A single port access technique is described to accomplish laparoscopic splenectomy.
Keywords: Laparoscopy, Splenectomy, Single port access surgery, SPA surgery, LESS
Abstract
Introduction:
Over the last decade, laparoscopic splenectomy has become the standard of care for spleen removal. Elimination of a large incision and difficult exposure has decreased postoperative morbidity and length of stay. Single port access (SPA) surgery was developed as an alternative to traditional multiport laparoscopy, potentially exploiting the already proven benefits of minimally invasive surgery. We apply the SPA technique to splenectomy via a single umbilical incision.
Methods:
SPA splenectomy was performed in a 36-year-old male for staging. The single-port access technique was used to gain abdominal entry. Exposure, dissection, and removal were performed via a single incision within the umbilicus. The final incision was extended for removal of a complete specimen for pathologic evaluation.
Results:
Splenic mobilization and control of the short gastrics was successfully performed via a single umbilical incision. The final incision was extended inferiorly for en bloc organ removal. Follow-up at 18 months revealed a well-healed incision with no signs of hernia formation.
Conclusions:
The single-port access technique has been successfully applied to splenectomy as an available alternative to multiport laparoscopic splenectomy. Use of standard instrumentation and trocars maintains costs and familiarity of the procedure. Exposure, visualization, and dissection are the same as in standard laparoscopy. SPA surgery may be more ergonomically pleasing to the surgeon and offer patient benefits, such as faster recovery and decreased adhesion formation in the long term.
INTRODUCTION
Since Georg Kelling's first laparoscopic procedure on dogs (1902) and Hans Christian Jacobaeus' first report of a laparoscopic operation in humans (1910), laparoscopic procedures have been refined and popularized to become a safe and effective surgical approach. Laparoscopic splenectomy was first introduced at Royal Brisbane Hospital in 1991. It was originally performed using a 5-trocar technique.1 Today, laparoscopic resection has become the standard of care for routine splenectomy.2,3 As with other laparoscopic procedures, laparoscopic splenectomy offers many advantages compared with the open procedure. Less blood loss and a shorter hospital course have been reported.4 Bowel function returns more quickly when the splenectomy is performed laparoscopically.5,6 There is also decreased narcotic requirement for postoperative pain control.7,8 These advantages lead to significantly fewer hospital days (range, 1 to 2) compared with an open procedure (range, 6 to 20).9 After being discharged from hospitals, patients are also able to resume their daily activities within 2 weeks.10
Compared with conventional multiple-port laparoscopic procedures, we have developed a unique single port access (SPA) surgical technique as the next step in minimal access surgery. SPA surgery allows us to place several trocars through a single portal of entry within the umbilicus. Without a need for a unique or additional access device, we combine this approach with the established basic principles and dissection techniques of current laparoscopic surgery being utilized by surgeons with a novel access technique. By positioning the port of entry into the umbilicus, the scar is easily concealed. We report successful resection for staging using this access technique.
METHODS
A 36-year-old African American male underwent splenectomy for staging of lymphoma. The standard SPA technique was used for abdominal entry. A 12-mm incision was made at the umbilicus. Blunt dissection was performed until fascia was exposed. A 5-mm clear trocar was passed through the fascia, and the abdominal cavity was insufflated with carbon dioxide to a standard pressure of 15mm. A 5-mm laparoscope was introduced. The abdominal cavity was explored. Skin and soft tissue flaps were raised in both directions lateral to the midline trocar (Figure 1). Two accessory trocars were then inserted superior and lateral to the initial trocar. Each trocar was introduced through separate fascial locations within the single umbilical incision (Figure 2a, b). Using a 30° scope through the clear central trocar, we are able to observe the second and third trocar entering the abdominal cavity safely. Once access was obtained, the intraabdominal procedure was virtually the same as multiport laparoscopy (Figure 3). First, the splenocolic ligament was taken down with a Harmonic scalpel. The patient was then placed in a reverse Trendelenburg position with the right side down to promote better visualization. Next, the posterior attachment to the diaphragm was released, and the short gastrics were transected. The inferior attachments of the spleen were freed by using a Harmonic scalpel and LigaSure. A 5mm trocar was then upsized to a 12mm trocar to accomodate the stapler. The splenic artery and vein were divided by using a stapling device. The stapling device was fired several times across the splenic hilum (Figure 4). At this point, the spleen was mobilized completely and retracted inferiorly. The left upper quadrant was irrigated and inspected for adequate hemostasis. The patient was placed in a flat position. The spleen was placed in an endocatch bag, and the umbilical incision was extended inferiorly to allow for extraction of the spleen. The trocars were removed, the abdomen desufflated, the fascia was re-approximated, and the skin was closed (Figure 5).
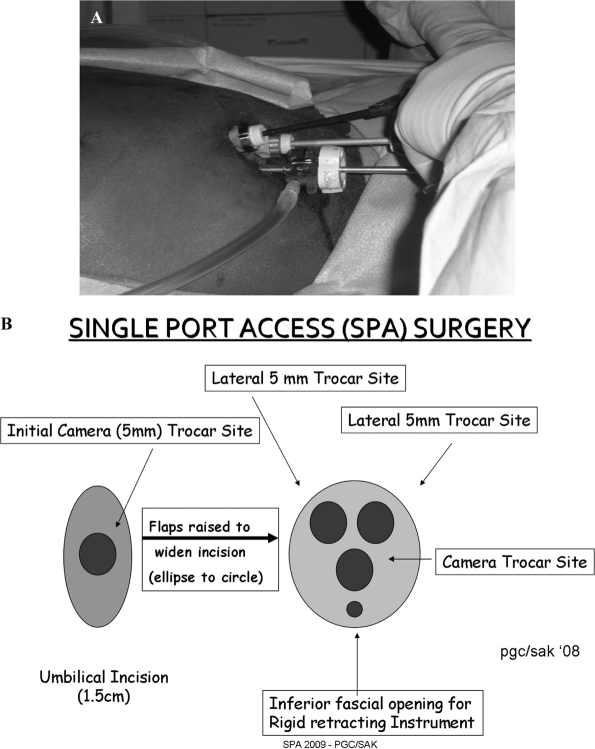
Figure 1.
Initial incision with skin flaps.
Figure 2.
a. External photo of SPA set up. Figure 2b. Schematic of SPA.
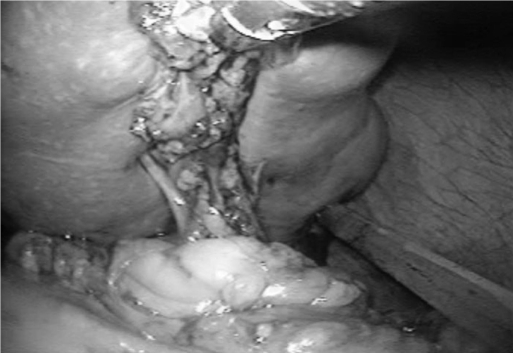
Figure 3.
Internal photo of lateral mobilization.
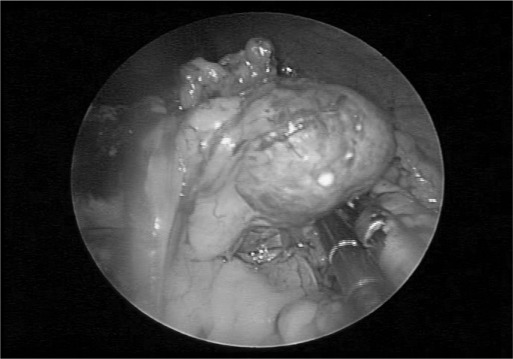
Figure 4.
Internal photo of splenic hilum.
Figure 5.
Final incision.
RESULTS
Successful splenic resection was performed via a single umbilical incision. Operative time was 3 hours with minimal blood loss. The patient was ambulatory on postoperative day one, advanced to a regular diet, and discharged home on postoperative day 3. Follow-up at 18 months revealed a well-healed umbilical incision. No complications of wound infection or hernia formation occurred.
DISCUSSION
Historically, splenectomy was indicated for staging of Hodgkin's lymphoma. As the field of oncology expanded and diagnostic testing improved, the need for surgical staging diminished. Patients could be adequately staged without undergoing major abdominal surgery. With the advances in minimally invasive surgery, splenectomy became a safer surgery with faster recovery. Although splenectomy is not currently recommended for all patients with Hodgkin's lymphoma, it can be an effective staging tool. In a review of 825 staging laparotomies,11 the clinical stage was changed as a result of laparotomy in 43.2% of cases. Staging laparotomy with splenectomy has proven to be a useful and safe clinical research tool and has been one of the major factors in increasing survival from Hodgkin's disease.11 Our patient is a 36-year-old male without comorbidities. He completed a course of chemotherapy and was clinically cancer free. This final staging splenectomy was performed to confirm that further treatment was unnecessary.
Laparoscopy is the current standard of care for splenectomy. Multiple trocars are inserted into the abdominal cavity; the spleen is dissected and then extracted after an incision is made. This technique has been proven to be superior compared with the open method. Less blood loss and a shorter hospital course have been reported.4 Bowel function returns more quickly when the splenectomy is performed laparoscopically.5,6 There is also decreased narcotic requirement for postoperative pain control.7,8 These advantages lead to significantly fewer hospital days (range, 1 to 2) compared with days required after the open procedure (range, 6 to 20).9 After being discharged from the hospital, patients are also able to resume their daily activities within 2 weeks.10
The single port access (SPA) technique may offer further improvements to the principles of minimally invasive surgery. This minimal access technique incorporates current laparoscopic equipment and positioning with a novel access technique, resulting in a well-hidden scar.
The initial development of the SPA technique was first reported in 2006.12 We began to gradually reduce and reposition trocars during laparoscopic cholecystectomy, beginning with repositioning the subxiphoid trocar into the umbilicus, alongside the optical trocar. Eventually, all trocars were placed within a single incision in the umbilicus.13 Next, we began to use this access technique for other procedures, realizing that the freedom of movement allowed access to multiple quadrants of the abdomen. The SPA technique has been applied to various general surgery, gynecology, and urology procedures, at times during the same operation without changing the access.14,15,16 Decreased portals of entry resulting in one incision may offer potential benefits associated with decreased scar formation. Short-term benefits may further exploit those of multiport laparoscopy, including decreased postoperative pain, quicker recovery of bowel function, shorter length of stay and return to activities of daily life. Long-term benefits of reduced scarring may also be seen. All of these potential benefits will need long-term evaluation of large case series. Additionally, prospective randomized comparisons to standard multiport techniques are necessary to prove advantages, if any.
CONCLUSION
The goal of single port access (SPA) surgery is to minimize the incision required to perform the procedure while maintaining the surgeon's comfort. This may result in less scar formation, less postoperative discomfort, and quicker return to daily activities. This procedure also reduces the cost and degree of single-access laparoscopic training through the use of familiar equipment and setup. SPA surgery can be applied to many different procedures. We present the SPA surgical technique applied to splenectomy, demonstrating an acceptable outcome while providing an alternative access with an enhanced cosmetic result.
Contributor Information
Steven J. Rottman, Drexel University College of Medicine, Department of Surgery, Philadelphia, Pennsylvania..
Erica R. Podolsky, Drexel University College of Medicine, Department of Surgery, Philadelphia, Pennsylvania..
Eugene Kim, Drexel University College of Medicine, Department of Surgery, Philadelphia, Pennsylvania..
Joseph Kern, Drexel University College of Medicine, Department of Surgery, Philadelphia, Pennsylvania..
Paul G Curcillo, II, Drexel University College of Medicine, Department of Surgery, Philadelphia, Pennsylvania..
References:
- 1. Rhodes M, Rudd M, O'Rourke N, Nathanson L, Fielding G. Laparoscopic splenectomy and lymph node biopsy for hematologic disorders. Ann Surg. 1995;43–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Friedman RL, Fallas MJ, Carroll BJ, et al. Laparoscopic splenectomy for idiopathic thrombocytopenia purpura. The gold standard. Surg Endosc. 1996;10:991–995 [DOI] [PubMed] [Google Scholar]
- 3. Leibowitz AB, Adamsky C, Gabrilove J, Labow DM. Intraoperative acute tumor lysis syndrome during laproscopic splenectomy preceded by splenic artery embolization. Surg Laparosc Endosc Percutan Tech. 2007;17(3):210–211 [DOI] [PubMed] [Google Scholar]
- 4. Smith L, Luna G, Merg AR, McNevin MA, Moore MR, Bax TW. Laparoscopic splenectomy for treatment of splenomegaly. Am J Surg. 2004;187(5):618–620 [DOI] [PubMed] [Google Scholar]
- 5. Cadiere GB, Verroken R, Himpens J, Bruyns J, Efira M, De Wit S. Operative strategy in laparoscopic splenectomy. J Am Coll Surg. 1994;179:668–672 [PubMed] [Google Scholar]
- 6. Watson DI, Coventry BJ, Chin T, Gill PG, Malycha P. Laparoscopic versus open splenectomy for immune thrombocytopenic purpura. Surgery. 1997;121:18–22 [DOI] [PubMed] [Google Scholar]
- 7. Silvestri F, Russo D, Fanin R, et al. Laparoscopic splenectomy in the management of hematological diseases. Haematologica. 1995;80:47–49 [PubMed] [Google Scholar]
- 8. Tsiotos GG, Schlinkert RT. Laparoscopic splenectomy for immune thrombocytopenic purpura. Arch Surg. 1997;132:642–646 [DOI] [PubMed] [Google Scholar]
- 9. Flowers JL, Lefor AT, Steers J, Heyman M, Graham SM, Imbembo AL. Laparoscopic splenectomy in patients with hematologic diseases. Ann Surg. 1996;224:19–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gigot JF, de Ville de Goyet J, Van Beers BE, et al. Laparoscopic splenectomy in adults and children: experience with 31 patients. Surgery. 1996;119:384–389 [DOI] [PubMed] [Google Scholar]
- 11. Taylor MA, Kaplan HS, Nelsen TS. Staging laparotomy with splenectomy for Hodgkin's disease: The Stanford experience. World J Surg. 1985;9:449–460 [DOI] [PubMed] [Google Scholar]
- 12. Podolsky ER, Rottman SJ, Poblete H, King SA, Curcillo PG. Single Port Access (SPA™) cholecystectomy: a completely transumbilical approach. J Laparoendosc Adv Surg Tech. 2009. April;19(2)219–222 [DOI] [PubMed] [Google Scholar]
- 13. Curcillo PG, King SA, Podolsky ER, Rottman SJ. Single Port Access (SPA™), Minimal Access Surgery Through a Single Incision Surgical Technology International, 2009;18:19–25 [PubMed] [Google Scholar]
- 14. Podolsky ER, Curcillo PG. Single Port Access (SPA) Surgery of the Alimentary Tract: 18 Months Experience with a Single Umbilical Approachç Gasteroenterology, Volume 136, Issue 5, Pages A-869, May 2009 [Google Scholar]
- 15. King SA, Atogho A, Podolsky ER, Curcillo PG. Single Port Access (SPA) Bilateral Oopherectomy and Hysterectomy. Laparoscopy Today, The Green Issue, 7;2,26–16. [Google Scholar]
- 16. Castellucci SA, Curcillo PG, Ginsberg PC, Saba S, Jaffe J, Harmon JD: Single Port Access Adrenalectomy. Journal of Endourology August 2008, 22:8;1573–1576 [DOI] [PubMed] [Google Scholar]