Abstract
Objective:
With increasing technology and computerized systems in the OR, the physician's responsibility is growing. For intraoperative evaluation of insufflation techniques, a data acquisition model for quality control study of potential insufflation problems is necessary.
Methods:
A computer-based, online data acquisition model was designed with a Pentium notebook, PCMCIA data acquisition board PCI-460-P1 and a Visual Designer 3.0 measurement program (both Intelligent Instrumentation, Inc., Tucson, AZ), temperature meters Therm 2280-1 and 2283-2 (Ahlborn, Holzkirchen, Germany) and temperature probes 401 AC and 402 AC (YSI, Inc., Yellow Springs, OH) and T-430-2R (Ahlborn, Holzkirchen, Germany). Gas flow was measured with laminar flow element LFE 1 and flow meters Digima premo 720 (both Special Instruments, Noerdlingen, Germany). During 73 standard laparoscopic procedures, gas flow (L/min) in the insufflation hose, pressure (mm Hg) in the hose and abdomen as well as temperature (°C) in the hose, abdomen and rectum were measured continuously at 3 Hz rate.
Results:
Actual values measured show a wide range often not identical with insufflator presetting. Pressure in the abdomen is usually less than hose pressure. Intraabdominal pressure peaks (≤50 mm Hg) occurred during insufficient anesthesia, while leaning on the abdomen, during trocar insertion and other manipulation. Blood irrigation fluids found in the hose (n=3/73) can lead to bacterial contamination. Negative pressure (−50 mm Hg) was measured due to Endobag removal. Negative flow (≤15 L/min) was caused by pressure on the abdomen, insufflator regulation and an empty CO2 gas tank. Gas temperature in the hose equals room temperature but can decrease in the abdomen to 27.7°C due to high gas flow, large amounts of gas used and prolonged insufflation. Further insufflation-related problems were documented.
Conclusions:
This computer-based measurement model proved to be useful for quality control study in the OR. Results demonstrate the need for intraoperative evaluation of insufflation techniques for laparoscopy. Although no obvious complication related to insufflation problems occurred, some findings potentially question patient security.
Keywords: Laparoscopy, Insufflation technique, Data acquisition, Quality control
INTRODUCTION
A physician feels responsible for proper and secure function of all equipment that is used on or around the patient. With increasing technology and computerized systems in the OR, the surgeon's responsibility is growing. One example is laparoscopy — a growing surgical technique in which many different robotics, technical and computerized devices are and will continue to be used.
Many articles have been published about laparoscopic procedures themselves within the last decade, but little is known about insufflation technique. No objective data regarding physical properties, the intraoperative function and the interaction between patient and the insufflation technique has been published; neither have any comprehensive models for its evaluation. The physician's general knowledge about basic physics is often not enough to solve technical insufflation problems immediately. As surgeons, we rely and depend on manufacturers and their promises about product properties. A comprehensive, experimental laboratory study about insufflation properties of a variety of insufflation components has shown remarkable differences in flow and resistance values.1 From this background rises the question: How can the surgeon verify proper and secure function of the insufflation technique?
We carried out an independent intraoperative study for quality control to verify and compare function parameters such as pressure, gas flow and temperature of the standard insufflation equipment used in pelviscopy and laparoscopy and to better understand the physical background in which laparoscopy is performed. A computer-based data acquisition model was developed with which different physical parameters can be measured, documented and graphically displayed online.
METHODS
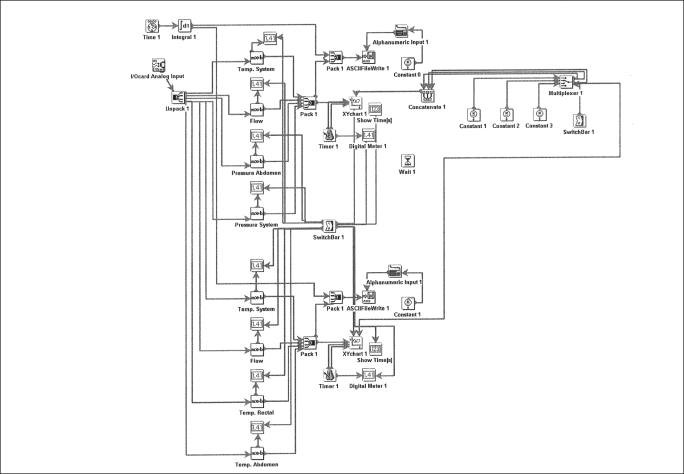
A Pentium notebook PC (Tecra 510 CDT; Toshiba, Inc., Irvine, CA) and a PCMCIA data acquisition board (PCI-460-P1; Intelligent Instrumentation, Inc., Tucson, AZ) were connected with different electronic meters for pressure (Digima premo 720; Special Instruments, Noerdlingen, Germany) and temperature (Therm 2280-1 for K probes (NiCr-Ni) and Therm 2283-2 for NTC probes; Ahlborn, Holzkirchen, Germany). Different temperature probes were used: NTC-probes 401 AC for intra-abdominal temperature and 402 AC for rectal temperature (YSI, Inc., Yellow Springs, OH); and K probe T-430-2R for insufflation hose temperature (Ahlborn, Holzkirchen, Germany). Gas flow was measured with a laminar flow element (LFE 1; Special Instruments, Noerdlingen, Germany). Measurement accuracy was +/−0.1%. The measurement scheme was graphically created with an adjustable, multiple-purpose measurement program (Visual Designer 3.0; Intelligent Instrumentation, Inc., Tucson, AZ; Figure 1) and transferred into the final program. Results were displayed with a scientific graphic program (Origin 4.1; Microcal, Inc., Northampton, MA). Costs for this entire model were approximately US$ 12,000.
Figure 1.
Visual Designer measurement diagram.
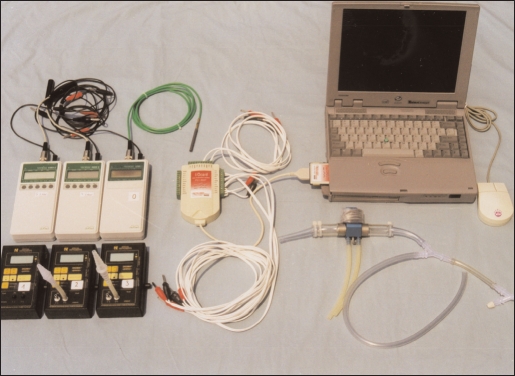
Before the operation, the equipment (Figure 2) was connected (as shown in Figure 3), and the rectal temperature probe was introduced. The measurement program was started and an intra-abdominal temperature probe and pressure trocar were inserted. Over the entire time of the procedure, parameters (gas flow in the hose; pressure in the hose and abdomen; and temperature in the hose, abdomen and rectum) were measured at 3 Hz rate. The values were converted and stored on a hard drive as ASCII files. A supervisor took additional information intraoperatively so problems would be easier to identify later on (Figure 4).
Figure 2.
Computer model with all measurement devices. Left bottom: Digima premo pressure meters; left top: Therm meters; middle: PC card and data acquisition board; right bottom: Laminar Flow Element; right top: Toshiba notebook.
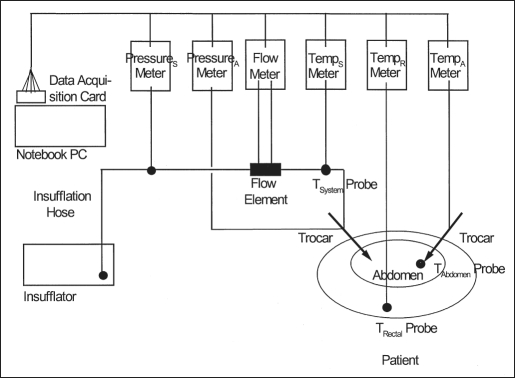
Figure 3.
Measurement scheme.
Figure 4.
OR setting at FMC with supervisor and PC- / equipment table in front, patient on OR table in the background.
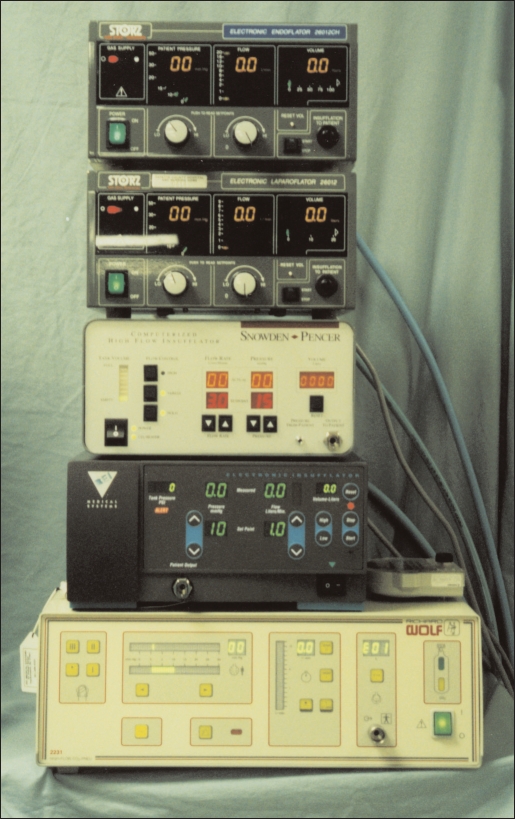
This computer model was used to evaluate different insufflators: the Karl Storz Endoflator 26012CH (flowmax 20 L/min), Karl Storz Laparoflator 26012C (10 L/min), Snowden & Pencer 89-8600 (15 L/min), BEI Medical 92000V (20 L/min) and Richard Wolf 2231 (15 L/min) (Figure 5).
Figure 5.
Insufflators evaluated (top to bottom): 1. Storz Endoflator, 2. Storz Laparoflator, 3. Snowden & Pencer, 4. BEI Medical, 5. Wolf.
All intraoperative measurements were performed at the Department of Surgery at Fayette Medical Center (FMC), Fayette, Alabama, USA. Although nothing was changed from standard laparoscopy for this experimental study, all patients underwent a comprehensive informed consent protocol, and their written consent was mandatory. Institutional review board approval from FMC was obtained.
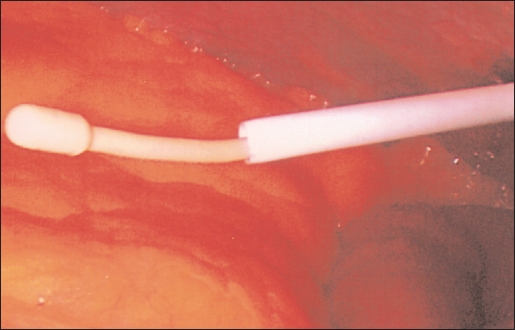
For unaffected results, the use of resistance unrestricted trocars (Storz HiCap 12-mm trocars: 8-mm insufflation diameter at supply, without stopcock and no Luer lock supply, Figure 6) for intra-abdominal pressure measurement and free intra-abdominal placement of the gas temperature probe is important (Figure 7).
Figure 6.
Storz HiCap trocar with low flow resistance.
Figure 7.
Free intra-abdominal placement of YSI temperature probe tip.
This model was used on a variety of 73 consecutive standard laparoscopic procedures (eg, cholecystectomy, hysterectomy, hernia, Nissen fundoplication, etc). The insufflator setting for all operations was 10 mm Hg nominal pressure and flowmax, O.R. temperature ∼23°C. A standard 10ft/3m insufflation hose with CO2 filter was used with all insufflators.
RESULTS
The measurements confirm that insufflators have different insufflation and flow properties despite having the same function. Pressure in the abdomen and insufflation hose are not always identical: abdominal pressure (≤50 mm Hg) is usually less than pressure in the system (≤75 mm Hg). Gas flow efficiency of insufflators is limited because high CO2 gas flow (>10 L/min) is rarely reached due to high resistance, especially in disposable trocars. The smaller the diameter at the insufflation supply, the higher the trocar flow resistance. Pressure peaks (≤50 mm Hg) in the abdomen at nominal pressure (10 mm Hg) occurred during trocar insertion and other abdominal manipulation — this can push gas or body fluids toward the insufflator. Negative pressure (≤50 mm Hg) and flow (≤-15 L/min) was measured during gallbladder removal with an Endobag (Table 1). During 73 procedures, body fluids were observed three times in the insufflation hose due to over pressure in the abdomen, insufficient relaxation and insufflator regulation with negative gas flow causing potential bacterial contamination if no CO2 gas filter was used.
Table 1.
Intraoperative activity affecting intra-abdominal pressure.
| Type of Manipulation | Pressure [mm Hg] |
|---|---|
| Trocar insertion | +18-23 |
| Intra-abdominal instruments manipulation | +25 |
| Physician leaning on abdomen | +30 |
| Insufficient patient relaxation | +50 |
| Insufflator switching on/off | −1−2 |
| Tissue removal with Endobag | −50 |
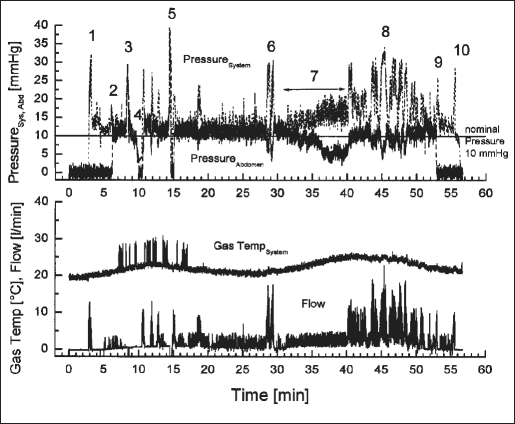
CO2 gas temperature in the hose equals room temperature. Changes in room temperature, depending on automatic air conditioning, are reflected in gas temperature fluctuation (Figure 8). Gas temperature in the abdomen can decrease up to 8.3°C (from 36.0 to 27.7°C, average 32.7°C, Table 2), and body core temperature can drop 1.01°C even with aggressive use of body surface warming equipment, especially under high-flow use of large amounts of gas and a prolonged period of insufflation. Snowden & Pencer's insufflator with internal gas heating cannot heat up CO2 to body temperature when it reaches the abdomen.
Figure 8.
Documentation of typical intraoperative insufflation problems (BEI Medical insufflator and Ethicon Endopath 512 trocar).
Table 2.
Intraoperative intra-abdominal gas temperature minimum.
| Intraoperative Intra-abdominal Gas Temperature Minimum (°C) | Patients (n) | Insufflation Time Average (Range) [min] |
|---|---|---|
| 35.01 - 36.00 | 2 | 47.5 (42 - 53) |
| 34.01 - 35.00 | 11 | 76.8 (21 - 159) |
| 33.01 - 34.00 | 13 | 78.4 (22 - 152) |
| 32.01 - 33.00 | 14 | 84.9 (27 - 182) |
| 31.01 - 32.00 | 8 | 116.9 (65 - 186) |
| 30.01 - 31.00 | 6 | 97.2 (30 - 269) |
| 29.01 - 30.00 | 1 | 140 |
| 28.01 - 29.00 | 0 | - |
| 27.01 - 28.00 | 2 | 204.5 (21 - 323) |
| Avg. 32.7 (35.4 - 27.7) | 57 | 91.5 (21 - 323) |
With this model, several intraoperative insufflation problems can be documented. An example is shown and explained in Figure 8.
Figure 8 is a graphical documentation of typical intraoperative insufflation problems: 1) start of insufflation; 2) trocar for abdominal pressure inserted; 3) abdominal pressure peak 30 mm Hg, over pressure recognized by BEI Medical insufflator, automatically shut off, negative gas flow −5 L/min; 4) not immediately recognized by staff, loss of pneumoperitoneum; 5) same as number 3, but now faster switched back on; 6) normal leakage reaction during Mesh insertion; 7) stop-cock at Ethicon insufflation trocar accidentally partly closed (ca. 30°); almost no insufflation diameter left, loss of pneumoperitoneum because of insufficient leakage reaction (flow limitation) until finally realized; 8) normal leakage compensation; 9) abdominal pressure trocar removed; 10) insufflation stopped; 11) measurement artifacts through electro-coagulation. Gas temperature curve in insufflation system is reflecting air condition regulation fluctuation.
DISCUSSION
With this computer model, for the first time objective data was measured about the real insufflation properties intraoperatively. The actual physical values measured show a wide range and are often not identical with the presetting on the insufflator. Some, especially overpressure of up to 50 mm Hg in the abdomen, can potentially threaten patient's safety.
Several attempts to evaluate properties of insufflation components have been made.2–4 They all neglect the effect of resistance on the performance of the entire insufflation system, evaluate components separately2,3 or measured at very low flow rates of 1-2 l/min.4 Previous measurements show the insufflation system has to be seen as a unit not as randomly combinable components.1 Function also often depends on the interaction between patient and equipment.
Though the results of our measurements are complex; the following statements can be made: Insufflators showed no significant difference regarding insufflation; insufflation problems described can occur with each of them. For better insufflator flow efficiency, reusable trocars should be used as they have, in general, less resistance than disposable ones.1 A filter in the insufflation system is necessary in order to prevent potential contamination of the insufflator. Insufflator-related pressure peaks of up to 40 mm Hg found in an abdomen model box in the laboratory study1 could not be confirmed. But intra-abdominal pressure peaks up to 50 mm Hg should be prevented by not leaning on the abdomen, providing sufficient relaxation and being careful with intra-abdominal instrument manipulation.
The significance of a decrease of intra-abdominal gas temperature and its potential correction is controversial. Internal heating of gas in the insufflator is inefficient because CO2 gas at the end of the insufflation hose is at room temperature. Maintaining body temperature with standard warming equipment, such as Bair Hugger®, Blanketrol®, heating blankets, and fluid warmer, etcetera, is possible and efficient, but take care of the problem (hypothermia) after it occurs. Prolonged CO2 pneumoperitoneum should be avoided in patients who could be affected by high-flow of CO2 gas and drop of abdominal temperature. Recent studies seem to have solved the problem with Insuflow®, a patient close-gas heating and hydration device.5
CONCLUSIONS
This computer-based measurement model has been proven to be useful for quality control study, intraoperative evaluation of the laparoscopic insufflation technique, and can measure different physical parameters in the OR. For other purposes, different devices can easily be substituted or added, and additional values can be calculated. Nevertheless, installation and adjustment of the PC card as well as graphic design of a complex measurement program can be challenging and difficult. Qualified technical support is essential.
The results demonstrate the need for intraoperative evaluation of the insufflation technique for laparoscopy and the need to document insufflation-related problems.6,7 Improvements in insufflation equipment, design of resistance optimized components, as well as standardization and adjustment of all insufflation components is necessary. Although no obvious complication related to insufflation problems occurred during our measurements, some results raise the potential of patient safety issues. Therefore, further investigation of the interaction between patient, physician and insufflation technique, the physical effects and its influence on the patient's physiology is necessary.
Acknowledgements:
The authors thank administration, OR personnel and all staff at Fayette Medical Center, Fayette, Alabama, for their comprehensive support and excellent cooperation during this study.
Footnotes
Disclosure Statement: We received no grant or financial support from any company for this study. We have no financial interest to promote products mentioned here. This study is absolutely independent and self-financed. We had no conflict of interests.
Contributor Information
Volker R. Jacobs, Department of Surgery, Fayette Medical Center (FMC), 1653 Temple Ave. N., Fayette, AL 35555, USA. Telephone: (205) 932-3879, Fax: (205) 932-5253, E-mail: drmorjo@aol.com.; Frauenklinik (OB/GYN), Christian-Albrechts-University, Michaelisstr. 16, 24105 Kiel, Germany. Telephone: +49-431-597-2100, Fax: +49-431-597-2146, E-mail: volkerjacobs@hotmail.com.
John E. Morrison, Jr, Department of Surgery, Fayette Medical Center (FMC), 1653 Temple Ave. N., Fayette, AL 35555, USA. Telephone: (205) 932-3879, Fax: (205) 932-5253, E-mail: drmorjo@aol.com.; Head of Department of Surgery at Fayette Medical Center.
Christoph Mundhenke, Frauenklinik (OB/GYN), Christian-Albrechts-University, Michaelisstr. 16, 24105 Kiel, Germany. Telephone: +49-431-597-2100, Fax: +49-431-597-2146, E-mail: volkerjacobs@hotmail.com..
Kirstin Golombeck, Frauenklinik (OB/GYN), Christian-Albrechts-University, Michaelisstr. 16, 24105 Kiel, Germany. Telephone: +49-431-597-2100, Fax: +49-431-597-2146, E-mail: volkerjacobs@hotmail.com..
Walter Jonat, Frauenklinik (OB/GYN), Christian-Albrechts-University, Michaelisstr. 16, 24105 Kiel, Germany. Telephone: +49-431-597-2100, Fax: +49-431-597-2146, E-mail: volkerjacobs@hotmail.com.; Director of Frauenklinik (OB/GYN), University of Kiel.
References:
- 1. Jacobs VR. Experimentelle Untersuchung zu den Insufflationseigenschaften verschiedener Veressnadeln, Trokare und Insufflatoren zum Aufbau eines Pneumoperitoneums in der Laparoskopie. [Experimental study on insufflation properties of different Veress needles, trocars and insufflators to establish pneumoperitoneum in laparoscopy.] Med Dissertation, 208 pages, University of Göttingen, Germany: 1996 [Google Scholar]
- 2. ECRI Laparoscopic insufflators. Health Devices. 1992;21:143–179 [PubMed] [Google Scholar]
- 3. ECRI High-Flow laparoscopic insufflators. Health Devices. 1995;24:252–285 [PubMed] [Google Scholar]
- 4. Borten M, Walsh AK, Friedman EA. Variations in gas flow of laparoscopic insufflators. Obstet Gynecol. 1986;68:522–526 [PubMed] [Google Scholar]
- 5. Ott DE, Reich H, Love B, et al. Reduction of laparoscopic-induced hypothermia, postoperative pain and recovery room length of stay by pre-conditioning gas with the Insuflowr device: a prospective randomized controlled multi-center study. JSLS. 1998;2(4):321–329 [PMC free article] [PubMed] [Google Scholar]
- 6. Jacobs VR, Morrison JE., Jr The real intra-abdominal pressure during laparoscopy: first intraoperative measurement model for insufflator evaluation in laparoscopy. Endo Expo `97, 6th Annual Meeting of the Society of Laparoendoscopic Surgeons (SLS), Orlando, FL, USA, December 3-6, 1997 JSLS. 1997;1(4):368–369 [Google Scholar]
- 7. Jacobs VR, Morrison JE., Jr Carbon dioxide gas heating in laparoscopy: is it worth it? Intraoperative evaluation of insufflators with vs. without CO2 gas heating device. Endo Expo `97, 6th Annual Meeting of the Society of Laparoendoscopic Surgeons (SLS), Orlando, FL, USA, December 3-6, 1997 JSLS. 1997;1(4):369 [Google Scholar]