Abstract
Duchenne muscular dystrophy (DMD) is caused by mutations in dystrophin and the subsequent disruption of the dystrophin-associated protein complex (DAPC). Utrophin is a dystrophin homolog expressed at high levels in developing muscle that is an attractive target for DMD therapy. Here we show that the extracellular matrix protein biglycan regulates utrophin expression in immature muscle and that recombinant human biglycan (rhBGN) increases utrophin expression in cultured myotubes. Systemically delivered rhBGN up-regulates utrophin at the sarcolemma and reduces muscle pathology in the mdx mouse model of DMD. RhBGN treatment also improves muscle function as judged by reduced susceptibility to eccentric contraction-induced injury. Utrophin is required for the rhBGN therapeutic effect. Several lines of evidence indicate that biglycan acts by recruiting utrophin protein to the muscle membrane. RhBGN is well tolerated in animals dosed for as long as 3 months. We propose that rhBGN could be a therapy for DMD.
Keywords: biotherapeutics, protein therapeutics
Duchenne muscular dystrophy (DMD) is a hereditary disease that affects ~1:3,500 boys, the majority of whom will die by their midtwenties (1). DMD is caused by mutations in dystrophin that result in the faulty assembly and function of an ensemble of structural and signaling molecules at the muscle cell surface termed the dystrophin-associated protein complex (DAPC) (2–4). There are currently no treatments that target the primary pathology of DMD.
One attractive therapeutic approach for DMD is the stabilization of the muscle cell membrane through up-regulation of utrophin, a dystrophin homolog. Transgenic overexpression of utrophin rescues dystrophic pathology and restores function in the dystrophin-deficient mdx mouse (5–7). In mature muscle, utrophin expression is restricted to the neuromuscular and myotendinous junctions. However, utrophin is expressed over the entire myofiber in developing and regenerating muscle (8–10). These observations raise the possibility that marshalling pathways that normally regulate utrophin expression in developing muscle could be a productive approach for developing DMD treatments.
The extracellular matrix protein biglycan plays an important role in developing muscle. In both humans and mice, biglycan is most highly expressed in immature and regenerating muscle (11, 12). Biglycan is a component of the DAPC, where it binds to α-dystroglycan (13) and α- and γ-sarcoglycan (14). Biglycan regulates the expression of the sarcoglycans as well as dystrobrevins, syntrophins, and nNOS, particularly in immature muscle. Finally, biglycan is important for timely muscle regeneration (11).
Locally delivered recombinant human biglycan (rhBGN) incorporates into the extracellular matrix of bgn−/o muscle where it persists for at least 2 wk and rescues the expression of several DAPC components (15). These results raise the possibility that rhBGN might enhance function in muscle that lacks dystrophin. Here we show that utrophin is down-regulated in immature biglycan null (bgn−/o) mice and that rhBGN up-regulates membrane-associated utrophin in cultured myotubes. Importantly, rhBGN can be delivered systemically to dystrophin-deficient mdx mice, where it up-regulates utrophin and other DAPC components at the sarcolemma, ameliorates muscle pathology, and improves function. Several lines of evidence indicate that biglycan acts by recruiting utrophin to the plasma membrane. We propose rhBGN as a candidate therapeutic for DMD.
Results
Endogenous Biglycan Regulates Utrophin Expression in Immature Muscle.
At postnatal day 14 (P14), utrophin is highly expressed in the perisynaptic sarcolemma (Fig. 1A) (9). To compare utrophin expression levels in the presence and absence of biglycan, we immunostained sections of muscle from bgn−/o mice and age-matched congenic controls. In all cases, the mutant and WT sections were mounted on the same slides, stained together and imaged concurrently (Materials and Methods). Fig. 1A shows that utrophin expression is decreased at the perisynaptic sarcolemma in bgn−/o muscle, whereas sarcolemmal dystrophin expression was unchanged. Quantification of 50 sarcolemmal segments from each of three animals from each genotype showed that utrophin levels were reduced by ~28% (Fig. 1B; Bgn−/o: 0.72 ± 0.03, WT: 1.0 ± 0.04, unpaired Student t test, P < 0.0001). In contrast, there was no significant difference in the expression of dystrophin in the sarcolemma (Fig. 1C; Bgn−/o: 1.01 ± 0.03, WT: 1.00 ± 0.03, unpaired Student t test, P = 0.76). Notably, the amount of utrophin transcript was indistinguishable in WT as compared with bgn−/o P14 muscle (text below and Fig. 1D). These results indicate that utrophin protein expression at the sarcolemma is selectively decreased in the absence of biglycan.
Fig. 1.
Utrophin is reduced at the sarcolemma of immature bgn−/o mice. (A) Quadriceps muscles from congenic P14 WT (Upper Panels) DJS and bgn−/o (Lower Panels) mice were harvested, sectioned, mounted on the same slides, and immunostained for dystrophin and utrophin. Utrophin expression is decreased in these developing biglycan null mice compared with WT mice, whereas dystrophin expression is not detectably altered. (Scale bar = 25 μm.) (B) Quantification of sarcolemmal utrophin expression. Images of utrophin-stained muscle sections as prepared in A were acquired and the levels of utrophin immunostaining at the perijunctional sarcolemma were measured as described in Materials and Methods. A total of 50 sarcolemmal segments from each of three animals from each genotype were analyzed. Utrophin immunoreactivity was decreased 28% in sections from bgn−/o muscle compared with WT (Bgn−/o: 0.72 ± 0.03, WT: 1.0 ± 0.04, unpaired Student t test, P < 0.0001; n = 150 sarcolemmal segments from three mice of each genotype). (C) Quantification of perijunctional sarcolemmal dystrophin. Dystrophin-stained sections were imaged and measured as in B. Dystrophin immunoreactivity was equivalent in P14 WT and bgn−/o sections (Bgn−/o: 1.01 ± 0.03, WT: 1.00 ± 0.03, unpaired Student t test, P = 0.76). (D) Quantitative real-time PCR analysis of utrophin transcripts in P14 WT and bgn−/o mice. Total RNA was extracted from quadriceps muscles from WT and bgn−/o mice and used for cDNA synthesis. Expression of utrophin mRNA was indistinguishable in WT and Bgn−/o muscles (WT: 1.0 ± 0.26, Bgn−/o: 0.99 ± 0.09, n = 3 animals from each genotype).
RhBGN Treatment Up-Regulates Membrane-Associated Utrophin in Cultured Muscle Cells.
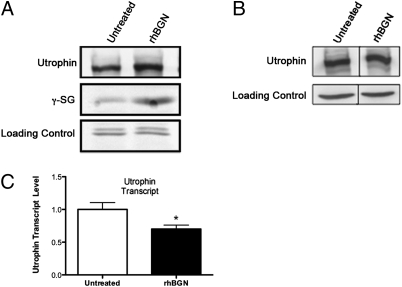
We next turned to a cell culture system to more precisely delineate the role of biglycan in regulating utrophin association with the sarcolemma. We stimulated bgn−/o myotubes with 1 nM rhBGN and assessed the levels of utrophin and γ-sarcoglycan in membrane fractions by Western blotting. As shown in Fig. 2A, rhBGN treatment up-regulates utrophin and γ-sarcoglycan protein in these membrane fractions. On the other hand, there was a reduction in utrophin transcript levels following rhBGN treatment (untreated: 1 ± 0.10; rhBGN treated: 0.7 ± 0.06; unpaired Student t test, P = 0.02; n = 6 separate experiments with three replicate flasks in each). Thus, the up-regulation of utrophin protein expression at the membrane is not associated with increases in the level of its transcript.
Fig. 2.
RhBGN treatment increases membrane-associated utrophin and γ-sarcoglycan protein in cultured myotubes. (A) Cultured bgn−/o myotubes were incubated for 8 h with either 1 nM rhBGN or vehicle as indicated. Shown are Western blots of membrane fractions probed for utrophin and γ-sarcoglycan (γ-SG). Note the increased expression of both utrophin and γ-sarcoglycan following rhBGN treatment. (B) Bgn−/o myotubes were treated as in A and whole-cell extracts were prepared. Proteins were separated by SDS/PAGE and immunoblotted for utrophin and actin (loading control). Total utrophin protein levels were similar in untreated and rhBGN treated cultures. (C) Quantitative RT-PCR analysis of untreated and rhBGN treated cultured bgn−/o myotubes. RhBGN treatment decreased utrophin transcript levels by ~30% (untreated: 1 ± 0.10; rhBGN treated: 0.7 ± 0.06; unpaired Student t test, P = 0.02; n = 6 separate experiments with three replicate flasks in each).
The results described above suggest that biglycan could regulate utrophin protein by mechanisms involving elevated translation, increased stability, and/or targeting of utrophin to the membrane. To distinguish among these possibilities, we assessed the level of total utrophin protein in control and biglycan-treated cultures. As shown in Fig. 2, total utrophin protein levels are indistinguishable in treated and untreated myotubes. The failure to detect changes in total cellular utrophin protein under conditions in which the membrane-bound fraction is increased indicates that biglycan regulates the association of utrophin with the membrane.
Systemic Delivery of rhBGN.
The role for biglycan in recruiting utrophin to the membrane, taken together with previous results, showing that both endogenous biglycan and intramuscularly delivered rhBGN can regulate DAPC proteins in vivo (15), raising the possibility that rhBGN could be a therapeutic agent for DMD. As a first step toward developing such a therapy, we asked whether rhBGN could be delivered systemically. A capture ELISA showed that rhBGN was readily detected in the circulation 30 and 60 min after i.p. delivery (Fig. S1A). To detect the recombinant protein in tissue, where endogenous biglycan is expressed (13), we injected animals i.p. with rhBGN conjugated to Alexa-555. As shown in Fig. S1B, this rhBGN is readily detected in the muscle extracellular matrix 48 h following injection. These observations indicate that the circulating recombinant protein partitions to muscle where it becomes stably associated with the ECM. This result is in agreement with our earlier findings that intramuscularly delivered rhBGN is stable in muscle for at least 2 wk following a single intramuscular injection in bgn−/o mice (15). This finding is also consistent with the efficacy of rhBGN observed 2 wk after a single injection in mdx mice (discussed below). Taken together, these findings indicate that rhBGN can be delivered systemically and can become localized to muscle for prolonged periods.
RhBGN Up-Regulates Utrophin and Other DAPC Components in mdx Mice.
We next asked whether rhBGN can up-regulate utrophin in mdx mice. A single i.p. dose of rhBGN was delivered to ~P18 mdx mice, and utrophin levels at the sarcolemma were assessed 2 wk later. Because utrophin expression increases transiently in regenerating myofibers (16) and is known to be enriched at synaptic and perisynaptic regions (8, 17), we restricted our analysis to extrasynaptic areas of nonregenerated (peripherally nucleated) myofibers. As shown in Fig. 3 A and B, rhBGN treatment increased utrophin expression at the sarcolemma >2.5-fold in quadriceps muscle mdx mice (vehicle: 1.0 ± 0.05, rhBGN: 2.5 ± 0.08, unpaired Student t test, P < 0.0001, n = 200 sarcolemmal segments from two animals from each group). Utrophin levels at the sarcolemma were also significantly increased in the tibialis anterior muscle (Fig. S2, vehicle: 1.0 ± 0.1, rhBGN: 1.7 ± 0.1, unpaired Student t test; n = 300 sarcolemmal segments from three animals from each group).
Fig. 3.
RhBGN treatment up-regulates utrophin at the sarcolemma of mdx mice. (A) Utrophin immunostaining of quadriceps muscles from P33 mdx littermate mice that received a single i.p. injection of either rhBGN or vehicle at P19. (Scale bar = 25 μm.) (B) Levels of immunostaining at the sarcolemma (e.g., arrows in A) of peripherally nucleated fibers. A total of 100 sarcolemmal segments from each of four animals were analyzed (two littermate pairs, one rhBGN- and one vehicle-injected animal per pair). Sarcolemmal utrophin immunoreactivity was >2.5-fold higher in sections from rhBGN- as compared with vehicle-injected animals (unpaired Student t test, P < 0.0001). (C) qRT PCR analysis of utrophin transcripts in from vehicle- or rhBGN-injected mdx mice. There was no significant difference in utrophin transcript levels in rhBGN treated mice compared with vehicle-injected controls (unpaired Student t test, P = 0.057; n = 8 vehicle- and 6 rhBGN-treated mice). (D) RhBGN treatment increases utrophin expression in muscle membrane fractions. Mdx mice from a single litter were injected at P16 and P38 (Left Pair) or P16, P38, and P63 (Right Pair) with rhBGN or vehicle. Muscles were harvested 3 wk after the last injection. (E) RhBGN treatment increases γ-sarcoglycan expression. Mdx mice were injected at 3-wk intervals starting at P14 with rhBGN or vehicle alone. Muscles were harvested at 15 wk of age and immunoblotted for γ-sarcoglycan. γ-Sarcoglycan is increased in the membrane fractions from rhBGN treated mdx mice compared with vehicle-treated animals.
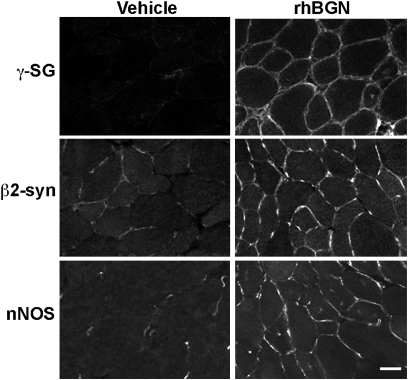
The levels of γ-sarcoglycan, β2-syntrophin, and nNOS are also increased at the sarcolemma following a single dose of rhBGN (Fig. 4). We observed no change in α-syntrophin levels. The elevation in γ-sarcoglycan and nNOS is in agreement with our observations in cell culture, in which rhBGN treatment increased the levels of these proteins at the membrane (Fig. 2) (15). Furthermore, these proteins as well as β2 syntrophin are dysregulated in bgn−/o mice (14, 15). Western blotting of membrane fractions provided further evidence that rhBGN treatment increased the levels of both utrophin and γ-sarcoglycan mdx mice (Fig. 3 C and D). Taken together, these results indicate that rhBGN treatment restores the expression of utrophin and DAPC proteins to the sarcolemma.
Fig. 4.
RhBGN up-regulates DAPC components at the sarcolemma of mdx mice. Mdx mice were injected with rhBGN or vehicle at P18 and muscles were harvested at 32P. Sections of TA from vehicle- or rhBGN-treated animals were immunostained with antibodies to the indicated DAPC components as described in Materials and Methods. RhBGN treatment increased the expression of sarcolemmal γ-sarcoglycan, β2-syntrophin, and nNOS in mdx mice.
Utrophin transcript levels were unchanged in rhBGN-treated mdx (Fig. 3C). This finding is in agreement with our in vivo and cell culture results with bgn−/o muscle (Figs. 1 and 2), and indicates than rhBGN regulates utrophin in mdx mice at a posttranscriptional level. Finally, these results show that rhBGN effects can be observed after multiple doses spanning 6–13 wk of treatment (Fig. 3D and E). Taken together, these immunohistochemical and biochemical results show that systemically delivered rhBGN can up-regulate utrophin and other DAPC protein in the membranes of dystrophic mice.
RhBGN Reduces Dystrophic Pathology in mdx Mice.
To determine whether rhBGN counters dystrophic pathology in mdx mice, we first administered a single i.p. dose of rhBGN or vehicle alone to ~P18 mdx mice and assessed muscle histologically 2 or 3 wk later. Fig. 5A (Upper Panel) shows a section of diaphragm from vehicle-injected mice displaying characteristic dystrophic pathology including a high proportion of centrally nucleated fibers (CNFs) and foci of necrosis/regeneration and areas of mononuclear cell infiltration (18). Strikingly, rhBGN treatment resulted in a ~50% reduction in the proportion of CNFs observed in muscle from rhBGN treated mice (17.7% ± 2.8 and 9.6% ± 1.7 for vehicle- and rhBGN-injected animals, respectively; unpaired Student t test, P = 0.028, n = 13 vehicle- and 11 rhBGN-injected animals; Fig. 5B). We also assessed serum creatine kinase (CK) levels, a marker of muscle damage, in mice that had been given 1, 2, or 10 mg/kg rhBGN. As reported by others (18), there was considerable variation in the baseline levels of CK among experiments. Although we observed a trend toward decreased CK levels in these animals, the data did not reach statistical significance (Fig. S3). Taken together, these findings indicate that rhBGN treatment reduces dystrophic pathology in mdx mice.
Fig. 5.
Systemically administered rhBGN counters dystrophic pathology in mdx mice. (A) H&E-stained sections of diaphragm from littermate mdx mice that were injected i.p. with vehicle (Upper Panels) or 100 μg rhBGN (Lower Panels) at P18 and harvested at P38. (Right Panels) Magnified view. Note the extensive areas of necrosis/regeneration and mononuclear cell infiltration in muscle from vehicle-injected as compared with rhBGN-injected mice. (Scale bars = 50 μm.) (B) RhBGN administration decreases proportion of CNFs in mdx muscle compared with vehicle-injected littermates (single injection; Materials and Methods). Percentages of CNFs were determined from H&E-stained diaphragm sections. RhBGN-treated mdx mice had ~50% fewer centrally nucleated myofibers as compared with vehicle-injected mdx mice (17.7% ± 2.8 and 9.6% ± 1.7 for vehicle- and rhBGN-injected animals, respectively; n = 13 vehicle-injected and 11 rhBGN-injected animals; unpaired Student t test, P = 0.028).
RhBGN Efficacy Is Utrophin Dependent.
We next asked whether the ability of rhBGN to counter dystrophic pathology in mdx mice is dependent upon utrophin. If utrophin is necessary for rhBGN action in mdx mice, the pathology of mice mutant for both utrophin and dystrophin would be unaffected by rhBGN administration. Fig. S4 shows that the histology and number of regenerated muscle fibers in mdx:utrn−/− mice were indistinguishable after a single injection of rhBGN or vehicle. Thus, utrophin is necessary for the therapeutic action of rhBGN.
RhBGN Treatment Improves Muscle Function in mdx Mice.
An effective treatment for DMD must improve muscle function. One of the primary causes of myofiber pathology, dysfunction, and death in DMD is increased susceptibility to contraction-induced damage. Such muscle damage can be assessed ex vivo by measuring the force produced after each of several successive eccentric (lengthening) contractions (ECCs) (19, 20). In these ex vivo mdx muscles, susceptibility to injury is evidenced by an increase in force drop after a series of ECCs. We injected mdx mice at 3-wk intervals (starting at P14) with either rhBGN or vehicle until 15 wk of age, and measured muscle physiology as previously described (21, 22). RhBGN treatment improved performance on muscle function measurements, as shown by a reduced amount of force drop following each consecutive ECC (Fig. 6 C and D). This improvement was robust and statistically significant from the second ECC onward (Fig. 6C.). We observed no change in other parameters of muscle function including the amount of specific force generated (Table S1). Such a profile of physiological improvement—increased resistance to damage with no change in specific force—is similar to that observed with adeno-associated virus delivery of microdystrophin (R4–R23) (23) or heregulin treatment (24). Thus rhBGN treatment improves muscle function in mdx mice.
Fig. 6.
Physiological improvement of muscle in rhBGN-treated mdx mice. Mdx mice were injected at 3-wk intervals starting at P14 with either rhBGN (25 μg/injection; i.p.) or vehicle and tissue was harvested at 15 wk of age. Representative first to fifth ECCs of extensor digitorum longus (EDL) muscles from mdx mice injected with (A) vehicle, or (B) rhBGN. (C) Comparisons of ECC force drop between the first and the second, third, fourth, and fifth ECC of vehicle-treated (6.4 ± 1.2%; 12.4 ± 1.9%; 18.4 ± 2.3%; 22.2 ± 7%; n = 16) and rhBGN-treated (3.9 ± 0.3%; 7.5 ± 0.5%; 11.6 ± 0.8%; 14.9 ± 1.2%; n = 16) mdx mice, respectively. There is significant difference in the force drop between ECCs of vehicle-treated and rhBGN-treated mdx mice on the second, third, fourth, and fifth contractions (P = 0.05, 0.02, 0.01, 0.02, respectively; unpaired Student t test). (D) Average force drop between first and fifth ECC in vehicle-treated and rhBGN-treated mdx mice (22.2 ± 2.7% vs.14.9 ± 1.2%, respectively; P = 0.02; n = 16 muscles in each group; unpaired Student t test).
RhBGN Is Well Tolerated in mdx Mice.
We have not observed deleterious effects of rhBGN administration in mdx mice, even after 3 mo of treatment. Organ weight is a long-standing and widely accepted measure of pharmacological toxicity (25, 26). As shown in Fig. S5A, there were no significant differences in the weights of the liver, kidney, lung, or spleen. There was an 8% decrease in the weight of the heart. Whole-animal weights were equivalent in vehicle- and rhBGN-dosed animals. Muscle weights were also unchanged with the exception of the soleus, which was 17% larger in rhBGN-treated animals. Furthermore, no indication of kidney or liver dysfunction was observed: there were no significant changes in the levels of serum creatinine, blood urea nitrogen (BUN), aspartate transaminase (AST), or bilirubin at single doses ranging from 1 to 10 mg/kg (Fig. S5B).
Discussion
In this report, we introduce a unique therapeutic approach for DMD based upon the systemic delivery rhBGN, a recombinant form of the extracellular matrix protein biglycan. Several characteristics of rhBGN suggest that it could be an effective therapy for DMD. (i) RhBGN counters dystrophic pathology and improves muscle function. (ii) Systemically delivered rhBGN localizes to muscle and a single dose is effective for up to 3 wk. Multiple doses at 3-wk intervals can sustain the response for at least 3 mo. (iii) RhBGN acts at least in part through utrophin, a pathway that has been extensively validated in animal studies (5, 27, 28). (iv) RhBGN restores the expression of DAPC components that are important for muscle integrity and function. (v) RhBGN could selectively target the tissues affected in DMD, as it binds to α- and γ-sarcoglycan (14), which are components of the dystrophin/utrophin protein complex and are expressed selectively in heart and skeletal muscle (29–32). (vi) RhBGN is well tolerated in mdx mice. (vii) Endogenous biglycan is expressed in normal and DMD muscle (33, 34) and is a highly conserved protein. RhBGN could thus be expected to elicit a minimal immune response. (viii) RhBGN is nonglycanated (i.e., lacking glycosaminoglycan side chains). This relatively uncomplicated structure simplifies its manufacture in a homogeneous form.
Several lines of evidence suggest that rhBGN counters pathology and improves muscle function through the up-regulation of utrophin and other DAPC components at the sarcolemma. First, rhBGN treatment up-regulates sarcolemmal utrophin in both acute (single dose) and prolonged, multidose paradigms (Fig. 3). Utrophin is necessary for rhBGN action, as we observed no improvement in muscle pathology in mdx:utrophin double null mice (Fig. S3). Importantly, up-regulation of utrophin by increasing gene expression (5) or rhBGN treatment, which recruits utrophin protein to the sarcolemma, both result in assembly of DAPC components and improvement in muscle function as measured by resistance to ECC. Furthermore, as discussed below, the recruitment of utrophin and other DAPC components to the sarcolemma, rather than the global up-regulation of utrophin mRNA or protein, is likely to be the therapeutically salient feature of rhBGN action.
Our results show that a single systemic injection of rhBGN is active for a strikingly long period (Figs. 3 and 5). This prolonged action of rhBGN is consistent with our previous studies in bgn−/o mice showing that intramuscularly delivered rhBGN is stable and biologically active for 3 wk (15). This protracted action seems likely to result from the binding of rhBGN to the ECM. Circulating levels of rhBGN fall rapidly and are undetectable by 24 h after i.p. injection (Fig. S1A). However, rhBGN is readily detected in the muscle ECM 2 d after i.p. injection. This stable association could be due in part to binding to collagen VI in the ECM (35) and to sarcoglycans at the sarcolemma (14). The long-acting properties of systemically delivered rhBGN in mice suggest that this therapeutic strategy could be practical for use in humans, where treatment will likely be required for years.
The results presented here indicate that rhBGN acts by recruiting utrophin protein to the sarcolemma. In cell culture, rhBGN rapidly up-regulates utrophin content in membrane fractions, but there is no increase in total utrophin protein levels (Fig. 2). In vivo, utrophin levels at the sarcolemma of immature biglycan−/o mice are decreased, whereas transcript levels are unchanged (Fig. 1). Furthermore, treatment of mdx mice with rhBGN results in up-regulation of utrophin at the sarcolemma with no increase in transcript levels (Fig. 3). The posttranscriptional action of rhBGN is further supported by its ability to increase the levels of membrane-associated utrophin in cultured myotubes after 8 h of treatment; this interval is far less than the 16 h required to synthesize a mature utrophin transcript (36). The data in cultured myotubes (Fig. 2) are consistent with a model in which increased levels of membrane (but not total) utrophin provide negative feedback for utrophin transcript levels. Taken together, our observation support the proposal that the recruitment of utrophin and other DAPC components to the membrane is the mechanism by which rhBGN counters dystrophic pathology in mdx mice. It is of particular note that total utrophin protein levels are up-regulated in DMD muscle (37–39). Therefore rhBGN can be expected to be effective in DMD patients.
Systemically delivered rhBGN increases nNOS at the sarcolemma (Fig. 4). We have previously reported that biglycan increases nNOS at the membrane in cultured myotubes (15). These data are in agreement with studies by Sonnemann et al. (40), in which delivery of TAT-μutr protein restores sarcolemmal nNOS in mdx mice. These observations are of particular interest, as up-regulation of nNOS could counter fatigue in dystrophic muscle (41). However, studies using viral delivery of utrophin failed to detect rescue of nNOS expression at the membrane (42). The basis for this discrepancy is unknown. One possibility is that are multiple mechanisms of utrophin-mediated DAPC restoration. For example, rhBGN binds DAPC components at the cell surface, a property that could promote the assembly of a more complete utrophin-associated complex, including nNOS.
The biglycan-mediated recruitment of utrophin to the sarcolemma represents a novel pathway for DMD treatment. Previous work has shown that utrophin expression is also regulated at transcriptional and translational levels, and efforts are underway to develop therapies that target these mechanisms (6, 43–45). In addition to having therapeutic efficacy on its own, the unique action of biglycan in recruiting utrophin to the sarcolemma could synergize with these other utrophin-directed strategies. Finally, rhBGN could be used in combination with therapies aimed at increasing muscle mass (21, 22), reducing inflammation (46, 47), or restoring dystrophin by antisense oligonucleotide-mediated exon skipping (48, 49).
Numerous protein-based therapies for a range of human disorders are currently in the clinic, and many more are in development. The methods for the manufacture and delivery of protein therapeutics are well understood. Furthermore, as a class, protein therapies have proved to be remarkably safe. Therefore, the path from these laboratory studies to clinical trials of rhBGN-based DMD therapies is clear.
Materials and Methods
Biglycan.
Recombinant, nonglycanated human biglycan (rhBGN) was produced in mammalian cells and purified as previously described (15). This form lacks GAG side chains. The Alexa 555 protein labeling kit (Invitrogen Corporation) was used to conjugate this fluor to rhBGN.
Animals and Injections.
All protocols were conducted under accordance and with the approval of Brown University's Institutional Animal Care and Use Committee. For single injections, P16-19 mice received an i.p. injection of 100 μg rhBGN in 25 μL 20 mM Tris, 0.5M NaCl, 0.2% CHAPS, or vehicle (20 mM Tris, 0.5 M NaCl, 0.2% CHAPS). Multiply injected mice received additional i.p. injections of 100 μg rhBGN or vehicle at 3-wk intervals. Mice were harvested 13–25 d after the final injection. For tracing studies, adult mdx mice received an i.p. injection of Alexa 555-labeled rhBGN, and diaphragms were harvested 48 h later.
Histology and Immunohistochemistry.
Frozen sections were prepared and stained as previously described (15). For bgn−/o analysis, P14 congenic bgn−/o and WT sections were mounted on the same slide, immunostained simultaneously, and imaged with a cooled CCD camera in the same session using identical exposures. All comparisons of sections from injected mice (vehicle and rhBGN) were also mounted, stained and imaged together. Sections were observed using a Nikon (Melville, NY) Eclipse E800 microscope and images acquired with Scanalytics IP Lab Spectrum software or NIS Elements (Nikon). Utrophin and dystrophin immunoreactivity intensity was quantified using Metamorph image analysis software (Universal Imaging) or ImageJ software (National Institutes of Health). We also observed structures in the interstitial space, which may be blood vessels, that showed increased utrophin in some experiments (Fig. 3). These structures were not included in our measurements. The average pixel intensities of sarcolemmal segments were measured, and the mean background (determined by measuring nonsarcolemmal regions from each condition) was subtracted from them. The average background levels were indistinguishable between conditions. Analysis in mdx mice was performed on quadriceps from two mice of each condition and on TAs from three mice of each condition. Sources and conditions for antibodies are given in SI Materials and Methods. For scoring the percentage of CNFs, all cross-sectioned myofibers outside of necrosis/regenerative foci in H&E-stained sections were counted under a 20× objective (270–1,913 fibers/muscle section).
Quantitative RT-PCR and Western Blot Analysis.
Utrophin transcript levels were measured using SYBR-Green (Invitrogen) as described in SI Materials and Methods. Culture methods, preparation of lysates, and membrane fractions and analysis by Western blot were by standard procedures detailed in SI Materials and Methods.
Muscle Physiology.
Mdx mice were injected i.p. with rhBGN (25 μg/animal) or vehicle every 3 wk starting at P14 and the physiological properties of the extensor digitorum longus (EDL) muscles were analyzed ex vivo at 3.5 mo of age as described previously (21, 22). Muscle length was adjusted to achieve maximal twitch response and this length (Lo) was measured. Eccentric contraction force decrease was calculated for each tetanus of a standard ECC protocol of supramaximal stimulus 700 ms, total lengthening Lo/10; lengthening velocity 0.5 Lo/s. EDL sections were obtained and images were acquired as above. Cross-sectional area was measured using ImageJ software (National Institutes of Health).
Supplementary Material
Acknowledgments
We thank Carolyn Schmiedel and Sarah Mentzer for superb technical assistance and Beatrice Lechner for qPCR analysis of bgn−/o muscle. We thank Stan Froehner (University of Washington, Seattle) for gifts of antibodies. We are also grateful to David McQuillan and Richard Owens (LifeCell Corporation, Branchburg, NJ) for recombinant biglycan, and members of the Fallon laboratory for valuable input. This work was supported in part by HD23924, AR57698, RR15578, and NS064295 (to J.R.F.); P20 RR018757 and KO8 HL072332 (to M.A.); AR 48871 and EY 013862 (to T.S.K); Parent Project Muscular Dystrophy, Charley's Fund, and the Nash Avery Foundation.
Footnotes
Conflict of interest statement: A.R.A., B.A.M., and J.R.F. are inventors on patents owned by Brown University covering biglycan as a therapeutic for neuromuscular diseases. J.F. is a Director and shareholder in Tivorsan pharmaceuticals.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1013067108/-/DCSupplemental.
References
- 1.Emery AEH. Duchenne Muscular Dystrophy. 2nd Ed. Oxford: Oxford University Press; 1993. [Google Scholar]
- 2.Koenig M, et al. Complete cloning of the Duchenne muscular dystrophy (DMD) cDNA and preliminary genomic organization of the DMD gene in normal and affected individuals. Cell. 1987;50:509–517. doi: 10.1016/0092-8674(87)90504-6. [DOI] [PubMed] [Google Scholar]
- 3.Blake DJ, Weir A, Newey SE, Davies KE. Function and genetics of dystrophin and dystrophin-related proteins in muscle. Physiol Rev. 2002;82:291–329. doi: 10.1152/physrev.00028.2001. [DOI] [PubMed] [Google Scholar]
- 4.Muntoni F, Torelli S, Ferlini A. Dystrophin and mutations: One gene, several proteins, multiple phenotypes. Lancet Neurol. 2003;2:731–740. doi: 10.1016/s1474-4422(03)00585-4. [DOI] [PubMed] [Google Scholar]
- 5.Tinsley J, et al. Expression of full-length utrophin prevents muscular dystrophy in mdx mice. Nat Med. 1998;4:1441–1444. doi: 10.1038/4033. [DOI] [PubMed] [Google Scholar]
- 6.Khurana TS, Davies KE. Pharmacological strategies for muscular dystrophy. Nat Rev Drug Discov. 2003;2:379–390. doi: 10.1038/nrd1085. [DOI] [PubMed] [Google Scholar]
- 7.Miura P, Jasmin BJ. Utrophin upregulation for treating Duchenne or Becker muscular dystrophy: How close are we? Trends Mol Med. 2006;12:122–129. doi: 10.1016/j.molmed.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 8.Khurana TS, et al. Immunolocalization and developmental expression of dystrophin related protein in skeletal muscle. Neuromuscul Disord. 1991;1:185–194. doi: 10.1016/0960-8966(91)90023-l. [DOI] [PubMed] [Google Scholar]
- 9.Clerk A, Morris GE, Dubowitz V, Davies KE, Sewry CA. Dystrophin-related protein, utrophin, in normal and dystrophic human fetal skeletal muscle. Histochem J. 1993;25:554–561. [PubMed] [Google Scholar]
- 10.Pons F, Nicholson LV, Robert A, Voit T, Leger JJ. Dystrophin and dystrophin-related protein (utrophin) distribution in normal and dystrophin-deficient skeletal muscles. Neuromuscul Disord. 1993;3:507–514. doi: 10.1016/0960-8966(93)90106-t. [DOI] [PubMed] [Google Scholar]
- 11.Casar JC, McKechnie BA, Fallon JR, Young MF, Brandan E. Transient up-regulation of biglycan during skeletal muscle regeneration: Delayed fiber growth along with decorin increase in biglycan-deficient mice. Dev Biol. 2004;268:358–371. doi: 10.1016/j.ydbio.2003.12.025. [DOI] [PubMed] [Google Scholar]
- 12.Lechner BE, Lim JH, Mercado ML, Fallon JR. Developmental regulation of biglycan expression in muscle and tendon. Muscle Nerve. 2006;34:347–355. doi: 10.1002/mus.20596. [DOI] [PubMed] [Google Scholar]
- 13.Bowe MA, Mendis DB, Fallon JR. The small leucine-rich repeat proteoglycan biglycan binds to alpha-dystroglycan and is upregulated in dystrophic muscle. J Cell Biol. 2000;148:801–810. doi: 10.1083/jcb.148.4.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rafii MS, et al. Biglycan binds to alpha- and gamma-sarcoglycan and regulates their expression during development. J Cell Physiol. 2006;209:439–447. doi: 10.1002/jcp.20740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mercado ML, et al. Biglycan regulates the expression and sarcolemmal localization of dystrobrevin, syntrophin, and nNOS. FASEB J. 2006;20:1724–1726. doi: 10.1096/fj.05-5124fje. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Helliwell TR, Man NT, Morris GE, Davies KE. The dystrophin-related protein, utrophin, is expressed on the sarcolemma of regenerating human skeletal muscle fibres in dystrophies and inflammatory myopathies. Neuromuscul Disord. 1992;2:177–184. doi: 10.1016/0960-8966(92)90004-p. [DOI] [PubMed] [Google Scholar]
- 17.Nguyen TM, et al. Full-length and short forms of utrophin, the dystrophin-related protein. FEBS Lett. 1995;358:262–266. doi: 10.1016/0014-5793(94)01441-3. [DOI] [PubMed] [Google Scholar]
- 18.Coulton GR, Morgan JE, Partridge TA, Sloper JC. The mdx mouse skeletal muscle myopathy: I. A histological, morphometric and biochemical investigation. Neuropathol Appl Neurobiol. 1988;14:53–70. doi: 10.1111/j.1365-2990.1988.tb00866.x. [DOI] [PubMed] [Google Scholar]
- 19.Moens P, Baatsen PH, Maréchal G. Increased susceptibility of EDL muscles from mdx mice to damage induced by contractions with stretch. J Muscle Res Cell Motil. 1993;14:446–451. doi: 10.1007/BF00121296. [DOI] [PubMed] [Google Scholar]
- 20.Gillis JM. Understanding dystrophinopathies: An inventory of the structural and functional consequences of the absence of dystrophin in muscles of the mdx mouse. J Muscle Res Cell Motil. 1999;20:605–625. doi: 10.1023/a:1005545325254. [DOI] [PubMed] [Google Scholar]
- 21.Bogdanovich S, et al. Functional improvement of dystrophic muscle by myostatin blockade. Nature. 2002;420:418–421. doi: 10.1038/nature01154. [DOI] [PubMed] [Google Scholar]
- 22.Bogdanovich S, Perkins KJ, Krag TO, Whittemore LA, Khurana TS. Myostatin propeptide-mediated amelioration of dystrophic pathophysiology. FASEB J. 2005;19:543–549. doi: 10.1096/fj.04-2796com. [DOI] [PubMed] [Google Scholar]
- 23.Liu M, et al. Adeno-associated virus-mediated microdystrophin expression protects young mdx muscle from contraction-induced injury. Mol Ther. 2005;11:245–256. doi: 10.1016/j.ymthe.2004.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krag TO, et al. Heregulin ameliorates the dystrophic phenotype in mdx mice. Proc Natl Acad Sci USA. 2004;101:13856–13860. doi: 10.1073/pnas.0405972101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Michael B, et al. Evaluation of organ weights for rodent and non-rodent toxicity studies: A review of regulatory guidelines and a survey of current practices. Toxicol Pathol. 2007;35:742–750. doi: 10.1080/01926230701595292. [DOI] [PubMed] [Google Scholar]
- 26.Peters JM, Boyd EM. Organ weights and water levels of the rat following reduced food intake. J Nutr. 1966;90:354–360. doi: 10.1093/jn/90.4.354. [DOI] [PubMed] [Google Scholar]
- 27.Ebihara S, et al. Differential effects of dystrophin and utrophin gene transfer in immunocompetent muscular dystrophy (mdx) mice. Physiol Genomics. 2000;3:133–144. doi: 10.1152/physiolgenomics.2000.3.3.133. [DOI] [PubMed] [Google Scholar]
- 28.Cerletti M, et al. Dystrophic phenotype of canine X-linked muscular dystrophy is mitigated by adenovirus-mediated utrophin gene transfer. Gene Ther. 2003;10:750–757. doi: 10.1038/sj.gt.3301941. [DOI] [PubMed] [Google Scholar]
- 29.Hack AA, Groh ME, McNally EM. Sarcoglycans in muscular dystrophy. Microsc Res Tech. 2000;48:167–180. doi: 10.1002/(SICI)1097-0029(20000201/15)48:3/4<167::AID-JEMT5>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 30.Barresi R, Moore SA, Stolle CA, Mendell JR, Campbell KP. Expression of gamma-sarcoglycan in smooth muscle and its interaction with the smooth muscle sarcoglycan-sarcospan complex. J Biol Chem. 2000;275:38554–38560. doi: 10.1074/jbc.M007799200. [DOI] [PubMed] [Google Scholar]
- 31.Wheeler MT, McNally EM. Sarcoglycans in vascular smooth and striated muscle. Trends Cardiovasc Med. 2003;13:238–243. doi: 10.1016/s1050-1738(03)00101-4. [DOI] [PubMed] [Google Scholar]
- 32.Anastasi G, et al. Sarcoglycan subcomplex expression in normal human smooth muscle. J Histochem Cytochem. 2007;55:831–843. doi: 10.1369/jhc.6A7145.2007. [DOI] [PubMed] [Google Scholar]
- 33.Haslett JN, Kunkel LM. Microarray analysis of normal and dystrophic skeletal muscle. Int J Dev Neurosci. 2002;20:359–365. doi: 10.1016/s0736-5748(02)00041-2. [DOI] [PubMed] [Google Scholar]
- 34.Zanotti S, et al. Decorin and biglycan expression is differentially altered in several muscular dystrophies. Brain. 2005;128:2546–2555. doi: 10.1093/brain/awh635. [DOI] [PubMed] [Google Scholar]
- 35.Wiberg C, et al. Biglycan and decorin bind close to the n-terminal region of the collagen VI triple helix. J Biol Chem. 2001;276:18947–18952. doi: 10.1074/jbc.M100625200. [DOI] [PubMed] [Google Scholar]
- 36.Tennyson CN, Klamut HJ, Worton RG. The human dystrophin gene requires 16 hours to be transcribed and is cotranscriptionally spliced. Nat Genet. 1995;9:184–190. doi: 10.1038/ng0295-184. [DOI] [PubMed] [Google Scholar]
- 37.Love DR, et al. Tissue distribution of the dystrophin-related gene product and expression in the mdx and dy mouse. Proc Natl Acad Sci USA. 1991;88:3243–3247. doi: 10.1073/pnas.88.8.3243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Khurana TS, Hoffman EP, Kunkel LM. Identification of a chromosome 6-encoded dystrophin-related protein. J Biol Chem. 1990;265:16717–16720. [PubMed] [Google Scholar]
- 39.Gramolini AO, Karpati G, Jasmin BJ. Discordant expression of utrophin and its transcript in human and mouse skeletal muscles. J Neuropathol Exp Neurol. 1999;58:235–244. doi: 10.1097/00005072-199903000-00003. [DOI] [PubMed] [Google Scholar]
- 40.Sonnemann KJ, et al. Functional substitution by TAT-utrophin in dystrophin-deficient mice. PLoS Med. 2009;6:e1000083. doi: 10.1371/journal.pmed.1000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kobayashi YM, et al. Sarcolemma-localized nNOS is required to maintain activity after mild exercise. Nature. 2008;456:511–515. doi: 10.1038/nature07414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li D, et al. Sarcolemmal nNOS anchoring reveals a qualitative difference between dystrophin and utrophin. J Cell Sci. 2010;123:2008–2013. doi: 10.1242/jcs.064808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gramolini AO, et al. Muscle and neural isoforms of agrin increase utrophin expression in cultured myotubes via a transcriptional regulatory mechanism. J Biol Chem. 1998;273:736–743. doi: 10.1074/jbc.273.2.736. [DOI] [PubMed] [Google Scholar]
- 44.Gramolini AO, Bélanger G, Jasmin BJ. Distinct regions in the 3′ untranslated region are responsible for targeting and stabilizing utrophin transcripts in skeletal muscle cells. J Cell Biol. 2001;154:1173–1183. doi: 10.1083/jcb.200101108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Miura P, Andrews M, Holcik M, Jasmin BJ. IRES-mediated translation of utrophin A is enhanced by glucocorticoid treatment in skeletal muscle cells. PLoS ONE. 2008;3:e2309. doi: 10.1371/journal.pone.0002309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Merlini L, et al. Early prednisone treatment in Duchenne muscular dystrophy. Muscle Nerve. 2003;27:222–227. doi: 10.1002/mus.10319. [DOI] [PubMed] [Google Scholar]
- 47.Biggar WD, et al. Deflazacort in Duchenne muscular dystrophy: A comparison of two different protocols. Neuromuscul Disord. 2004;14:476–482. doi: 10.1016/j.nmd.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 48.Mann CJ, et al. Antisense-induced exon skipping and synthesis of dystrophin in the mdx mouse. Proc Natl Acad Sci USA. 2001;98:42–47. doi: 10.1073/pnas.011408598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.van Deutekom JC, et al. Local dystrophin restoration with antisense oligonucleotide PRO051. N Engl J Med. 2007;357:2677–2686. doi: 10.1056/NEJMoa073108. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.