Examines the issues of safety and efficacy of laparoscopic cholecystectomy for emergency treatment of acute calculous cholecystitis.
Abstract
Objective:
Acute cholecystitis has been considered as a relative or absolute contraindication to laparoscopic cholecystectomy. The purpose of this study is to present our experience of laparoscopic cholecystectomy as a safe and effective treatment of acute cholecystitis.
Methods:
Laparoscopic cholecystectomy was offered to 34 consecutive patients with acute calculous cholecystitis, diagnosed according to strict clinical and ultrasonographic criteria. We used only three trocars. The gallbladder was routinely aspirated and sharp graspers were used. We adopted the fundus-first method of dissection when safe identification of the Calot' s triangle was difficult. The cystic duct was ligated whenever necessary.
Results:
The procedure was completed in 31 patients. The mean length of the laparoscopic procedure was 43 minutes, their mean hospital stay was 2.8 days. For the open group the mean length of the operative procedure was 66 minutes, while the mean hospital stay was 5.3 days. The overall morbidity rate was low.
Conclusions:
The benefits of laparoscopic cholecystectomy can be safely extended to patients with acute cholecystitis. The operation must be done early in the course of the disease. The surgeon should have adequate laparoscopic experience and maintain a low threshold for conversion to open exploration. Modifications in technique should be adopted to achieve a successful outcome.
INTRODUCTION
The introduction of laparoscopic cholecystectomy in surgical practice was pioneered by Mouret in 1987.1 It rapidly replaced “traditional” open cholecystectomy as the curative treatment of cholecystolithiasis.2,3 The switch to laparoscopic cholecystectomy was attributed to its obvious benefits of a reduction in hospital stay, decreased postoperative pain, early return to normal activity and an improved cosmetic result.4
Many authors consider acute cholecystitis with associated inflammatory edema and adhesions a relative or absolute contraindication to laparoscopic cholecystectomy.5,6 This philosophy of treatment denies those patients presenting with acute cholecystitis the advantages of a laparoscopic approach. The aim of this study is to demonstrate the safety and efficacy of laparoscopic cholecystectomy performed as emergency treatment for patients with acute calculous cholecystitis. Technical modifications adopted during this study will be presented.
PATIENTS AND METHODS
From April, 1994, through March, 1996, 34 patients presenting with acute abdominal pain were included in this study. Patients were admitted through the emergency room. Routine investigation included a complete blood count, liver function tests and abdominal ultrasonographic scan. Those patients diagnosed as having acute calculous cholecystitis were offered laparoscopic cholecystectomy as the primary surgical treatment. Informed consent was obtained. Parenteral third-generation cephalosporines were started preoperatively and continued at least two days postoperatively. Operative intervention was performed within 12 hours of admission. All operations were per-formed by one surgical team. Each member of the team had performed at least 20 laparoscopic cholecystectomies. The removed specimens were sent for histopathological examination and only those patients with confirmed acutely inflamed gallbladder were included in the study. The operation was carried out in the classical manner but several modifications were used (Table 1) to make exposure and dissection of the gallbladder easier. The gallbladder was aspirated by a Veress needle introduced through the skin directly over the fundus of the gallbladder. Operative cholangiography was not performed routinely in this study. A closed suction drainage system was inserted below the liver at the conclusion of the procedure. The drain was removed when discharge was minimal.
Table 1.
Modifications Adopted in the Technique
| ♦ The use of 10 mm trocars at all sites of port insertion. |
| ♦ Aspiration of gallbladder contents. |
| ♦ The use of sharp grasper to retract the thick gallbladder wall. |
| ♦ Dissection of the fundus first in selected cases. |
| ♦ Ligation of the cystic duct, using Roeder slip knot, rather than clipping. |
| ♦ Routine suction drainage. |
| ♦ Maintaining a low threshold of conversion. |
RESULTS
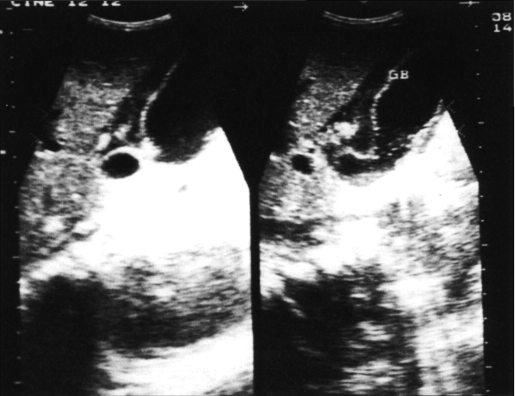
Thirty-four patients diagnosed as having acute calculous cholecystitis were offered laparoscopic cholecystectomy over a 24-month period. They were six males and 28 females, with a mean age of 41 years (range 23-66). All patients presented with acute upper abdominal pain. Other presenting features are shown in (Table 2). The diagnosis was based upon clinical, laboratory and ultra-sonographic criteria (Table 3). Inclusion criteria are shown in (Table 4). Patients included in the study fulfilled all the essential criteria and at least one of each category of the additional criteria. Eight patients (23.5%) had altered liver function tests (raised hepatic enzymes, elevated serum bilirubin or both) but none were jaundiced. Four patients (11.7%) were diabetic. The leukocytic count ranged from 10,000 to 24800 /mm3 (mean 12.4). Thirty-one patients had multiple gallstones and only three had a single stone in the gallbladder. Ultrasonography failed to detect stones in one patient (2.9%), however, computerized tomography detected a stone impacted in the cystic duct of this patient. A positive sonographic Murphy's sign (maximal tenderness elicited when the transducer passed over the gallbladder) was detected in 21 patients (62%). Ultrasonographic signs (Figure 1) predicted acute inflammation of the gallbladder in all cases.
Table 2.
Presenting Features on Admission
| Number | % | |
|---|---|---|
| Acute upper abdominal pain | 34 | 100 |
| Fever | 25 | 74 |
| Nausea | 10 | 29 |
| Vomiting | 8 | 24 |
| Palpable gallbladder | 15 | 44 |
| Leukocytosis | 27 | 79 |
| Altered liver functions | 8 | 24 |
Table 3.
Ultrasonographic Criteria for Diagnosing Acute Calcular Cholecystitis
| Number | % | |
|---|---|---|
| Distended gallbladder | 30 | 88 |
| Thickened gallbladder wall > 6 mm | 34 | 100 |
| Double wall sign (i.e. edema of the wall) | 14 | 41 |
| The presence of stone(s) | 33 | 97 |
| Positive ultrasonographic Murphy's sign | 21 | 62 |
| The presence of pericholecystic fluid | 6 | 18 |
Table 4.
Inclusion Criteria
| Essential Criteria |
| Acute right upper abdominal pain. |
| Radiological evidence of gallbladder stones. |
| Histopathological confirmation of an acute inflammatory process. |
| Additional Criteria |
| Other clinical signs of acute inflammation. |
| One or more ultrasonographic evidence of acute inflamation. |
Figure 1A.
Sonographic evidence of acute cholecystitis: thick layered gallbladder wall with stone inside.
Figure 1B.
Sonographic evidence of acute cholecystitis: pericholecystic collection.
The procedure was successfully completed in 31 patients (Table 5), including the diabetic patients. In four cases, the gallbladder dissection was initiated at the fundus as identification of the cystic duct and cystic artery was difficult. The main histopathological findings included a thick edematous gallbladder wall, mucosal congestion with frequent ulceration and leukocytic infiltration. The mean length of the laparoscopic procedure, measured from skin incision to skin closure, was 43 minutes (range 25 - 85). Patients required 0-6 doses of narcotic analgesics (mean 2.1). The morbidity rate was 8.8% (3/34); all complications were minor except for one patient who had a bile duct injury consisting of partial avulsion of the cystic duct from the common bile duct. The cystic duct injury was detected intraoperatively and the case was converted to open laparotomy. The common bile duct was repaired around a T-tube. Two patients had prolonged postoperative bilious drainage that responded to conservative treatment. All of these cases responded satisfactorily and were well on follow-up. Three patients (8.8%) had their operation converted to an open cholecystectomy; one due to the bile duct injury mentioned above, and the other two because of severe inflammatory edema and adhesions that rendered dissection of Calot's triangle unsafe. There was no mortality and no re-operation in this series. We did not encounter any cases of gangrenous or emphysematous cholecystitis.
Table 5.
The Length of Operative Procedure and Hospital Stay
| Laparoscopic | Open | |
|---|---|---|
| (n=31) | (n=3) | |
| Mean length of procedure (minutes) | 43 | 66 |
| Range (minutes) | 25-85 | 48-75 |
| Mean length of hospital stay (days) | 2.8 | 5.3 |
| Range (days) | 2-5 | 3-9 |
DISCUSSION
Cholecystectomy remains the only curative treatment for gallbladder stones. The laparoscopic approach has replaced conventional laparotomy because of its well established advantages.7 Fifteen percent to 20 percent of patients with gallbladder stone disease present with acute inflammation. Acute inflammation of the gallbladder distorts the anatomy due to edema and adhesions. Acute cholecystitis, therefore, carries a high rate of complications.8 Many patients presenting with acute cholecystitis have been denied laparoscopic treatment for fear of these complications. Published studies concerning laparoscopic cholecystectomy for acute cholecystitis suggest contradictory results.9–12 In these studies, the conversion rate ranged from 3% to 75% and the complication rate from 3% to 45%. These results are inferior to those of elective laparoscopic cholecystectomy as it is to be expected that removal of the acutely inflamed gallbladder is a more difficult operative procedure.
The Diagnosis:
As early intervention is crucial to the successful completion of the procedure, early diagnosis is particularly important.13,14 Acute cholecystitis should be excluded in any patient presenting with acute upper right quadrant pain, fever and leukocytosis. Although cholescintigraphy has a higher accuracy rate than ultrasound scanning, the former is not widely available and is far more expensive. There are many sonographic signs of acute cholecystitis.15,16 The most reliable ultrasonographic signs of acute cholecystitis are a thickened edematous gallbladder wall, a positive sonographic Murphy's sign and the presence of pericholecystic fluid collection.17 These signs are not found in every case of acute cholecystitis. Multiple positive ultrasono graphic findings yield greater accuracy in the diagnosis of acute cholecystitis. Ultrasonography was used as the primary diagnostic modality in this series and it predicted acute inflammation of the gallbladder in all cases. Ultrasound failed to detect a stone in only one patient. Ultrasonography, however, does not predict the severity of inflammation and hence is of little value in predicting the possibility of conversion except in those complications such as perforation.
The Management:
Laparoscopic cholecystectomy was offered to all patients diagnosed as having acute calculous cholecystitis. We used a modified three-trocar technique. All operations were done early (within 12 hours of admission), but this was not always early enough. Some patients, including two of the converted cases, presented to the emergency department 24 hours after the onset of symptoms. A delay in surgical interference only allows the inflammatory process to intensify, rendering operation more difficult and conversion more likely. In this series the conversion rate was 8.8% and the complication rate was 8.8%. These rates are higher than the average rates for elective cholecystectomy, 18,19 but are satisfactory for this group of patients with acute disease. In those cases converted, removal of the gallbladder was difficult even at laparotomy.
The use of three trocars as a modification of laparoscopic technique appeared to be very valuable. We feel that manipulation of instruments through these three trocar sites allowed for easier handling and maneuverability of the gall-bladder.
One of the major difficulties in acute cases is grasping the gallbladder for adequate retraction. Aspiration of gallbladder content makes grasping and retracting the thickened wall easier. Sharp graspers should be used routinely to secure the gallbladder. Injury of the wall does not usually lead to leakage of gallbladder content because of its thickness and decompressed state. Ligation of the cystic duct is sometimes required as the metal clip may be too small to safely occlude the edematous duct. We used an extra-corporeal knot-tying technique for these ligatures.
Operative cholangiography was not done routinely in this study. Operative cholangiography is thought to serve two main functions; the first is to detect common bile duct stones and the second to delineate biliary anatomy prior to dissection of structures in Calot's triangle and enhance the safety of this procedure. Its efficacy in both functions is not absolute. Therefore, the decision to perform routine operative cholangiography in every case of laparoscopic cholecystectomy is controversial and many surgeons prefer to use it selectively.20–22 In those cases where we dissected the fundus first, this approach was used because it was impossible to clearly identify the cystic duct and artery through a Calot's triangle exploration. Bleeding from the liver bed was a problem during this approach, but it could be usually controlled or minimized with electrocautery. The fundus-first operation took longer, but was safely completed in all of these cases.
The fact that the laparoscopic procedures can be abandoned to a traditional open cholecystectomy if difficulty is encountered contributes to the safety of the patient. For these reasons, we believe laparoscopic cholecystectomy should be offered as the standard treatment for patients with acute cholecystitis as it is for patients with chronic gall-bladder disease.
A low threshold for conversion to an open procedure should be maintained. The decision to convert should be taken early in the procedure. The reason for conversion should not be a complication but rather to avoid one. In the two cases converted in this series, the decision was taken within the first 10 minutes after exploring Calot's tri-angle and assessing the severity of edema and adhesions. The most important indication for conversion is the inability to clearly and safely identify structures in the Calot's tri-angle.
In those cases of acute cholecystitis treated with laparoscopic means, patients enjoy all of the advantages of a laparoscopic approach, namely reduced postoperative pain, shorter hospital stay and a better cosmetic result.
CONCLUSION
Laparoscopic cholecystectomy should be the standard pri-mary surgical treatment for patients presenting with acute cholecystitis. Early intervention is crucial for successful completion of the procedure. Ultrasonography is the method of choice for early diagnosis of these cases because of its wide availability and great accuracy. The procedure should be attempted only by experienced surgeons. The technique should be modified as necessary to achieve a successful outcome.
The question of whether to do a laparoscopic cholecystostomy or laparotomy in difficult cases remains to be answered by the operating surgeon, depending upon his experience and laparoscopic skill level.
References:
- 1. Mouret G. From the first laparoscopic cholecystectomy to the frontiers of laparoscopic surgery. The prospective futures. Dig Surg. 1991;8:124–125 [Google Scholar]
- 2. The Southern Surgeons Club A prospective analysis of 1,518 laparoscopic cholecystectomies. N Engl J Med. 1991;161:385–387 [DOI] [PubMed] [Google Scholar]
- 3. Soper NJ, Stockmann PT, Dunnegan DL, Ashley SW. Laparoscopic cholecystectomy. The new “Gold standard”? Arch Surg. 1992;127:400–403 [DOI] [PubMed] [Google Scholar]
- 4. Buanes T, Mjaland O. Complications in laparoscopic and open cholecystectomy: A prospective comparative trial. Surg Laparosc Endosc. 1996;6:266–272 [PubMed] [Google Scholar]
- 5. Soper NJ. Laparoscopic treatment of gallstones. In Andersen DK, Gadacez TR, Schirmer BD, Soper NJ, eds. Advances in Minimally Invasive Surgery. New York: World Medical Press, 1993:37–73 [Google Scholar]
- 6. Phillips EH, Carroll BJ, Fallas MJ. Laparoscopically guided cholecystectomy: A detailed report of the first 453 cases performed by one surgical team. Am Surg. 1993;59:235–242 [PubMed] [Google Scholar]
- 7. Perissat J. Laparoscopic cholecystectomy: The European experience. Am J Surg. 1993;165:444–449 [DOI] [PubMed] [Google Scholar]
- 8. Hermann RE. Surgery for acute and chronic cholecystitis. Surg Clin North Am. 1990;70:1263–1275 [DOI] [PubMed] [Google Scholar]
- 9. Singer JA, McKeen RV. Laparoscopic cholecystectomy for acute or gangrenous cholecystitis. Am Surg. 1994;60:326–328 [PubMed] [Google Scholar]
- 10. Soper NJ, Brunt LM, Gallery MP, Edmundowicz SA, Alipert G. Role of laparoscopic cholecystectomy in the management of acute gall stone pancreatitis. Am J Surg. 1994;167:42–51 [DOI] [PubMed] [Google Scholar]
- 11. Fabre JM, Fagot H, Domergue J, Guillon F, Balmes M, Zaragosa C, Baumel H. Laparoscopic cholecystectomy in complicated cholelithiasis. Surg Endosc. 1994;8:1198–201 [DOI] [PubMed] [Google Scholar]
- 12. Kum CK, Goh PM, Isaac JR, Tekant Y, Ngoi SS. Laparoscopic cholecystectomy for acute cholecystitis. Br J Surg. 1994;81:1651–1654 [DOI] [PubMed] [Google Scholar]
- 13. Hawasli A. Timing of laparoscopic cholecystectomy in acute cholecystitis. J Laparosc Endo Surg. 1994;4:9-16 [DOI] [PubMed] [Google Scholar]
- 14. Miyazaki K, Uchiyama A, Nakayama F. Use of ultrasono-graphic risk score in the timing of operative intervention for acute cholecystitis. Arch Surg. 1988;123:487–489 [DOI] [PubMed] [Google Scholar]
- 15. Simeone JF, Brink JA, Mueller PR, et al. The sonographic diagnosis of acute gangrenous cholecystitis: importance of the Murphy sign. AJR. 1989;152:289–290 [DOI] [PubMed] [Google Scholar]
- 16. Lauritsen KB, Sommer W, Hahn L, Henriksen JH. Cholescintigraphy and ultrasonography in patients suspected of having acute cholecystitis. Scand J Gastroenterol 1988;23:42–46 [DOI] [PubMed] [Google Scholar]
- 17. Rails PW, Colletti PM, Lapin SA, et al. Real-time sonography in suspected acute cholecystitis. Prospective evaluation of primary and secondary signs. Radiology. 1985;155:767–771 [DOI] [PubMed] [Google Scholar]
- 18. William's LF, Chapman WC, Bonau RA, Boyd RW, Jacobs JK. Comparison of laparoscopic cholecystectomy with open cholecystectomy in a single center. Am J Surg. 1993;165:459–465 [DOI] [PubMed] [Google Scholar]
- 19. Larson GM, Vitale GC, Casey J, et al. Multipractice analysis of laparoscopic cholecystectomy in 1,983 patients. Am J Surg. 1992;165:221–226 [DOI] [PubMed] [Google Scholar]
- 20. Lorimer JW, Fairfull-Smith RJ. Intraoperative cholangiography is not essential to avoid duct injuries during laparoscopic cholecystectomy. Am J Surg. 1995;169:244–247 [DOI] [PubMed] [Google Scholar]
- 21. Lillemoe KD, Yeo CJ, Talamini MA, et al. Selective cholangiography: current role in laparoscopic cholecystectomy. Ann Surg. 1992;215:669–676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dorazio RA. Selective operative cholangiography in laparoscopic cholecystectomy. Am Surg. 1995;61:911–913 [PubMed] [Google Scholar]