Abstract
Background and Objectives:
It is essential to minimize pain after laparoscopic surgery. This study examined the effect of wound infiltration by a long-acting local anesthetic.
Methods:
This prospective, randomized study includes 190 laparoscopic procedures carried out by the same surgeon. The patients were randomly allocated into 2 groups. The control group comprised 75 cases of laparoscopic cholecystectomy (LC) and 20 cases of laparoscopic inguinal hernia repair (LIHR) without the use of a local anesthetic; only saline was used. The study group comprised 75 cases of LC and 20 cases of LIHR with preincisional periportal infiltration with 20 mL of ropivacaine (10 mg/mL). The postoperative pain scores at 3, 6, 12, and 24 hours determined with a visual analogue scale (VAS), nausea, and the kind and amount of analgesic drugs were assessed.
Results:
In the study group in 41% of LC cases and 85% of LIHR cases, no analgesia was required at all; likewise, in the control group in 20% of LC cases and 44% of LIHR cases, no analgesia was required. The difference was statistically significant (P<0.05). In the remainder, pain at 3 and 6 hours and total analgesic requirements in the study group were less than that in the control group (P<0.05). The postoperative nausea and shoulder pain remained statistically unchanged (P>0.05).
Conclusions:
It seems that wound infiltration with ropivacaine in laparoscopy provides satisfactory postoperative analgesia, diminishing or reducing the need for opioids.
Keywords: Laparoscopy, Laparoscopic cholecystectomy, Hernia repair, Local anesthesia, Analgesia, Ropivacaine
INTRODUCTION
It is well known that laparoscopy causes less postoperative pain than does open cholecystectomy,1,2 as do other laparoscopic procedures, eg, inguinal hernia repair.3,4 However, it is not completely painless.5 This pain is thought to be multifactorial in nature and severity, and various methods of analgesia have been introduced. They aim at avoidance of opioids and include nonsteroidal antiinflammatory drugs (NSAIDs), intraperitoneal local anesthesia,6 local anesthetic infiltration of the wound,7 intraperitoneal saline,8 adequate removal of the insufflation gas, heated gas, low pressure gas,9 and nitrous oxide pneumoperitoneum. The combination of techniques that have parietal, diaphragmatic, and visceral components may reduce pain after laparoscopy. The accurate assessment of pain is difficult because of its individual threshold, subjectivity, and difficulty in measurement. However, most of all, the prevention of pain should be directed peripherally at inputs along sensory axons or central neurons.10 Preincisional or preemptive analgesia with long-acting local anesthesia theoretically achieves peripheral blockage of pain stimuli, which is more advantageous than treating pain after it occurs. However, little is known about preemptive infiltration of trocar sites by local anesthetics. It is postulated that this reduces postoperative pain and analgesic requirements. Bupivacaine has been used recently for somatovisceral blockage with satisfactory results.11–13 In this prospective, randomized trial, we chose ropivacaine, a long-acting (duration 8 to 10 hours) local anesthetic, because of its postulated safety and theoretical improved efficacy. The purpose was to evaluate the analgesic effect of preincisional port-site wound infiltration in reducing postoperative pain after laparoscopic procedures in comparison with placebo use.
MATERIALS AND METHODS
This prospective, randomized trial was designed to include 190 laparoscopic procedures (150 cholecystectomies and 40 inguinal hernia repairs) carried out by the same surgeon. It conforms to CONSORT guidelines for the reporting of clinical trials. Ethical approval by the scientific committee of our hospital was achieved as was written consent from the patients. Patients were randomly allocated into 2 groups. The randomization was conducted by sealed envelope on the patient's arrival at the operating theater until the planned number of equivalent groups was reached. An independent surgeon was responsible for the randomization as well as for the preparation of an unmarked syringe containing 20 mL of ropivacaine or saline. The operating surgeon, the staff, and the patients were blinded to this procedure. In the control group including 75 cases of LC and 20 cases of LIHR, wound infiltration with local anesthetic was not used; only saline was used. In the study group including 75 cases of LC and 20 cases of LIHR, preincisional periportal infiltration with ropivacaine was applied. The patients belonged to ASA II or I, according to the classification of the American Society of Anesthesiologists. Patients with a previous upper abdominal operation or suspected bile duct stones by ultrasonography and liver function tests were excluded from laparoscopic cholecystectomy; those with a previous lower abdominal operation, except of appendectomy, were excluded from laparoscopic hernia repair.
Similar anesthetic and operative techniques were applied in all patients. Patients were premedicated with oral diazepam 0.15 mg/kg 1 hour before the operation. All patients received an intravenous injection of midazolam 2 mg and ondansetron 4 mg just before the anesthesia. General anesthesia with an endotracheal tube was achieved by using fentanyl 3 to 5 μg/kg and propofol 2 to 3 mg/kg followed by cisatracurium 0.1 mg/kg and sevoflurane to maintain it. Pneumoperitoneum was achieved by insertion under direct vision of a special cone-shaped trocar 10 to 12 mm (Ethicon, Cincinnati, OH, USA) through the infraumbilical region (Hasson open method) and insufflation of warmed carbon dioxide. This first trocar was used for the introduction of an optic direct view 0° for cholecystectomy and oblique view 30° for hernia repair.
Intraabdominal pressure was maintained at 12 mm Hg for cholecystectomy and at 16 mm Hg for hernia repair.
Before the skin incision and trocar placement, local infiltration of the port sites throughout all layers with 20 mL ropivacaine (Astra, Södertôlje, Sweden) containing 10 mg/mL (study group) or saline (control group) was performed. The local anesthetic or saline was equally allocated according to the diameter of the trocar; 7 mL for 10 to 12 mm and 3 mL for 5 mm.
Laparoscopic cholecystectomy was performed with the patient in a slight reverse Trendelenburg position with a 4-trocar technique, according to the “American” variable. Hernia repair was performed with the patient in the opposite position (slight Trendelenburg) with a 3-trocar technique. The hernia repair was achieved by a transabdominal preperitoneal (TAPP) approach and placement of a 6 × 11-cm polypropylene mesh (Prolene, Ethicon, Cincinnati, OH, USA) under the transversalis fascia to reinforce the posterior wall. It was secured at the site with titanium clips.
A drain was not used in any case. Antibiotic prophylaxis was attempted with 3 doses of a second-generation cephalosporin.
An independent nurse recorded the postoperative pain at the 3rd, 6th, 12th, and 24th hour after the operation according to patient's perception. The randomization was blind to both of them. Pain assessment was based on a 0 to 10 visual analogue scale (VAS, 0: no pain, 10: the worst imaginable pain). Preoperatively, the nurse introduced patients to the concept of a VAS scale. If the VAS score was above 3, an intramuscular (IM) injection of diclofenac 75 mg was applied. If pain was persistent, an IM injection of dextropropoxyphene 75 mg at first, and then if this was inadequate meperidine 50 mg was administered.
Postoperative nausea and shoulder pain were noted. The nausea was assessed by the patient's complaint and the need for the use of an antiemetic drug.
Parametric data were compared between groups by analysis of variances (ANOVA) and post-hoc testing. Statistical significance was assumed if P<0.05. Nonparametric data were analyzed with chi-square tests between groups. The analysis was performed with the Statistical Package for the Social Sciences (SPSS, Inc., Chicago, IL, USA).
RESULTS
Cholecystectomy was performed in the control group in 14 men and 61 women with a mean age of 55 years (range 22 to 82) and in the study group in 16 men and 59 women with a mean age of 56 years (range 17 to 88), suffering from symptomatic cholelithiasis. Inguinal hernia repair was performed in the control group in 16 patients including 14 men and 2 women with a mean age of 58 years (range 33 to 71), in which the hernia was bilateral in 4 cases and recurrent in 5 cases. It was performed in the study group in 14 patients including 13 men and 1 woman with a mean age of 60 years (range 35 to 72), in which the hernia was bilateral in 6 cases and recurrent in 6 cases.
The laparoscopic procedure was completed successfully in all cases without any intraoperative complications or need of conversion to an open operation.
The mean duration of the operation was 47 minutes (range 25 to 90) for cholecystectomy and 40 minutes (range 25 to 65) for hernia repair in the study group. It was 50 minutes (range 35 to 85) for LC and 45 minutes (range 30 to 90) for LIHR in the control group.
No cardiotoxicity, neurotoxicity or any other toxic effect was associated with the local use of ropivacaine. All but 4 patients recovered well and had an uneventful postoperative course without any complications or death. In 3 cases (2 in the study and 1 in the control group), after laparoscopic cholecystectomy (morbidity 1.5%), an ultrasound revealed mild infrahepatic bile collection (biloma) manifested by persistent right upper quadrant pain, fever, and leukocytosis. It was managed successfully by drainage under ultrasound guidance and antibiotics. In 1 case in the study group, after laparoscopic bilateral repair of a large recurrent inguinal hernia, moderate scrotal swelling was seen due to right spermatic cord edema. It was resolved in a few weeks.
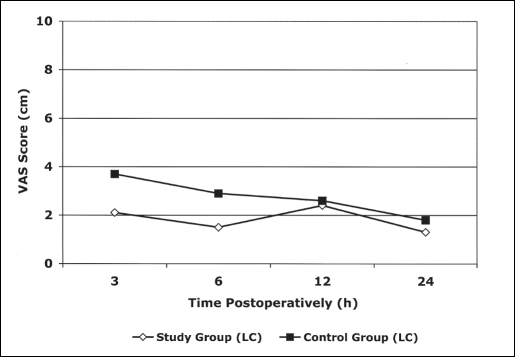
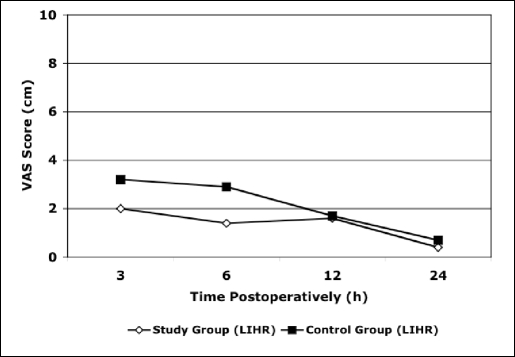
Postoperative analgesia was not required in the study group in 31 patients after LC (41%) and in 12 patients after LIHR (85%); in the control group in 15 patients after LC (20%) and in 7 patients after LIHR (44%). The differences were statistically significant (P<0.05). The VAS scores in the study group were significantly lower than those in the control group at the 3rd and 6th hours (P<0.01), whereas they did not differ significantly at the 12th and 24th hours (P>0.05) (Figures 1 and 2).
Figure 1.
Postoperative visual analogue scale (VAS) scores in the patients of the study group and control group after laparoscopic cholecystectomy (LC).
Figure 2.
Postoperative visual analogue scale (VAS) scores in the patients of the study group and control group after laparoscopic inguinal hernia repair (LIHR).
Shoulder pain was experienced in the study group in 20 patients after LC (27%) and in 1 patient after LIHR (7%); in the control group in 22 patients after LC (30%) and in 2 patients after LIHR (12%). The differences were not statistically significant (P>0.05). The pain was managed with diclofenac, a nonsteroidal antiinflammatory drug.
Opioids were used in the study group in 24 patients after LC (32%) and in 1 patient after LIHR (7%); in the control group in 36 patients after LC (51%) and in 8 patients after LIHR (50%). The differences were statistically significant (P<0.05). Their administration depended on the patient's description of persistent pain despite diclofenac administration. They include 8 doses of meperidine (50 mg each) after LC and 40 doses of dextropropoxyphene (75 mg each) in the study group and 20 doses of meperidine and 80 doses of dextropropoxyphene in the control group. After LIHR, 0 doses of meperidine and 2 doses of dextropropoxyphene were administered in the study group, and 3 doses of meperidine and 12 doses of dextropropoxyphene were administered in the control group.
Postoperative nausea was experienced in the study group in 18 patients after LC (24%) and in 1 patient after LIHR (7%); in the control group in 11 patients after LC (25%) and in 2 patients after LIHR (12%). The differences were not statistically significant (P>0.05). The nausea was managed with metoclopramide or ondansetron in more persistent cases.
The mean duration of hospital stay was 2.1 days (range 1 to 7) for cholecystectomy and 1.4 days (range 1 to 4) for hernia repair in the study group. It was 1.9 days (range 1 to 4) for LC and 1.5 days (range 1 to 3) for LIHR in the control group.
The mean time of return to normal activity was 5.1 days (range 4 to 10) after LC and 6.2 days (range 5 to 14) after LIHR in the study group. It was 5.3 days (range 4 to 9) for LC and 6.4 days (range 4 to 10) for LIHR in the control group.
DISCUSSION
Laparoscopic cholecystectomy reduces the incidence of postoperative right upper quadrant pain seen after open procedures.14,15 It has been reported that after laparoscopic cholecystectomy no analgesia was required by 26% of patients, nonnarcotic analgesia by 42%, and narcotic analgesia by 32%.7
Our results have been compared separately for 2 different laparoscopic procedures, ie, cholecystectomy and inguinal hernia repair. The results are reported here in the same article, and both evaluate the relief of pain coming from the port-site wounds. More specifically, in our study the use of ropivacaine increased the rate of no analgesia required from 20% to 41% after laparoscopic cholecystectomy and from 44% to 85% after laparoscopic TAPP inguinal hernia repair. Likewise, it decreased the rate of opioid requirement and the quantity, from 51% to 32% after laparoscopic cholecystectomy and from 50% to 7% after laparoscopic TAPP inguinal hernia repair. Postoperative nausea and shoulder pain remained statistically unchanged. However, it is important to note that in this study after laparoscopic cholecystectomy, one third of our patients with ropivacaine infiltration still required opium analgesia; this indicates perhaps that the origin of pain may have been other than at the port site. The port-site wounds consist of the most usual cause of pain in the immediate postoperative hours; other less common sources of distress are visceral mainly from cholecystectomy and shoulder tip pain attributed to diaphragmatic stretching.5
Periportal peritoneal injection of a long-acting local anesthetic reduces immediate postoperative pain after laparoscopic cholecystectomy. The parietal peritoneum injury at the port sites may be a source of pain. For this reason, infiltration to around this level is preferable.16 This approach was our policy.
In a recent review article,5 it was affirmed that regarding pre- or postoperative wound injection, one is not more effective than the other. However, Sarac et al17 suggested that preemptive injection is not as effective as postoperative injection. Therefore, it seems that this is a debatable issue. In this study, we preferred the preincisional use to block sensory inflow at the periphery, preventing the pain stimuli. It seems that recent reports11–13 support this preemptive local infiltration.
Intraperitoneal use of bupivacaine alone6 or in combination with normal saline8 in pain control after laparoscopic cholecystectomy has not gained wide acceptance. Also, instilling bupivacaine into the confined preperitoneal space has no effect on postoperative pain after TAPP laparoscopic hernia repair, and its routine use cannot be recommended.18
Some refinements in laparoscopic cholecystectomy techniques have been made, but the use of the open Hasson's method for the initial peritoneal access has not been widely accepted. Half of the bowel injury during laparoscopic cholecystectomy has happened as a result of a blind insertion of the Veress needle or the first trocar placement.19 We now routinely use the open method under direct vision to avoid this and other rare inadvertent visceral or vessel injuries. However, this approach using sutures for fascial repair may be a further source of pain. The incidence of herniation through port sites has not yet been accurately documented.
Also, the local anesthetic can be infused into a surgical wound in day surgery inguinal hernia repair for pain relief.20
Ropivacaine is a recently introduced long-acting local anesthetic with lower toxicity, fewer side effects, and is longer-lasting than bupivacaine. The duration of its action is 8 to 10 hours. Preoperative local infiltration of the inguinal wound for pain relief after open tension-free hernia repair is an effective and safe method.21–23 The addition of other drugs (ketorolac or clonidine) to the local anesthetic to increase the duration of their postoperative analgesic effect is debatable.24–26
Despite pain control, postoperative nausea and vomiting are common side effects after general anesthesia and surgery, especially in patients undergoing laparoscopic procedures. The intravenous administration of metoclopramide or especially ondansetron, as in our experience, may be beneficial.27
CONCLUSION
Our study suggests that preincisional periportal infiltration by ropivacaine is a safe, effective, and affordable method for pain relief after laparoscopic cholecystectomy or laparoscopic inguinal hernia repair. Its efficacy diminishes or reduces the quantity of opioids required. The VAS scores at 24 hours were similar for both laparoscopic procedures.
References:
- 1. McMahon AJ, Russell IT, Ramsay G, et al. Laparoscopic and minilaparotomy cholecystectomy: a randomized trial comparing postoperative pain and pulmonary function. Surgery. 1994;115:533–539 [PubMed] [Google Scholar]
- 2. Squirrell DM, Majeed AW, Troy G, Peacock JE, Nicholl JP, Johnson AG. A randomized, prospective, blinded comparison of postoperative pain, metabolic response, and perceived health after laparoscopic and small incision cholecystectomy. Surgery. 1998;123:485–495 [DOI] [PubMed] [Google Scholar]
- 3. Wilson M, Deans G, Brough W. Prospective trial comparing Lihctenstein with laparoscopic tension-free mesh repair of inguinal hernia. Br J Surg. 1995;82:274–277 [DOI] [PubMed] [Google Scholar]
- 4. Kozol R, Lange P, Kosir M, Beleski K, Mason K, Tennenberg S. A prospective randomized study of open vs laparoscopic inguinal hernia repair. An assessment of postoperative pain. Arch Surg. 1997;132:292–295 [DOI] [PubMed] [Google Scholar]
- 5. Wills VL, Hunt DR. Pain after laparoscopic cholecystectomy. Br J Surg. 2000;87:273–284 [DOI] [PubMed] [Google Scholar]
- 6. Forani M, Miglietta C, Di Gioia S, Garrone C, Morino M. The use of intraoperative topical bupivacaine in the control of postoperative pain following laparoscopic cholecystectomy. Minerva Chir. 1996;51:881–885 [PubMed] [Google Scholar]
- 7. Ure BM, Troidl H, Spangenberger W, et al. Preincisional local anaesthesia with bupivacaine and pain after laparoscopic cholecystectomy. A double-blind randomized clinical trial. Surg Endosc. 1993;7:482–488 [DOI] [PubMed] [Google Scholar]
- 8. Tsimoyiannis EC, Glantzounis G, Lekkas ET, Siakas P, Jabarin M, Tzourou H. Intraperitoneal normal saline and bupivacaine infusion for reduction of postoperative pain after laparoscopic cholecystectomy. Surg Laparosc Endosc. 1998;8:416–420 [PubMed] [Google Scholar]
- 9. Wallace DH, Serpell MG, Baxter JN, O'Dwyer PJ. Randomized trial of different insufflation pressures for laparoscopic cholecystectomy. Br J Surg. 1997;84:455–458 [PubMed] [Google Scholar]
- 10. Wu CT, Yu JC, Yeh CC, Li CY, Ho ST, Wong CS. Preincisional dextromethorphan treatment decreases postoperative pain and opioid requirement after laparoscopic cholecystectomy. Anesth Analg. 1999;88:1331–1334 [DOI] [PubMed] [Google Scholar]
- 11. Kato J, Ogawa S, Katz H, Nagai H, Kashiwazaki M, Saeki H, Suzuki H. Effects of presurgical local infiltration of bupivacaine in the surgical field on postsurgical wound pain in laparoscopic gynecologic examinations: a possible preemptive analgesic effect. Clin J Pain. 2000;16:12–17 [DOI] [PubMed] [Google Scholar]
- 12. Hasaniya NW, Zayed FF, Faiz H, Severino R. Preinsertion local anesthesia at the trocar site improves perioperative pain and decreases costs of laparoscopic cholecystectomy. Surg Endosc. 2001;15:962–964 [DOI] [PubMed] [Google Scholar]
- 13. Lee IO, Kim SH, Kong MH, et al. Pain after laparoscopic cholecystectomy: the effect and timing of incisional and intraperitoneal bupivacaine. Can J Anaesth. 2001;48:545–550 [DOI] [PubMed] [Google Scholar]
- 14. Stiff G, Rhodes M, Kelly A, Telford K, Armstrong CP, Rees BI. Long-term pain: less common after laparoscopic than open cholecystectomy. Br J Surg. 1994;81:1368–1370 [DOI] [PubMed] [Google Scholar]
- 15. Berggren U, Gordh T, Grama D, Haglund U, Rastad J, Arvidsson D. Laparoscopic versus open cholecystectomy: hospitalization, sick leave, analgesia and trauma responses. Br J Surg. 1994;81:1362–1365 [DOI] [PubMed] [Google Scholar]
- 16. Alexander DJ, Ngoi SS, Lee L, et al. Randomized trial of periportal peritoneal bupivacaine for pain relief after laparoscopic cholecystectomy. Br J Surg. 1996;83:1223–1225 [PubMed] [Google Scholar]
- 17. Sarac AM, Aktan AO, Baykan N, Yegen C, Yalin R. The effect and timing of local anesthesia in laparoscopic cholecystectomy. Surg Laparosc Endosc. 1996;6:362–366 [PubMed] [Google Scholar]
- 18. Deans GT, Wilson MS, Brough WA. Controlled trial of preperitoneal local anaesthetic for reducing pain following laparoscopic hernia repair. Br J Surg. 1998;85:1013–1014 [DOI] [PubMed] [Google Scholar]
- 19. Deziel D, Millikan K, Economou S, Doolas A, Ko S, Airan M. Complications of laparoscopic cholecystectomy: a national survey of 4292 hospitals and an analysis of 77604 cases. Am J Surg. 1993;165:9–14 [DOI] [PubMed] [Google Scholar]
- 20. Oakley MJ, Smith JS, Anderson JR, Fenton-Lee D. Randomized placebo-controlled trial of local anaesthetic infusion in day-case inguinal hernia repair. Br J Surg. 1998;85:797–799 [DOI] [PubMed] [Google Scholar]
- 21. Johanson B, Hallerback B, Stubberod A, et al. Preoperative local infiltration with ropivacaine for postoperative pain relief after inguinal hernia repair. A randomized controlled trial. Eur J Surg. 1997;163:371–378 [PubMed] [Google Scholar]
- 22. Pettersson N, Emanuelsson BM, Reventlid H, Hahn RG. High-dose ropivacaine wound infiltration for pain relief after inguinal hernia repair: a clinical and pharmacokinetic evaluation. Reg Anesth Pain Med. 1998;23:189–196 [DOI] [PubMed] [Google Scholar]
- 23. Pettersson N, Berggren P, Larsson M, Westman B, Hahn RG. Pain relief by wound infiltration with bupivacaine or high-dose ropivacaine after inguinal hernia repair. Reg Anesth Pain Med. 1999;24:569–575 [DOI] [PubMed] [Google Scholar]
- 24. Connelly NR, Reuden SS, Albert M, Page D. Use of preincisional ketorolac in hernia patients: intravenous versus surgical site. Reg Anesth. 1997;22:229–232 [DOI] [PubMed] [Google Scholar]
- 25. Connelly NR, Reuden SS, Albert M, et al. Use of clonidine in hernia patients: intramuscular versus surgical site. Reg Anesth Pain Med. 1999;24:422–425 [DOI] [PubMed] [Google Scholar]
- 26. Elliott S, Eckersall S, Fligelstone L, Jothilingam S. Does the addition of clonidine affect of analgesia of bupivacaine wound infiltration in inguinal hernia surgery? Br J Anaesth. 1997;79:446–449 [DOI] [PubMed] [Google Scholar]
- 27. Fujii Y, Tanaka H, Kawasaki T. Randomized clinical trial of granisetron, droperidol and metoclopramide for the treatment of nausea and vomiting after laparoscopic cholecystectomy. Br J Surg. 2000;87:285–288 [DOI] [PubMed] [Google Scholar]