In those cases where a PEG tube cannot be placed safely, a laparoscopic-assisted technique may be a viable option to complete the procedure.
Keywords: PEG, Gastrostomy, Laparoscopic
Abstract
Background:
Percutaneous endoscopic gastrostomy (PEG) is the most common way of placing a feeding tube. Sometimes PEG cannot be used to safely place a feeding tube, most commonly secondary to an inability to transilluminate the abdominal wall. Whereas open gastrostomy was previously necessary in such cases, laparoscopic-assisted percutaneous endoscopic gastrostomy (LAPEG) is a viable option and is reviewed here.
Methods:
All patients referred for surgical feeding tube placement after unsuccessful PEG were considered for LAPEG. A diagnostic laparoscopy was performed to identify the reason for the failed PEG attempt. Additional ports were placed as needed for the retraction of organs and lysis of adhesions. The stomach was visualized, and the PEG was placed.
Results:
Eight patients who underwent an unsuccessful PEG were taken to the operating room for LAPEG. All patients had successful LAPEG placement. No postoperative complications occurred. The most common reason identified for failed PEG attempt was adhesions followed by overlying organs. Average OR time was 32 minutes.
Conclusion:
When conventional PEG placement is not possible, LAPEG placement should be considered as a time efficient, minimally invasive alternative to open gastrostomy.
INTRODUCTION
Percutaneous endoscopic gastrostomy (PEG) was first introduced in 1980 by Michael Gauderer and Jeff Ponsky.1 Originally designed for pediatrics, it was quickly adopted for use in adult patients. PEG revolutionized feeding tube placement by providing a safe and reliable method for gastrostomy, which could be done by both surgeons and gastroenterologist, while avoiding laparotomy and having a low associated morbidity. PEG has gained wide acceptance, and now over 200,000 PEGs are performed annually in the United States.2
The most common indication for PEG placement is long-term nutritional support. Candidates for PEG include, but are not limited to, those with a history of neurological disease, stroke, cancer, oropharyngeal abnormalities, ventilator dependency, inflammatory bowel disease, and trauma.2–5 PEGs are not recommended for patients requiring <4 weeks of enteral feeding.3 PEGs have also been used as a drainage, decompressive, or gastrointestinal access port in select surgical patients.2,6
The principles of any safely placed gastrostomy include (1) good control of the placement site on the stomach, (2) protection of the surrounding organs, and (3) reliable approximation of the gastric and abdominal wall. Technical factors that may preclude adherence to any one of these principles include intraabdominal adhesions, overriding organs, intraabdominal masses, hepatomegaly, hiatal hernias, obesity, and ascities.3,7
If there is an inability to transilluminate the abdominal wall because of these factors, then a PEG cannot be safely placed.4,7
Although open surgical feeding tube placement may have been the only alternative in the past, today other options exist including several variations of radiographically guided percutaneous and laparoscopically placed catheters.2,4,7,8 Laparoscopic-assisted percutaneous endoscopic gastrostomy (LAPEG), reviewed here, provides a simple, safe option for placing a gastrostomy after an initial unsuccessful PEG attempt.
METHODS
From May 2006 to August 2008, all patients referred to one surgeon for surgical feeding tube placement were considered for LAPEG. A retrospective review of the data was completed. Seven patients were identified as candidates for LAPEG after previously failed attempts at PEG placement, and one patient had a PEG placed that continuously leaked (Table 1). Patients were not considered for LAPEG as a first-line procedure for feeding tube placement.
Table 1.
Patient Demographics and History
| Patient | Age | Sex | History | Indication* |
|---|---|---|---|---|
| 1 | 87 | F | Esophageal Stricture | PEG leaking |
| 2 | 87 | F | Dementia | FTT |
| 3 | 69 | M | Hiatial Hernia | VDRF |
| 4 | 77 | F | Dementia | FTT |
| 5 | 67 | M | MR*/, Dementia | FTT |
| 6 | 95 | M | Dementia | FTT |
| 7 | 89 | F | Dementia | FTT |
| 8 | 90 | F | Dementia | FTT |
PEG = percutaneous endoscopic gastrostomy, MR = mental retardation, FTT = failure to thrive, VDRF = Ventilator Dependent Respiratory Failure
Patients were brought into the operating room and placed under general anesthesia. A 5-mm optical trocar was used to gain access to the abdominal cavity in the right upper quadrant. If the patient had previous surgery in the right upper quadrant, the left upper quadrant was used instead. The abdomen was then explored to identify the reason for the PEG failure (Figure 1). The stomach was then visualized and positioned for PEG insertion. This was done by positioning the patient in a reverse Trendelenburg, retracting any overlying organs, and lysis of adhesions as needed. One or two additional ports were placed to aid in this task.
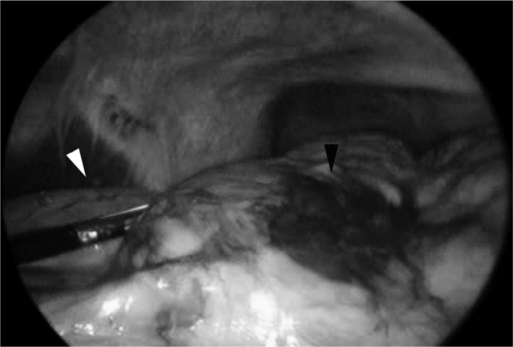
Figure 1.
White arrow on stomach. Black arrow on overriding colon with hematoma from previous percutaneous endoscopic gastrostomy attempt.
An upper endoscopy was performed simultaneously with the laparoscope still in place. The abdominal insufflation pressure was decreased from 15 mm Hg to 6 mm Hg. The PEG was then placed under direct visualization by using the Ponsky pull technique via a small stab incision in the left upper quardrant.9 The separate incision was used to maintain a snug fit around the tube and avoid the leakage that is typically associated with using one of the larger 5-mm port sites. The needle placement into the stomach and the approximation of the gastric and abdominal walls were confirmed visually (Figures 2 and 3).
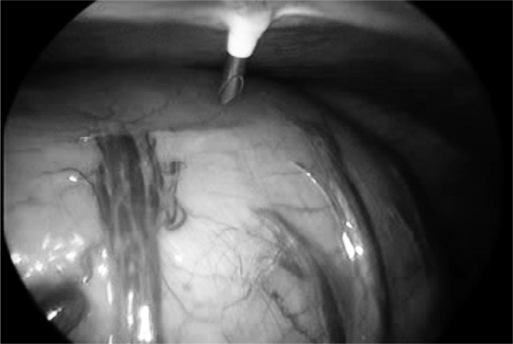
Figure 2.
Direct visualization of needle into stomach.
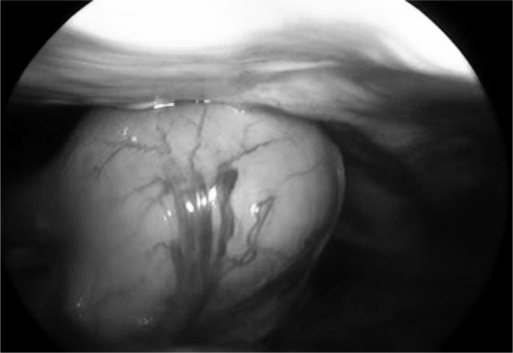
Figure 3.
Approximation of gastric and abdominal walls.
RESULTS
Laparoscopic-assisted percutaneous endoscopic gastrostomy tube placement was performed successfully in 8 patients. No conversions to open gastrostomy were necessary, and no operative complications occurred. All patients were successfully started on tube feeds within 48 hours of the procedure and advanced to goal rate without difficulty. No postoperative complications were noted during the hospitalization, although no long-term follow-up was conducted once the patients were discharged.
The most common reason for unsuccessful PEG placement was the inability to transilluminate the abdominal wall (5 patients). Other reasons for PEG failure included the inability to pass the trocar (2 patients) and continuous leakage after apparently successful placement (1 patient) (Table 2).
Table 2.
Operative Findings and Results
| Patient | Reason for Percutaneous Endoscopic Gastrostomy Failure | Findings on Diagnostic Laparoscopy | Ports |
|---|---|---|---|
| 1 | Not secure to abdominal wall | Adhesions, Omentum between stomach and abdominal wall | 3 |
| 2 | No transillumination | Overlying liver | 2 |
| 3 | No transillumination | Normal | 1 |
| 4 | Unable to pass trocar | Adhesions | 2 |
| 5 | No transillumination | Adhesions and overlying colon | 2 |
| 6 | No transillumination | Overlying colon with hematoma | 2 |
| 7 | Unable to pass trocar | Adhesions | 2 |
| 8 | No transillumination | Overlying colon | 1 |
Intraoperative findings showed that abdominal adhesions were the most common culprit in unsuccessful PEG placement followed by overlying organs. One patient had no obvious finding to explain the failure to transilluminate at the time of the attempted PEG. The patient with a leaking PEG was found to have omentum between the stomach and abdominal wall preventing a secure fit. The number of ports used ranged from 1 to 3. The average operative time was 32 minutes with a range of 19 minutes to 62 minutes.
CONCLUSION
The major disadvantage of LAPEG compared with PEG is the increased cost.10 This is significant enough to prohibit routine use of LAPEG. Contraindications include any medical condition that would preclude the use of general anesthesia, abdominal insufflation, or an upper endoscopy. A relative contraindication would be extensive previous abdominal surgery restricting access to the upper abdomen. A laparoscopically placed jejunostomy tube or an open procedure may be chosen as an alternative. Another potential limitation is the need for an assistant competent to operate the endoscope, although this may provide a good teaching opportunity for residents to handle an endoscope.
The successful record of the PEG has made it one of the most commonly performed procedures in the United States. The LAPEG maintains the fundamental advantage of the PEG: essentially, a low morbidity procedure for gastrostomy tube placement while avoiding laparotomy. It is still a sutureless technique and therefore does not require the surgeon to have advanced laparoscopic training and keeps anesthesia time to a minimum, all while providing a reliable approximation of the stomach and abdominal wall. It has the added benefit of being a diagnostic and therapeutic procedure. Furthermore, the direct visualization in LAPEG allows for superior adherence to the safe principles of gastrostomy placement. Therefore, when conventional PEG placement is not possible, LAPEG placement should be considered as a time efficient, minimally invasive alternative to open gastrostomy.
Contributor Information
Gustavo Lopes, Department of Surgery, US Air Force, Eglin Air Force Base Hospital, FL, USA.
Mark Salcone, Department of Surgery, University of Medicine and Dentistry of New Jersey, School of Osteopathic Medicine, Stratford, New Jersey, USA.
Marc Neff, Kennedy Health System, Cherry Hill, New Jersey, USA..
References:
- 1. Gauderer M, Ponsky J, Izant R. Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15:872–875 [DOI] [PubMed] [Google Scholar]
- 2. Gauderer M. Percutaneous endoscopic gastrostomy-20 years later: a historical perspective. J Pediatr Surg. 2001;36(1):217–219 [DOI] [PubMed] [Google Scholar]
- 3. Prosser B. Common issues in PEG tubes-what every fellow should know. Gastrointest Endosc. 2006;64(6):970–972 [DOI] [PubMed] [Google Scholar]
- 4. Denzer U, Mergener K, Kanzler S, et al. Mini-laparoscopically guided percutaneous gastrostomy and jejunostomy. Gastrointest Endosc. 2003;58(3):434–438 [DOI] [PubMed] [Google Scholar]
- 5. Potack J, Chokhavatia S. Complications of and controversies associated with percutaneous endoscopic gastrostomy: report of a case and literature review. Medscape J Med. 2008;10(6):142. [PMC free article] [PubMed] [Google Scholar]
- 6. Stellato T, Gauderer M. Percutaneous endoscopic gastrostomy for gastrointestinal decompression. Ann Surg. 1987;205:119–122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Croshaw R, Nottingham J. Laparoscopic-assisted percutaneous endoscopic gastrostomy: its role in providing enteric access when percutaneous endoscopic gastrostomy is not possible. Am Surg. 2006;72(12):1222–1224 [PubMed] [Google Scholar]
- 8. McLoughlin R, So B, Gray R. Flouroscopically guided percutaneous gastrostomy: current status. Can Assoc Radiol J. 1996;47:10–15 [PubMed] [Google Scholar]
- 9. Ponsky J, Gauderer M. Percutaneous endoscopic gastrostomy: A nonoperative technique for feeding gastrostomy. Gastrointest Endosc. 1981;27:9–11 [DOI] [PubMed] [Google Scholar]
- 10. Barkmeier J, Trerotola S, Weibbke E, et al. Percutaneous radiologic, surgical endoscopic, and percutaneous endoscopic gastrostomy/gastrojejunostomy: comparative study and cost analysis. Cardiovasc Intervent Radiol. 1998;21:324–328 [DOI] [PubMed] [Google Scholar]