A review of the English literature concerning spilled gallstones during laparoscopic cholecystectomy is compared with one institution's experience of four cases during 1,726 laparoscopic cholecystectomies performed over a four-year period. Strategies regarding management and treatment are discussed.
Keywords: Cholecystectomy-laparoscopic, Adverse effects, Wound infection, Abscess
Abstract
Objective:
Our purpose was to report the occurrence of abscess following spilled gallstones during laparoscopic cholecystectomy as experienced at Good Samaritan Hospital, and to compare it to the experience of other institutions in order to identify the incidence, characteristics and possible risk factors for the development of this complication.
Methods:
Four case reports of abscess following spilled gallstones during laparoscopic cholecystectomy are presented. The English literature was reviewed, and characteristics of the case reports found in the literature were compared.
Results:
In four years at this institution, four reports of abscess formation following laparoscopic cholecystectomy have been identified. Two occurred in elderly females and were located in the right flank in both. Two were in middle-aged men, both diabetic. One abscess was in the right flank and one in the right pleural space. Twenty-three cases were found in the literature. The average age was 65 years; there were 12 men and 11 women. The locations of abscess formation were trocar sites (most common), right subphrenic space, right flank or retroperitoneum, and pelvis. The average time to presentation was 4-5 months (range 4 days - 12 months).
Conclusions:
Abscess formation following spilled gall-stones during laparoscopic cholecystectomy occurs infrequently, but can be debilitating and require more than one procedure. The older population appears to be at greater risk. Future prospective studies of patients who undergo laparoscopic cholecystectomy are needed to more accurately determine the incidence of this complication and to identify the population at risk.
INTRODUCTION
Laparoscopic cholecystectomy is the standard of care for the surgical treatment of gallbladder disease. Since its introduction in 1987 by Dubois et al.,1 the surgical community has sought to determine the full spectrum of complications associated with this technique. Several published series of laparoscopic cholecystectomies have found an overall morbidity of about 5%.2–4 The most common complications were retained common bile duct stones, bile leak, superficial wound infection, and, the most serious, bile duct injury. One complication that may be occurring more often with the laparoscopic technique is gallbladder perforation and spillage of stones into the peritoneal cavity. How often this event leads to adverse sequela remains unanswered. In the following article, four cases of adverse sequela from spilled gallstones are presented with an extensive review of the literature in order to evaluate the incidence, etiology, possible risk factors, and treatment of spilled gallstones and intra-abdominal abscess.
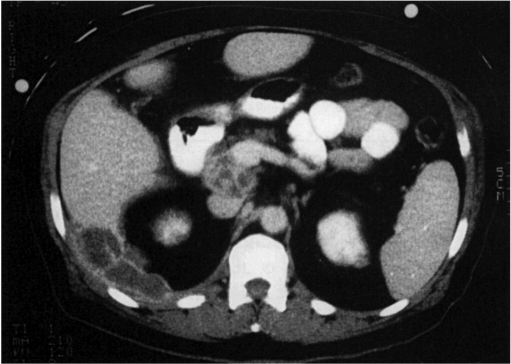
CASE 1
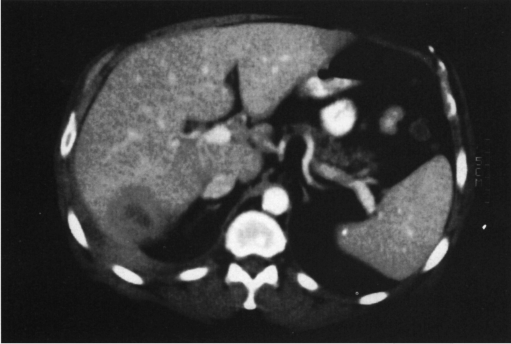
Six weeks following coronary artery bypass grafting (CABG), a 58-year-old white male with uncontrolled diabetes developed right upper quadrant pain, nausea, vomiting and elevated liver function tests. He underwent laparoscopic cholecystectomy for acute cholecystitis. There was spillage of stones and bile during the case and only some of the stones were retrieved. His initial postoperative course was uneventful. He presented three months later, febrile, complaining of right upper quadrant and right flank pain. Computed tomography (CT) of the abdomen revealed a large subhepatic and retroperitoneal fluid collection which was percutaneously drained (Figure 1). The culture grew Klebsiella. He was treated with intravenous piperacillin and then switched to oral ciprofloxacin for a ten day course. His symptoms were relieved only to recur two months later. The CT scan showed recurrence of the abscess (Figure 2). He was taken to the operating room for a posterior exploration that revealed retained gallstones at the base of the abscess. These were removed and the wound debrided and irrigated. The culture again grew Klebsiella sensitive to ciprofloxacin. He was discharged with another course of ciprofloxacin and wound care. He returned again five months later to have further debridement. He has since required another exploration in the operating room and is currently recovering.
Figure 1.
Retroperitoneal abscess three months after laparoscopic cholecystectomy. Stones were spilled during the procedure. Stones were removed during open debridement.
Figure 2.
Recurrent abscess two months after percutaneous drainage of abscess in Figure 1.
CASE 2
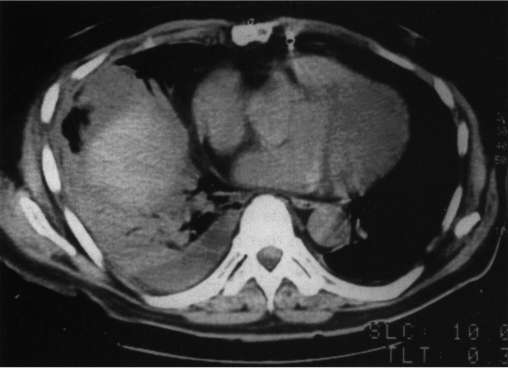
A 53-year-old white male, status post CABG, underwent elective laparoscopic cholecystectomy for chronic cholecystitis during which there was spillage of bile and stones into the peritoneal cavity. He received a preoperative dose of cefotetan and was discharged home on amoxicillin/clavulanic acid. He returned six days later with fever and leukocytosis. A CT of the abdomen revealed a right pleural effusion and a fluid collection in the gallbladder fossa (Figure 3). The fluid was percutaneously drained, and the culture grew Enterococcus sensitive to ampicillin. He was treated with intravenous cefotetan and metronidazole and discharged on amoxicillin/clavulanic acid with resolution of his symptoms.
Figure 3.
Pleural effusion six days after laparoscopic cholecystectomy with stone spillage.
CASE 3
An 85-year-old white female presented to the emergency department complaining of a painful indurated area over her right flank. The patient reportedly fell at home three days prior to presentation and hit her right side on a chair. She did not admit to any other injuries. She also denied recent febrile illness. She did report occasional pain over her right side but attributed this to her osteoarthritis. Laboratory evaluation demonstrated a white blood cell count of 15,000 with a left shift.
She had a history of laparoscopic cholecystectomy in 1991 and reported persistent pain in her right upper quadrant since her surgery. A right upper quadrant ultrasound revealed no abnormalities. Laboratory studies were also negative. She denied history of jaundice, dark urine or acholic stools.
The area over the right flank was clinically felt to represent an abscess of unknown etiology and was opened in the emergency department under local anesthesia. A large amount of pus was released and the wound was packed open. A CT scan was ordered to rule out a perforated viscus or a renal tumor. The next morning numerous small gallstones were noted to be on the packing as it was removed. The CT scan showed a large abscess cavity involving the right retroperitoneum (Figure 4). The patient was taken to the operating room where the cavity was widely opened and drained. Additional gallstones were recovered. The patient recovered without any additional problems and the wound is now healed.
Figure 4.
Retroperitoneal abscess several years after laparoscopic cholecystectomy. Bright area in center of abscess represents "spilled" gallstones that were removed during abscess drainage.
CASE 4
A 91-year-old white female nursing home resident was found to have a chronically draining sinus tract located on her right side just above the posterior superior iliac spine.
She had previously undergone drainage of a subcutaneous abscess in this location. This condition had been managed with repeated local debridements and dressing changes for a period of two years. A sinogram was obtained in an effort to elucidate the etiology of the problem, but it was not helpful.
The patient underwent a formal debridement of the area in an effort to eliminate the source of chronic infection. As the tract was explored, a large (2 × 2 cm) gallstone was retrieved from the tract with several smaller stones. The wound was packed open and had healed after two weeks. The patient had undergone a laparoscopic cholecystectomy 30 months prior to her presentation to our service.
DISCUSSION
The complication of gallbladder perforation and spilled gallstones has been reviewed by several authors2,3,5–7 (Table 1). The incidence of perforation ranged from 9% to 40% stones were retained 1% to 13% of the time. Soper et al.6 conducted a prospective study specifically designed to identify the rate of spilled stones. They reported a rate of 32%, with a 5% incidence of acute gallbladders.
Table 1.
Incidence of Perforation
| Author | No. Patients | Perforation | Retained Stones | Acute GB |
|---|---|---|---|---|
| Donahue et al.3 | 200 | 26% | 13% | 6% |
| Peters et al.2 | 283 | 40% | NL | 5% |
| Huang et al.5 | 200 | 10% | 5% | 15% |
| Soper et al.6 | 250 | 32% | NL | 5% |
| Strasberg et al.7 | 2201 | 9% | 1% | NL |
NL = not listed; GB = gallbladder
The incidence of gallbladder perforation is believed to exceed that of the traditional open method, although not officially reported in the literature. During laparoscopic cholecystectomy, there are three maneuvers that can result in gallbladder perforation. First, the gallbladder is used for traction to assist in the dissection of the cystic duct and cystic artery. This exposes the gallbladder to excessive traction forces and graspers that may tear the wall of the gall-bladder. Secondly, the gallbladder may be entered during dissection from the liver bed. Finally, the gallbladder is extracted from the abdomen through a small incision, at which time it may be put under high pressures. Perforation is easily avoided if extension of the skin incision is per-formed when needed. The amount of inflammation pre-sent may also contribute to the rate of perforation.
Inflammation could cause the gallbladder wall to be friable and more prone to tearing under the stress of traction. It may also cause it to be more difficult to define the plane between the liver and the gallbladder during dissection. Huang and colleagues5 found that 12 of 20 gallbladders perforated were acutely inflamed.
Despite the high rate of perforation and associated stone spillage, it is not entirely clear what the full implications of this event are. In the one prospective analysis of this problem, Soper et al.6 found only an increase in operative time when perforation and spillage occurred. This time was spent retrieving stones and irrigating the abdomen. None of the 250 patients developed an intra-abdominal abscess over a 3-16 month follow-up. Nonetheless, abscess formation or chronically draining sinus tracts due to retained stones has been documented. In Donohue's3 series, a patient required laparotomy with drainage of the abscess and removal of the retained stones. A patient in Huang's5 series developed a chronically draining sinus tract at the subcostal trocar site. The authors of this review have encountered four cases of intra-abdominal abscess due to spilled stones during laparoscopic cholecystectomy. Three of the laparoscopic cholecystectomies were done at Good Samaritan Hospital where 1,726 laparoscopic cholecystectomies have been performed since 1993. The fourth case was performed at a smaller affiliate hospital. Two of these four presented back at Good Samaritan Hospital where the diagnosis of abscess secondary to spilled stones was made. The other two patients were evaluated at other hospitals. Although it has not been prospectively evaluated, it is the authors' experience that stones are spilled frequently. How the stones are dealt with appears to be surgeon-specific, depending on the perceived severity of the spillage.
Finally, there are 23 case reports in the English literature dating back to 1992 that describe intra-abdominal abscess secondary to retained gallstones1,5,12–29 (Table 3). The mean age of the patients was 65 years (range 31-90 years). The gender distribution was 12 males and 11 females. The average time to presentation was 4-5 months (range 4 days - 12 months). The abscess or sinus tract was located by CT or ultrasound. The sites of involvement were all trocar sites (7), subphrenic (5), right flank or retroperitoneum (3), subhepatic (4), omentum (3), pulmonary (2), pelvis/ovary (4). Some cases had more than one location. Four cases required more than one procedure. The bacteria involved (when described) were Escherichia coli (6), Klebsiella (4), Enterobacter (1), Enterococcus (1), Lactobacillus (1), and Serratia (1). The gallbladder was acutely inflamed in five cases. Of these, 2 were empyema and one was gangrenous. The type of stone extracted, when reported, was bilirubinate in four and cholesterol in one.
Table 3.
Reported Cases in the Literature
| Author/year | Age/gender | Presentation | Site | Treatment | Bacteria | Other |
|---|---|---|---|---|---|---|
| Anteby, 199212 | 53, F | 4 mos | Lt. ovary/pelvis | Laparotomy | NR | Gangrenous gallbladder |
| Baird, 199213 | NR, F | 10 days | Subhepatic | Percutaneous laparotomy | NR | Empyema |
| Brazensky, 199314 | 75, M | 4 mos | Rt. pleural effusion | Thoracoscopy | E coli, Klebsiella | Empyema |
| Campbell, 19921 | 80, F | 4 days: fever, RUQ pain, leukocytosis | GB fossa | Percutaneous drainage | Serratia marcescens | - |
| 3 mos: fever, redness, swelling | Rt. flank | Multiple I&D | NR | - | ||
| 9 mos | Rt. flank | Laparotomy, stone removal | NR | - | ||
| 12 mos | Lt. femoral hernia | McVay repair, stone removal | NR | - | ||
| Catarci, 199315 | 60, M | 3 mos: fever, abd. pain, drainage | Epigastric trocar site | Laparotomy, stone removal | NR | - |
| Culles, 199216 | 63, M | 6 mos: Small bowel obstruction | Omentum | Laparotomy, stone removal | NR | - |
| Dreznik, 199317 | 31, F | 4 mos | Subcostal trocar site | I&D | NR | - |
| Eldar, 199418 | 52, F | 12 mos | Umbilical trocar site | I&D | NR | - |
| Eisenstat, 199319 | 82, M | 4 mos | Umbilical, preperitoneal | Multiple laparotomies & stone removal | Lactobacillus casei | IDDM, chronic cholecystitis |
| Gallinaro, 199420 | 71, F | 8 mos | Rt. flank, retroperitoneum | I&D | Escherichia coli | Acute cholecystitis |
| Golub, 199421 | 71, F | 6 wks | Umbilical trocar | I&D | Klebsiella | Cholesterol stones |
| 5 mos | Omentum | Laparotomy, stone removal | NR | - | ||
| Guy, 199322 | 77, F | 5 mos | Epigastric trocar | I&D | NR | Empyema |
| Huang, 19925 | 69, M | 2 wks | Subcostal trocar site | I&D | NR | Acute cholecystitis |
| Lee, 199323 | 58, F | 4 mos: cholelithoptysis | Subphrenic | Laparotomy, stone removal | Enterobacter | Mixed stones; NIDDM |
| Lee, 199323 | 52, M | 9 mos: cholelithoptysis | Subphrenic, retroperitoneal | Laparotomy, stone removal | Klebsiella | Bilirubinate stones |
| Leslie, 199424 | 58, M | 5 mos | Subphrenic, empyema | Percutaneous drainage × 3, laparotomy, stone removal | Escherichia coli | - |
| Mellinger, 199425 | 54, F | 7 mos | Rt. flank, retroperitoneal | I&D × 2, laparotomy, resect 11th rib, stone removal | Escherichia coli | Chronic cholecystitis |
| Tschmelitsch, 199326 | 57, M | 5 mos | Rt. lower quadrant | Laparotomy, stone removal | Escherichia coli | - |
| Trerotola, 199327 | 79, M | 2 mos | Subhepatic | Percutaneous drainage & stone removal | Klebsiella, Enterococcus | - |
| VanBrunt, 199428 | 72, M | 2 mos | Subhepatic | Percutaneous drainage | NR | - |
| Wilton, 199329 | 53, M | 9 mos | Subphrenic | Percutaneous drainage & stone removal | NR | - |
| Tursi, 199332 | 70, F | 2 mos | Pelvis/ovary | Laparotomy, BSO | NR | Chronic cholecystitis |
| Neumeyer, 199633 | 90, M | 4 mos | Pleural effusion; subphrenic | Thoracoscopic drainage | NR | Bilirubinate stones |
RUQ=right upper quadrant; GB=gallbladder; I&D=incision & drainage; NR=not recorded; BSO=bilateral salpingo-oophorectomy; IDDM=insulin dependent diabetes mellitus; NIDDM= non-insulin dependent diabetes mellitus
Despite the high rate of spillage reported in the literature, the incidence of abscess appears to be low (Table 2). Our experience at Good Samaritan Hospital is similar to these reports: four cases of abscess out of 1,726 laparoscopic cholecystectomies done in four years. This causes one to wonder what it is about those patients who develop abscesses that puts them at risk. After reviewing the 23 case reports in the literature, a few observations were made. The mean age of the patients, 65 years, exceeded the mean age of patients undergoing laparoscopic cholecystectomy by more than ten years.3–6,8,9 Two of the patients described in the literature, and two of our patients were documented as being diabetic; also, two patients had a recent history of CABG suggesting that the patient's medical condition may increase the risk for abscess formation.
Table 2.
Incidence of Abscess
| Author | No. Patients | Abscess |
|---|---|---|
| Huang et al.5 | 200 | 1 |
| Donahue et al.3 | 200 | 1 |
| SSC4 | 1518 | 2 |
| Martin et al.9 | 162 | 1 |
| Yves-Marie et al.8 | 60 | 1 |
| Deziel et al.10 | 77604 | 6 |
| Perissat et al.11 | 700 | 6 |
SSC = Southern Surgeons Club
The type and amount of biliary disease may also put the patient at risk. As previously mentioned, patients with acute cholecystitis may be more likely to experience spillage of bile and stones. Even in the absence of clinically acute inflammation, up to 30% of bile cultures are positive for bacteria.30 Whether the bile is infected or not may not be as important to abscess formation as the stone itself. In an animal study, Johnston, et al.30 found that rats under-going laparotomy with placement of a stone and bile intraperitoneally developed adhesions around the stone. Two rats developed abscess at the stone site. Surprisingly, the bile was sterile in the group that developed abscess. It is possible that the stone itself harbored active bacteria. A study by Stewart et al.31 examined 32 pigment stones and 35 cholesterol stones. Seventy-eight percent of the pigment stones had evidence of bacterial microcolonies whereas none of the cholesterol stones showed evidence of bacteria. Only five of the 23 cases reported in the literature document the type of stone spilled. Of these, four were found to be bilirubinate. This spillage of black pigment stones may be more likely to precipitate an abscess.
Prevention of abscess by prevention of spillage is the best policy. Gentle traction and careful dissection should be maintained in all cases. If perforation does occur, the spill should be contained by placing an endo-loop or clips over the area or placing the grasper in such a way as to close the perforation. This may prevent stones from falling out during the rest of the dissection. Removal of the gallbladder from the epigastric or umbilical incision should be visualized with the scope to identify spillage if it occurs. If the stone or stones are too large, the fascial incision can be easily extended. The gallbladder can be suction evacuated to reduce its size, and the stones removed with a ring forceps. Finally, the gallbladder can be placed in a sterile bag for removal.
When stones are spilled, as many as possible should be retrieved, even if operative time is increased. Several devices exist to facilitate this process. One may use a spoon, disposable bag or sleeve, or the large 20-mm shuttle collector. There are some who recommend immediate laparotomy for spilled stone removal. Most authors disagree with this approach, believing that time is better spent preventing perforation, containing the spill, and retrieving stones laparoscopically, since most patients will not develop a major complication from this event. The role of perioperative antibiotics in prevention of postoperative abscess has not been defined, but probably has little effect.
When intra-abdominal abscess does occur most patients present within five months, but some may take longer than one year. The diagnosis should be suspected if the patient has a history of laparoscopic cholecystectomy. The operative record should be reviewed for report of stone spillage during the procedure, although this may not be accurate. The authors of this review now consistently document whether stones were spilled and if the stones were retrieved, but this is most likely an exception to the usual dictated reports. The operative reports of the four cases in this study did not describe perforation or spillage of stones. Also, the pathology report may be helpful if no stones were found with the specimen, especially if stones were documented by preoperative ultrasound. This was the case in the fourth patient.
The typical symptoms are pain and fever. A chronic sinus tract may also be present. The diagnosis is made by CT or ultrasound, and first attempts at cure are made using these modalities for percutaneous drainage. Additional procedures may be required, and some patients may require laparotomy for complete drainage and removal of stones. Antibiotic coverage should be based on culture results and coverage of the more common biliary organisms.
CONCLUSION
During laparoscopic cholecystectomy, perforation of the gallbladder with spillage of stones is common, but the development of intra-abdominal abscess is not. Because of the low incidence of intra abdominal abscess, immediate laparotomy is not indicated, but attempts should be made to remove all the stones laparoscopically. Meticulous surgical technique is the best preventative measure. When intra-abdominal abscesses do occur, they can be very debilitating and require more than one procedure to achieve resolution of the abscess.
After reviewing the available data in the literature, there may be a patient population at higher risk for developing long-term complications from retained gallstones. Older, debilitated patients with underlying medical conditions (i.e., IDDM) may be at greater risk. A prospective analysis of all patients undergoing laparoscopic cholecystectomy is needed to accurately determine the incidence of these long-term complications and the specific population at risk.
Footnotes
Presented at the Annual Meeting of the Society of Laparoendoscopic Surgeons, Endo Expo ′96, December 5-7, 1996 in Orlando, Florida.
References:
- 1. Campbell WB, McGarity WC. An unusual complication of laparoscopic cholecystectomy. Am Surg. 1992;58:64l–642 [PubMed] [Google Scholar]
- 2. Peters JH, Gibbons GD, Innes JT, et al. Complications of laparoscopic cholecystectomy. Surgery. 1991;110:769–778 [PubMed] [Google Scholar]
- 3. Donohue JH, Farnell MB, Grant CS, et al. Laparoscopic cholecystectomy: early Mayo Clinic experience. Mayo Clin Proc. 1992;67:449–455 [DOI] [PubMed] [Google Scholar]
- 4. The Southern Surgeons Club A prospective analysis of 1518 laparoscopic cholecystectomies. N Engl J Med. 1991;324:1073–1078 [DOI] [PubMed] [Google Scholar]
- 5. Huang CS, Tai FC, Shi MY, Chen SF, Wang NY. Complications of laparoscopic cholecystectomy: An analysis of 200 cases. J Formos Med Assoc. 1992;91:785–792 [PubMed] [Google Scholar]
- 6. Soper NJ, Dunnegan DL. Does intraoperative gallbladder perforation influence the early outcome of laparoscopic cholecystectomy? Surg Laparosc Endosc. 1991;1:156–l6l [PubMed] [Google Scholar]
- 7. Strasberg SM, Sanabria JR, Clavien PA. Complications of laparoscopic cholecystectomy. Can J Surg. 1992;35:275–280 [PubMed] [Google Scholar]
- 8. Dion YM, Morin J. Laparoscopic cholecystectomy: a report of 60 cases. Can J Surg. 1990;33:483–486 [PubMed] [Google Scholar]
- 9. Martin IG, Holdsworth PJ, Asker J, et al. Laparoscopic cholecystectomy as a routine procedure for gallstones: results of an “all-comers” policy. Br J Surg. 1992;79:807–810 [DOI] [PubMed] [Google Scholar]
- 10. Deziel DJ, Millikan KW, Economou SG, Doolas A, Ko ST, Airan MC. Complications of laparoscopic cholecystectomy: a national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg. 1993;165:9–14 [DOI] [PubMed] [Google Scholar]
- 11. Perissat J, Collet D, Belliard R, Desplantez J, Magne E. Laparoscopic cholecystectomy: the state of the art. A report on 700 consecutive cases. World J Surg. 1992;l6:1074–1082 [DOI] [PubMed] [Google Scholar]
- 12. Anteby E, Hurwitz A, Palti Z, et al. Gallstones in an ovarian dermoid cyst. N Engl J Med. 1992;327:129–130 [DOI] [PubMed] [Google Scholar]
- 13. Baird DR, Wilson JP, Mason EM, et al. An early review of 800 laparoscopic cholecystectomies at a university-affiliated community teaching hospital. Am Surg. 1992;58:206–210 [PubMed] [Google Scholar]
- 14. Brazinsky SA, Colt HG. Thoracoscopic diagnosis of pleurolithiasis after laparoscopic cholecystectomy. Chest. 1993;104;1273-1274 [DOI] [PubMed] [Google Scholar]
- 15. Catarci M, Zoraca F, Scaccia M, Carboni M. Lost intraperitoneal stones after laparoscopic cholecystectomy: harmless sequela or reason for reoperation? Surg Laparosc Endosc. 1993;3:318–322 [PubMed] [Google Scholar]
- 16. Culles SN, Jeffery PC, McLauchlan G, Bornman PC. Intraperitoneal abscess after laparoscopic cholecystectomy. Surg Laparosc Endosc. 1992;2:337–338 [PubMed] [Google Scholar]
- 17. Dreznik Z, Soper NJ. Trocar site abscess due to spilled gall-stones: an unusual late complication of laparoscopic cholecystectomy. Surg Laparosc Endosc. 1993;3:223–224 [PubMed] [Google Scholar]
- 18. Eldar S, Schein M. Discharge of a gallstone 1 year after laparoscopic cholecystectomy. Arch Surg. 1994;129:1105. [DOI] [PubMed] [Google Scholar]
- 19. Eisenstat S. Abdominal wall abscess due to spilled gallstones. Surg Laparosc Endosc. 1993;3:485–486 [PubMed] [Google Scholar]
- 20. Gallinaro RN, Miller FB. The lost gallstone. Complication after laparoscopic cholecystectomy. Surg Endosc. 1994;8:913–914 [DOI] [PubMed] [Google Scholar]
- 21. Golub R, Nwogu C, Cantu R, Stein H. Gallstone shrapnel contamination during laparoscopic cholecystectomy. Surg Endosc. 1994;8:898–900 [DOI] [PubMed] [Google Scholar]
- 22. Guy PR, Watkin DS, Thompson MH. Late discharge of stones after laparoscopic cholecystectomy. Br J Surg. 1993;80:1052. [DOI] [PubMed] [Google Scholar]
- 23. Lee VS, Paulson EK, Libby E, Flannery JE, Meyers WC. Cholelithoptysis and cholelithorrhea: rare complications of laparoscopic cholecystectomy. Gastroenterology. 1993;105:1877–1881 [DOI] [PubMed] [Google Scholar]
- 24. Leslie KA, Rankin RN, Duff JH. Lost gallstones during laparoscopic cholecystectomy: are they really benign? Can J Surg. 1994;37:240–242 [PubMed] [Google Scholar]
- 25. Mellinger JD, Eldridge TJ, Eddelmon ED, Crabbe MM. Delayed gallstone abscess following laparoscopic cholecystectomy. Surg Endosc. 1994;8:1332–1334 [DOI] [PubMed] [Google Scholar]
- 26. Tschmelitsch J, Glaser K, Klingler A, Klingler P, Bodner E. Late complication caused by stone spillage during laparoscopic cholecystectomy. Lancet. 1993;342:369. [DOI] [PubMed] [Google Scholar]
- 27. Trerotola SO, Lillemoe KD, Malloy PC, Osterman FA., Jr Percutaneous removal of “dropped” gallstones after laparoscopic cholecystectomy. Radiology. 1993;188(2):419–421 [DOI] [PubMed] [Google Scholar]
- 28. VanBrunt PH, Lanzafame RJ. Subhepatic inflammatory mass after laparoscopic cholecystectomy. A delayed complication of spilled gallstones. Arch Surg. 1994;129:882–883 [DOI] [PubMed] [Google Scholar]
- 29. Wilton PB, Andy OJ, Jr, Peters JJ, Thomas CF, Patel VS, Scott-Conner CE. Laparoscopic cholecystectomy, leave no (spilled) stone unturned. Surg Endosc. 1993;7:53–538 [DOI] [PubMed] [Google Scholar]
- 30. Johnston S, O'Malley K, McEntee G, Grace P, Smyth E, Bouchier-Hayes DB. The need to retrieve the dropped stone during laparoscopic cholecystectomy. Am J Surg. 1994;167:608–610 [DOI] [PubMed] [Google Scholar]
- 31. Stewart L, Smith AL, Pellegrini CA, Motson RW, Way LW. Pigment gallstones form as a composite of bacterial microcolonies and pigment solids. Ann Surg. 1987;206:242–250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Tursi JP, Reddy UM, Huggins G. Cholelithiasis of the ovary. Obstet Gynecol. 1993;82:653–654 [PubMed] [Google Scholar]
- 33. Neumeyer DA, LoCicero J, 3rd, Pinkston P. Complex pleural effusion associated with a subphrenic gallstone phlegmen following laparoscopic cholecystectomy. Chest. 1996;109:284–286 [DOI] [PubMed] [Google Scholar]