Abstract
Background: The increasing trend in body mass index (BMI) and overweight in rapidly developing economies is well recognized.
Objective: We assessed the association between socioeconomic status and BMI and overweight in low- to middle-income countries.
Design: We conducted a cross-sectional analysis of nationally representative samples of 538,140 women aged 15–49 y drawn from 54 Demographic and Health Surveys conducted between 1994 and 2008. BMI, calculated as weight in kilograms divided by height squared in meters, was specified as the outcome, and a BMI (in kg/m2) of ≥25 was additionally specified to model the likelihood of being overweight. Household wealth and education were included as markers of individual socioeconomic status, and per capita Gross Domestic Product (pcGDP) was included as a marker of country-level economic development.
Results: Globally, a one-quartile increase in wealth was associated with a 0.54 increase in BMI (95% CI: 0.50, 0.64) and a 33% increase in overweight (95% CI: 26%, 41%) in adjusted models. Although the strength of this association varied across countries, the association between wealth and BMI and overweight was positive in 96% (52 of 54) of the countries. Similar patterns were observed in urban and rural areas, although SES gradients tended to be greater in urban areas. There was a positive association between pcGDP and BMI or overweight, with only weak evidence of an interaction between pcGDP and wealth.
Conclusion: Higher BMI and overweight remain concentrated in higher socioeconomic groups, even though increasing BMI and overweight prevalence are important global public concerns.
See corresponding editorial on page 232
INTRODUCTION
Weights of individuals in developing countries have shown an upward shift with corresponding increases in prevalence of overweight and obesity in developing countries (1–5). These overall assessments, however, mask the substantial variation within and between developing countries, especially along socioeconomic dimensions (2). In several developing countries (6–11), weight status is positively associated with socioeconomic status (SES), which is in stark contrast to the patterns observed in developed countries (12–16). It has been hypothesized that the association between SES and weight within countries is contingent on the country's overall level of economic development, with the prevalence of overweight shifting from high to low socioeconomic groups in countries at higher levels of economic development (17–19). A review of 333 studies showed a gradual reversal of the social gradient in weight, in which the proportion of positive associations between SES and weight increased (and the proportion of negative associations decreased) when moving from countries ranked high to medium to low in development (20). However, the review also showed that for women in low- and middle-income countries, a positive association between SES and weight was the most common pattern. Furthermore, in a sample of 41 countries, obesity was observed to be most prevalent in the richest quintile, although this was based on self-reported height and weight data (21).
Despite the increasing prevalence of overweight in developing countries (22), and the policy relevance of ascertaining who is more likely to be burdened with the problem of overweight, there is limited systematic evidence on the association between SES and weight in developing countries. Two previous studies (18, 19) that partially used the same data as this article provide an important baseline assessment of the association between obesity and overweight, SES, and a country's level of economic development. However, the data in these studies were from considerably fewer countries than the present study and were from before 2000. Moreover, the previous analyses used educational attainment as the only indicator of SES.
By using the largest available, comparable, and most recent sample of adult women in the reproductive age group from 54 low- to middle-income countries with objective measurements of height and weight, we provide an update on the associations between SES and body mass index (BMI) and overweight and their potential modification by country-level economic development. In addition, the present analyses include household wealth as a dimension of SES along with individual education, focus on the entire nutritional spectrum with the use of BMI, and assess geographic heterogeneity in the SES and BMI and overweight association.
METHODS
Data sources
The data for this study came from Demographic and Health Surveys (DHS) conducted in 54 countries between 1994 and 2008 (Table 1) (23). The DHS are household sample surveys measuring indicators of population, health, and nutrition, with special emphasis on maternal and child health (24). The target population in most DHS was all women (or in some cases ever-married women) of reproductive age (15–49 y). Due to coverage, comparability, and data quality, the DHS is an important data source for studying population health across developing countries (25–27). DHS uses extensive interviewer training, standardized measurement tools and techniques, an identical core questionnaire, and instrument pretesting to ensure standardization and comparability across diverse sites and time (28) (see www.measuredhs.com/pubs/pdf/DHSG4/Recode4DHS.pdf). The DHS uses a multistage stratified design with probabilistic sampling with each elementary unit having a defined probability of selection (29). Every survey was stratified by urban and rural status and additionally by country-specific geographic or administrative regions. Detailed sampling plans are available from survey final reports at www.measuredhs.com/pubs/search/search_results.cfm?Type=5&srchTp=type&newSrch=1. Each survey by country and year, along with per capita Gross Domestic Product (pcGDP) for the year corresponding to the survey, sample sizes, and distribution of BMI and overweight prevalence are described in Table 1. Supplementary Table 1 under “Supplemental data” in the online issue shows each survey by country and year along with number of primary sampling units (PSUs), sample sizes, response rates, and anthropometric (height and weight) measurement protocol.
TABLE 1.
Per capita Gross Domestic Product (GDP), survey year, sample size, BMI, and percentage overweight for women in 54 low- and middle-income countries1
| Country | Per capita GDP | Survey year | Sample size | BMI | Percentage overweight |
| kg/m2 | % | ||||
| Armenia | 3903.5 | 2005 | 6301 | 25.2 ± 5.32 | 43.3 ± 49.6 |
| Azerbaijan | 6120.9 | 2006 | 8147 | 25.2 ± 5.2 | 45.4 ± 49.8 |
| Bangladesh | 1314.9 | 2007 | 10,839 | 20.9 ± 3.7 | 13.8 ± 34.4 |
| Benin | 1307.9 | 2006 | 16,712 | 22.5 ± 4.1 | 18.1 ± 38.5 |
| Bolivia | 3302.8 | 2003 | 17,278 | 25.5 ± 4.6 | 46.7 ± 49.9 |
| Brazil | 6628.8 | 1996 | 3449 | 23.9 ± 4.3 | 33.7 ± 47.3 |
| Burkina Faso | 1025.8 | 2003 | 12,255 | 20.9 ± 3.4 | 8.6 ± 28.0 |
| Cambodia | 1456.7 | 2005 | 8353 | 21.1 ± 2.7 | 7.3 ± 26.0 |
| Cameroon | 1943.6 | 2004 | 5180 | 21.0 ± 3.1 | 9.2 ± 29.0 |
| CAR | 591.3 | 1994–1995 | 2369 | 23.6 ± 4.2 | 29.3 ± 45.5 |
| Chad | 1513.4 | 2004 | 3582 | 21.2 ± 3.5 | 11.3 ± 31.7 |
| Colombia | 6702.7 | 2005 | 35,452 | 24.8 ± 4.8 | 42.2 ± 49.4 |
| Comoros | 886.3 | 1996 | 888 | 22.6 ± 3.8 | 21.7 ± 41.3 |
| Congo (Brazaville) | 3566.1 | 2005 | 6863 | 22.8 ± 4.3 | 24.7 ± 43.1 |
| Congo (DRC) | 312.5 | 2007 | 4726 | 21.6 ± 3.6 | 12.9 ± 33.5 |
| Cote d'Ivoire | 1662.0 | 1998–1999 | 3011 | 23.0 ± 4.1 | 23.5 ± 42.4 |
| Dominican Republic | 4259.5 | 1996 | 7943 | 24.3 ± 4.8 | 37.5 ± 48.4 |
| Egypt | 5896.7 | 2008 | 16,409 | 28.7 ± 5.4 | 75.2 ± 43.2 |
| Ethiopia | 434.5 | 2005 | 6645 | 20.4 ± 3.1 | 6.3 ± 24.3 |
| Gabon | 12,131.5 | 2000 | 2795 | 23.2 ± 3.9 | 25.2 ± 43.4 |
| Ghana | 1518.5 | 2008 | 4808 | 23.4 ± 4.7 | 28.1 ± 45.0 |
| Guatemala | 3764.9 | 1998–1999 | 2740 | 24.8 ± 4.2 | 40.8 ± 49.1 |
| Guinea | 939.7 | 2005 | 3962 | 21.8 ± 3.4 | 13.5 ± 34.1 |
| Haiti | 1196.3 | 2005–2006 | 5253 | 22.3 ± 4.2 | 20.6 ± 40.5 |
| Honduras | 3555.5 | 2005–2006 | 19,250 | 25.2 ± 5.1 | 43.9 ± 49.6 |
| India | 2085.4 | 2005–2006 | 118,760 | 21.0 ± 4.1 | 15.1 ± 35.8 |
| Jordan | 4302.8 | 2007 | 5200 | 28.3 ± 5.8 | 68.9 ± 46.3 |
| Kazakhstan | 4289.3 | 1999 | 2283 | 23.9 ± 5.1 | 31.2 ± 46.4 |
| Kenya | 1337.2 | 2003 | 7707 | 22.8 ± 4.3 | 24.2 ± 42.8 |
| Kyrgyz Republic | 1190.3 | 1997 | 3783 | 23.3 ± 4.3 | 26.5 ± 44.1 |
| Lesotho | 1003.7 | 2004 | 3413 | 25.0 ± 5.3 | 41.2 ± 49.2 |
| Liberia | 333.6 | 2007 | 6915 | 22.6 ± 4.1 | 21.0 ± 40.7 |
| Madagascar | 757.2 | 2003–2004 | 7808 | 21.3 ± 3.2 | 10.4 ± 30.5 |
| Malawi | 643.8 | 2004 | 11,130 | 22.1 ± 3.3 | 13.9 ± 34.6 |
| Mali | 1034.6 | 2006 | 14,275 | 22.3 ± 4.1 | 18.6 ± 38.9 |
| Moldova | 2358.5 | 2005 | 7241 | 25.1 ± 5.7 | 41.1 ± 49.2 |
| Morocco | 3223.6 | 2003–2004 | 16,643 | 24.2 ± 4.5 | 36.0 ± 48.0 |
| Mozambique | 626.3 | 2003 | 11,706 | 22.3 ± 3.6 | 16.1 ± 36.8 |
| Namibia | 6009.1 | 2006–2007 | 9534 | 23.2 ± 5.5 | 27.9 ± 44.9 |
| Nepal | 1024.4 | 2006 | 10,739 | 20.6 ± 3.0 | 7.9 ± 27.0 |
| Nicaragua | 2175.2 | 2001 | 12,580 | 25.5 ± 4.9 | 46.5 ± 49.9 |
| Niger | 661.4 | 2006 | 4542 | 21.9 ± 4.0 | 17.3 ± 37.8 |
| Nigeria | 1597.9 | 2003 | 7442 | 22.4 ± 4.2 | 19.8 ± 39.9 |
| Peru | 5624.0 | 2004 | 5915 | 25.2 ± 4.2 | 45.1 ± 49.8 |
| Rwanda | 855.7 | 2005 | 5642 | 22.0 ± 2.9 | 12.9 ± 33.5 |
| Senegal | 1565.5 | 2005 | 4578 | 22.2 ± 4.4 | 20.1 ± 40.1 |
| Swaziland | 5104.0 | 2006–2007 | 4858 | 26.4 ± 5.8 | 50.7 ± 50.0 |
| Tanzania | 1005.0 | 2004–2005 | 10,233 | 22.3 ± 3.9 | 18.0 ± 38.4 |
| Togo | 695.8 | 1998 | 3717 | 21.6 ± 3.1 | 10.5 ± 30.6 |
| Turkey | 8705.2 | 2003 | 3288 | 26.7 ± 5.0 | 58.2 ± 49.3 |
| Uganda | 991.0 | 2006 | 2859 | 22.0 ± 3.6 | 15.5 ± 36.2 |
| Uzbekistan | 1235.4 | 1996 | 4376 | 22.9 ± 4.0 | 23.5 ± 42.4 |
| Zambia | 1379.5 | 2007 | 7045 | 22.6 ± 3.9 | 19.6 ± 39.7 |
| Zimbabwe | 392.0 | 2005–2006 | 8718 | 23.1 ± 4.1 | 25.2 ± 43.4 |
| Total | 2031.4 | 538,140 | 23.0 ± 4.8 | 26.5 ± 44.1 |
Percentage overweight represents the number of women with a BMI (in kg/m2) ≥25 divided by the total number of women and then multiplied by 100. The per capita GDP is for the year in which the individual survey was held. CAR, Central African Republic; DRC, Democratic Republic of Congo.
Mean ± SD (all such values).
Study population and sample size
The study population comprises women (n = 688,838) aged 15–49 y. There were 112,225 women (16.3% of the sample) for whom height or weight was intentionally not measured (see Supplementary Table 1 for anthropometric measurement protocol by survey). Among those for whom height or weight should have been measured, 37,023 (6.4%) did not have a height or weight measure in the data, and a further 1770 women (0.3%) had biologically implausible height (<100 cm or >200 cm) or weight (<20 kg or >150 kg). Twenty-eight observations (<1%) were missing data on covariates. The final analytic sample was 538,140 women surveyed and measured between 1994 and 2008 in 54 countries.
Outcome
BMI, calculated as weight in kilograms divided by height squared in meters, was used to assess weight status and was our primary outcome. Trained investigators weighed each woman by using a solar-powered scale with an accuracy of ±100 g and measured each woman by using an adjustable board calibrated in millimeters, and theoretically accurate to 1 mm (28). In contrast to previous assessments that have focused exclusively on obesity or overweight, we chose BMI as our primary focus because it captures the entire nutritional spectrum in a population as opposed to an exclusive focus on the high-risk group. We also considered the likelihood of being overweight as a secondary outcome using the BMI (in kg/m2) cutoff of ≥25 (30), which provides a policy relevant measure from the prevention standpoint.
Independent variables
Household wealth, individual education, and country-level wealth were the key independent variables of interest. Age and place of residence were included as individual covariates (Table 2). Household wealth was defined in terms of ownership of material possessions (31), with each woman assigned a wealth score on the basis of a combination of different household characteristics that were weighted according to a factor analysis procedure. We used the constructed wealth index measure provided by the DHS that is calculated by developing z scores for each indicator variable and conducting a principal components analysis on these z scores. For each household, the values of the indicator variables were multiplied by the factor loadings and summed to produce a standardized household index value with a mean of 0 and an SD of 1. This standardized score was then divided into quintiles for each country (32–34). Education was specified as a woman having no schooling, having completed primary schooling, or having completed secondary or higher schooling. Place of residence was defined in terms of whether the household was located in a census-defined urban or rural area. Country-level wealth was measured as pcGDP on the basis of purchasing-power-parity, measured in current international dollars for each country for the year corresponding to the survey (35).
TABLE 2.
Frequency distribution of the sample of women and BMI and proportion overweight by categories of independent variables across 54 low- and middle-income countries1
| Frequency | BMI | Proportion overweight | |
| kg/m2 | |||
| Wealth | |||
| Bottom quartile | 136,826 | 21.80 ± 4.102 | 0.17 ± 0.40 |
| Second quartile | 135,636 | 22.49 ± 4.49 | 0.22 ± 0.42 |
| Third quartile | 134,052 | 23.29 ± 4.84 | 0.29 ± 0.45 |
| Top quartile | 131,626 | 24.34 ± 5.12 | 0.38 ± 0.48 |
| Schooling | |||
| None | 152,987 | 21.80 ± 4.70 | 0.17 ± 0.40 |
| Primary | 151,562 | 23.23 ± 4.69 | 0.28 ± 0.45 |
| Secondary or higher | 233,591 | 23.55 ± 4.97 | 0.32 ± 0.47 |
| Age | |||
| 15–19 y | 104,050 | 21.00 ± 3.30 | 0.10 ± 0.30 |
| 20–29 y | 191,390 | 22.41 ± 4.07 | 0.21 ± 0.41 |
| 30–39 y | 142,632 | 23.86 ± 5.05 | 0.35 ± 0.48 |
| 40–49 y | 100,068 | 24.87 ± 5.73 | 0.43 ± 0.50 |
| Residence | |||
| Rural | 291,057 | 22.10 ± 4.30 | 0.19 ± 0.40 |
| Urban | 247,083 | 23.95 ± 5.08 | 0.35 ± 0.48 |
| Total | 538,140 | 22.30 ± 4.75 | 0.27 ± 0.44 |
Proportion overweight represents the number of women with a BMI (in kg/m2) ≥25 divided by the total number of women.
Mean ± SD (all such values).
Analysis
Individual country files were created ensuring consistency of variable definitions across countries. These individual files were then concatenated, which led to a multilevel data structure of women at level 1 who were nested within PSUs at level 2, which were nested within countries at level 3 (36). We used multilevel linear regression to model the variation in BMI (y) for a woman i in PSU j in country k (37). We estimated the following model:
where β0 represents the mean BMI for the reference groups (ie, rural women aged <20 y with no schooling and in the bottom wealth quartile) across all countries; and BXijk represents a vector of regression coefficients associated with variables representing household wealth quartiles, schooling categories, age, and urban residence. The terms inside the brackets represent random effects associated with country k (v0k), PSU j (u0jk), and a residual term for every woman i (e0ijk). Making identical and independent distribution assumptions, we estimated a variance at level 1 ( : between-individual), level 2 (
: between-individual), level 2 ( : between-PSU), and level 3 (
: between-PSU), and level 3 (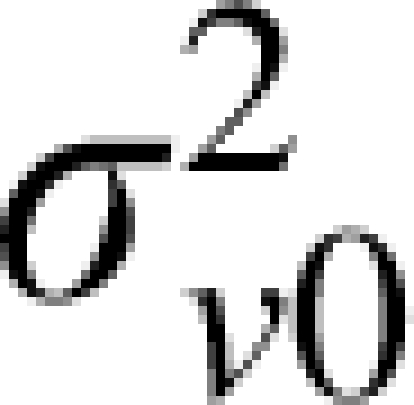 : between-country) in BMI. The multilevel modeling approach allowed the decomposition of variation in BMI attributable to PSU and countries and provided a precision-weighted estimate for country-specific predictions (37). We extended the above model to also consider random coefficients at the country level for the regression coefficients associated with household wealth. We further extended the model to then include country-level wealth and an interaction between country-level wealth and household wealth. We also estimated multilevel logistic regression with similar structure to model the likelihood of being overweight (37). Models were estimated by using MLwiN 2.20 (38).
: between-country) in BMI. The multilevel modeling approach allowed the decomposition of variation in BMI attributable to PSU and countries and provided a precision-weighted estimate for country-specific predictions (37). We extended the above model to also consider random coefficients at the country level for the regression coefficients associated with household wealth. We further extended the model to then include country-level wealth and an interaction between country-level wealth and household wealth. We also estimated multilevel logistic regression with similar structure to model the likelihood of being overweight (37). Models were estimated by using MLwiN 2.20 (38).
Ethical review
The DHS data collection procedures were approved by the ORC Macro Institutional Review Board (Calverton, MD) as well as by the relevant body in each country that approves research studies on human subjects. Oral informed consent for the interview/survey was obtained from respondents by interviewers. The study was reviewed by Harvard School of Public Health Institutional Review Board and was considered exempt from full review because the study was based on an anonymous public use data set with no identifiable information on the survey participants.
RESULTS
The mean BMI across all 54 countries was 23.0 and varied between 20.4 in Ethiopia and 28.7 in Egypt (Table 1). The mean prevalence of overweight was 27%. Egypt had the highest fraction of overweight women (75%), whereas Ethiopia had the lowest burden of overweight (6%) (Table 1). In pooled samples, mean BMI and percentage overweight were consistently higher among women of higher SES (Table 2).
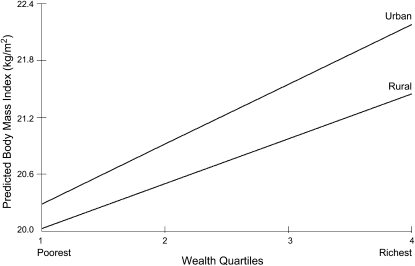
In mutually adjusted pooled models, BMI was positively associated with wealth quartiles; BMI in the top and third quartiles of household wealth was 1.82 (95% CI: 1.78, 1.86) and 1.07 (95% CI 1.03, 1.11) greater than those in the bottom quartile of household wealth, respectively (Table 3). Compared with those with no schooling, women with primary or secondary/higher schooling had 0.69 (95% CI 0.66, 0.72) and 0.47 (95% CI 0.43, 0.50) higher BMI, respectively. Similar patterns were observed for overweight; women in the top wealth quartile had an odds ratio of 2.34 (95% CI: 2.27, 2.41) compared with women in the bottom wealth quartile (Table 3). Likewise, women with secondary/higher schooling had an odds ratio of 1.27 (95% CI: 1.25, 1.30) compared with women with no schooling. The association between wealth quartiles and BMI and overweight was positive in urban and rural areas, with the wealth differentials appearing sharper in urban areas (Figure 1).
TABLE 3.
Unadjusted and mutually adjusted estimates of wealth quartiles, schooling, age, and place of residence on BMI and overweight accounting for within- and between-country variation for women across 54 low- and middle-income countries1
| BMI |
Overweight |
||||||||
| Unadjusted model |
Mutually adjusted model |
Unadjusted model |
Mutually adjusted model |
||||||
| n | β | 95% CI | β | 95% CI | OR | 95% CI | OR | 95% CI | |
| Wealth | |||||||||
| Bottom quartile (reference) | 136,826 | — | — | — | — | — | — | — | — |
| Second quartile | 135,636 | 0.56 | (0.53, 0.59) | 0.49 | (0.45, 0.52) | 1.34 | (1.31, 1.36) | 1.30 | (1.27, 1.32) |
| Third quartile | 134,052 | 1.27 | (1.23, 1.30) | 1.07 | (1.03, 1.11) | 1.85 | (1.82, 1.88) | 1.72 | (1.68, 1.77) |
| Top quartile | 131,626 | 2.16 | (2.12, 2.20) | 1.82 | (1.78, 1.86) | 2.61 | (2.56, 2.66) | 2.34 | (2.27, 2.41) |
| Education | |||||||||
| None (reference) | 152,987 | — | — | — | — | — | — | — | — |
| Primary | 151,562 | 0.23 | (0.20, 0.27) | 0.69 | (0.66, 0.72) | 1.19 | (1.16, 1.21) | 1.40 | (1.36, 1.40) |
| Secondary or higher | 233,591 | −0.06 | (−0.09, −0.02) | 0.47 | (0.43, 0.50) | 1.11 | (1.08, 1.13) | 1.27 | (1.25, 1.30) |
| Age | |||||||||
| 15–19 y (reference) | 104,050 | — | — | — | — | — | — | — | — |
| 20–29 y | 191,390 | 1.35 | (1.32, 1.38) | 1.39 | (1.36. 1.42) | 2.37 | (2.32, 2.44) | 2.45 | (2.39, 2.51) |
| 30–39 y | 142,632 | 2.76 | (2.73, 2.79) | 2.85 | (2.82, 2.88) | 4.57 | (4.48, 4.66) | 4.97 | (4.85, 5.10) |
| 40–49 y | 100,068 | 3.64 | (3.60, 3.67) | 3.76 | (3.72, 3.79) | 6.16 | (5.99, 6.30) | 6.96 | (6.75, 7.17) |
| Residence | |||||||||
| Rural (reference) | 291,057 | — | — | — | — | — | — | — | — |
| Urban | 247,083 | 1.34 | (1.30, 1.38) | 0.47 | (0.43, 0.51) | 1.79 | (1.75, 1.80) | 1.25 | (1.22, 1.32) |
Overweight represents women with a BMI (in kg/m2) ≥25. OR, odds ratio. The P value for the trend in wealth quartiles was significant, P < 0.0001. Statistical tests were based on a 2-tailed Wald test using chi-square distribution.
FIGURE 1.
Association between BMI and wealth quartiles by urban or rural area of residence for women across 54 low- and middle-income countries. Note: The interaction test was significant at P < 0.0001. The patterns were similar when we considered the likelihood of having a BMI (in kg/m2) ≥25 (overweight) as the outcome. Statistical tests were based on a 2-tailed Wald test using chi-square distribution.
Weight status varied substantially between countries even after accounting for within-country covariates and within-country geographic variation. In adjusted models, around a global mean BMI of 19.86, 95% of the countries had a mean within the range of 16.55 and 23.17 (see Supplementary Table 2 under “Supplemental data” in the online issue). Country-specific differences around the global mean BMI were considerable; Egypt, Jordan, Swaziland, Turkey, and Nicaragua were the top 5 countries with BMIs greater than the average, whereas in Bangladesh, Ethiopia, Cambodia, Nepal, and India, women had substantially lower BMIs (Supplementary Table 3 under “Supplemental data” in the online issue). Patterns were similar for overweight (Supplementary Table 2 and 3). The correlation in mean BMI and percentage overweight across countries was 0.89.
The association between BMI and wealth was positive in every country except in Moldova and Kazakhstan, and even the negative association observed in these 2 countries was not statistically insignificant (Table 4). However, the strength of the positive association varied considerably across countries. In 5 of the 54 countries (9%), a quartile change in wealth was associated with a change of >1 in BMI, and in 28 countries (52%) the change was ≥0.50 or ≤1. The odds ratio of being overweight for a quartile change in wealth also varied considerably (Table 4). Although in 69% of the countries (37 of 54) the 95% CI around the odds ratio did not include 1 with the estimates >1, in 3 countries (Moldova, Turkey, and Jordan) a quartile increase in wealth was associated with a lower odds ratio of being overweight. In 14 countries, no association was observed between wealth quartile and likelihood of being overweight (P < 0.05). However, it must be remembered that with greatly varying sample sizes the ability to detect robust differences varies considerably between countries. These overall country-specific patterns were also observed in urban and rural areas (Supplementary Table 4 under “Supplemental data” in the online issue); in 65% and 24% of the countries an odds ratio >1 was associated with being overweight for a quartile increase in wealth in urban and rural areas, respectively.
TABLE 4.
Change in BMI and the odds ratio (OR) of being overweight for a one-quartile increase in household wealth for women across 54 low- and middle-income countries1
| BMI |
Overweight |
||||
| Country | n | Wealth slope | 95% CI | Wealth OR | 95% CI |
| Moldova | 7241 | −0.38 | (−0.61, −0.15) | 0.79 | (0.68, 0.90) |
| Kazakhstan | 2283 | −0.17 | (−0.46, 0.11) | 0.95 | (0.80, 1.11) |
| Colombia | 35,452 | 0.01 | (−0.19, 0.20) | 0.90 | (0.79, 1.01) |
| Turkey | 3288 | 0.01 | (−0.23, 0.26) | 0.83 | (0.70, 0.96) |
| Armenia | 6301 | 0.05 | (−0.17, 0.28) | 0.91 | (0.79, 1.05) |
| Jordan | 5200 | 0.06 | (−0.17, 0.29) | 0.85 | (0.73, 0.97) |
| Kyrgyz Republic | 3783 | 0.11 | (−0.15, 0.37) | 1.08 | (0.92, 1.26) |
| CAR | 2369 | 0.15 | (−0.12, 0.42) | 1.30 | (1.09, 1.53) |
| Uzbekistan | 4376 | 0.16 | (−0.09, 0.42) | 1.14 | (0.97, 1.32) |
| Brazil | 3449 | 0.20 | (−0.05, 0.44) | 1.02 | (0.87, 1.18) |
| Bolivia | 17,278 | 0.22 | (0.01, 0.42) | 0.97 | (0.85, 1.10) |
| Peru | 5915 | 0.31 | (0.08, 0.55) | 1.36 | (1.17, 1.56) |
| Rwanda | 5842 | 0.31 | (0.09, 0.54) | 1.09 | (0.94, 1.26) |
| Morocco | 16,643 | 0.36 | (0.15, 0.58) | 1.14 | (1.00, 1.30) |
| Comoros | 888 | 0.40 | (0.06, 0.75) | 1.26 | (1.02, 1.54) |
| Azerbaijan | 8147 | 0.43 | (0.21, 0.66) | 1.38 | (1.21, 1.58) |
| Malawi | 11,130 | 0.43 | (0.23, 0.64) | 1.12 | (0.97, 1.28) |
| Dominican Republic | 7943 | 0.44 | (0.22, 0.66) | 1.13 | (0.98, 1.30) |
| Congo (DRC) | 4726 | 0.47 | (0.22, 0.72) | 1.44 | (1.23, 1.66) |
| Senegal | 4578 | 0.47 | (0.22, 0.71) | 1.44 | (1.24, 1.67) |
| Guinea | 3962 | 0.49 | (0.24, 0.73) | 1.52 | (1.30, 1.77) |
| Cambodia | 8353 | 0.50 | (0.28, 0.72) | 1.42 | (1.23, 1.62) |
| Nicaragua | 12,580 | 0.51 | (0.30, 0.72) | 1.11 | (0.97, 1.27) |
| Ethiopia | 6645 | 0.52 | (0.29, 0.75) | 1.49 | (1.27, 1.73) |
| Liberia | 6915 | 0.52 | (0.29, 0.75) | 1.47 | (1.26, 1.69) |
| Togo | 3717 | 0.52 | (0.26, 0.77) | 1.42 | (1.23, 1.63) |
| Nepal | 10,739 | 0.53 | (0.31, 0.74) | 1.47 | (1.27, 1.68) |
| Madagascar | 7808 | 0.54 | (0.31, 0.77) | 1.37 | (1.18, 1.57) |
| Mali | 14,275 | 0.55 | (0.34, 0.76) | 1.54 | (1.34, 1.76) |
| Chad | 3582 | 0.56 | (0.30, 0.82) | 1.53 | (1.30, 1.78) |
| Egypt | 16,409 | 0.57 | (0.37, 0.77) | 0.95 | (0.83, 1.08) |
| Burkina Faso | 12,255 | 0.58 | (0.36, 0.79) | 1.56 | (1.36, 1.78) |
| Cote d'Ivoire | 3811 | 0.66 | (0.39, 0.93) | 1.53 | (1.30, 1.80) |
| Gabon | 2795 | 0.69 | (0.42, 0.96) | 1.53 | (1.32, 1.75) |
| Nigeria | 7442 | 0.69 | (0.46, 0.92) | 1.52 | (1.29, 1.79) |
| Guatemala | 2740 | 0.71 | (0.44, 0.98) | 1.65 | (1.44, 1.89) |
| Mozambique | 11,706 | 0.71 | (0.50, 0.93) | 1.34 | (1.13, 1.57) |
| Tanzania | 4858 | 0.71 | (0.50, 0.93) | 1.64 | (1.43, 1.87) |
| Congo (Brazaville) | 6863 | 0.73 | (0.50, 0.96) | 1.46 | (1.26, 1.68) |
| Zimbabwe | 8718 | 0.76 | (0.54, 0.99) | 1.53 | (1.32, 1.75) |
| Benin | 16,712 | 0.77 | (0.56, 0.97) | 1.59 | (1.39, 1.81) |
| Honduras | 19,250 | 0.79 | (0.59, 1.00) | 1.34 | (1.18, 1.52) |
| Zambia | 7045 | 0.80 | (0.57, 1.03) | 1.64 | (1.41, 1.89) |
| Niger | 4542 | 0.81 | (0.57, 1.06) | 1.82 | (1.56, 2.12) |
| Swaziland | 4858 | 0.85 | (0.62, 1.09) | 1.09 | (0.94, 1.26) |
| Cameroon | 5180 | 0.89 | (0.65, 1.13) | 1.63 | (1.40, 1.88) |
| Haiti | 5253 | 0.89 | (0.65, 1.13) | 1.64 | (1.41, 1.89) |
| Lesotho | 3413 | 0.98 | (0.73, 1.23) | 1.37 | (1.17, 1.60) |
| India | 118,760 | 1.00 | (0.81, 1.19) | 1.66 | (1.47, 1.88) |
| Bangladesh | 10,839 | 1.01 | (0.79, 1.22) | 1.68 | (1.47, 1.92) |
| Uganda | 2859 | 1.04 | (0.79, 1.30) | 1.70 | (1.44, 2.00) |
| Kenya | 7707 | 1.05 | (0.82, 1.28) | 1.72 | (1.48, 1.97) |
| Ghana | 4808 | 1.12 | (0.88, 1.36) | 1.86 | (1.60, 2.16) |
| Namibia | 9534 | 1.20 | (0.98, 1.42) | 1.66 | (1.45, 1.90) |
Overweight represents women with a BMI (in kg/m2) ≥25. CAR, Central African Republic; DRC, Democratic Republic of Congo. Statistical tests were based on a 2-tailed Wald test using chi-square distribution.
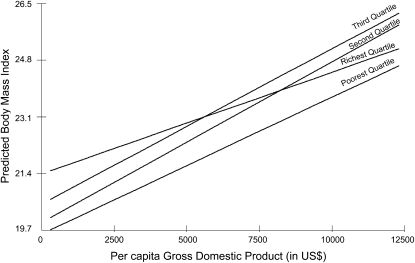
In adjusted models, country pcGDP was positively associated with BMI; a $1000 increase in pcGDP increased BMI by 0.4 (95% CI: 0.2, 0.5) and the odds ratio of being overweight by 1.13 (95% CI: 1.06, 1.20). There was an apparent interaction between wealth, pcGDP, and BMI/overweight (P < 0.0001). Although there was a positive association between wealth and pcGDP across all wealth categories, for the richest quartile the association between pcGDP and BMI/overweight was shallower in comparison with the poorer 3 wealth quartiles (Figure 2). Only in countries with a pcGDP >≈$5500 does the wealth gradient in BMI/overweight seem to be less marked or where the richest quartile has lower levels of BMI/overweight than does the poorest quartile (P = 0.062). It should be noted that in our sample only 8 of the 54 countries had a pcGDP of >≈$5500. Furthermore, the second- and third-richest quartiles were consistently more likely to be overweight than the poorest quartile across the whole spectrum of pcGDP.
FIGURE 2.
Association between BMI and per capita Gross Domestic Product by wealth quartiles for women across 54 low- and middle-income countries. Note: P values for the interaction test between the second-richest, third-richest, and richest quartile per capita Gross Domestic Product were 0.0005, 0.162, and 0.062, respectively, compared with the poorest quartile. The patterns were similar when we considered the likelihood of having a BMI (in kg/m2) ≥25 (overweight) as the outcome. Statistical tests were based on a 2-tailed Wald test using chi-square distribution.
We conducted sensitivity analyses by adjusting for mean age at the country level, in addition to individual age adjustment or age distribution within countries, and this did not alter our primary findings related to the association between BMI and household wealth and education, separately (Supplementary Table 5 under “Supplemental data” in the online issue); how the effect of household wealth varies across countries (Supplementary Table 6 under “Supplemental data” in the online issue); and country-specific differential on the association between household wealth and BMI (Supplementary Table 7 under “Supplemental data” in the online issue).
DISCUSSION
By using large representative samples of women from 54 low- to middle-income countries, we observed a robust positive association between SES and BMI and between SES and overweight. The association between wealth quartiles and weight was considerably stronger and consistent compared with the association between educational attainment and weight. There was also a positive, albeit weak, association between country economic position and BMI and overweight. At the individual level, the second wealthiest quartile had consistently higher BMI/overweight than did the third wealthiest quartile; likewise, the third wealthiest quartile also had consistently higher BMI/overweight than did the poorest wealth quartile. This pattern was observed at every level of country-level economic development. Only women in the richest quartile in richer countries were relatively less likely to have high BMI or to be overweight than women in the second- and third-richest wealth quartiles in richer countries.
Before we discuss these findings, we highlight the data limitations of the study. Our assessment of SES, through household wealth and individual education, was measured at the same time as BMI. Consequently, the association between SES and BMI/overweight should not be interpreted in unidirectional causal terms because there is likely to be a reciprocal association; for example, relative weight may influence social mobility at marriage. However, the motivation in this study was to assess the patterning in weight rather than ascertain the causal effects of SES on weight. Also, the countries included in this study were not surveyed at the same time, even though a majority of countries (43 of 54) were surveyed after 2000. Separately, our analysis was restricted to young to middle-aged women, even though similar patterns have been observed for men in country-specific studies, such as India (39). However, the socioeconomic differences in BMI/overweight between men seem to be less pronounced in some studies (20). Whether the observed association for women also holds for men in comparable samples with objective measures of height and weight remains an important empirical question.
We should note that a given BMI may confer a greater risk of obesity-related diseases, at least among certain populations, such as in Asians (40). Although this questions the relevance of a BMI cutoff as a measure of weight status, these cutoffs remain the most widely available measure for studying weight status in populations. Consequently, our findings that use BMI as an outcome, as opposed to the BMI cutoff, are more pertinent for understanding population patterns in weight status.
A higher prevalence of overweight among women of high SES has been postulated to be linked to cultural norms that may favor fatter body shapes (2). Cultural practices around food and physical activity are also possible explanations for higher BMI among women of higher SES. Crucially, higher income and wealth has been historically associated with diets rich in animal fats, which in turn are associated with higher prevalence of overweight among high socioeconomic groups (41). For instance, it has been shown that higher-income groups in India consume a diet containing 32% of energy from fat compared with consumption of a diet containing 17% of energy from fat in lower-income groups (42). Furthermore, it is possible that women of high SES in developing countries face multiple barriers to engaging in physical activity and eating healthful foods despite having more knowledge about healthy food, healthy behavior, and resources (43). At the same time, women of low SES are more likely to be involved in daily activities that are substantially more labor intensive. Finally, food remains expensive in several developing countries; a problem that has emerged quite forcefully in recent times, which makes it difficult for low socioeconomic groups to increase their energy intake (44). The issue of overweight primarily afflicting the affluent might continue because even with economic growth (which provides the immediate opportunity to consume more by increasing standards of living), the distribution of growth has remained extremely unequal in several countries. The social patterning of weight, therefore, continues to closely approximate the maldistribution of income and other resources (45).
Our study findings, with objective height and weight measurements, reveal the same patterns as those observed in another study that examined socioeconomic disparities in self-reported weight status across 41 countries (21). Within-country studies (Bangladesh, Colombia, Tanzania, and Ghana) using different data sources have also shown results similar to those presented here (46–49); for instance, although the prevalence of overweight is increasing among poorer quintiles in Brazil, and the patterns differs by region, the SES-weight status gradient is still positive according to data combined from 3 surveys between 1975 and 2003 (50). In Morocco, data from 1998 showed that the prevalence of obesity was higher among adults of higher economic status although, there was lower prevalence of obesity among more educated urban adults (51). In Latin America, studies have identified mixed results depending on which indicators of SES are used (the region within-country or the group) (52–54).
Our study also provides important updates as well as advances on the associations between SES and weight, which were previously investigated by using similar data sets in 2 studies (Supplementary Table 8 under “Supplemental data” in the online issue) (18, 19). Whereas previous assessments were based on data before 2000, the majority of the data in this study (43 of 54 surveys) were collected during the first decade of the 21st century. Also, our focus on BMI, in addition to overweight, captures nutritional status from a population perspective, which to our knowledge has not previously been presented. Notably, we provide important extensions by including wealth in addition to years of schooling. As we show, the association between weight and years of schooling was not as consistent, robust, and strong as the association between wealth and BMI. Indeed, wealth was the most important predictor of an individual's BMI. Moreover, by showing that wealth substantially attenuated the independent effects of urban-rural differences, our analysis shows that the urban-rural differences presented in previous studies may be misleading (18, 19). This suggests that urban-rural differences are largely a product of the differences in household wealth between urban and rural areas. Finally, our findings related to adjusted country-specific patterns in the association between SES and nutritional status are perhaps more relevant than testing only for an interaction between country-level economic development, individual SES, and weight status.
In summary, in 54 low- to middle-income countries, higher BMI and overweight remain concentrated in high socioeconomic groups, even though increasing BMI and overweight is an important public health concern in many of these countries. The expected social patterning underlying epidemiologic transitions whereby SES is inversely associated with overweight has therefore yet to occur. The distributive aspects of BMI and overweight by socioeconomic groups need to be central to the deliberations and development of appropriate policy responses to improving nutritional status of populations in developing countries.
Supplementary Material
Acknowledgments
We acknowledge the support of Macro International Inc (Washington, DC) for providing access to the various Demographic and Health Surveys.
The authors' responsibilities were as follows—SVS: conceived the study, analyzed the data, interpreted the results, and wrote the manuscript; JMP and EÖ: contributed to the analysis and writing; and GDS: contributed to critical revisions of the manuscript. All authors reviewed and approved the final version of the manuscript submitted for publication. All authors confirmed that they had no conflicts of interest.
REFERENCES
- 1.Wang H, Du S, Zhai F, Popkin BM. Trends in the distribution of body mass index among Chinese adults, aged 20-45 years (1989-2000). Int J Obes (Lond) 2007;31:272–8 [DOI] [PubMed] [Google Scholar]
- 2.Sobal J, Stunkard AJ. Socioeconomic status and obesity: a review of the literature. Psychol Bull 1989;105:260–75 [DOI] [PubMed] [Google Scholar]
- 3.Hossain P, Kawar B, El Nahas M. Obesity and diabetes in the developing world—a growing challenge. N Engl J Med 2007;356:213–5 [DOI] [PubMed] [Google Scholar]
- 4.Kelly T, Yang W, Chen CS, Reynolds K, He J. Global burden of obesity in 2005 and projections to 2030. Int J Obes (Lond) 2008;32:1431–7 [DOI] [PubMed] [Google Scholar]
- 5.Prentice AM. The emerging epidemic of obesity in developing countries. Int J Epidemiol 2006;35:93–9 [DOI] [PubMed] [Google Scholar]
- 6.Subramanian SV, Davey Smith G. Patterns, distribution, and determinants of under- and overnutrition: a population-based study of women in India. Am J Clin Nutr 2006;84:633–40 [DOI] [PubMed] [Google Scholar]
- 7.Fezeu L, Minkoulou E, Balkau B, et al. Association between socioeconomic status and adiposity in urban Cameroon. Int J Epidemiol 2006;35:105–11 [DOI] [PubMed] [Google Scholar]
- 8.Dahly DL, Gordon-Larsen P, Popkin BM, Kaufman JS, Adair LS. Associations between multiple indicators of socioeconomic status and obesity in young adult Filipinos vary by gender, urbanicity, and indicator used. J Nutr 2010;140:366–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nguyen MD, Beresford SA, Drewnowski A. Trends in overweight by socio-economic status in Vietnam: 1992 to 2002. Public Health Nutr 2007;10:115–21 [DOI] [PubMed] [Google Scholar]
- 10.Perez-Cueto FJ, Kolsteren PW. Changes in the nutritional status of Bolivian women 1994-1998: demographic and social predictors. Eur J Clin Nutr 2004;58:660–6 [DOI] [PubMed] [Google Scholar]
- 11.Subramanian SV, Perkins JM, Khan KT. Do burdens of underweight and overweight coexist among lower socioeconomic groups in India? Am J Clin Nutr 2009;90:369–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zaninotto P, Head J, Stamatakis E, Wardle H, Mindell J. Trends in obesity among adults in England from 1993 to 2004 by age and social class and projections of prevalence to 2012. J Epidemiol Community Health 2009;63:140–6 [DOI] [PubMed] [Google Scholar]
- 13.Roskam AJ, Kunst AE, Van Oyen H, et al. Comparative appraisal of educational inequalities in overweight and obesity among adults in 19 European countries. Int J Epidemiol 2010;39:392–404 [DOI] [PubMed] [Google Scholar]
- 14.Groth MV, Fagt S, Stockmarr A, Matthiessen J, Biltoft-Jensen A. Dimensions of socioeconomic position related to body mass index and obesity among Danish women and men. Scand J Public Health 2009;37:418–26 [DOI] [PubMed] [Google Scholar]
- 15.Wang Y, Beydoun MA. The obesity epidemic in the United States: gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev 2007;29:6–28 [DOI] [PubMed] [Google Scholar]
- 16.Sarlio-Lahteenkorva S, Lahelma E. The association of body mass index with social and economic disadvantage in women and men. Int J Epidemiol 1999;28:445–9 [DOI] [PubMed] [Google Scholar]
- 17.Monteiro CA, Moura EC, Conde WL, Popkin BM. Socioeconomic status and obesity in adult populations of developing countries: a review. Bull World Health Organ 2004;82:940–6 [PMC free article] [PubMed] [Google Scholar]
- 18.Monteiro CA, Conde WL, Lu B, Popkin BM. Obesity and inequities in health in the developing world. Int J Obes Relat Metab Disord 2004;28:1181–6 [DOI] [PubMed] [Google Scholar]
- 19.Mendez MA, Monteiro CA, Popkin BM. Overweight exceeds underweight among women in most developing countries. Am J Clin Nutr 2005;81:714–21 [DOI] [PubMed] [Google Scholar]
- 20.McLaren L, Gauvin L. Does the ‘average size’ of women in the neighbourhood influence a woman's likelihood of body dissatisfaction? Health Place 2003;9:327–35 [DOI] [PubMed] [Google Scholar]
- 21.Moore S. Global and national socioeconomic disparities in obesity, overweight, and underweight status. J Obes 2010. Available from: http://www.hindawi.com/journals/jobes/2010/514674.htm [DOI] [PMC free article] [PubMed]
- 22.Ezzati M, Vander Hoorn S, Lawes CM, et al. Rethinking the “diseases of affluence” paradigm: global patterns of nutritional risks in relation to economic development. PLoS Med 2005;2:e133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Demographic and Health Surveys. Calverton, MD: Measure DHS, 2009 [Google Scholar]
- 24.Rutstein SO, Rojas G. Guide to DHS statistics. Calverton, MD: ORC Macro, 2003 [Google Scholar]
- 25.Wirth ME, Wirth E, Delamonica E, Sacks D, Balk A, Minujin A. Monitoring health equity in the MDGs: a practical guide. New York, NY: CIESIN/UNICEF, 2006 [Google Scholar]
- 26.Vaessen M. The potential of the demographic and health surveys (DHS) for the evaluation and monitoring of maternal and child health indicators : Khlat M, Demographic evaluation of health programmes (Proceedings). Paris, France: Committee for International Cooperation in National Research in Demography/United Nations Population Fund, 1996 [Google Scholar]
- 27.Pullum TW. An assessment of the quality of data on health and nutrition in the DHS surveys, 1993-2003. Calverton, MD: Macro International Inc, 2008 [Google Scholar]
- 28.Demographic and Health Survey Interviewer's Manual. Calverton, MD: ORC Macro, 2006 [Google Scholar]
- 29.Demographic and Health Survey Sampling manual. DHS-III. Calverton, MD: Macro International, 1996 [Google Scholar]
- 30.WHO Expert Consultation. Appropriate body mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157–63 [DOI] [PubMed] [Google Scholar]
- 31.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data–or tears: an application to educational enrollments in states of India. Demography 2001;38:115–32 [DOI] [PubMed] [Google Scholar]
- 32.Gwatkin DR, Rustein S, Johnson K, Pande RP, Wagstaff A. Socioeconomic differences in health, nutrition, and population in India. Washington, DC: World Bank, 2000 [Google Scholar]
- 33.Rutstein SO, Johnson K. The DHS wealth asset index. DHS comparative report. Calverton, MD: ORC Macro, 2004 [Google Scholar]
- 34.Rutstein SO. The DHS wealth index: approaches for rural and urban areas. Washington, DC: Macro International Inc, 2008 [Google Scholar]
- 35.World Economic Outlook Database Washington, DC: International Monetary Fund, 2010 [Google Scholar]
- 36.Subramanian SV, Jones K, Duncan C. Multilevel methods for public health research. : Kawachi I, Berkman LF, Neighborhoods and health. New York, NY: Oxford University Press, 2003:65–111 [Google Scholar]
- 37.Goldstein H. Multilevel statistical models. London, United Kingdom: Arnold, 2003 [Google Scholar]
- 38.Rasbash J, Steele F, Browne WJ, Goldstein HA. User's guide to MLwiN, version 2.10. Bristol, United Kingdom: Centre for Multilevel Modelling, University of Bristol, 2009 [Google Scholar]
- 39.Subramanian SV, Perkins JM, Khan KT. Do burdens of underweight and overweight coexist among lower socioeconomic groups in India? Am J Clin Nutr 2009;90:369–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Snehalatha C, Viswanathan V, Ramachandran A. Cutoff values for normal anthropometric variables in Asian Indian adults. Diabetes Care 2003;26:1380–4 [DOI] [PubMed] [Google Scholar]
- 41.Drewnowski A, Popkin BM. The nutrition transition: new trends in the global diet. Nutr Rev 1997;55:31–43 [DOI] [PubMed] [Google Scholar]
- 42.Shetty PS. Nutrition transition in India. Public Health Nutr 2002;5:175–82 [DOI] [PubMed] [Google Scholar]
- 43.Griffiths P, Bentley M. Women of higher socio-economic status are more likely to be overweight in Karnataka, India. Eur J Clin Nutr 2005;59:1217–20 [DOI] [PubMed] [Google Scholar]
- 44.Sen A. The rich get hungrier. The New York Times 2008 May 28 [Google Scholar]
- 45.Subramanian SV, Kawachi I, Davey Smith G. Income inequality and the double burden of under- and overnutrition in India. J Epidemiol Community Health 2007;61:802–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Islam MZ, Akhtaruzzaman M, Lamberg-Allardt C. Nutritional status of women in Bangladesh: comparison of energy intake and nutritional status of a low income rural group with a high income urban group. Asia Pac J Clin Nutr 2004;13:61–8 [PubMed] [Google Scholar]
- 47.Villamor E, Msamanga G, Urassa W, et al. Trends in obesity, underweight, and wasting among women attending prenatal clinics in urban Tanzania, 1995–2004. Am J Clin Nutr 2006;83:1387–94 [DOI] [PubMed] [Google Scholar]
- 48.Amoah AG. Sociodemographic variations in obesity among Ghanaian adults. Public Health Nutr 2003;6:751–7 [DOI] [PubMed] [Google Scholar]
- 49.Gilbert-Diamond D, Baylin A, Mora-Plazas M, Villamor E. Correlates of obesity and body image in Colombian women. J Womens Health (Larchmt) 2009;18:1145–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Monteiro CA, Conde WL, Popkin BM. Income-specific trends in obesity in Brazil: 1975-2003. Am J Public Health 2007;97:1808–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Benjelloun S. Nutrition transition in Morocco. Public Health Nutr 2002;5:135–40 [DOI] [PubMed] [Google Scholar]
- 52.Fernald LC. Socio-economic status and body mass index in low-income Mexican adults. Soc Sci Med 2007;64:2030–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Goulart AC, Silva FM, de Castro I, Lotufo PA, Cardoso MA, Bensenor IM. Race and parity as risk factors for obesity among low income women in Brazil. Nutr Res Rev 2007;27:27–32 [Google Scholar]
- 54.Nagata JM, Valeggia CR, Barg FK, Bream KD. Body mass index, socio-economic status and socio-behavioral practices among Tz'utujil Maya women. Econ Hum Biol 2009;7:96–106 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.