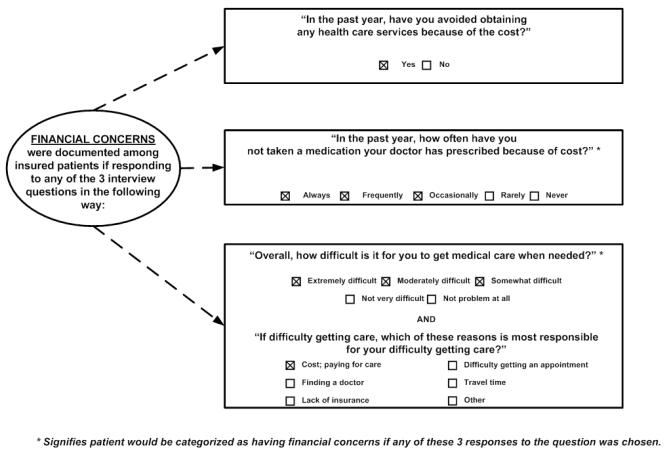
For this study, we compared 3 categories of health insurance coverage: no insurance, insurance with financial concerns about accessing care, and insurance without financial concerns. Health insurance information was determined from the medical records. In instances where patients had more than one form of health insurance, we used the following hierarchy: (1) fee-for-service (PPO), (2) health maintenance organization (HMO), (3) Medicare, (4) Medicaid, (5) Veterans Administration, (6) other, or (7) none. Patients with health care insurance were further classified using structured interviews as having or not having financial concerns in accessing medical care . Using patient-centered questions that have been used to describe economic barriers to seeking care in patients with coronary artery disease,18, 19 patients with health insurance were defined to have financial concerns in accessing care if, because of concerns about costs, they either (1) avoided care, (2) were non-adherent to medications, or (3) were unable to obtain health care services (Figure 1).
Figure 1. Study Definition of Financial Concerns in those with Health Insurance.
Insured patients in the study were categorized as having financial concerns in accessing care if, because of costs, they avoided medical care, taking medications, or had difficulties accessing care.
Study Outcomes
The primary outcome was time to hospital presentation (prehospital delays), which was determined as the time from symptom onset to hospital presentation, and was obtained from the available medical records (including all emergency department, and physician records). Time to hospital presentation was collected in the following discrete categories: ≤1 hour, >1-2 hours, >2-4 hours, >4-6 hours, >6-12 hours, >12-24 hours, and >24 hours. In order to enhance interpretability, the number of categories was reduced by merging them into the following commonly used and clinically relevant classification: ≤2 hours, >2 to 6 hours, or >6 hours.8, 9, 20 As a sensitivity analysis, we also examined time to hospital presentation using the original 7 time categories.
Demographic, Social and Patient-Centered Variables
Demographic variables included age, sex, race, and residential area. Information on race was self-identified and collected during patient interviews. Residential area was determined from the 2000 U.S. Census21 by examining the proportion of rural residents for each zip code and categorized as: a) urban (<10% rural), 2) mixed (10-33% rural), or 3) rural (>33% rural).
Additionally, during the index AMI hospitalization, detailed information on patients’ social background, health status, and psychological factors—variables which have not been systematically examined in prior studies of prehospital delays—were also obtained, as these may confound the association between insurance status and prehospital delays. Social variables included marital status (single, widowed or married), educational level (did not complete high school, high school graduate, college graduate or graduate school degree), and perceived social support as measured by the 7-item ENRICHD Social Support Inventory (ESSI). Based upon prior work,22 low social support was defined as a score of ≥3 on 2 or more items (excluding items on instrumental social support and marital status) and having a sum score of ≥18 on the remaining 5 items.
Patients’ baseline disease-specific health status (including angina frequency and angina stability over the 4 weeks preceding the index MI) was assessed using the Seattle Angina Questionnaire (SAQ), a validated disease-specific quality-of-life instrument for coronary artery disease.23 Scores for each SAQ domain range from 0 to 100, with higher scores indicating better functional status (i.e., less frequent angina and more stable angina). Angina frequency was categorized into 3 clinically meaningful categories: daily to weekly angina (scores: 0-60), monthly angina (61-99), or no angina (100).24
The TRIUMPH registry also collected information on psychological variables, including depression and perceived stress. Depression was assessed with the 9-item Patient Health Questionnaire (PHQ).25 Patients were classified as having no depression (PHQ score: 0-4), mild (PHQ, score: 5-9), and moderate to severe depression (PHQ score: 10-27).26 Levels of perceived stress were measured with the 4-item Perceived Stress Scale (PSS),27 with scores of ≥4 categorized as representing high perceived stress.28
Statistical Analysis
Unadjusted analyses evaluated baseline differences between the 3 insurance groups (uninsured, insured with financial concerns, insured without financial concerns) using analyses of variance for continuous variables and Chi-square tests for categorical variables. Normality was confirmed for continuous variables.
Because the primary outcome was ordinal, multivariable hierarchical cumulative-logit models were constructed to evaluate the independent relationship between health insurance and prehospital delay. This method adjusts for clustering at the site level and between-hospital effects and provides a single odds ratio (OR) of cumulative probabilities for the relation between a predictor variable and each combination of higher risk versus lower risk outcome categories (e.g., >6 hours vs. ≤6 hours and >2 hours vs. ≤2 hours).
Besides insurance status, all models included established predictors of prehospital delay (age, race, sex, diabetes mellitus, residential area [rural, mixed, vs. urban]),6 social factors (marital status, education level, and perceived social support), patients’ health status (SAQ angina frequency and angina stability), psychological factors (depression and perceived stress), and other clinical variables (See online Appendix 2 for definitions of clinical variables). Clinical variables included medical comorbidities (hypercholesterolemia, hypertension, peripheral arterial disease, prior AMI, prior percutaneous coronary intervention [PCI] or coronary artery bypass surgery [CABG], prior stroke, chronic kidney disease, chronic lung disease, chronic heart failure), recent smoking, obesity (body mass index ≥30), family history of coronary artery disease, AMI characteristics and severity (ST elevation vs. non-ST elevation AMI, left ventricular ejection fraction <40%, Killip class [class I/II vs. III/IV]), absence of chest pain in the prehospital setting, and time of day during hospital presentation (weekday, weeknight vs. weekend admission).
At least 1 study covariate was missing in 12.3% of patients, and the average number of missing data fields per patient was 0.23. Missing covariate data was assumed to be missing at random and imputed using IVEWARE software.29 Rates of missing delay time were not significantly different across insurance categories (P=.65) and potential bias attributable to those without prehospital delay times was addressed by creating a non-parsimonious model for the propensity of missing data on delay time.30 The reciprocal of this probability was used to weight the associations among responders in the hierarchical cumulative-logit model. Results with and without weighting were comparable, so only the weighted are presented.
As a sensitivity analysis, while time to hospital presentation was evaluated as 3 clinically meaningful time categories, we examined the relationship between insurance status and the original 7 time categories described above. Additionally, we systematically eliminated each of the 3 questions used to define insured patients with financial concerns and examined the robustness of the relationship between insurance status and prehospital delays. In all models, the validity of the ordinal relationship between insurance status and the dependent variable (i.e., the assumption of common slopes for all cumulative logits) was verified.
We also examined as secondary analyses whether prehospital delays among patients presenting with ST-elevation AMI were associated with lower rates of treatment with thrombolytic therapy or PCI using multivariable modified Poisson regression models. All analyses were conducted with SAS Version 9.1.3 (SAS Institute, Cary, NC), IVEWARE (University of Michigan, MI), and R Version 2.6.0 (Free Software Foundation, Boston, MA). All tests for statistical significance were two-tailed and evaluated at a significance level of 0.05.
RESULTS
Of 3721 patients in the cohort, 2294 (61.7%) were insured without financial concerns, while 738 (19.8%) were uninsured and 689 (18.5%) were insured but had financial concerns about accessing care. Among those with insurance reporting financial concerns,, 82.8% avoided medical care, 55.6% avoided taking medications, and 12.8% had difficulty obtaining health care services due to costs, with 44.1% meeting at least 2 of these criteria. Compared with patients without financial concerns, a greater proportion of insured patients with financial concerns received their insurance coverage from Medicaid (11.3% vs. 5.5%) and a smaller proportion had fee-for-service (43.0% vs. 52.7%) plans (P for difference across plans <.001) (Table 1).
Table 1.
Baseline Characteristics by Health Care Insurance Status.a
| Health Care Insurance Status |
||||
|---|---|---|---|---|
| Insured Without Financial Concerns (n=2294) |
Insured With Financial Concerns (n=689) |
No Insurance (n=738) |
P Value |
|
| INSURANCE PAYOR | <.001 | |||
| PPO | 1,208 (52.7) | 296 (43.0) | 0 (0.0) | |
| HMO | 345 (15.0) | 86 (12.5) | 0 (0.0) | |
| Medicare | 505 (22.0) | 160 (23.2) | 0 (0.0) | |
| Medicaid | 127 (5.5) | 78 (11.3) | 0 (0.0) | |
| Veterans Administration | 29 (1.3) | 17 (2.5) | 0 (0.0) | |
| Other | 80 (3.5) | 52 (7.5) | 0 (0.0) | |
| DEMOGRAPHICS | ||||
| Age. mean (SD), y | 61.6 (12.5) | 56.5 (11.3) | 51.7 (8.6) | < .001 |
| Female sex | 739 (32.2) | 265 (38.5) | 215 (29.1) | <.001 |
| Race | <.001 | |||
| White | 1706 (74.5) | 473 (68.8) | 337 (46.0) | |
| Black | 473 (20.7) | 177 (25.7) | 290 (39.6) | |
| Other | 110 (4.8) | 38 (5.5) | 106 (14.5) | |
| Residential areab | <.001 | |||
| Urban | 1294 (56.4) | 386 (56.1) | 521 (70.9) | |
| Mixed | 326 (14.2) | 106 (15.4) | 78 (10.6) | |
| Rural | 673 (29.4) | 196 (28.5) | 136 (18.5) | |
| SOCIO-ECONOMIC FACTORS | ||||
| Marital Status | <.001 | |||
| Married | 1367 (59.7) | 319 (46.3) | 272 (37.0) | |
| Single | 634 (27.7) | 294 (42.7) | 430 (58.4) | |
| Widowed | 288 (12.6) | 76 (11.0) | 34 (4.6) | |
| Education | <.001 | |||
| Lower than high school | 365 (6.0) | 172 (25.1) | 204 (27.7) | |
| High school | 1338 (58.8) | 411 (59.9) | 439 (59.6) | |
| College | 350 (15.4) | 73 (10.6) | 73 (9.9) | |
| Graduate school | 223 (9.8) | 30 (4.4) | 20 (2.7) | |
| PSYCHOLOGICAL FACTORS | ||||
| Depression (PHQ) | <.001 | |||
| Not clinically depressed | 1347 (62.3) | 264 (41.4) | 389 (56.1) | |
| Mild | 509 (23.5) | 186 (29.2) | 157 (22.7) | |
| Moderate | 185 (8.6) | 106 (16.6) | 84 (12.1) | |
| Moderately severe | 87 (4.0) | 55 (8.6) | 49 (7.1) | |
| Severe | 34 (1.6) | 26 (4.1) | 14 (2.0) | |
| Perceived stress | <.001 | |||
| Low perceived stress | 1185 (53.4) | 193 (28.8) | 270 (37.4) | |
| High perceived stress | 1035 (46.6) | 47 (71.2) | 451 (62.6) | |
| Low social support | 259 (11.7) | 188 (28.3) | 168 (23.2) | <.001 |
| HEALTH STATUS | ||||
| SAQ angina frequency | <.001 | |||
| Daily or weekly | 340 (14.9) | 131 (19.0) | 142 (19.3) | |
| Monthly | 640 (28.0) | 220 (32.0) | 221 (30.1) | |
| None | 1307 (57.1) | 337 (49.0) | 372 (50.6) | |
| SAQ Angina stability, mean (SD) | 45.7 (20.9) | 42.7 (23.2) | 42.9 (22.8) | <.001 |
| MEDICAL HISTORY | ||||
| Hypercholesterolemia | 1230 (53.6) | 344 (49.9) | 262 (35.5) | <.001 |
| Hypertension | 1546 (67.4) | 473 (68.7) | 444 (60.2) | <.001 |
| Peripheral arterial disease | 129 (5.6) | 28 (4.1) | 11 (1.5) | <.001 |
| Diabetes mellitus | 656 (28.6) | 246 (35.7) | 205 (27.8) | <.001 |
| Prior MI | 479 (20.9) | 173 (25.1) | 116 (15.7) | <.001 |
| Prior PCI or CABG | 625 (27.2) | 220 (31.9) | 122 (16.5) | <.001 |
| Prior stroke | 135 (5.9) | 35 (5.1) | 17 (2.3) | <.001 |
| Chronic kidney disease | 173 (7.5) | 48 (7.0) | 24 (3.3) | <.001 |
| Chronic lung disease | 167 (7.3) | 54 (7.8) | 27 (3.7) | <.001 |
| Chronic heart failure | 161 (7.0) | 76 (11.0) | 49 (6.6) | 0.001 |
| Smoked within last 30 days | 1256 (54.8) | 452 (65.6) | 520 (70.5) | <.001 |
| Obese (BMI ≥ 30) | 891 (40.1) | 311 (46.3) | 271 (41.2) | 0.02 |
| Family history of CAD | 1716 (75.6) | 522 (76.9) | 505 (69.0) | <.001 |
| CLINICAL FEATURES MI ADMISSION | ||||
| ST-segment elevation MI | 1040 (45.3) | 307 (44.6) | 329 (44.6) | 0.90 |
| Ejection fraction <40% | 371 (18.8) | 115 (19.6) | 153 (24.9) | 0.004 |
| Killip class | 0.12 | |||
| I or II | 2240 (98.6) | 672 (98.5) | 715 (97.5) | |
| III or IV | 31 (1.4) | 10 (1.5) | 18 (2.5) | |
| No arrival chest pain | 233 (10.3) | 50 (6.5) | 37 (4.5) | <.001 |
| Time of hospital arrival | 0.30 | |||
| Weekday | 850 (37.1) | 253 (36.8) | 284 (38.5) | |
| Weeknight | 694 (30.3) | 226 (32.8) | 241 (32.7) | |
| Weekend | 748 (32.6) | 209 (30.4) | 213 (28.9) | |
Values are expressed as number (percentage) unless otherwise indicated.
Residential area was determined by the proportion of rural residents for each zip code from the 2000 U.S. Census21 and categorized as: a) urban (<10% rural), 2) mixed (10-33% rural), or 3) rural (>33% rural).
Abbreviations: BMI, body mass index (kilograms per meters squared); CABG, coronary artery bypass grafting; CAD, coronary artery disease; HMO, health maintenance organization; MI, myocardial infarction; PCI, percutaneous coronary interventions; PHQ, Patient Health Questionnaire; PPO, Preferred Provider Organization; SAQ, Seattle Angina Questionnaire.
There were substantial differences in baseline characteristics between the 3 insurance groups (Table 1). Compared with insured patients without financial concerns, uninsured patients and insured patients with financial concerns were more frequently younger, non-white, single, and current smokers, and less likely to have completed high school. These patients also had higher levels of perceived stress, more severe depressive symptoms, and more frequent angina in the weeks preceding their index AMI. Furthermore, as compared with patients with any insurance, uninsured patients were less likely to have had a prior AMI, PCI or CABG; less likely to have coexisting hypercholesterolemia, hypertension, peripheral arterial disease, stroke, chronic kidney disease, and chronic lung disease; and more likely to live in urban areas and present with a left ventricular ejection fraction <40% during the index AMI.
Delays to Hospital Presentation
While 1273 (34.2%) patients presented promptly within 2 hours of symptom onset, the largest proportion of patients (n=1567, 42.1%) had delay times exceeding 6 hours. There were important differences in time from symptom onset to hospital presentation during AMI by insurance status (P <.001) (Table 2). A greater proportion (36.6%) of insured patients without financial concerns arrived ≤2 hours of symptom onset compared with 33.5% of insured patients with financial concerns, and 27.5% of uninsured patients. Conversely, a smaller proportion (39.3%) of insured patients without financial concerns arrived >6 hours from symptom onset, as compared with 44.6% of insured patients with financial concerns, and 48.6% of uninsured patients.
Table 2.
Hospital Presentation Times By Health Care Insurance Status.a
| Health Care Insurance Status |
||||
|---|---|---|---|---|
| Insured Without Financial Concerns (n=2294) |
Insured With Financial Concerns (n=689) |
No Insurance (n=738) |
P Value |
|
| TIME TO HOSPITAL PRESENTATION, n (%) | <.001 | |||
| ≤ 2 hours | 839 (36.6) | 231 (33.5) | 203 (27.5) | |
| > 2 to 6 hours | 554 (24.1) | 151 (21.9) | 176 (23.8) | |
| > 6 hours | 901 (39.3) | 307 (44.6) | 359 (48.6) | |
Values are presented as number (percentage).
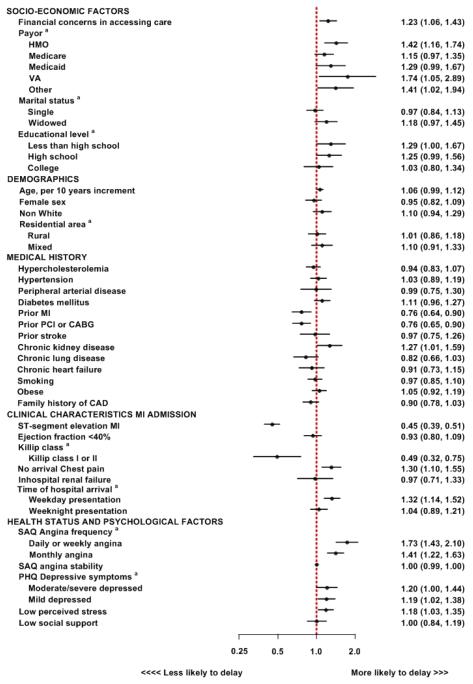
In unadjusted analyses, as compared with insured patients without financial concerns, insured patients with financial concerns (unadjusted OR, 1.22; 95% confidence interval [CI], 1.06-1.40) and uninsured patients (unadjusted OR, 1.30; 95% CI, 1.12-1.51) were more likely to delay seeking care during AMI. After adjustment for demographics, clinical comorbidities, AMI characteristics, baseline health status, social factors, and psychosocial variables, insured patients with financial concerns (adjusted OR 1.21; 95% CI, 1.05-1.41; P=.01) and uninsured patients (adjusted OR 1.38; 95% CI, 1.17-1.63; P<.001) continued to have longer times to hospital presentation (Table 3). In sensitivity analyses, these estimates were similar when prehospital delay was examined as 7 distinct time categories (results not shown). Moreover, because patients with managed-care or public insurance plans were also more likely to have prehospital delays (Appendix 3A), we additionally adjusted for payor type in the subgroup of patients with any insurance and found that the relationship with longer delay times remained similar for insured patients with financial concerns: adjusted OR, 1.23, 95% CI, 1.06-1.43, P=.008 (Appendix 3B). Finally, we found that the relationship between insurance status and prehospital delays was similar when we systematically eliminated each of the criterion questions used to define financial concerns among those with health insurance (See Appendix 4)
Table 3. Association Between Insurance Status and Prehospital Delays.
The effect of sequential adjustments for demographic, clinical, and psychosocial variables on the relationship between (1) insurance with financial concerns and (2) no insurance, with prehospital delays is depicted. The odds ratio (OR) reflects the cumulative probabilities of hospital presentation times of >6 hours vs. ≤6 hours and >2 hours vs. ≤2 hours.
| Adjusted for a | OR (95% CI) |
P Value |
|---|---|---|
| Unadjusted except for site | ||
| Insured With Financial Concerns | 1.22 (1.06, 1.40) | .005 |
| No insurance | 1.30 (1.12, 1.51) | <.001 |
| Adjusted for site, age, gender, race, and residential area | ||
| Insured With Financial Concerns | 1.27 (1.10, 1.47) | <.001 |
| No insurance | 1.44 (1.23, 1.68) | <.001 |
| Adjusted for site, age, gender, race, residential area, comorbidities, and clinical characteristics | ||
| Insured With Financial Concerns | 1.25 (1.08, 1.45) | .003 |
| No insurance | 1.41 (1.20, 1.66) | <.001 |
| Adjusted for site, age, gender, race, residential area, comorbidities, clinical characteristics, baseline CAD health status, social and psychological factors | ||
| Insured With Financial Concerns | 1.21 (1.05, 1.41) | .01 |
| No insurance | 1.38 (1.17, 1.63) | <.001 |
Reference group = insured without financial concerns.
Abbreviations: CAD, coronary artery disease; CI, confidence interval; OR, odds ratio.
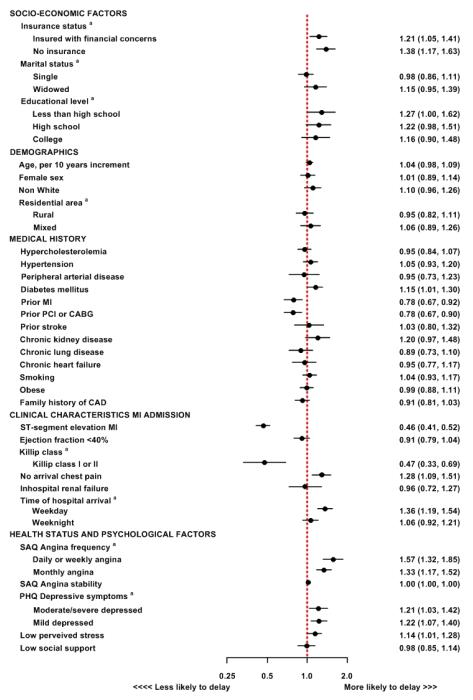
The final model results for prehospital delays are presented in Figure 2. Consistent with prior studies,6, 7, 9 coexisting diabetes mellitus and weekday working hours were associated with an increased risk of prehospital delays, while a low Killip Class, a prior history of AMI, or prior coronary revascularization were each associated with shorter delay times. However, previously described associations between age, female sex, and black race with prehospital delays6, 7, 9 were attenuated after adjustment for insurance status, social and psychological factors, as well as clinical characteristics. Notably, lower educational level, higher angina frequency in the weeks preceding the AMI, and depressive symptoms were associated with prehospital delays, whereas patients with higher perceived stress scores were more likely to present promptly (See Figure 2).
Figure 2. Adjusted Cumulative Probabilities for Covariates in Final Multivariable Model for Prehospital Delays.
Odds ratios in the model represent cumulative probabilities between a predictor variable and each combination of higher risk versus lower risk outcome categories (e.g., >6 hours vs. ≤6 hours and >2 hours vs. ≤2 hours). Error bars denote 95% confidence intervals. Abbreviations: CABG, coronary artery bypass grafting; CAD, coronary artery disease; MI, myocardial infarction; PCI, percutaneous coronary interventions; SAQ, Seattle Angina Questionnaire. a Reference categories for the following variables: (1) Insurance status: Insured without financial concerns; (2) Marital status: Married; (3) Educational level: Graduate School; (4) Residential area: Urban; (5) Killip class: Killip class III or IV; (6) Time of hospital arrival: Weekend; (7) SAQ Angina frequency: No angina; (8) PHQ Depressive symptoms: Not depressed.
Finally, among patients presenting with ST-elevation AMI, those with prehospital delays exceeding 6 hours were less likely to receive primary reperfusion therapy with either thrombolytics or percutaneous coronary intervention: ≤2 hours (reference group), 93.5%; >2 to 6 hours, 92.5%, adjusted Relative Risk (RR), 1.00, 95% CI, 0.97-1.04, P=.88; >6 hours, 83.9%; adjusted RR, 0.91, 95% CI, 0.85-0.96; P=.002 (Table 4).
Table 4.
Impact of Time to Hospital Presentation on Subsequent Treatment in Patients with ST-elevation Myocardial Infarction.a
| PCI |
Thrombolysis |
PCI or Thrombolysis |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prehospital Delay | N (%) | RR | 95CI% | P-value | N (%) | RR | 95%CI | P-value | N (%) | RR | 95%CI | P-value |
| ≤ 2 hours (n=749) | 680 (90.8) | [Reference Category] | 116 (15.5) | [Reference Category] | 700 (93.5) | [Reference Category] | ||||||
| > 2-6 hours (n=400) | 356 (89.0) | 1.00 | 0.95-1.04 | .83 | 59 (14.8) | 0.93 | 0.63-1.36 | .69 | 370 (92.5) | 1.00 | 0.97-1.04 | .88 |
| > 6 hours (n=527) | 430 (81.6) | 0.90 | 0.84-0.95 | <.001 | 39 (7.4) | 0.61 | 0.48-0.77 | <.001 | 442 (83.9) | 0.91 | 0.85-0.96 | .002 |
Adjusted for site, age, gender, race, residential area, comorbidities, clinical characteristics, baseline CAD health status, and psychosocial factors.
Abbreviations: CI, confidence interval; PCI, percutaneous coronary interventions, RR, relative risk.
DISCUSSION
In this prospective, multi-site, AMI registry, we found that nearly 2 in every 5 patients were uninsured or were insured but reported financial concerns in accessing care. These patients, in turn, were more likely to delay seeking emergency care for an AMI, even after extensive adjustment for clinical, social, and psychological factors. These findings underscore important consequences from inadequate health care insurance coverage for the substantial number of Americans experiencing AMIs and suggest that efforts to reduce prehospital delay times may have limited impact without first ensuring that access to health insurance is improved and that financial concerns are addressed in patients who seek emergency care.
To our knowledge, this study is the first to demonstrate an association between the lack of health care insurance and prehospital delays during AMI. While this observation may seem intuitive, uninsured patients have not been previously found to have higher rates of prehospital delays.31, 32 Our findings on insurance status may have differed from earlier studies because of a higher proportion of uninsured patients in this contemporary registry. Moreover, our study’s use of patient interviews, rather than administrative data, allowed us to adjust for patients’ health status and important social and psychological confounders to better clarify the independent association of insurance status with prehospital delays in AMI.
Perhaps most importantly, our study was also able to evaluate the impact of financial concerns in accessing medical care among those with insurance on delays in seeking care. Through detailed, structured interviews, we identified individuals who reported financial burdens related to use of health care services despite the presence of insurance. This process utilized a patient’s perspective and is a significant advance from the use of coarse administrative data sources. Remarkably, more than half of all insured patients with financial concerns in our study had fee-for-service or health maintenance organization insurance plans. Thus, having private health care insurance did not guarantee use of health care services that were essential for these patients, perhaps because they perceived them as unaffordable in the face of competing financial demands.
Several studies have previously described patients who forego routine medical treatment because of high cost burden as the ‘underinsured’.15-17, 19, 33 Such avoidance of care due to costs was associated with more angina, poorer health status, and higher rates of rehospitalization.19, 33 While underinsurance has not been well-studied to date, this group represents a growing U.S. patient population susceptible to disparities in care for emergent conditions like AMI. In this study, we were able to show an association between financial concerns in accessing care among insured patients and delays to hospital presentation. However, we did not have sufficiently detailed information on patients’ health insurance plans or preferences in decision-making to determine whether perceived financial concerns among those with insurance were due to underinsurance or personal choices to forego broader insurance coverage plans for lower premiums. To further inform health-policy decision-making, however, additional studies are required to determine whether and which aspects of underinsurance—high out-of-pocket health care costs (copayments, coinsurance, deductibles), low lifetime health benefit ceilings, or lack of catastrophic or stop-loss provisions—may be responsible for perceived cost burden.
The finding that uninsured and insured patients with financial concerns about accessing medical treatment delay seeking care for potentially fatal but treatable medical conditions raises particular concerns, as the majority of these families in the U.S. are the ‘working poor’, often with 2 full-time workers in the household.1, 4, 34 The inability to address patients’ concerns about costs of emergency care may, in part, explain the failure of prior intervention studies to reduce prehospital delay times during AMI.14, 35 Moreover, because black and female patients are more likely to face financial concerns in accessing medical care despite insurance or be uninsured,19 addressing insurance coverage has the potential to reduce disparities in care for these vulnerable populations. In fact, we found that previously described associations between race, age, and sex—which are largely non-modifiable demographic characteristics—with prehospital delays7, 9 were substantially attenuated after adjustment for insurance status and other social, psychological, and clinical variables in this study.
It is likely that uninsured patients and insured patients with financial concerns about accessing care not only delay seeking care for AMI, but also for other common medical conditions, such as stroke, pneumonia, and appendicitis.36 As a result, interventions that broaden and ensure the affordability of health insurance coverage in the U.S. may reduce times to presentation for all emergent medical conditions. Such policy interventions are particularly important in light of a recent analysis that found that as many as 45,000 deaths annually in the U.S. are attributable to lack of health insurance alone.37 These interventions would also address critics of EMTALA, who argue that the legislation’s unfunded mandate over the past 2 decades has imposed undue economic burdens on hospitals and paradoxically decreased the availability of emergency care services that the law was intended to promote.38, 39
Finally, our study also provides insights into other novel, and potentially modifiable, patient characteristics associated with prehospital delays during AMI that are distinct from previously described—but often non-modifiable—predictors, such as age, sex, race, diabetes mellitus, and absence of chest pain. Specifically, we found an association between lower educational level, recent angina, and depressive symptoms with prehospital delays. In contrast, high levels of perceived stress were associated with shorter times to hospital presentation. Since large community-based education programs for AMI in the U.S. have not been previously successful in reducing times from symptom onset to hospital presentation,14, 35, 40 future educational public health efforts may need to address these specific predictors, in addition to insurance status, in developing new interventions.
Our study should be interpreted in the context of the following limitations. Delay times were not documented in the medical records in 12% of patients and we did not have a mechanism to validate delay times reported in the medical records. However, documenting delay times by patients’ recall has been widely employed in other studies and rates of missing delay times in this study did not differ from prior studies.7, 9 Importantly, rates of missing delay times were similar across insurance groups and were accounted for in our propensity-weighted analyses.
Second, while our models adjusted for an extensive number of demographic, social, clinical, and psychological factors, we did not have information on other factors that may have influenced prehospital delay times, including the use of Emergency Medical Services for hospital transport, geographical distance from site of ischemic symptom occurrence to presenting hospital, and traffic patterns in urban and rural areas. Moreover, we did not have information on each patient’s annual hospital expenditures, deductibles, medical co-payments, and covered medical benefits to directly assess underinsurance, nor did we have information on annual household income and expenses to determine the extent to which perceived financial concerns about accessing care were due to limited disposable income rather than patients’ conscious choices to forego broad insurance coverage in exchange for lower premiums.
Third, while we found that the uninsured and the insured with financial concerns were associated with delays, nearly 2 in 5 insured patients without financial concerns also had delays to hospital presentation exceeding 6 hours. This suggests that other patient factors accounted for prehospital delays, and improving health insurance coverage, while important, is but one component in a comprehensive strategy to reduce times to hospital presentation during AMI. Fourth, our cohort was drawn from a sample of 24 urban hospitals throughout the U.S. and may not be generalizable to other sites or regions. Lastly, our study cohort does not include patients who never sought care or who died before hospitalization. Since we found that uninsured and insured patients with financial concerns had greater delays in seeking treatment, our estimates are likely to be conservative estimates of the association between insurance status and prehospital delay for AMI.
In conclusion, in this large multicenter registry, we found that patients with either no insurance or insured patients with financial concerns about accessing medical treatment were more likely to delay seeking emergency care for AMI, a commonly occurring condition. Efforts to reduce prehospital delays for AMI, as well as for other emergency conditions, may have limited impact unless U.S. health care insurance coverage is extended and improved.
Acknowledgements
Funding Sources
The TRIUMPH study was supported by grants from the National Heart, Lung, and Blood Institute Specialized Center of Clinically Oriented Research in Cardiac Dysfunction and Disease (grant no. P50 HL077113) and Cardiovascular Therapeutics, Palo Alto, California.
Dr. Ross is currently supported by the National Institute on Aging (K08 AG032886) and by the American Federation of Aging Research through the Paul B. Beeson Career Development Award Program.
Mr. Rathore is supported, in part, by CTSA Grant Number UL1 RR024139 from the National Institutes of Health’s Center for Research Resources, the National Institute of General Medical Sciences Medical Scientist Training Program grant 5T32GM07205, and an Agency for Healthcare Research and Quality Dissertation Grant (1R36HS01828301).
The funding organizations and sponsors of the study had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
APPENDIX 1. Sites and Investigators Participating in TRIUMPH
Saint Luke’s Mid America Heart Institute is the TRIUMPH Coordinating Center and members of the Cardiovascular Outcomes Research Consortium participating in this study included: Barnes Jewish Hospital/Washington University, Saint Louis, MO – Richard Bach MD; Bridgeport Hospital, Bridgeport, CT – Stuart Zarich MD; Christiana Care Health System, Newark, DE – William Weintraub MD; Denver General Health System, Denver, CO – Frederick Masoudi MD MSPH, Edward Havranek MD; Duke University, Durham, NC – Karen Alexander MD, Eric Peterson MD MPH; Grady Health Systems/Emory University, Atlanta, GA – Susmita Parashar MD MPH MS, Viola Vaccarino MD PhD; Henry Ford Hospital, Detroit, MI – Aaron Kugelmass MD, David Lanfear MD; John H. Stroger Jr. Hospital of Cook County, Chicago IL –Amit Amin MD, Sandeep Nathan MD, Russell Kelley MD ; Leonard J. Chabert Medical Center, Houma, LA – Lee Arcement MD MPH; MeritCare Medical System, Fargo ND – Walter Radtke MD, Thomas Haldis MD; Montefiore Medical Center, Bronx, NY – V.S. Srinivas MD; Presbyterian Hospital, Albuquerque, NM – Dan Friedman MD; Saint Luke’s Mid America Heart Institute, Kansas City, MO – John Spertus MD MPH; Sentara Health System (both Sentara and Sentara Leigh Hospitals), Norfolk, VA – John E. Brush Jr. MD, Truman Medical Center and the University of Missouri – Kansas City, Kansas City, MO – Mukesh Garg MD, Darcy Green Conaway MD; Tufts-New England Medical Center, Boston MA – Jeffrey T. Kuvin MD; University of Colorado Health System, Denver, CO – John Rumsfeld MD PhD, John Messenger MD; University of Iowa, Iowa City, IA – Phillip Horwitz MD; University of Michigan Health Systems, Ann Arbor, MI – Brahmajee Nallamothu MD MPH; University of Texas Southwestern, Dallas, TX – Darren McGuire MD MHSc; VA Iowa City Health Care System, Iowa City, IA – Phillip Horwitz MD; Virginia Commonwealth University, Richmond, VA – Michael C. Kontos MD; Yale University/Yale-New Haven Hospital, New Haven, CT – Harlan Krumholz MD.
APPENDIX 2. Data Definitions of Clinical Variables
Clinical variables were obtained by medical chart abstraction at enrolment, unless otherwise specified, and included:
|
Documented from Baseline Patient Interview
APPENDIX 3. Association Between Insurance Status and Prehospital Delays After Adjusting for Insurance Payor Type
Among those with insurance, patients with managed-care or public insurance plans were more likely to have prehospital delays (Appendix 3A). However, additional adjustment for payor type in the multivariable models did not meaningfully change the association between insured patients with financial concerns about accessing care and prehospital delays (Appendix 3B).
Appendix 3A.
| Time from Symptom Onset to Arrival |
|||||
|---|---|---|---|---|---|
| Payor Type* | ≤ 2 hours n = 1070 |
>2 to 6 hours n = 704 |
> 6 hours n = 1208 |
Unadjusted OR (95% CI) |
P Value |
| Commercial/PPO | 646 (60.4) | 325 (46.2) | 533 (44.1) | Reference | Reference |
| HMO | 123 (11.5) | 109 (15.5) | 199 (16.5) | 1.41 (1.16-1.71) | <.001 |
| Medicare | 192 (17.9) | 181 (25.7) | 291 (24.1) | 1.49 (1.28-1.73) | <.001 |
| Medicaid | 58 (5.4) | 53 (7.5) | 94 (7.8) | 1.56 (1.23-1.99) | <.001 |
| VA | 14 (1.3) | 7 (1.0) | 25 (2.1) | 2.06 (1.26-3.36) | .004 |
| Other | 37 (3.5) | 29 (4.1) | 66 (5.5) | 1.54 (1.13-2.10) | .006 |
Patients without health insurance were excluded in this analysis.
Appendix 3B.
Multivariable Model for Patients with Insurance, Adjusted for Payor Type.
 |
Reference category for Payor: PPO. See legend as for Figure 2 for further details.
APPENDIX 4. Results of Sensitivity Analyses
The impact of systematically eliminating each of the 3 questions used to define financial concerns among those with insurance in sensitivity analyses is presented in the following tables.
Appendix 4A.
Number of patients in the insurance groups when each criterion used to define financial concerns among those with insurance was systematically eliminated.
| (1) Avoided health care services because of cost |
(2) Not taken medication as prescribed because of cost |
(3) Difficulties getting medical care because of cost |
Number of patients |
|||
|---|---|---|---|---|---|---|
| Insured Without Financial Concerns |
Insured With Financial Concerns |
No insurance |
||||
|
Meeting all 3 criteria |
X | X | X | 2294 | 689 | 738 |
|
Eliminating criterion no. 1 |
X | X | 2548 | 435 | 738 | |
|
Eliminating criterion no. 2 |
X | X | 2396 | 587 | 738 | |
|
Eliminating criterion no. 3 |
X | X | 2323 | 660 | 738 | |
Appendix 4B. Adjusted Model Estimates of the Association Between Insurance Status and Prehospital Delays Using Alternative Definitions of ‘Insured with Financial Concerns’. .
Reference group = insured without financial concerns.
| Underinsurance definition | OR (95% CI) | P Value |
|---|---|---|
| Meeting all 3 criteria (Main Study Findings) | ||
| Insured With Financial Concerns | 1.21 (1.05-1.41) | .01 |
| No insurance | 1.38 (1.17-1.63) | <.001 |
| Eliminating “Avoided health care services because of cost” | ||
| Insured With Financial Concerns | 1.23 (1.03-1.47) | .02 |
| No insurance | 1.38 (1.17-1.63) | <.001 |
| Eliminating “Not taken medication as prescribed because of cost” | ||
| Insured With Financial Concerns | 1.26 (1.07-1.48) | <.01 |
| No insurance | 1.40 (1.19-1.66) | <.001 |
| Eliminating “Difficulties getting medical care because of cost” | ||
| Insured With Financial Concerns | 1.19 (1.02-1.39) | .02 |
| No insurance | 1.39 (1.18-1.64) | <.001 |
Adjusted for site, age, gender, race, residential area, comorbidities, clinical characteristics, baseline CAD health status, and psychosocial factors.
Footnotes
Data Access and Responsibility Dr. Chan had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflicts of Interest and Disclosures Dr. Spertus developed and owns the copyrights for the Seattle Angina Questionnaire. All other co-authors report no disclosures or conflicts of interest.
Authorship: Dr. Chan had full access to all of the data, and takes responsibility for the integrity of the data and the accuracy of the data analysis. Specific contributions by individual authors are described below:
Study Concept and design: Smolderen, Spertus, Chan.
Acquisition of Data: Spertus, Chan.
Analysis and interpretation of data: Smolderen, Spertus, Nallamothu, Krumholz, Tang, Ross, Ting, Alexander, Rathore, Chan.
Drafting of the manuscript: Smolderen, Chan.
Critical revision of the manuscript for important intellectual content: Smolderen, Spertus, Nallamothu, Krumholz, Tang, Ross, Ting, Alexander, Rathore, Chan.
Statistical Analysis: Tang, Jones.
Study Supervision: Smolderen, Spertus, Nallamothu, Krumholz, Tang, Ross, Ting, Alexander, Rathore, Chan.
References
- 1.Kaiser Commission on Medicaid and the Uninsured [Accessed February 3, 2010];The Uninsured: A Primer. 2006 January; at http://www.kff.org/uninsured/7451.cfm.
- 2.Gabel JR, McDevitt R, Lore R, Pickreign J, Whitmore H, Ding T. Trends in underinsurance and the affordability of employer coverage, 2004-2007. Health Aff (Millwood) 2009;28:w595–606. doi: 10.1377/hlthaff.28.4.w595. [DOI] [PubMed] [Google Scholar]
- 3.Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061–9. doi: 10.1001/jama.284.16.2061. [DOI] [PubMed] [Google Scholar]
- 4.Ross JS, Bradley EH, Busch SH. Use of health care services by lower-income and higher-income uninsured adults. JAMA. 2006;295:2027–36. doi: 10.1001/jama.295.17.2027. [DOI] [PubMed] [Google Scholar]
- 5.EMTALA Emergency Medical Treatment and Labor Act of 1986. Public Law. pp. 99–272.
- 6.Moser DK, Kimble LP, Alberts MJ, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on cardiovascular nursing and stroke council. Circulation. 2006;114:168–82. doi: 10.1161/CIRCULATIONAHA.106.176040. [DOI] [PubMed] [Google Scholar]
- 7.Ting HH, Bradley EH, Wang Y, et al. Factors associated with longer time from symptom onset to hospital presentation for patients with ST-elevation myocardial infarction. Arch Intern Med. 2008;168:959–68. doi: 10.1001/archinte.168.9.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. Decade-long trends and factors associated with time to hospital presentation in patients with acute myocardial infarction: the Worcester Heart Attack study. Arch Intern Med. 2000;160:3217–23. doi: 10.1001/archinte.160.21.3217. [DOI] [PubMed] [Google Scholar]
- 9.Sheifer SE, Rathore SS, Gersh BJ, et al. Time to presentation with acute myocardial infarction in the elderly: associations with race, sex, and socioeconomic characteristics. Circulation. 2000;102:1651–6. doi: 10.1161/01.cir.102.14.1651. [DOI] [PubMed] [Google Scholar]
- 10.Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics--2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:e21–181. doi: 10.1161/CIRCULATIONAHA.108.191261. [DOI] [PubMed] [Google Scholar]
- 11.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 12.Andersen HR, Nielsen TT, Rasmussen K, et al. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N Engl J Med. 2003;349:733–42. doi: 10.1056/NEJMoa025142. [DOI] [PubMed] [Google Scholar]
- 13.Ting HH, Bradley EH, Wang Y, et al. Delay in presentation and reperfusion therapy in ST-elevation myocardial infarction. Am J Med. 2008;121:316–23. doi: 10.1016/j.amjmed.2007.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dracup K, McKinley S, Riegel B, et al. A randomized clinical trial to reduce patient prehospital delay to treatment in acute coronary syndrome. Circ Cardiovasc Qual Outcomes. 2009;2:524–32. doi: 10.1161/CIRCOUTCOMES.109.852608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Keeler E. Effects of cost sharing on use of medical services and health. J Med Pract Manag. 1992;8:317–21. [Google Scholar]
- 16.Blewett LA, Ward A, Beebe TJ. How much health insurance is enough? Revisiting the concept of underinsurance. Med Care Res Rev. 2006;63:663–700. doi: 10.1177/1077558706293634. [DOI] [PubMed] [Google Scholar]
- 17.Weinick RM, Byron SC, Bierman AS. Who can’t pay for health care? J Gen Intern Med. 2005;20:504–9. doi: 10.1111/j.1525-1497.2005.0087.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spertus J, Decker C, Woodman C, et al. Effect of difficulty affording health care on health status after coronary revascularization. Circulation. 2005;111:2572–8. doi: 10.1161/CIRCULATIONAHA.104.474775. [DOI] [PubMed] [Google Scholar]
- 19.Rahimi AR, Spertus JA, Reid KJ, Bernheim SM, Krumholz HM. Financial barriers to health care and outcomes after acute myocardial infarction. JAMA. 2007;297:1063–72. doi: 10.1001/jama.297.10.1063. [DOI] [PubMed] [Google Scholar]
- 20.Vogel RA. HCFA’s Cooperative Cardiovascular Project: a nationwide quality assessment of acute myocardial infarction. Clin Cardiol. 1994;17:354–6. doi: 10.1002/clc.4960170703. [DOI] [PubMed] [Google Scholar]
- 21.U.S. Census Bureau [Accessed February 3, 2010]; at http://factfinder.census.gov/home/saff/main.html?_lang=en.
- 22.Enhancing recovery in coronary heart disease patients (ENRICHD): study design and methods. The ENRICHD investigators. Am Heart J. 2000;139:1–9. doi: 10.1016/s0002-8703(00)90301-6. [DOI] [PubMed] [Google Scholar]
- 23.Spertus JA, Winder JA, Dewhurst TA, et al. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25:333–41. doi: 10.1016/0735-1097(94)00397-9. [DOI] [PubMed] [Google Scholar]
- 24.Spertus JA, Salisbury AC, Jones PG, Conaway DG, Thompson RC. Predictors of quality-of-life benefit after percutaneous coronary intervention. Circulation. 2004;110:3789–94. doi: 10.1161/01.CIR.0000150392.70749.C7. [DOI] [PubMed] [Google Scholar]
- 25.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 26.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 28.Otte C, McCaffery J, Ali S, Whooley MA. Association of a serotonin transporter polymorphism (5-HTTLPR) with depression, perceived stress, and norepinephrine in patients with coronary disease: the Heart and Soul Study. Am J Psychiatry. 2007;164:1379–84. doi: 10.1176/appi.ajp.2007.06101617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Raghunathan TE, Solenberger PW, Van Hoeyk J. IVEware: Imputation and Variance Estimation Software - User Guide. Survey Research Center, Institute for Social Research University of Michigan; Michigan: 2002. [Google Scholar]
- 30.Lunceford JK, Davidian M. Stratification and weighting via the propensity score in estimation of causal treatment effects: a comparative study. Stat Med. 2004;23:2937–60. doi: 10.1002/sim.1903. [DOI] [PubMed] [Google Scholar]
- 31.Foraker RE, Rose KM, McGinn AP, et al. Neighborhood income, health insurance, and prehospital delay for myocardial infarction: the atherosclerosis risk in communities study. Arch Intern Med. 2008;168:1874–9. doi: 10.1001/archinte.168.17.1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McGinn AP, Rosamond WD, Goff DC, Jr., Taylor HA, Miles JS, Chambless L. Trends in prehospital delay time and use of emergency medical services for acute myocardial infarction: experience in 4 US communities from 1987-2000. Am Heart J. 2005;150:392–400. doi: 10.1016/j.ahj.2005.03.064. [DOI] [PubMed] [Google Scholar]
- 33.Tamblyn R, Laprise R, Hanley JA, et al. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA. 2001;285:421–9. doi: 10.1001/jama.285.4.421. [DOI] [PubMed] [Google Scholar]
- 34.Steinbrook R. Health care reform in Massachusetts--a work in progress. N Engl J Med. 2006;354:2095–8. doi: 10.1056/NEJMp068097. [DOI] [PubMed] [Google Scholar]
- 35.Luepker RV, Raczynski JM, Osganian S, et al. Effect of a community intervention on patient delay and emergency medical service use in acute coronary heart disease: The Rapid Early Action for Coronary Treatment (REACT) Trial. JAMA. 2000;284:60–7. doi: 10.1001/jama.284.1.60. [DOI] [PubMed] [Google Scholar]
- 36.Braveman P, Schaaf VM, Egerter S, Bennett T, Schecter W. Insurance-related differences in the risk of ruptured appendix. N Engl J Med. 1994;331:444–9. doi: 10.1056/NEJM199408183310706. [DOI] [PubMed] [Google Scholar]
- 37.Wilper AP, Woolhandler S, Lasser KE, McCormick D, Bor DH, Himmelstein DU. Health insurance and mortality in US adults. Am J Public Health. 2009;99:2289–95. doi: 10.2105/AJPH.2008.157685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bitterman RA. Explaining the EMTALA paradox. Ann Emerg Med. 2002;40:470–5. doi: 10.1067/mem.2002.128799. [DOI] [PubMed] [Google Scholar]
- 39.Wanerman R. The EMTALA Paradox. Emergency Medical Treatment and Labor Act. Ann Emerg Med. 2002;40:464–9. doi: 10.1067/mem.2002.126743. [DOI] [PubMed] [Google Scholar]
- 40.Dracup K, Alonzo AA, Atkins JM, et al. The physician’s role in minimizing prehospital delay in patients at high risk for acute myocardial infarction: recommendations from the National Heart Attack Alert Program. Working Group on Educational Strategies To Prevent Prehospital Delay in Patients at High Risk for Acute Myocardial Infarction. Ann Intern Med. 1997;126:645–51. doi: 10.7326/0003-4819-126-8-199704150-00010. [DOI] [PubMed] [Google Scholar]