Abstract
Aims
Risk stratification in individuals with type 1 Brugada electrocardiogram (ECG) pattern (type 1 ECG) for primary prevention of sudden death (SD).
Methods and results
Three hundred and twenty patients (258 males, median age 43 years) with type 1 ECG were enrolled. No patient had previous cardiac arrest. Fifty-four per cent of patients had a spontaneous and 46% a drug-induced type 1 ECG. One-third had syncope, two-thirds were asymptomatic. Two hundred and forty-five patients underwent electrophysiologic study (EPS) and 110 patients received an implantable cardiac defibrillator (ICD). During follow-up [median length 40 months (IQ20-67)], 17 patients had major arrhythmic events (MAE) (14 resuscitated ventricular fibrillation (VF) and three SD). Both a spontaneous type 1 ECG and syncope significantly increased the risk (2.6 and 3.0% event rate per year vs. 0.4 and 0.8%). Major arrhythmic events occurred in 14% of subjects with positive EPS, in no subjects with negative EPS and in 5.3% of subjects without EPS. All MAE occurred in subjects who had at least two potential risk factors (syncope, family history of SD, and positive EPS). Among these patients, those with spontaneous type 1 ECG had a 30% event rate.
Conclusion
(1) In subjects with the Brugada type 1 ECG, no single clinical risk factor, nor EPS alone, is able to identify subjects at highest risk; (2) a multiparametric approach (including syncope, family history of SD, and positive EPS) helps to identify populations at highest risk; (3) subjects at highest risk are those with a spontaneous type 1 ECG and at least two risk factors; (4) the remainder are at low risk.
Keywords: Brugada syndrome, Risk stratification, Programmed ventricular stimulation, Sudden cardiac death
Introduction
Brugada type 1 electrocardiogram (ECG) pattern is characterized by coved-type ST segment elevation (>2 mm) in the right precordial leads.1–5 This pattern may be present in the basal ECG or be unmasked by the infusion of Na channel-blocking drugs in subjects with type II or III ECG patterns.6–8
Individuals with type 1 Brugada ECG pattern may suffer from malignant ventricular arrhythmias (Brugada syndrome).9–11 It is generally agreed that patients with Brugada syndrome and documented cardiac arrest should receive an implantable cardiac defibrillator (ICD). In the remaining subjects, the best policy is controversial.12
Many data13–22 suggest that patients with syncope, particularly if they have a spontaneous type 1 ECG pattern, have a significant risk; some authors13–17 therefore suggest ICD implantation in these cases, too. In the remaining population of asymptomatic subjects, the risk is lower but not negligible.13,17 How to manage these latter cases, and in particular how to recognize those at highest risk who would benefit from ICD implantation,23,24 is an unsolved issue.
The usefulness of electrophysiologic study (EPS) in risk stratification, i.e. the inducibility of sustained ventricular tachycardia/ventricular fibrillation (VT/VF) is controversial.17,25–27 Indeed, some authors, particularly the Brugada brothers,10,13,14 strongly support the prognostic value of EPS, while others15,16,19 completely deny its usefulness.
To address the problem of risk stratification in subjects with type 1 Brugada pattern, we analysed the prospective experiences of five Italian centres. The aim was to evaluate the usefulness of a combined approach that considered both clinical data and the results of EPS.
Methods
Study population
This prospective study involved 320 patients (258 males, mean age 43± years) with type 1 Brugada pattern enrolled in five Italian centres since 1998: Conegliano, Asti, Rome, Udine, and Portogruaro. No patient had previous cardiac arrest or documented VT/VF.
In accordance with current guidelines, the type 1 Brugada ECG pattern was defined in the presence of coved ST elevation (>2 mm) in one or more leads from V1 to V3, either spontaneous or induced by class I anti-arrhythmic drug administration (I-type 1). Spontaneous type 1 pattern was defined when at least one ECG documented a type 1 pattern in the absence of anti-arrhythmic drugs. A type 1 ECG pattern recorded in II–III intercostals spaces was considered diagnostic. Type II ECG pattern was defined in the presence of a >2 mm J point elevation and >1 mm saddleback-type ST elevation with positive T wave. Type III pattern was defined as a <1 mm saddleback- or coved-type ST elevation. Sodium channel blockers used were flecainide (2 mg/kg i.v. in 10 min) or ajmaline (1 mg/kg i.v. in 5 min). Testing was performed in subjects with type II or III patterns. The test was considered positive only if a coved-type 1 ECG pattern was documented. Individuals with type II or III patterns in whom anti-arrhythmic drugs did not reproduce a type 1 pattern were excluded from the study.
All ECG of patients participating in the study were analysed by a central board.
In all patients with spontaneous or drug-induced type 1 pattern, a thorough family history was collected in order to search for subjects who had died suddenly with a type 1 Brugada ECG pattern or before the age of 40 years in the absence of known heart disease.
Patients without syncope were regarded as asymptomatic. Syncope was defined as loss of consciousness in accordance with the current literature. For the purpose of this paper, no attempt was made to differentiate vaso-vagal from possible arrhythmic forms. All syncopes were therefore included. Patients with resuscitated cardiac arrest were excluded from this study.
All patients underwent echocardiography, laboratory tests, and other examinations, if appropriate, in order to exclude the presence of an underlying structural heart disease. In all cases, EPS was proposed.
Electrophysiologic study
After informed written consent had been obtained, EPS including ventricular premature stimulation (VPS) was carried out. Ventricular premature stimulation was performed at two right ventricular sites: first at the apex and then at the outflow tract. Ventricular premature stimulation was carried out in the different centres by utilizing two protocols with comparable aggressiveness. Protocol A included two pacing cycle lengths (600 and 400 ms) with up to two extrastimuli. The extrastimuli were anticipated in 10 ms decrements up to the shortest coupling interval that resulted in ventricular capture. Protocol B included two pacing cycle lengths (600 and 400 ms) with up to three extrastimuli. The extrastimuli were anticipated in 10 ms decrements up to a shortest coupling interval of 200 ms.
The endpoint of VPS was the induction of a sustained ventricular arrhythmia (polymorphic or monomorphic ventricular tachycardia, VF) leading to collapse and requiring shock or the completion of the protocol. Positive EPS was defined when a sustained ventricular arrhythmia (>30′) requiring shock was induced. Negative EPS was defined when no ventricular arrhythmia or a self-terminating ventricular arrhythmia was induced but did not require shock.
Protocol A was employed in 91 cases, protocol B in 154. In 75 cases, EPS was not performed.
Implantable cardiac defibrillator implantation
Patients were informed of their potential risk, which was based mainly on the presence of a spontaneous type 1 pattern and a history of syncope. The prognostic value of a family history of sudden death (SD) and of inducibility of VT/VF by EPS was explained as questionable risk factors. The decision to implant an ICD was taken after written informed consent had been provided.
All ICD implanted were capable of recording and storing ECG data at the time of episodes of shock. Detailed ICD programming was left to investigator preference, also on the basis of the different devices employed. However, in all cases, a single VF zone was programmed with a lower detection rate of 180 b.p.m. Ventricular back-up pacing was programmed at a rate of 35–50 b.p.m.
Follow-up
Follow-up examinations were performed every 6 months or in the event of symptoms. All patients were called for the last follow-up examination between January and June 2009. All patients were followed up for at least 1 year. Ten patients were lost to the last follow-up examination. In patients with ICD, analysis of arrhythmias and of appropriate and inappropriate shocks was also performed. Patients were considered to have major arrhythmic events (MAE) if they suddenly died or if VT/VF was recorded by the implanted ICD or by conventional ECG.
Statistical analysis
Statistical analysis was carried out with Systat 12 (2008, Chicago, IL, USA) and JMP 4.0 for Windows (SAS Institute, 2000, Cary, NC, USA) packages. For continuous variables (after checking they had normal distribution), comparisons among groups were made by means of Student's t-test or ANOVA. Pearson's χ²-test was used for categorical variables. Event analysis over time was made by using the Cox proportional hazard regression model. Risk was quantified as a hazard ratio with 95% confidence interval (CI). Survival curves were constructed by means of the Kaplan–Meier method and compared by the log-rank test. For event prediction, C-statistic analysis was used. Like the area under the ROC curve, the C-statistic ranges from 0.5 (i.e. no discrimination) to 1.0 (maximum discrimination ability).
Data are presented as medians and interquartiles for continuous measures and as proportions for categorical variables. All P values are two-tailed, and statistical significance was established as P < 0.05.
Results
Clinical characteristics
Table 1 shows the clinical and ECG characteristics of patients. In brief, 54% of patients had a spontaneous type 1 pattern, while in the remainder, a type 1 ECG pattern was induced by anti-arrhythmic drugs. Ninety-four patients (29%) had a family history of SD.
Table 1.
Baseline characteristics of the entire population of 320 patients
| Median (IQ) age | 43 (33–54) |
| Male sex | 258 (81%) |
| Resting ECG | |
| Type 1 | 174 (54%) |
| Type 2 | 90 (28%) |
| Type 3 | 56 (17%) |
| Positive family history of sudden death | 94 (29%) |
| Syncope | 105 (34%) |
| EPS performed | 245 (77%) |
| ICD implanted | 110 (34%) |
About one-third of patients had syncopal episodes, while two-thirds were asymptomatic. Among the latter, 46 had a family history of SD and 40 had a history of Brugada syndrome (without familial SD), while 129 had neither a family history of SD nor a family history of Brugada syndrome.
Electrophysiologic study
Electrophysiologic study was performed in 245 patients; 75 patients refused EPS. Table 2 summarizes the clinical characteristics of subjects who underwent EPS and of those who did not. In general, the two groups were similar, with the exception of a higher prevalence of syncope in patients who underwent EPS.
Table 2.
Clinical differences between patients who underwent electrophysiologic study (EPS) (n = 245) and those who did not (n = 75)
| EPS NP (n = 75) | EPS (n = 245) | P-value | |
|---|---|---|---|
| Age (years) | 41 (IQ 32–53) | 44 (IQ 34–53) | 0.31 |
| Sex (male) | 81% | 80% | 0.85 |
| Family history of SCD | 23% | 31% | 0.14 |
| History of syncope | 18% | 37% | 0.003 |
| Basal type 1 ECG pattern | 45% | 57% | 0.072 |
EPS NP, EPS not performed.
Positive EPS included the induction of polymorphic VT/VF in all but three cases. In these three cases, a fast monomorphic sustained VT was induced. In all cases, induced arrhythmias required shock.
As shown in Table 3, EPS was positive in 50% of symptomatic vs. 32% of asymptomatic subjects (P = 0.07). Furthermore, EPS was positive in 49% of subjects with spontaneous type 1 ECG pattern vs. 26% of those with drug-induced type 1 ECG pattern (P = 0.43). Electrophysiologic study was positive in 35/91 (38%) patients who underwent protocol A and in 61/154 (39%) patients who underwent protocol B (P = 0.84). VT/VF was induced by a single extrastimulus in 2%, by double extrastimuli in 74%, and by triple extrastimuli in 24% (2/96, 71/96, and 23/96, respectively).
Table 3.
Percentages of positive electrophysiologic study (EPS) (EPS+) in the entire population of 245 patients who underwent EPS, and in different subsets of patients: symptomatic, asymptomatic, basal type 1 ECG, type 1 ECG induced by drugs
| n | EPS+ (n) | % EPS+ | |
|---|---|---|---|
| All patients | 245 | 96 | 39 |
| Symptomatica | 91 | 46 | 50 |
| Asymptomatic | 154 | 50 | 32 |
| Basal type 1 ECG | 140 | 69 | 49 |
| Drug-induced type 1 ECG | 105 | 27 | 26 |
aSymptomatic for syncope.
Implantable cardiac defibrillator implantation
Implantable cardiac defibrillators were implanted in 110 patients. The clinical and EPS characteristics of these patients are summarized in Table 4. In brief, 84% were males, 38% had a family history of SD, 74% had a spontaneous type 1 ECG pattern, 58% had syncope, and 81% had a positive EPS.
Table 4.
Clinical and electrophysiologic characteristics of patients who received [implantable cardiac defibrillator (ICD)] or did not receive (no ICD) an ICD
| No ICD (n= 210) | ICD (n = 110) | P-value | |
|---|---|---|---|
| Male | 165 (78%) | 93 (84%) | 0.25 |
| Syncope | 41 (19%) | 64 (58%) | <0.001 |
| Basal type 1 ECG | 92 (44%) | 82 (74%) | <0.001 |
| EPS+ | 6/139 (4%) | 90/106 (85%) | <0.001 |
| Family history of SD | 52 (25%) | 42 (38%) | 0.02 |
| Median (IQ) | 41 (21–67) | 40 (23–67) | 0.73 |
| follow-up (months) |
The entire population comprised 320 patients. The results of EPS refer to a subset of 245 patients who underwent EPS. EPS+ = positive EPS.
Follow-up
During follow-up [median length 40 months (IQ20-67)], 17 patients suffered MAE (14 VF recorded by ICD and three SDs). Among the 14 VF, which were interrupted by the ICD, the shock was delivered 10–22′ after the onset of the arrhythmia. Major arrhythmic events occurred in 10.4% of symptomatic and 2.8% of asymptomatic subjects.
Clinical outcome predictors
The following variables were analysed as potential predictors of MAE: age, gender, syncope, basal type 1 ECG, and family history of SD.
Table 5 shows outcome rate per year by risk factor, a significantly increased risk was associated with basal type 1 ECG and syncope, which displayed 2.6 and 3.0% event rates, respectively. Male gender (1.7% event rate per year) and family history of SD (2.2% event rate per year) showed only a trend towards increased risk. On univariate and multivariate analysis, a significant increase in risk was found for basal type 1 ECG and syncope (Table 6).
Table 5.
Outcome rate per year by risk factor in the entire population of 320 patients
| Events rate per year (%) | P-value | |
|---|---|---|
| Age | ||
| >43 years | 1.9 | 0.47 |
| <43 years | 1.3 | |
| Male | 1.7 | 0.41 |
| Female | 0.9 | |
| Syncope | 3.0 | 0.004 |
| No syncope | 0.8 | |
| Basal type 1 ECG | 2.6 | 0.004 |
| 1C ECG | 0.4 | |
| Family history | 2.2 | 0.27 |
| No family history | 1.3 | |
Table 6.
Univariate and multivariate analysis in the entire population of 320 cases
| Univariate analysis |
Multivariate analysis |
|||||
|---|---|---|---|---|---|---|
| Hazard ratio | 95% CI | P | Hazard ratio | 95% CI | P-value | |
| Age (per year) | 0.9 | 0.8–1.0 | 0.19 | – | – | – |
| Male | 2.1 | 0.6–13.3 | 0.28 | – | – | – |
| Syncope | 3.1 | 1.2–9.2 | 0.01 | 2.8 | 1.1–8.1 | 0.03 |
| Basal type 1 ECG | 6.6 | 1.8–41.8 | 0.001 | 6.2 | 1.8–39.9 | 0.002 |
| Family history of SD | 1.9 | 0.7–4.8 | 0.22 | – | – | – |
Role of electrophysiologic study as a single predictor of outcome
Major arrhythmic events occurred in 14% of patients with positive EPS, in 0% of those with negative EPS, and in 5.3% of those who did not undergo EPS (P < 0.001). The positive predictive value of EPS was therefore 14% and the negative predictive value was 100%.
In subjects with positive EPS, MAE occurred in 17% of those who underwent protocol A and in 11.4% of those who underwent protocol B (6/35 and 7/61, respectively, P = 0.40).
Major arrhythmic events occurred in 0, 15.5, and 8.6% of patients in whom VT/VF was induced by single, double, and triple extrastimuli, respectively (0/2, 11/71, 2/23, P = 0.23).
Multiparametric (clinical and instrumental) risk stratification
As shown in Table 7, the presence of one clinical risk factor displayed only a low ability to predict MAE (C-statistics 0.58–0.71). By contrast, an increased risk was observed on combining two or more clinical risk factors (C-statistics 0.66–0.77). The combination best able to predict MAE was spontaneous type 1 pattern, family history of SD, and syncope (C-statistics 0.77; 95% CI: 0.71–0.82). A positive EPS increased the ability of clinical factors to predict the risk (Δ C-statistic 0.11–0.21).
Table 7.
Discriminate analysis by C-statistic in 245 patients who underwent electrophysiologic study (EPS) in whom all risk factors were able to be evaluated
| Clinical variables | C-statistics (95% CI) | EPS+ added (95% CI) | Δ C-statistics | P-value |
|---|---|---|---|---|
| Family history of SD (FAM) | 0.58 (0.51–0.64) | 0.79 (0.74–0.84) | 0.21 | <0.001 |
| Basal type 1 ECG (ECG) | 0.64 (0.58–0.70) | 0.82 (0.77–0.87) | 0.18 | <0.001 |
| Syncope (SYN) | 0.71 (0.65–0.77) | 0.86 (0.81–0.90) | 0.15 | <0.001 |
| FAM + ECG | 0.66 (0.60–0.72) | 0.81 (0.75–0.85) | 0.15 | <0.001 |
| FAM + SYN | 0.73 (0.68–0.80) | 0.87 (0.82–0.91) | 0.14 | <0.001 |
| ECG + SYN | 0.76 (0.70–0.81) | 0.87 (0.82–0.91) | 0.11 | <0.001 |
| FAM + ECG + SYN | 0.77 (0.71–0.82) | 0.87 (0.82–0.90) | 0.10 | 0.001 |
In the first column, clinical variables are analysed singly and in different combinations. In the fourth column, the added value of EPS is shown and expressed as delta C-statistics.
In the group of 245 patients who underwent EPS, the combination best able to predict major events was that of syncope, basal type 1 ECG, family history of SD, and positive EPS (C-statistic 0.87; 95% CI: 0.82–0.90).
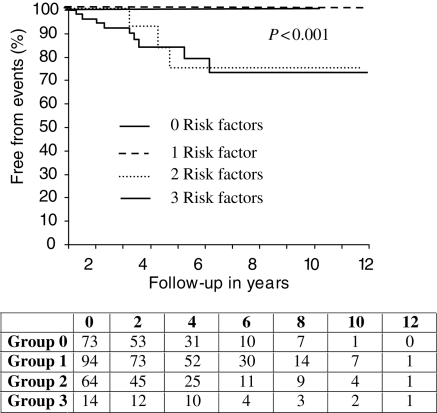
In those patients who underwent EPS, Kaplan–Meier curves were plotted on considering three risk factors: syncope, family history of SD, and positive EPS. No events occurred in subjects without any of these risk factors or with only one. Indeed, MAE occurred only in subjects with two or three risk factors (P < 0.001) (Figure 1).
Figure 1.
Kaplan–Meier survival curves in the entire population of 245 patients who underwent electrophysiologic study (EPS). Risk factors considered were: family history of sudden death, syncope, and positive EPS. Curves are plotted according to the presence of 0, 1, 2, or 3 risk factors.
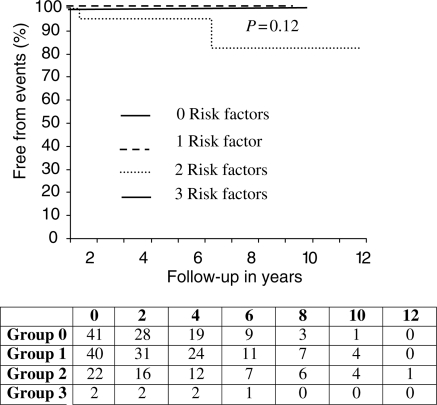
In the subgroup of 140 patients with a spontaneous type 1 pattern (Figure 2), MAE occurred in about 30% of subjects with two or three risk factors (P < 0.001). In the remaining 105 patients (Figure 3), i.e. those with a type 1 ECG pattern induced by anti-arrhythmic drugs, only two MAE occurred in subjects with two risk factors (P = 0.12).
Figure 2.
Kaplan–Meier survival curves in the population of 140 patients with basal type 1 ECG who underwent electrophysiologic study (EPS). Risk factors considered were: familial history of sudden death, syncope, and positive EPS. Curves are plotted according to the presence of 0, 1, 2, or 3 risk factors.
Figure 3.
Survival Kaplan–Meier curves in the population of 105 patients with drug-induced type 1 ECG who underwent electrophysiologic study (EPS). Risk factors considered were: family history of sudden death, syncope, and positive EPS. Curves are plotted according to the presence of 0, 1, 2, or 3 risk factors.
Discussion
Malignant arrhythmias and SD can occur in subjects with the Brugada type 1 ECG pattern. In early reports,13–17 malignant arrhythmias and SD were reported to be frequent. More recent papers, however, have shown that they are relatively rare.10,11
Our study confirms these latter data. In this prospective study, which enrolled individuals with the type 1 ECG pattern without previous cardiac arrest, malignant arrhythmias occurred in 5.3% of cases. Specifically, they occurred in 10.4% of symptomatic and 2.8% of asymptomatic subjects (P = 0.004) during a median follow-up 3.3 years. It follows that malignant arrhythmias occurred in 3.0 and 0.8%/patient/year in symptomatic and asymptomatic subjects (P = 0.004), respectively (Table 5).
In patients with Brugada syndrome and documented cardiac arrest, ICD implantation is mandatory. In the remaining patients, who constitute the vast majority of subjects encountered in the clinical setting, the best policy is unclear.12 The relative rarity of fatal events, however, suggests that it is not reasonable to implant an ICD in all subjects with a type 1 ECG pattern, particularly if they have no symptoms. Therefore, the main problem is to predict, in the setting of the entire population with the type 1 ECG pattern, which subjects have the highest risk of suffering a potentially fatal event.
In agreement with most authors, in our study a spontaneous type 1 ECG pattern proved to be a clinical risk factor, both on univariate and multivariate analysis (Table 6). On the other hand, a type 1 ECG pattern induced only by drugs identified subjects at low risk. Specifically, major events occurred in 8.6% of patients with a spontaneous type 1 ECG pattern vs. 1.3% of those with a drug-induced type 1 ECG pattern (P = 0.004). A history of syncope was confirmed to be a risk factor (10.4% event rate vs. 2.8% in asymptomatic patients, P = 0.004). Finally, a family history of SD was confirmed to be a weak risk factor (7.4 vs. 4.4%, P = 0.27). In general, however, all three clinical risk factors showed a low positive predictive value (8.6, 10.4, and 7.4%, respectively).
In the current literature, the predictive value of EPS is controversial.23,24 Indeed, while some authors13,14 report a high prognostic significance of EPS, others deny its usefulness. However, many of the multicentre studies that have indicated the scant usefulness of EPS display major methodological problems. In particular, these studies used heterogeneous stimulation protocols.15,16,19,25–27 Furthermore, the precise protocols are often not clearly specified. For example, some authors simply state that ‘heterogeneous protocols were used’,15 while others use ambiguous definitions, such as ‘up to three extrastilmuli were employed’,19 which does not indicate whether all patients had triple extrastimuli or whether some underwent a less aggressive protocol. The latter hypothesis seems more probable in a recent large multicentre study by Probst et al.,19 on the basis of the previously published experiences of the participating centres.
It follows that the category of patients with negative EPS may include those in whom the non-inducibility of VT/VF is due to the low intensity of stimulation. In other words, it is possible that some of them would have a positive EPS if more aggressive stimulation were used.
In our multicentre study, two comparably aggressive protocols were employed, and were completed in all cases. As a result, in agreement with many authors, our EPS was frequently positive in both symptomatic and asymptomatic subjects. Indeed, in our study, EPS was positive in 50% of symptomatic and 32% of asymptomatic subjects. Consequently, when considered alone, EPS displayed a low positive predictive value (14%). Thus, a positive EPS cannot be considered a gold standard with regard to the decision to implant an ICD.
By contrast, EPS showed a 100% negative predictive value. Indeed, major events occurred only in subjects with positive EPS (14%), while no MAE occurred in patients with negative EPS. The latter data, which conflict with the results of other authors, may be simply explained by the fact that all our patients underwent an aggressive protocol.
In any case, despite the limit of low positive predictive values, our data support the usefulness of EPS in evaluating risk in subjects with the type 1 Brugada pattern, as proposed by the Brugada brothers13,14 and others.18 In particular, it can help to identify subjects at low risk, i.e. those who really do have a negative EPS. This information is lacking in patients who do not undergo EPS; in our study, 5.3% of these patients suffered MAE.
Considering that subjects with the Brugada type 1 ECG pattern may have different risk factors, each of which, however, when considered singly, has a low predictive value, we decided to evaluate the usefulness of a multiparametric, clinical, and electrophysiologic approach. In this way, we identified different populations of patients at increasing risk, in whom multiple clinical risk factors were present: basal type 1 ECG, family history of SD, and syncope.
On combining two or more clinical risk factors, an increasing risk was observed (C-statistic 0.66–0.77), the combination best able to predict MAE being a spontaneous type 1 ECG pattern, family history of SD, and syncope (C-statistics 0.77; 95% CI: 0.71–0.82). A positive EPS increased the ability of clinical risk factors to predict outcome (Δ C-statistic 0.11–0.21).
In the group of 245 patients who underwent EPS, the combination best able to predict major events was that of syncope, basal type 1 ECG, family history of SD, and positive EPS (C-statistic 0.87; 95% CI: 0.82–0.90).
On analysing Kaplan–Meier curves plotted on the entire population, with spontaneous or drug-induced type 1 pattern, all events were seen to have occurred in subjects who had at least two of the main risk factors (family history of SD, syncope or EPS+), while no events occurred in those without or with only one risk factor.
In other words, in this study, no subject without a family history of SD, without syncope, and with negative EPS suffered events. Furthermore, no patient with only one risk factor had events. This means that, when considered individually, familial SD, syncope, and positive EPS did not predict the occurrence of events.
Events occurred only in patients with spontaneous or drug-induced type 1 pattern in whom two or three of the factors were present (i.e. syncope + positive EPS, familial SD + syncope, familial SD + positive EPS, or all three together). In subjects with spontaneous type 1 ECG pattern and two or more risk factors, the risk was about 30%. In those with drug-induced type 1 ECG, the risk was very low (<2%) and was confined to subjects with two risk factors. This latter finding suggests a limited clinical value of the drug test when Brugada syndrome is only suspected (type II or III ECG) in the absence of symptoms and of a family history of SD.
Study limitations
This prospective study assembled two similar prospective studies performed by two groups of centres. One group employed protocol A; the other employed protocol B. The two protocols were not identical, but both were aggressive. Therefore, they were judged comparable. The results, which showed 38 and 39% of positive EPS with the two protocols, respectively, confirm that this was indeed the case.
The choice of performing or not performing EPS, after informed consent had been given, depended on the decision of each single patient. A higher proportion of patients who underwent EPS had syncope and a family history of SD. These characteristics probably influenced the individual decision to undergo EPS. During follow-up, major events occurred in 4/75 (5.3%) patients who did not undergo EPS and in 13/245 (5.3%) who did. As there is no difference between these percentages, it seems that the differences between these two populations did not influence the outcome.
The events evaluated during follow-up (MAE) included SD and ICD-recorded fast VT/VF which were converted by means of shock. Sustained VT/VF interrupted by shock is only a surrogate of SD. Indeed, we cannot claim that patients in whom sustained VT/VF was interrupted by ICD would have died suddenly in the absence of the device. On the other hand, as an ICD was implanted in about one-third of cases, we cannot exclude the possibility that the remaining two-thirds of patients had asymptomatic, self-terminating VT/VF. Notably, patients with ICD more frequently had clinical risk factors, particularly positive EPS.
Conclusions
Risk stratification in subjects with type 1 Brugada ECG pattern is a complex problem. In our study, we analysed several risk factors, which, however, when considered singly, displayed a low positive predictive value: basal type 1 pattern, syncope, familial SD, and positive EPS. We therefore propose a multiparametric (clinical and electrophysiologic) approach which helps to identify populations at higher risk.
On the basis of our data, subjects at higher risk are those with a basal type 1 ECG pattern who have at least two of the following risk factors: syncope, family history of SD, and positive EPS. Even in the presence of a basal type 1 ECG, no single risk factor, including EPS, is able to identify subjects at the highest risk. Electrophysiologic study may be useful when evaluated together with other clinical risk factors. A positive EPS together with other risk factors helps in deciding on ICD implantation. A negative EPS (using an aggressive protocol) can help to avoid ICD implantation. Patients with a drug-induced type 1 ECG have a very low risk; in the absence of other risk factors, EPS is of scant usefulness.
Our conclusions support the suggestions of the second consensus conference by Antzelevitch et al. published in 2005.8
Funding
Funding to pay the Open Access publication charges for this article was provided by ‘Amici del Cuore’ from Conegliano-Vittorio Veneto (Treviso) and IRCAB Foundation from Udine.
Conflict of interest: none declared.
References
- 1.Brugada P, Brugada J. Right bundle branch block, persistent ST-segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. J Am Coll Cardiol. 1992;20:1391–1396. doi: 10.1016/0735-1097(92)90253-j. [DOI] [PubMed] [Google Scholar]
- 2.Brugada J, Brugada R, Brugada P. Right bundle-branch block and ST-segment elevation in leads V1 through V3. A marker for sudden death in patients without demonstrable structural heart disease. Circulation. 1998;97:457–460. doi: 10.1161/01.cir.97.5.457. [DOI] [PubMed] [Google Scholar]
- 3.Proclemer A, Facchin D, Feruglio A, Nucifora R. Fibrillazione ventricolare recidivante, blocco di branca destra, persistente sopraslivellamento del tratto ST in V1-V3: una nuova sindrome aritmica? G Ital Cardiol. 1993;23:1211–1218. [PubMed] [Google Scholar]
- 4.Martini B, Nava A, Thiene G, Buja GF, Canciani B, Scognamiglio R, Daliento L, Dalla Volta S. Ventricular fibrillation without apparent heart disease: description of six cases. Am Heart J. 1989;118:1203–1209. doi: 10.1016/0002-8703(89)90011-2. [DOI] [PubMed] [Google Scholar]
- 5.Corrado D, Basso C, Buja G, Nava A, Rossi L, Thiene G. Right bundle branch block, right precordial ST-segment elevation, and sudden death in young people. Circulation. 2001;103:710. doi: 10.1161/01.cir.103.5.710. [DOI] [PubMed] [Google Scholar]
- 6.Wilde AA, Antzelevitch C, Borggrefe M, Brugada J, Brugada R, Brugada P, Corrado D, Hauer RN, Kass RS, Nademanee K, Priori SG, Towbin JA. Proposed diagnostic criteria for the Brugada syndrome. Consensus report. Circulation. 2002;106:2514–2519. doi: 10.1161/01.cir.0000034169.45752.4a. [DOI] [PubMed] [Google Scholar]
- 7.Wilde AA, Antzelevitch C, Borggrefe M, Brugada J, Brugada R, Brugada P, Corrado D, Hauer RN, Kass RS, Nademanee K, Priori SG, Towbin JA. Proposed diagnostic criteria for the Brugada syndrome. Study Group on the Molecular Basis of Arrhythmias of the European Society of Cardiology. Eur Heart J. 2002;23:1648–1654. doi: 10.1053/euhj.2002.3382. [DOI] [PubMed] [Google Scholar]
- 8.Antzelevitch C, Brugada P, Borggrefe M, Brugada J, Brugada R, Corrado D, Gussak I, LeMarec H, Nademanee K, Perez Riera AR, Shimizu W, Schulze-Bahr E, Tan H, Wilde A. Brugada sindrome. Report of the second consensus conference. Circulation. 2005;111:659–670. doi: 10.1161/01.CIR.0000152479.54298.51. [DOI] [PubMed] [Google Scholar]
- 9.Gussak I, Antzelevitch C, Bjerregaard P, Towbin JA, Chaitman BR. The Brugada sindrome: clinical, electrophysiologic and genetic aspects. J Am Coll Cardiol. 1999;33:5–15. doi: 10.1016/s0735-1097(98)00528-2. [DOI] [PubMed] [Google Scholar]
- 10.Brugada P, Benito B, Brugada R, Brugada J. Brugada syndrome: update 2009. Hellenic J Cardiol. 2009;50:352–372. [PubMed] [Google Scholar]
- 11.Fowler SJ, Priori SG. Clinical spectrum of patients with a Brugada ECG. Curr Opin Cardiol. 2008;24:74–81. doi: 10.1097/hco.0b013e32831cb920. [DOI] [PubMed] [Google Scholar]
- 12.Zipes DP, Camm JA, Borggrefe M, Buxton AE, Chaitman B, Fromer M, Gregoratos G, Klein G, Moss AJ, Myerburg RJ, Priori SG, Quinones MA, Roden DM, Silka MJ, Tracy C, Blanc JJ, Budaj A, Dean V, Deckers JW, Despres C, Dickstein K, Lekakis J, McGregor K, Metra M, Morais J, Osterspey A, Tamargo JL, Zamorano JL, Smith SC, Jacobs AK, Adams CD, Antman EM, Anderson JL, Hunt SA, Halperin JL, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhytmias and the prevention of sudden cardiac death. A report of the American College of Cardiology/American Heart Association Task Force and the Europe Society of Cardiology Committee for Practice Guidelines developed in collaboration with European Heart Rhythm Association and The Heart Rhythm Society. Europace. 2006;8:746–837. doi: 10.1093/europace/eul108. [DOI] [PubMed] [Google Scholar]
- 13.Brugada J, Brugada R, Brugada P. Determinants of sudden death in individuals with the electrocardiographic pattern of Brugada syndrome and no previous cardiac arrest. Circulation. 2003;108:3092–3096. doi: 10.1161/01.CIR.0000104568.13957.4F. [DOI] [PubMed] [Google Scholar]
- 14.Brugada P, Brugada R, Mont L, Rivero M, Geelen P, Brugada J. Natural history of Brugada sindrome: the prognostic value of programmed electrical stimulation of the heart. J Cardiovasc Electrophysiol. 2003;14:455–457. doi: 10.1046/j.1540-8167.2003.02517.x. [DOI] [PubMed] [Google Scholar]
- 15.Priori SG, Napolitano C, Gasparini M, Pappone C, Della Bella P, Giordano U, Bloise R, Giustetto C, De Nardis R, Grillo M, Ronchetti E, Faggiano G, Nastoli J. Natural history of Brugada sindrome. Insight for risk stratification and management. Circulation. 2002;105:1342–1347. doi: 10.1161/hc1102.105288. [DOI] [PubMed] [Google Scholar]
- 16.Eckardt L, Probst V, Smits JP, Bahr ES, Wolpert C, Schimpf R, Wichter T, Boisseau P, Heinecke A, Breithardt G, Borggrefe M, LeMarec H, Böcker D, Wilde AA. Long-term prognosis of individuals with right precordial ST-segment—elevation Brugada syndrome. Circulation. 2005;111:257–263. doi: 10.1161/01.CIR.0000153267.21278.8D. [DOI] [PubMed] [Google Scholar]
- 17.Brugada P, Brugada R, Brugada J, Priori S-G, Napolitano C. Should patients with an asymptomatic Brugada electrocardiogram undergo pharmacological and electrophysiological testing? Circulation. 2005;112:279–292. doi: 10.1161/CIRCULATIONAHA.104.485326. [DOI] [PubMed] [Google Scholar]
- 18.Giustetto C, Drago S, Demarchi PG, Dalmasso P, Bianchi F, Masi AS, Carvalho P, Occhetta E, Rossetti G, Riccardi R, Bertona R, Gaita F. Risk stratification of the patients with Brugada type electrocardiogram: a community-based prospective study. Europace. 2009;11:507–513. doi: 10.1093/europace/eup006. [DOI] [PubMed] [Google Scholar]
- 19.Probst V, Veltmann C, Eckardt L, Meregalli PG, Gaita F, Tan HL, Babuty D, Sacher F, Giustetto C, Schulze-Bahr E, Borggrefe M, Haissaguerre M, Mabo P, Le Marec H, Wolpert C, Wilde AA. Long-term prognosis of patients diagnosed with Brugada syndrome. Results from the FINGER Brugada Syndrome Registry. Circulation. 2010;121:635–643. doi: 10.1161/CIRCULATIONAHA.109.887026. [DOI] [PubMed] [Google Scholar]
- 20.Tsuji H, Sato T, Morisaki K, Iwasaka T. Prognosis of subjects with Brugada-type electrocardiogram in a population of middle-aged Japanese diagnosed during a health examination. Am J Cardiol. 2008;102:584–587. doi: 10.1016/j.amjcard.2008.04.066. [DOI] [PubMed] [Google Scholar]
- 21.Benito B, Sarkozy A, Mont L, Henkens S, Berruezo A, Tamborero D, Arzamendi D, Berne P, Brugada R, Brugada P, Brugada J. Gender differences in clinical manifestations of Brugada syndrome. J Am Coll Cardiol. 2008;52:1567–1573. doi: 10.1016/j.jacc.2008.07.052. [DOI] [PubMed] [Google Scholar]
- 22.Sidik NP, Quay NC, Loh FC, Chen LY. Prevalence of Brugada sign and syndrome in patients presenting with arrhythmic symptoms at a Heart Rhythm Clinic in Singapore. Europace. 2009;11:650–656. doi: 10.1093/europace/eup079. [DOI] [PubMed] [Google Scholar]
- 23.Sarkozy A, Boussy T, Kourgiannides G, Chierchia GB, Richter S, De Potter T, Geelen P, Wellens F, Spreeuwenberg MD, Brugada P. Long-term follow up of primary prophylactic implantable cardioverter-defibrillator therapy in Brugada syndrome. Eur Heart J. 2007;28:334–344. doi: 10.1093/eurheartj/ehl450. [DOI] [PubMed] [Google Scholar]
- 24.Sacher F, Probst V, Iesaka Y, Jacon P, Laborderie J, Mizon-Gérard F, Mabo P, Reuter S, Lamaison D, Takahashi Y, O'Neill MD, Garrigue S, Pierre B, Jaïs P, Pasquié J-L, Hocini M, Salvador-Mazenq M, Nogami A, Amiel A, Defaye P, Bordachar P, Boveda S, Maury P, Klug D, Babuty D, Haïssaguerre M, Mansourati J, Clémenty J, Le Marec H. Outcome after implantation of a cardioverter-defibrillator in patients with Brugada syndrome: a multicenter study. Circulation. 2006;114:2317–2324. doi: 10.1161/CIRCULATIONAHA.106.628537. [DOI] [PubMed] [Google Scholar]
- 25.Gehi AK, Duong TD, Metz LD, Gomes JA, Mehta D. Risk stratification of individuals with the Brugada electrocardiogram: a meta-analysis. J Cardiovasc Electrophysiol. 2006;17:577–583. doi: 10.1111/j.1540-8167.2006.00455.x. [DOI] [PubMed] [Google Scholar]
- 26.Paul M, Gerss J, Schulze-Bahr E, Wichter T, Vahlhaus C, Wilde AA, Breithardt G, Eckardt L. Role of programmed ventricular stimulation in patients with Brugada syndrome: a meta-analysis of worldwide published data. Eur Heart J. 2007;28:2126–2133. doi: 10.1093/eurheartj/ehm116. [DOI] [PubMed] [Google Scholar]
- 27.Gasparini M, Priori S, Mantica M, Coltorti F, Napoletano C, Galimberti P, Bloise R, Cerotti C. Programmed electrical stimulation in Brugada sindrome: how reproducible are the results? J Cardiovasc Electrophysiol. 2002;13:880–887. doi: 10.1046/j.1540-8167.2002.00880.x. [DOI] [PubMed] [Google Scholar]