Results of this study suggest that patients who have failed therapies for overactive bladder might be more effectively treated using therapies directed towards uroepithelial dysfunction and neural upregulation associated with interstitial cystitis.
Keywords: Overactive bladder, Interstitial cystitis/painful bladder syndrome, Cystoscopy, Hydrodistention, Potassium Sensitivity Test
Abstract
Objective:
We evaluated the prevalence of positive potassium sensitivity and cystoscopy with hydrodistention findings in patients with overactive bladder.
Method:
This was a prospective cohort study of 98 patients who presented with overactive bladder symptoms. The diagnosis of overactive bladder is established by the presence of irritable voiding symptoms. All patients completed a PUF questionnaire and underwent potassium sensitivity testing. Eighty patients underwent urodynamic testing, and 42 patients underwent cystoscopic hydrodistention while under general anesthesia.
Results:
The Potassium Sensitivity Test was positive in 59 (60.2%) of the 98 patients, 37 (56%) of wet overactive bladder patients, and 22 (68.8%) of dry overactive bladder patients. Their mean PUF score was 7. Thirty-three (78.5%) of the patients who underwent cystoscopic hydrodistention had glomerulations consistent with NIH criteria for interstitial cystitis, and 26 of these patients tested positive for potassium sensitivity. Fifty-one (63.8%) of the patients who underwent urodynamics tested positive for potassium sensitivity.
Conclusion:
Many patients with symptoms of overactive bladder with little or no pain have cystoscopic evidence of interstitial cystitis and a positive Potassium Sensitivity Test. Therapies directed toward the uroepithelial dysfunction and neural upregulation associated with interstitial cystitis/painful bladder syndrome may be an important adjunct for patients who have failed or have had a partial response to anticholinergic therapy and behavior modification.
INTRODUCTION
Overactive bladder (OAB) was recently defined by the International Continence Society as “urgency, with or without urge incontinence, usually with frequency and nocturia… if there is no proven infection or other obvious pathology.”1 Furthermore, there is a long list of associated disorders that can cause these symptoms to develop. Therapy that is symptom based is often very effective, but there are times when this management plan can be inadequate.
During the last decade, our knowledge of the neural pathways involved in the control of the lower urinary tract has been greatly expanded. The control of the lower urinary tract is dependent on input from the lower urinary tract and the pelvic floor into the central nervous system (CNS). Control is regulated both within the spinal cord (sacral micturition center) and within supraspinal areas (pons micturition center). Proposed factors involved in the pathophysiology of overactive bladder include neurogenic and/or myogenic causes. Possible factors associated with a neurogenic cause include damage to central neurologic pathways leading to a loss of peripheral inhibition, reduced suprapontine inhibition, injury to axons within the spinal cord, increased lower urinary tract afferent output, and enhancement of excitatory neurotransmission within the micturition reflex pathways. In recent years, our interest in the pathophysiology of overactive bladder has shifted from the detrusor muscle to the afferent innervation of the lower urinary tract. With this shift, we have opened the door to improved understanding of the symptoms of overactive bladder in patients who have a component of their pathology arising from the afferent arm of the lower urinary tract and pelvic floor innervation. This new understanding will provide more options in the management of these complicated patients as well.
Interstitial cystitis (IC), also known as painful bladder syndrome (PBS),2 is a clinical syndrome of urinary urgency, frequency, pelvic pain, or combination of all of these3,4 without an obvious identifiable cause, ie, infection, neoplastic process, and others. Symptom flares are often associated with sexual relations, menstrual cycle, certain types of foods, and stress. Given that the primary symptoms are sensory based–urgency, frequency, and pain–a conclusion can be drawn that these patients' symptoms would arise from anupregulated afferent output from the lower urinary tract. If this is true, then one would expect an overlap between the diagnosis of overactive bladder and the diagnosis of interstitial cystitis in a portion of patients who present with overactive bladder symptoms.
This study examined that potential overlap by using a symptom-based diagnosis of overactive bladder and 2 common tools to diagnose interstitial cystitis/painful bladder syndrome: the potassium sensitivity test (PST) and cystoscopy with hydrodistention. It is our belief that many patients have overactive bladder due to an overactive afferent arm of their micturition reflex and would benefit from therapies directed toward this upregulation. Discussion will follow that further reviews the potential that interstitial cystitis is in fact a visceral pain syndrome that has afferent upregulation as a key component to its pathophysiology.
METHODS
Of the 532 women treated at The Midwest Regional Center for Chronic Pelvic Pain and Bladder Control in Lima, Ohio from October 2000 to October 2002, 98 women (18 to 62 years old) were diagnosed with overactive bladder. These 98 patients did not report pelvic pain as part of their symptoms. Some of the women were initially treated by their family physicians with anticholinergic medication and failed to have satisfactory improvement in symptoms. All 98 patients fit the diagnosis of overactive bladder according to the standard definition of having urinary urgency (sensation of incomplete emptying of the bladder), frequency of at least 8 times in 24 hours, and nocturia, with or without incontinence for more than 6 months in duration.5–8
All 98 patients had laboratory studies carried out including urinalysis, urine cytology, urine culture, and a cervical Ureaplasma culture. All tests came back negative. These patients also had negative abdominal and pelvic examinations that indicated that their lower abdomen, pelvic floor, and bladder were not tender.
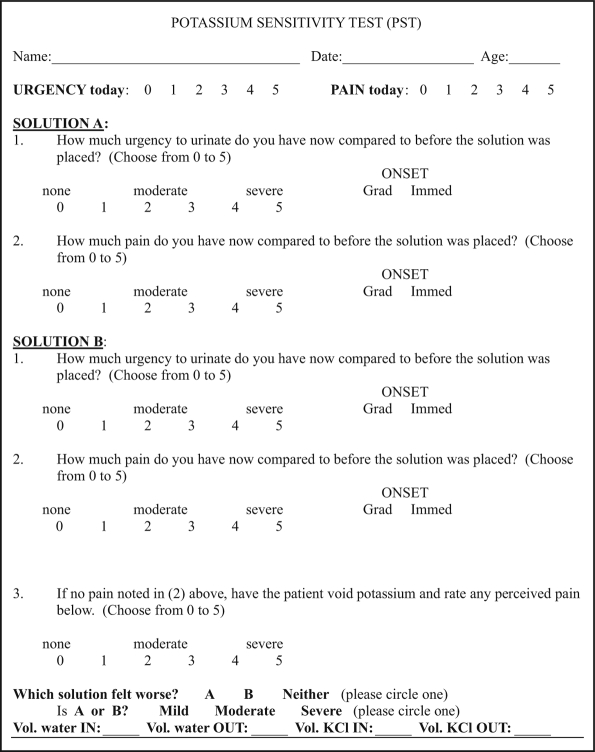
All patients were then tested for potassium sensitivity as described by Parsons.9 In this test, the patient was asked to rate her pain level and sensation of urgency at 3 points: her initial baseline pain level prior to the infusion of 40 mL of sterile water (solution A) into her bladder, after solution A was retained for 3 to 5 minutes, and after solution A was drained and 40 mL of a 400 mEq/L solution of potassium chloride (solution B) was infused into the bladder. The patient was asked to rate her symptom according to the degree of provocation of urgency and pain on a scale of 0, indicating no provocation, to 5, indicating marked provocation (Figure 1). A positive test was defined by a change in score of 2 or more from the baseline.
Figure 1.
Potassium sensitivity test.
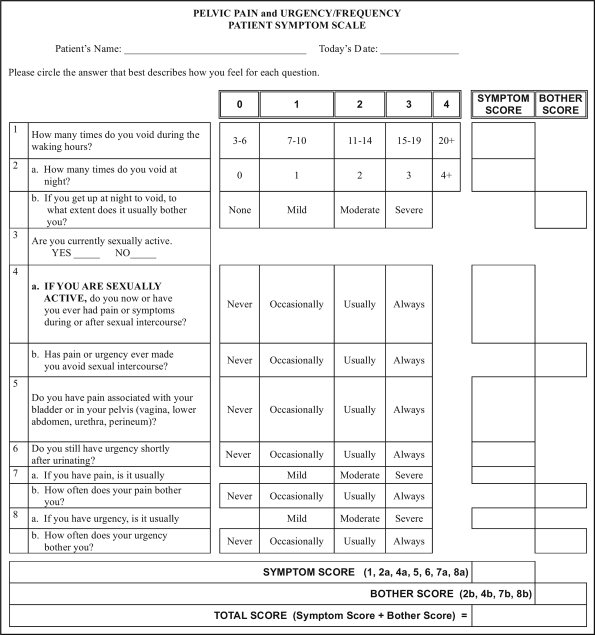
In addition to the PST, all women were given the PUF questionnaire4 (Figure 2).
Figure 2.
Pelvic pain and urgency/frequency patient symptom scale questionnaire.
All patients were offered a urodynamic evaluation. Eighty of the cohort had a urodynamic evaluation, and 42 patients received cystoscopy and hydrodistention of the bladder while under general anesthesia. The patients who underwent cystoscopy and hydrodistention either had severe symptoms or chose not to be on pentosan polysulfate unless an IC diagnosis was made. The bladder hydrodistention was carried out by applying 80 cm to 100 cm of passive hydrostatic pressure using sterile water. The bladder was distended for at least 2 minutes before the water was slowly drained out. The submucosal petechiae hemorrhages, also known as glomerulations, were observed as the bladder was being emptied or during the second fill. An interstitial cystitis diagnosis was made according to the NIH guidelines by noting the presence of 10 glomerulations per quadrant in 3 of the 4 quadrants of the bladder cavity and the presence of terminal hematuria.
The researchers were blind to the findings of the potassium sensitivity test, PUF questionnaire, and cystoscopy and hydrodistention.
RESULTS
There were 532 patients evaluated through the pelvic pain center; 98 women (18.4%) had a diagnosis of overactive bladder (OAB). Of these 98 women, 59 (60.2%) had a positive potassium sensitivity test; 39 (39.8%) had a negative test. The average PUF score was 7 for all of the 98 patients.
Eighteen patients chose not to go through with urodynamic testing due to personal reasons, and 80 patients underwent urodynamic testing. In this group of patients, the average first sensation (1S) was 59 mL, and their average cystometric bladder capacity was 480cc.
Fifty-one (63.75%) women in this group had a positive potassium sensitivity test. The first sensation (1S) for these women who tested positive was 56 mL and their average cystometric bladder capacity was 465 mL.
Only 42 patients underwent cystoscopic hydrodistention. Thirty-three (78.5%) patients were found to have glomerulations consistent with the NIH criteria for interstitial cystitis, and 31 (73.8%) of the 42 women had a positive PST; 26 (61.9%) of the 42 patients had both a positive PST and positive cystoscopic findings; 5 (11.9%) patients had a positive PST but negative cystoscopy. Seven (16.7%) patients had a negative PST yet positive cystoscopic findings. Four of the 42 (9.4%) patients were negative for both PST and cystoscopy. The average first sensation (1S) for the groups with positive potassium sensitivity and cystoscopic finding was 40 mL, and their cystometric bladder capacity was 440 mL. Their average bladder capacity while under general anesthesia was 1000 mL. These 42 patients had a mean PUF score of 8.
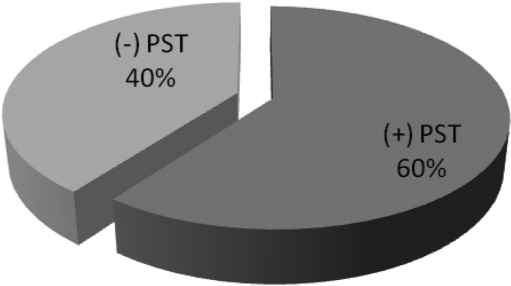
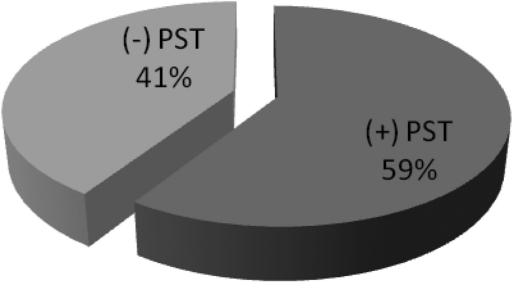
Of the 98 patients with OAB, 66 (67.3%) had urinary incontinence, and 37 (56%) of these patients had a positive potassium sensitivity test (Figure 3). The breakdown of this urinary incontinence group included 17 patients (17.35%) exhibiting true detrusor instability and 49 (50%) patients with stress incontinence in addition to urgency, frequency, and nocturia.
Figure 3.
Potassium sensitivity test results for overactive bladder patients (n = 98).
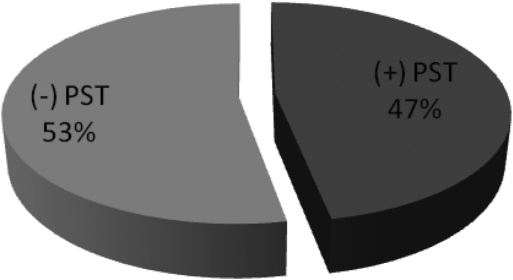
In the group of 17 OAB patients (17.35%) who presented with true detrusor instability (Figure 4), only 8 patients (47%) tested positive for potassium sensitivity, and 7 women (41.2%) had a positive cystoscopic finding for interstitial cystitis.
Figure 4.
Potassium sensitivity test results for overactive bladder patients with detrusor instability (n = 17).
Of the 49 women (50%) with OAB and stress urinary incontinence (Figure 5), 29 women (59%) had a positive potassium sensitivity test.
Figure 5.
Potassium sensitivity test results for wet overactive bladder patients with urinary urgency, urinary frequency, nocturia, and stress urinary incontinence (n = 49).
Thirty-two (32.65%) of the 98 OAB patients had only urinary urgency, frequency, and nocturia (Figure 6). Twenty-two (68.75%) patients in this group had a positive potassium sensitivity test. (Table 1).
Figure 6.
Potassium sensitivity test results for dry overactive bladder patients with urinary urgency, urinary frequency, and nocturia (n = 32).
Table 1.
Potassium Sensitivity Test Results for Overactive Bladder Patients
| All Patients | Urinary Incontinence Patients | CH* | |||||
|---|---|---|---|---|---|---|---|
| (n=98) | UU/UF/N* (n=32) | UU/UF/N + SUI* (n=49) | DI* (n=17) | (+) CH (n=33) | (−) CH (n=9) | ||
| (+) PST* | 59 | 22 | 29 | 9 | 26 | 5 | |
| (−) PST | 39 | 10 | 20 | 8 | 7 | 4 | |
PST = potassium sensitivity test; UU = urinary urgency; UF = urinary frequency; N = nocturia; SUI = stress urinary incontinence; DI = detrusor instability; CH = cystoscopic hydrodistention
DISCUSSION
Overactive bladder is a highly prevalent disorder that impacts millions of people worldwide. Despite the advancements in therapeutic options that we can now offer, the majority of patients with overactive bladder have some persistent symptoms even though their quality of life might in fact be improved and their urgency, frequency, and incontinence reduced. Although a symptom-based diagnosis lends itself to a higher number of patients receiving care as a result of a simplified treatment algorithm, it must be realized that not all patients will respond to this initial management. When this occurs, the clinician must recognize that other causes need to be considered, and these will lead to new treatment options.
At this time, we are unable to predict by history alone, but as clinicians we must remember that symptoms of OAB and IC/PBS are the result of various triggers, and the main clinical difference is generally the presence or absence of pain. But the symptoms are the final expression of various and overlapping pathologies at the urothelium, bladder wall, pelvic floor, and central processing. Management is presently based on a symptom-based diagnosis, but especially in patients with less than adequate response to therapy, we must consider other pathologies. The PST may identify a subgroup of patients with urothelial dysfunction and/or C-fiber upregulation that may benefit by targeting these pathologies rather than the muscarinic receptor alone (ie, anticholinergic drugs).
The debate as to how to diagnose interstitial cystitis continues to grow and like overactive bladder, interstitial cystitis/painful bladder syndrome is increasingly thought to be a clinical syndrome that can easily be diagnosed.10 Additionally, it is increasingly being diagnosed in many patients who suffer from common pain disorders, eg, vulvodynia, chronic pelvic pain, endometriosis, fibromyalgia, and functional bowel disease.11,12 Many causes of interstitial cystitis have been proposed, including infection, neurogenic, autoimmune, GAG layer dysfunction, and mast cell abnormalities, but these changes may be a reflection of end-organ effect and not the primary pathology. The end result of all of these potential etiologies is an upregulation of sensory output from the bladder and/ordysregulation of sensory processing arising from the sacral cord. These changes are the hallmark of any visceral pain syndrome. Many of these patients can progress to develop global hypersensitivity and show abnormal signal processing in the suprasacral areas, eg, limbic system, insular and thalamus.
Current theories of the pathophysiology of interstitial cystitis are predominantly conjecture, but increasingly authors are describing IC as simply a form of a visceral pain syndrome.13 Visceral pain syndromes involve chronic neurogenic inflammation, primary afferent overactivity, and central nervous system sensitization that all interact to perpetuate pain.14 The bladder is an ideal organ to induce this dysregulation of dorsal horn activity because it has the highest neural density of any pelvic organ.15 The majority of the afferent nerves arising from the bladder are silent, but with prolonged stimulation (and this can occur with many types of insults), these silent C-fibers can become active.16 This new barrage of nociceptive or painful input onto the dorsal horn initiates a series of biochemical changes that can become permanent (often referred to as central sensitization), depending on the duration and severity of the input. These changes result in a decrease in the threshold (the amount of stimulus needed to be perceived as painful) within the dorsal horn.17 This alteration in sensory processing results in a phenomenon known as allodynia. This is exemplified in patients whose bladders feel painfully full and urgent at a volume of only 3oz. These changes are collectively referred to as spinal cord windup and are an example of abnormal neuronal plasticity.18,19
As noted above, bladder C-fibers are typically silent and are activated not by volume, but by cold and/or chemical irritation.20 This physiologic characteristic is the key to understanding the importance of the potassium sensitivity test. The C-fibers are located within the uroepithelium and submucosa of the bladder. If the protective effects of the glycosaminoglycan (GAG) layer are somehow deficient, the potasium ions will depolarize and/or activate the C-fibers; thus, a positive PST will be demonstrated. A positive PST can therefore occur from increased permeability of the urothelium, from an increase in activated C-fibers, or from a combination of both. The etiology of OAB is diverse and involves release of acetylcholine from nerve fibers and bladder urothelium, as well as the release of ATP. Both these events occur as a result of bladder wall stretch, inflammation, and pH changes. Spontaneous myogenic activity and neuroplasticity often occur as well.21 ATP release from the urothelium is upregulated in various clinical situations including where patients are >65 years of age and where OAB is present and in feline interstitial cystitis.22 PZX3 receptors (1 of the 7 subtypes of ATP receptors) are involved in this reaction and are also involved in both nociceptive and non-nociceptive afferent pathways. The fact that the urothelium has been found to have sensory function and is involved in normal and abnormal sensory processing is the key to understanding that there is symptomatic as well as neuropathologic overlap in patients with OAB and IC.
We have shown that 60% of patients with overactive bladder symptoms have evidence of a positive PST. This suggests that these patients have a deficiency in the GAG layer and/or an increase in activated C-fibers. Additionally, many authors9,23–25 have shown that a positive PST correlates with a diagnosis of interstitial cystitis In the patients with an overactive bladder who also underwent cystoscopy with hydrodistention, we found that 73.8% have cystoscopic evidence compatible with interstitial cystitis, and 61.9% of these same patients have both a positive PST and cystoscopic findings compatible with interstitial cystitis. These data emphasize that patients with overactive bladder often have pathology that would best be managed with therapy directed towards the interstitial cystitis/painful bladder syndrome component (afferent upregulation and urothelial dysfunction) rather than using only muscarinic blockade, ie, anticholinergic therapies.
By categorizing the OAB patients by their symptoms, we found that 56% of the patients with urinary incontinence or wet overactive bladder had a positive PST, while 68.75% of the dry OAB patients exhibiting only urinary urgency, frequency, and nocturia had a positive PST. The higher incidence of positive PST in patients with dry overactive bladder suggests that interstitial cystitis/painful bladder syndrome could be a contributing factor in the symptoms of these patients. Clinical research has shown that the use of anticholinergic drugs for the treatment of overactive bladder symptoms reduces urinary urgency by about 60%, reduces micturition frequency by about 25%, and reduces urinary incontinence by about 80%.26–28 These data support the notion that dry OAB patients have symptoms that would be better managed with therapy directed towards interstitial cystitis/painful bladder syndrome. It has recently been demonstrated in a randomized 2-year study of 82 patients with OAB that 0.2% chondroitin sulfate installation provided much better response than Tolterodine provided (73% vs 43% at 12 months and 56% vs 14% after 24 months) after 12 months of therapy.29 The prolonged benefit of this glycosaminoglycan supplement demonstrates the importance of correcting urothelial dysfunction in patients who have a poor response to anticholinergics alone. Whether the label applied to a particular patient is IC/PBS or remains OAB is controversial but our inability to establish an appropriate label should not limit the therapies we offer.
CONCLUSION
Many patients with symptoms of overactive bladder were found to have cystoscopic findings of interstitial cystitis/ painful bladder syndrome and a positive PST. Given the multiple pathophysiologic causes of overactive bladder, it should not surprise us that some patients have evidence of C-fiber upregulation (positive PST). These findings encourage us to realize that patients who have failed traditional therapies for overactive bladder might be more effectively treated using therapies directed towards the uroepithelial dysfunction30 and neural upregulation associated with interstitial cystitis.31
Contributor Information
Maurice K. Chung, Midwest Regional Center for Chronic Pelvic Pain, Lima, Ohio, USA..
Charles W. Butrick, Kansas City, Missouri, USA..
Cherie W. Chung, Midwest Regional Center for Chronic Pelvic Pain, Lima, Ohio, USA.
References:
- 1. Abrams P, Cardozo L, Fall M, et al. The standardization of terminology of lower urinary tract function: report from the Standardization Subcommittee of the International Continence Society. Neurourol Urodyn. 2002;21:167. [DOI] [PubMed] [Google Scholar]
- 2.Association of Reproductive Health Professionals. Interstitial Cystitis Association. Outcome of the Washington, DC consensus meeting on interstitial cystitis/painful bladder syndrome: a multidisciplinary meeting of researchers, clinicians, and patients; Washington, DC. February 10, 2007. Consensus Group on IC/PBS. [Google Scholar]
- 3. Jones CA, Nyber L. Epidemiology of interstitial cystitis. Urology. 1997;49(5a):2–9 [DOI] [PubMed] [Google Scholar]
- 4. Parsons CL, Dell J, Stanford E, et al. Increased prevalence of interstitial cystitis: previously unrecognized urologic and gynecologic cases identified using a new symptom questionnaire and intravesical potassium sensitivity. Urology. 2002;60:573–578 [DOI] [PubMed] [Google Scholar]
- 5. Abrams P, Wein AJ. Correspondence Urology. 1998;51:1062 [Google Scholar]
- 6. Nishizawa O. Discussion: assessment of symptoms in patients with an overactive bladder. Urology. 1997;50(suppl 6A):23 [Google Scholar]
- 7. Abrams P, Wein AJ. The Overactive Bladder: A Widespread and Treatable Condition. Stockholm, Sweden: Erik Sparre Medical AB; 1998 [Google Scholar]
- 8. Clinical Practice Guidelines: Urinary Incontinence in Adults. 1996. AHCPR publication; 96–0682 [Google Scholar]
- 9. Parsons CL, Zupkas P, Parsons JK. Intravesical potassium sensitivity in patients with interstitial cystitis and urethral syndrome. Urology. 57:428–432, 2001; discussion 432-433 [DOI] [PubMed] [Google Scholar]
- 10. Wein AJ, Rovner ES. The overactive bladder: an overview for primary care health providers. Int J Fertil. 1999;44(2):56–66 [PubMed] [Google Scholar]
- 11. Parsons CL, Bullen M, Kahn BS, et al. A gynecologic presentation of interstitial cystitis as detected by intravesical potassium sensitivity. Obstet Gynecol. 2001;98:127–132 [DOI] [PubMed] [Google Scholar]
- 12. Koziol JA. Epidemiology of interstitial cystitis. Urol Clin North Am. 1994;21(1):7–20 [PubMed] [Google Scholar]
- 13. Rosamilia A, Dwyera PL. Pathophysiology of interstitial cystitis. Curr Opin Obstet Gynecol. 2000;12:405–410 [DOI] [PubMed] [Google Scholar]
- 14. Wesselmann U. Interstitial cystitis as a visceral pain syndrome. Urology. 2001;51(suppl 6):102. [DOI] [PubMed] [Google Scholar]
- 15. Cervero F. Sensory innervation of the viscera: peripheral basis of visceral pain. Physiol Rev. 1994;74:95–138 [DOI] [PubMed] [Google Scholar]
- 16. Mayer EA. Clinical implications of visceral hyperalgesia. Contemp Intern Med. 1994;46:42–54 [PubMed] [Google Scholar]
- 17. Markenson J. Mechanisms of chronic pain. Am J Med. 1996;101(suppl 1a):6s–18s [DOI] [PubMed] [Google Scholar]
- 18. Coderre P, Katz J, Vaccarino A, Melzack R. Contribution of central neuroplasticity to pathologic pain: review of clinical and experimental medicine. Pain. 1993;52:259–285 [DOI] [PubMed] [Google Scholar]
- 19. Woolf CJ. Evidence for a central component of post heightened injury pain hypersensitivity. Nature. 1983;306:686. [DOI] [PubMed] [Google Scholar]
- 20. de Groat WC, Downie JW, Levin RM, et al. Basic neurophysiology and neuropharmacology In: Abrams P, Khoury S, eds. Incontinence: First International Consultation on Incontinence. Plymouth, United Kingdom: Health Publications; 1999 [Google Scholar]
- 21. Steers WD. Pathophysiology of overactive bladder and urge urinary incontinence. Rev Urol. 2002;4(suppl 4):S7–S18 [PMC free article] [PubMed] [Google Scholar]
- 22. de Groat WC. The urothelium in overactive bladder: passive bystander or active participant? Urology. 2004;64(suppl1):7–11 [DOI] [PubMed] [Google Scholar]
- 23. Abrams P, Khoury S, Wein A, et al., eds. Incontinence: First International Consultation on Incontinence. Plymouth, United Kingdom: Plymbridge Distributors Ltd. 1999;105–154 [Google Scholar]
- 24. Chambers GK, Fenster HN, Cripps S, et al. An Assessment of the Use of Intravesical Potassium in the Diagnosis of Interstitial Cystitis. J Urol. 1999;162:699–701 [DOI] [PubMed] [Google Scholar]
- 25. Parsons CL, Forrest J, Nickel JC, et al. Effect of Pentosan Polysulfate Therapy on Intravesical Potassium Sensitivity. Urology. 2002;59:329–333 [DOI] [PubMed] [Google Scholar]
- 26. Pelman RS, Capo JP, Forero-Schwanhaeuser S. Solifenacin at 3 years: a review of efficacy and safety. Postgrad Med. 2008;120(2):86–92 [DOI] [PubMed] [Google Scholar]
- 27. Van Kerrebroeck P, Kreder K, Jonas U, et al. Tolterodine once-daily: superior efficacy and tolerability in the treatment of the overactive bladder. Urology. 2001;57:414–421 [DOI] [PubMed] [Google Scholar]
- 28. Nitti VW, Dmochowski R, Sand PS, et al. Efficacy, safety and tolerability of Fesoterodine for overactive bladder syndrome. J Urol. 2007;178(6):2488–2494 [DOI] [PubMed] [Google Scholar]
- 29. Gauruder-Burmester A, Popken G. Follow-up at 24 months after treatment of overactive bladder with 0.2% sodium chrondroitin sulfate. Aktuelle Urol. 2009;40(6)355–359 [DOI] [PubMed] [Google Scholar]
- 30. Chiang G, Patra P, Letourneau R, et al. Pentosanpolysulfate inhibits mast cell histamine secretion and intracellular calcium ion levels: an alternative explanation of its beneficial effect in interstitial cystitis. J Urol. 2000;164:2119–2125 [PubMed] [Google Scholar]
- 31. Yoshimura N, Satoshi S, Chancellor MB, de Groat WC. Targeting afferent hyperexcitability for therapy of the painful bladder syndrome. Urology. 2002;59(suppl 5A):61–67 [DOI] [PubMed] [Google Scholar]