Abstract
Objective
To evaluate visual acuity outcomes after cataract surgery in patients with varying degrees of age-related macular degeneration (AMD).
Design
Cohort study.
Participants
A total of 4757 participants enrolled in the Age-Related Eye Disease Study (AREDS), a prospective, multicenter, epidemiological study of the clinical course of cataract and AMD and a randomized controlled trial of antioxidants and minerals.
Methods
Standardized lens and fundus photographs, performed at baseline and annual visits, were graded by a centralized reading center using standardized protocols for severity of AMD and lens opacities. History of cataract surgery was obtained every 6 months. Analyses were conducted using multivariate logistic regression.
Main Outcome Measure
The change in best-corrected visual acuity (BCVA) after cataract surgery compared with preoperative BCVA.
Results
Visual acuity results were analyzed for 1939 eyes that had cataract surgery during AREDS. The mean time from cataract surgery to measurement of postoperative BCVA was 6.9 months. After adjustment for age at surgery, gender, type, and severity of cataract, the mean change in visual acuity at the next study visit after the cataract surgery was as follows: Eyes without AMD gained 8.4 letters of acuity (P<0.0001), eyes with mild AMD gained 6.1 letters of visual acuity (P<0.0001), eyes with moderate AMD gained 3.9 letters (P<0.0001), and eyes with advanced AMD gained 1.9 letters (P = 0.04). The statistically significant gain in visual acuity after cataract surgery was maintained an average of 1.4 years after cataract surgery.
Conclusions
On average, participants with varying severity of AMD benefited from cataract surgery with an increase in visual acuity postoperatively. This average gain in visual acuity persisted for at least 18 months.
Cataract surgery is currently one of the most commonly performed surgeries in the United States.1 Advances in surgical techniques, changing indications, and a growing and aging population have led to a steady increase in cataract surgery rates in the United States during the past 2 decades.2–4 Both initial and fellow-eye cataract surgery have been demonstrated to be highly cost-effective compared with procedures across multiple medical specialties.5,6 The benefit of cataract surgery in the general population with respect to visual acuity and visual function has been established.7,8 Cataract and age-related macular degeneration (AMD) often present concurrently in older persons.9–11 The presence of AMD has been highlighted as an important risk factor for poor visual outcome after cataract surgery.12–14 Given the expected increase in AMD prevalence during the next 2 decades,15 an analysis of the potential risks and benefits of cataract surgery in patients with AMD is of public health interest.
Several studies have examined the potential benefit of cataract surgery with respect to visual acuity and visual function in patients with AMD.16–22 However, prior studies have been limited by the lack of a standardized grading system for AMD and cataract, inclusion of patients with other ocular comorbidities, small sample sizes, and lack of manifest refracted visual acuities before and after cataract surgery.16–19,21 Furthermore, in previous studies persons with advanced AMD were underrepresented in the cohort16,20,21 or not included.19,22
The Age-Related Eye Disease Study (AREDS) was a prospective multicenter study of the clinical course of cataract and AMD, and participants were enrolled with varying degrees of AMD. This study was also a controlled clinical trial that evaluated the effects of high-dose vitamin and mineral supplementation on the incidence and progression of lens opacities and AMD. The results showed that high doses of vitamins C, E, and beta-carotene did not have an effect on the progression or development of cataract.23 However, the combination of the vitamins and zinc reduced the risk of progression to advanced AMD by 25%.24
In AREDS, ocular status at annual visits was documented by both comprehensive ophthalmic examinations and annual lens and fundus photography. The ocular photographs were graded centrally by masked observers using standardized photographs and protocols at the University of Wisconsin reading center. The AREDS cohort provides an opportunity to evaluate the potential benefits of cataract surgery in patients with AMD. The purpose of this study is to evaluate the visual outcomes after cataract surgery in the AREDS cohort.
Materials and Methods
Details of the AREDS study design have been published25 and are briefly summarized below. A total of 4757 persons, aged 55 to 80 years, were enrolled in the study at 11 clinical centers across the United States from November 1992 to January 1998. The randomized controlled clinical trial ended in October 2001, and participants were invited to continue follow-up until December 2005. Institutional review board approval was obtained at each clinical site, and all participants signed informed consent. Participants were required to have good baseline visual acuity in at least 1 eye (Snellen equivalent of ≥20/32) and media clear enough to obtain good-quality fundus photographs.
Participants in AREDS had comprehensive eye examinations every 6 months, with lens and fundus photographs taken at enrollment and annually thereafter beginning 2 years after enrollment until 2001. During the last 4 years of the follow-up study, patients were contacted at 6 months and examined annually. Best-corrected visual acuity (BCVA) was obtained by trained and certified examiners. The ocular photographs were graded at a reading center with standardized protocols by trained and certified examiners using the Age-Related Eye Disease System for classifying cataracts.26 Cataract grade was further classified into a previously described 3-point ordinal scale.27
Eyes were classified into 1 of 3 nuclear opacity groups, ignoring cortical opacity:
Grade 1: Nuclear grade ≤2
Grade 2: Nuclear grade >2 and <4
Grade 3: Nuclear grade ≥4
Eyes were further classified into 1 of 3 cortical opacity groups, ignoring nuclear opacity:
Grade 1: Cortical = 0%
Grade 2: Cortical >0% and ≤5%
Group 3: Cortical >5%
Posterior subcapsular opacities were not considered in this report, because they were uncommon in the cohort and, when present, often occurred in combination with nuclear or cortical opacities.27
The AREDS classification of AMD lesions was used to categorize patients into 1 of 4 severity groups (Table 1).28 Fundus photographs were graded for drusen characteristics (size, type, area), pigmentary abnormalities (increased pigment, depigmentation, geographic atrophy), and presence of abnormalities characteristic of neovascular AMD (retinal pigment epithelial detachment, serous or hemorrhagic sensory retinal detachment, subretinal or subretinal pigment epithelial hemorrhage, subretinal fibrous tissue), and individual eyes were categorized into 4 separate groups (control, mild, intermediate, and advanced AMD). Eyes that received treatment for neovascular AMD, such as laser photocoagulation or photodynamic therapy, were defined to have advanced AMD regardless of fundus lesions.
Table 1. Age-Related Macular Degeneration Levels Defined for Eyes.
| AMD Level | Criteria |
|---|---|
| No AMD | No drusen or nonextensive small (<63 μm) drusen |
| Mild | Presence of ≥1 of the following:
|
| Intermediate | Presence of ≥1 of the following:
|
| Advanced | Presence of ≥1 of the following:
|
AMD = age-related macular degeneration.
At each study visit, self-reports of cataract surgery since the last study visit were collected. The examining investigator also documented the presence or absence of the natural lens at the slit-lamp examination. For our analysis, we included eyes that had cataract surgery during AREDS. We excluded eyes that had cataract surgery at baseline (n = 419).
The primary outcome of our analysis was the change in BCVA after cataract surgery compared with the BCVA before surgery. Because participants were evaluated every 6 months, the documented preoperative BCVA closest to the date of cataract surgery and the first recorded BCVA after cataract surgery were used. Thus, the preoperative visual acuity may not have always been in the immediate preoperative period and could have been recorded up to 6 months or greater before the date of cataract surgery. Visual acuity data obtained after the first postoperative month were considered for analysis. Change in visual acuity was the difference in the BCVA score between the closest pair of postoperative and preoperative visits. The AMD and cataract grade used for our analysis were obtained from the closest study visits before and after the date of cataract surgery. To assess the longer-term change in visual acuity after cataract surgery, a secondary analysis was performed using the postoperative BCVA that was obtained 1 year (±1 month) from the time of the postoperative BCVA used in our primary analysis. Eyes with cataract surgery at baseline were excluded from the primary and secondary analyses. Data regarding the incidence and severity of adverse side effects associated with cataract surgery were not collected in this study.
To examine visual acuity outcomes after cataract surgery, we developed a multivariate model using repeated-measures regression analysis. Because some patients contributed both eyes to the analysis, we accounted for the correlation between eyes within a person by specifying a compound symmetry covariance structure. The MIXED procedure of the SAS System (SAS version 9.1; SAS, Cary, NC) was used. Risk factors considered as covariates in the model were age at surgery, gender, preoperative AMD level, and nuclear and cortical opacity groups. Each covariate was evaluated separately in the model while adjusting for age at surgery. Factors significant at a 0.15 level were then included together in a model. Nominal statistical significance was set at 0.05 for the visual acuity analysis.
Results
There were a total of 2601 cataract surgeries on 2601 eyes of 1583 patients. This number was reduced to 1939 eyes (1244 patients) after further exclusion of eyes with missing data. Analyses of eyes that were not included in our analyses because of missing data revealed that they were more likely to be of participants who had lower education levels (data not shown). There were no differences in the baseline ocular characteristics among those included and those not included in the analyses.
Characteristics of the eyes included in the analyses are summarized in Table 2, and a graphical representation of this data in relation to visual acuity is depicted in Figure 1. The mean time from the last recorded preoperative visual acuity to the operative date was 6.6 months (±8.3, median 4.3, range: 0.03–83.6), and the mean time from the operative date to the postoperative BCVA was 6.9 months (±6.9, median 5.1, range: 1.0–82.3). For the secondary analysis, the mean time from the operative date to the postoperative BCVA was 1.4 years (±0.3, median 1.4, range: 1.0–3.3). Figure 2 shows postoperative visual acuities for the eyes used in our primary and secondary analyses.
Table 2. Ocular Characteristics of Participants Undergoing Cataract Surgery (n = 1939).
| No AMD | Mild AMD | Intermediate AMD | Advanced AMD | |
|---|---|---|---|---|
| Sample size | 626 (32%) | 406 (21%) | 712 (37%) | 195 (10%) |
| Nuclear cataract | ||||
| Grade 1 | 67 (11%) | 41 (10%) | 54 (8%) | 9 (5%) |
| Grade 2 | 319 (51%) | 227 (56%) | 403 (57%) | 99 (51%) |
| Grade 3 | 240 (38%) | 138 (34%) | 255 (36%) | 87 (45%) |
| Cortical cataract | ||||
| Grade 1 | 270 (43%) | 155 (38%) | 267 (38%) | 67 (34%) |
| Grade 2 | 175 (28%) | 122 (30%) | 256 (36%) | 65 (33%) |
| Grade 3 | 181 (29%) | 129 (32%) | 189 (27%) | 63 (32%) |
AMD = age-related macular degeneration.
Figure 1.
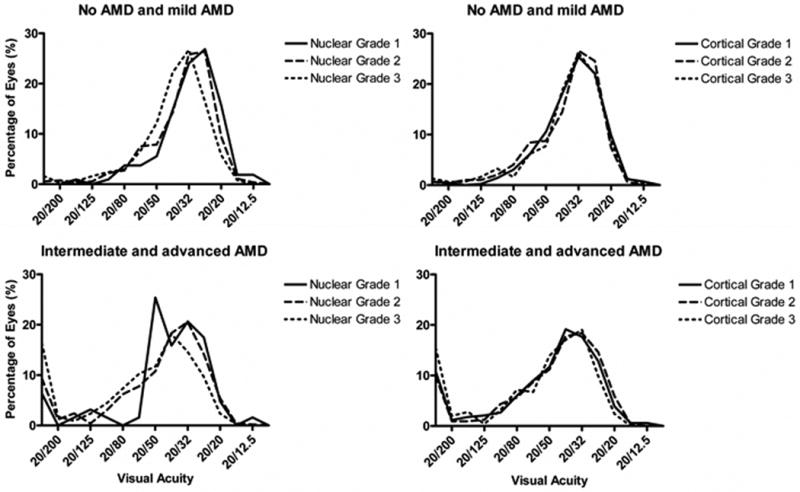
Baseline visual acuity and cataract severity of eyes in the primary analysis. Cataract grade is shown as a function of visual acuity in eyes with no AMD and mild AMD, as well as intermediate AMD and advanced AMD. The visual acuity score is represented as Snellen equivalents. AMD = age-related macular degeneration.
Figure 2.
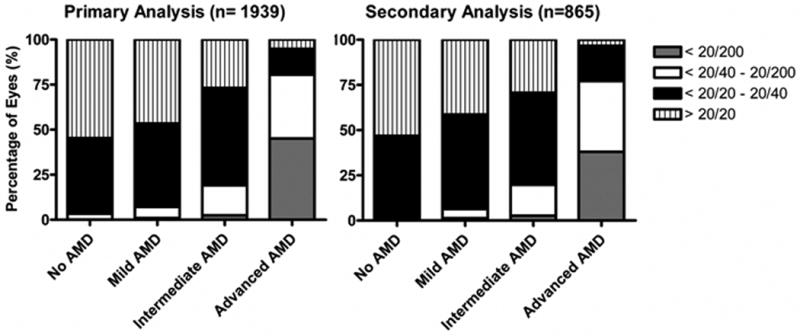
Comparison of preoperative visual acuity of eyes analyzed in both primary and secondary analyses. Percentages are shown for eyes with varying degrees of preoperative visual acuity and AMD severity used in primary and secondary analyses. The visual acuity score is represented as Snellen equivalents. AMD = age-related macular degeneration.
Results of the multivariable repeated-measures regression analysis are shown in Table 3. After adjustment for covariates, including age at surgery, gender, and nuclear and cortical cataract group, we observed a statistically significant mean gain of visual acuity after cataract surgery in all AMD groups. Patients without AMD gained 8.4 letters (P<0.0001), patients with mild AMD gained 6.1 letters (P<0.0001), patients with intermediate AMD gained 3.9 letters (P<0.0001), and patients with advanced AMD gained 1.9 letters (P = 0.04). Subgroup analyses of the advanced AMD group with respect to type of lesion (central geographic atrophy only, neovascularization only, and both central geographic atrophy and neovascularization) demonstrated no clear differences in visual acuity outcome among the eyes with different subtypes of advanced AMD (data not shown). The postoperative visual acuity as a function of preoperative visual acuity is graphically shown in Figure 3. After cataract surgery, the proportion of persons improving by more than 10 letters was 40.9% in the no AMD group, 32.4% in the mild AMD group, 28.8% in the intermediate AMD group, and 23.6% in the advanced AMD group. The proportion of persons improving by 15 letters or more was 23% in the no AMD group and approximately 15% in each of the other 3 AMD severity groups (Fig 4). Significant improvement in visual acuity was seen in patients receiving either AREDS supplementation or placebo, demonstrating that nutritional supplementation did not have an effect on visual acuity outcomes (data not shown). In eyes with preoperative visual acuity of 20/40 or worse, a greater gain in visual acuity after cataract surgery was observed (Table 4).
Table 3. Adjusted* Gain in Visual Acuity Score after Cataract Surgery† Based on Preoperative Severity of Age-Related Macular Degeneration and Cataract (n = 1939).
| Group | Estimate (Gain of Letters on the Visual Acuity Score) | 95% CI | P |
|---|---|---|---|
| No AMD | 8.36 | 7.21–9.51 | <0.0001 |
| Mild AMD | 6.13 | 4.78–7.48 | <0.0001 |
| Intermediate AMD | 3.92 | 2.82–5.03 | <0.0001 |
| Advanced AMD | 1.94 | 0.05–3.82 | 0.04 |
| Nuclear cataract | |||
| Grade 1 | 0.84 | −1.11–2.79 | 0.40 |
| Grade 2 | 4.89 | 4.02–5.75 | <0.0001 |
| Grade 3 | 9.53 | 8.52–10.55 | <0.0001 |
| Cortical cataract | |||
| Grade 1 | 3.75 | 2.62–4.89 | <0.0001 |
| Grade 2 | 5.50 | 4.32–6.68 | <0.0001 |
| Grade 3 | 6.01 | 4.80–7.23 | <0.0001 |
AMD = age-related macular degeneration; CI = confidence interval.
Adjusted for age at time of surgery.
Analyses represent change in BCVA at a mean time of 6.9 months after cataract surgery.
Figure 3.
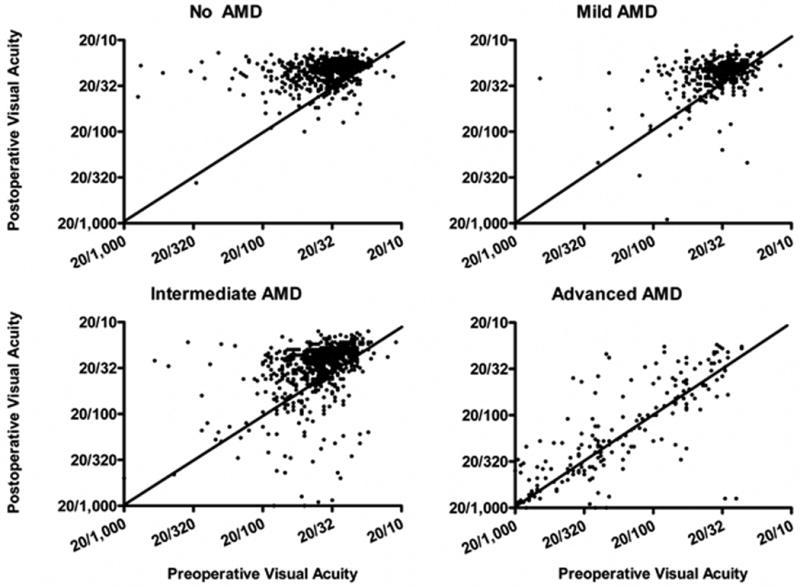
Visual acuity scores before and after cataract surgery in the primary analysis. Visual acuity scores and the corresponding Snellen equivalents are represented in the preoperative (x-axis) and postoperative (y-axis) visits. The diagonal lines intersecting at the origin represent no change in visual acuity, whereas those values below the diagonal demonstrate a decrease in visual acuity postoperatively.
Figure 4.
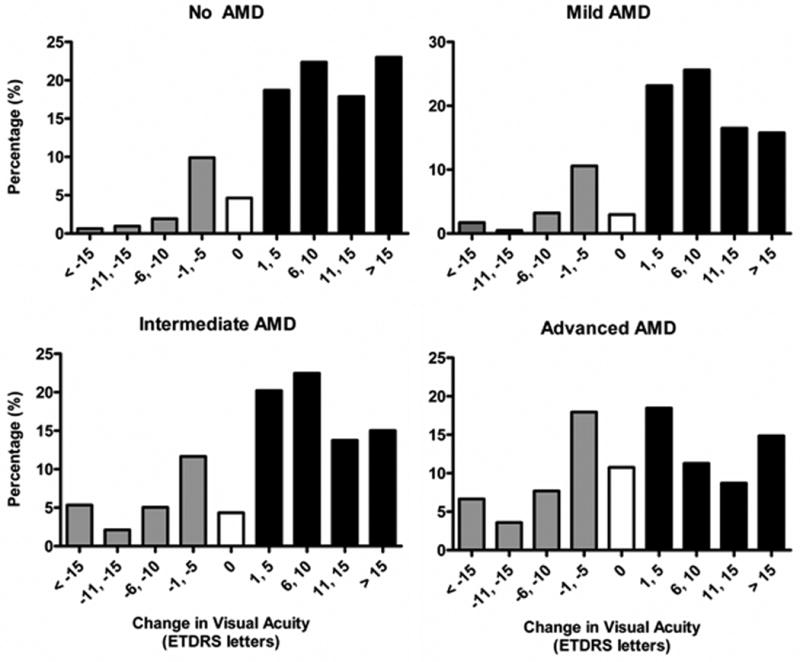
Change in visual acuity after cataract surgery in patients with varying severity of AMD. Percentage of patients with gain or loss of letters on the logarithm of the minimal angle of resolution visual acuity chart is shown for eyes with no AMD, mild AMD, intermediate AMD, and advanced AMD. AMD = age-related macular degeneration; ETDRS = Early Treatment Diabetic Retinopathy Study.
Table 4. Adjusted* Gain in Visual Acuity Score after Cataract Surgery† Based on Preoperative Severity of Age-Related Macular Degeneration and Cataract in Eyes with Preoperative Visual Acuity of 20/40 or Worse (n = 1006).
| Group | Estimate (Gain in Letters in the Visual Acuity Score) | 95% CI | P |
|---|---|---|---|
| No AMD | 15.40 | 13.49–17.31 | <0.0001 |
| Mild AMD | 10.93 | 8.69–13.17 | <0.0001 |
| Intermediate AMD | 6.73 | 5.12–8.34 | <0.0001 |
| Advanced AMD | 2.29 | 0.09–4.49 | 0.04 |
CI = confidence interval; AMD = age-related macular degeneration.
Adjusted for age at time of surgery.
Analyses represent change in BCVA at a mean time of 6.4 months after cataract surgery.
After adjusting for covariates, we also found a statistically significant gain in visual acuity in patients with nuclear and cortical cataracts after cataract surgery. We observed an increased gain in visual acuity with increasing severity of nuclear or cortical cataract grade after adjustment for AMD level. After adjustment for cortical cataract severity, participants with grade 1 nuclear cataract gained 0.8 letters (P = 0.40) of acuity after cataract surgery, whereas those with grade 2 nuclear cataracts gained 4.9 letters of acuity (P<0.0001) and those with grade 3 nuclear cataracts gained 9.5 letters (P<0.0001). After adjustment for nuclear cataract severity, participants with grade 1 cortical cataract gained 3.8 letters (P<0.0001) of acuity after cataract surgery, those with grade 2 cortical cataracts gained 5.5 letters (P<0.0001) of acuity after cataract surgery, and those with grade 3 cortical cataracts gained 6.0 letters (P<0.0001) of acuity after cataract surgery.
An analysis of visual acuity at 1 year (±1 month) after the postoperative date used in the primary analysis was done to assess longer-term outcomes of cataract surgery. A total of 865 eyes from the 1939 eyes in the primary analysis had visual acuity data within the specified time window. Multivariable repeated-measures regression analysis demonstrated that the statistically significant gain in visual acuity after cataract surgery was still present an average postoperative follow-up of 1.4 years (median 1.4, range: 1–3.3), demonstrated in Table 5. As in our primary analysis, we found the increased severity of lens opacity (except for grade 1 nuclear cataracts) was associated with greater gain in visual acuity after cataract surgery (data not shown). Also similar to our primary analysis, subgroup analyses of the advanced AMD group with respect to type of lesion (central geographic atrophy only, neovascularization only, and both central geographic atrophy and neovascularization) demonstrated no clear differences among the subtypes of advanced AMD. A greater gain in visual acuity after cataract surgery was observed in eyes with preoperative acuity of 20/40 or worse (Table 6).
Table 5. Adjusted* Gain in Visual Acuity Score after Cataract Surgery at a Mean Postoperative Time of 1.4 Years Based on Preoperative Severity of Age-Related Macular Degeneration and Cataract (n = 865).
| Group | Estimate (Gain in Letters in the Visual Acuity Score) | 95% CI | P |
|---|---|---|---|
| No AMD | 9.43 | 7.72–11.14 | <0.0001 |
| Mild AMD | 7.25 | 5.10–9.41 | <0.0001 |
| Intermediate AMD | 4.48 | 2.78–6.18 | <0.0001 |
| Advanced AMD | 3.40 | 0.64–6.16 | 0.02 |
CI = confidence interval; AMD = age-related macular degeneration.
Adjusted for age at time of surgery.
Table 6. Adjusted* Gain in Visual Acuity Score after Cataract Surgery at a Mean Postoperative Time of 1.4 Years Based on Preoperative Severity of Age-Related Macular Degeneration and Cataract in Patients with Preoperative Visual Acuity of 20/40 or Worse (n = 468).
| Group | Estimate (Gain in Letters in the Visual Acuity Score) | 95% CI | P |
|---|---|---|---|
| No AMD | 16.47 | 13.46–19.48 | <0.0001 |
| Mild AMD | 11.33 | 7.71–14.94 | <0.0001 |
| Intermediate AMD | 6.82 | 4.24–9.40 | <0.0001 |
| Advanced AMD | 3.88 | 0.48–7.28 | 0.03 |
CI = confidence interval; AMD = age-related macular degeneration.
Adjusted for age at time of surgery.
Discussion
This study describes the visual acuity outcomes from the largest cohort of persons with AMD undergoing cataract surgery that has been reported to date. Furthermore, this study of cataract surgery outcomes in such patients is the only study published to date that used a standardized and validated photographic technique for grading both the severity of AMD and the amount of lens opacities.
After adjustment for covariates including severity of nuclear and cortical cataract, we found a statistically significant gain of visual acuity in patients with AMD after cataract surgery. This gain in visual acuity was seen in all levels of AMD, including advanced cases with central geographic atrophy or neovascular changes. Furthermore, this statistically significant gain in visual acuity was maintained for at least 1 year after cataract surgery.
The findings of this study are particularly important in light of epidemiologic studies that suggest a harmful effect of cataract surgery on the acceleration of AMD progression. Findings from large epidemiological studies29,30 of the increased risk of advanced AMD after cataract surgery have led some investigators to speculate that cataract surgery in patients with AMD is a “gamble” for both the patient and the surgeon.31 Other investigators have called for more “stringent” indications for cataract surgery in patients with AMD.30 Data from AREDS suggest that there is little evidence of effect of cataract surgery on the risk of progression to advanced AMD.32 These findings from AREDS demonstrate a benefit of cataract surgery in patients with varying degrees of AMD, including those with advanced disease. Because the decision to perform cataract surgery in AREDS was not controlled, there is a potential for differences in the decision making to perform cataract surgery in patients with AMD. It is possible that cataract surgery was more likely to be performed in patients with a perceived more favorable outcome (i.e., patients with less severe AMD). Despite this potential difference in clinical judgment, we still observed a significant gain in visual acuity in patients with advanced AMD, which further supports our conclusion of a visual acuity benefit of cataract surgery in patients with all types of AMD.
In conclusion, self-reported vision-related quality of life is an important outcome measure to consider when determining the potential benefits of any intervention such as cataract surgery. Previous studies using various patient questionnaires have demonstrated a positive impact in this outcome in patients with AMD undergoing cataract surgery.17–22,33 The National Eye Institute Visual Function Questionnaire (NEI-VFQ) was constructed to evaluate the impact of visual disability on health-related quality of life across several common eye conditions. The NEI-VFQ has been extensively validated in a variety of eye diseases, including AMD and cataract within the AREDS population.34 Although the NEI-VFQ was administered to the AREDS participants, only a limited number of participants had appropriately timed NEI-VFQ scores that corresponded to the preoperative and postoperative visits used in our analysis. The National Eye Institute Visual Function Questionnaire scores have been shown to be more responsive to visual acuity change in the better-seeing eye.34 Nevertheless, the AREDS data without the NEI-VFQ results suggest that vision improves after cataract surgery in patients with varying degrees of AMD severity, even in eyes with advanced AMD.
Acknowledgments
Supported by the intramural program funds and contracts from the National Eye Institute/National Institutes of Health, Department of Health and Human Services, Bethesda, Maryland.
Footnotes
Financial Disclosure(s): The author(s) have no proprietary or commercial interest in any materials discussed in this article.
For complete listing of the AREDS Research Group, please see AREDS Report No. 8, Arch Ophthalmol 2001;119:1417-36.
References
- 1.Rutkow IM. Surgical operations in the United States: then (1983) and now (1994) Arch Surg. 1997;132:983–90. doi: 10.1001/archsurg.1997.01430330049007. [DOI] [PubMed] [Google Scholar]
- 2.Tan AG, Wang JJ, Rochtchina E, et al. Increase in cataract surgery prevalence from 1992–1994 to 1997–2000: analysis of two population cross-sections. Clin Experiment Ophthalmol. 2004;32:284–8. doi: 10.1111/j.1442-9071.2004.00817.x. [DOI] [PubMed] [Google Scholar]
- 3.Baratz KH, Gray DT, Hodge DO, et al. Cataract extraction rates in Olmsted County, Minnesota, 1980 through 1994. Arch Ophthalmol. 1997;115:1441–6. doi: 10.1001/archopht.1997.01100160611015. [DOI] [PubMed] [Google Scholar]
- 4.Klein BE, Klein R, Lee KE. Incidence of age-related cataract over a 10-year interval: the Beaver Dam Eye Study. Ophthalmology. 2002;109:2052–7. doi: 10.1016/s0161-6420(02)01249-6. [DOI] [PubMed] [Google Scholar]
- 5.Busbee BG, Brown MM, Brown GC, Sharma S. Incremental cost-effectiveness of initial cataract surgery. Ophthalmology. 2002;109:606–12. doi: 10.1016/s0161-6420(01)00971-x. discussion 612–3. [DOI] [PubMed] [Google Scholar]
- 6.Busbee BG, Brown MM, Brown GC, Sharma S. Cost-utility analysis of cataract surgery in the second eye. Ophthalmology. 2003;110:2310–7. doi: 10.1016/S0161-6420(03)00796-6. [DOI] [PubMed] [Google Scholar]
- 7.Steinberg EP, Tielsch JM, Schein OD, et al. National study of cataract surgery outcomes: variation in 4-month postoperative outcomes as reflected in multiple outcome measures. Ophthalmology. 1994;101:1131–40. doi: 10.1016/s0161-6420(94)31210-3. discussion 1140–1. [DOI] [PubMed] [Google Scholar]
- 8.Javitt JC, Brenner MH, Curbow B, et al. Outcomes of cataract surgery: improvement in visual acuity and subjective visual function after surgery in the first, second, and both eyes. Arch Ophthalmol. 1993;111:686–91. doi: 10.1001/archopht.1993.01090050120041. [DOI] [PubMed] [Google Scholar]
- 9.Wang JJ, Foran S, Mitchell P. Age-specific prevalence and causes of bilateral and unilateral visual impairment in older Australians: the Blue Mountains Eye Study. Clin Experiment Ophthalmol. 2000;28:268–73. doi: 10.1046/j.1442-9071.2000.00315.x. [DOI] [PubMed] [Google Scholar]
- 10.Liu IY, White L, LaCroix AZ. The association of age-related macular degeneration and lens opacities in the aged. Am J Public Health. 1989;79:765–9. doi: 10.2105/ajph.79.6.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klein R, Klein BE, Linton KL. Prevalence of age-related maculopathy: the Beaver Dam Eye Study. Ophthalmology. 1992;99:933–43. doi: 10.1016/s0161-6420(92)31871-8. [DOI] [PubMed] [Google Scholar]
- 12.Schein OD, Steinberg EP, Cassard SD, et al. Predictors of outcome in patients who underwent cataract surgery. Ophthalmology. 1995;102:817–23. doi: 10.1016/s0161-6420(95)30952-9. [DOI] [PubMed] [Google Scholar]
- 13.Lundqvist B, Monestam E. Longitudinal changes in subjective and objective visual function 5 years after cataract surgery: Clin Experiment Ophthalmol prospective population-based study. J Cataract Refract Surg. 2006;32:1944–50. doi: 10.1016/j.jcrs.2006.06.023. [DOI] [PubMed] [Google Scholar]
- 14.Lundstrom M, Stenevi U, Thorburn W. Outcome of cataract surgery considering the preoperative situation: a study of possible predictors of the functional outcome. Br J Ophthalmol. 1999;83:1272–6. doi: 10.1136/bjo.83.11.1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Klein R, Klein BE, Knudtson MD, et al. Fifteen-year cumulative incidence of age-related macular degeneration: the Beaver Dam Eye Study. Ophthalmology. 2007;114:253–62. doi: 10.1016/j.ophtha.2006.10.040. [DOI] [PubMed] [Google Scholar]
- 16.Shuttleworth GN, Luhishi EA, Harrad RA. Do patients with age related maculopathy and cataract benefit from cataract surgery? Br J Ophthalmol. 1998;82:611–6. doi: 10.1136/bjo.82.6.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Armbrecht AM, Findlay C, Kaushal S, et al. Is cataract surgery justified in patients with age related macular degeneration? A visual function and quality of life assessment. Br J Ophthalmol. 2000;84:1343–8. doi: 10.1136/bjo.84.12.1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mallah MK, Hart PM, McClure M, et al. Improvements in measures of vision and self-reported visual function after cataract extraction in patients with late-stage age-related maculopathy. Optom Vis Sci. 2001;78:683–8. doi: 10.1097/00006324-200109000-00014. [DOI] [PubMed] [Google Scholar]
- 19.Lundstrom M, Brege KG, Floren I, et al. Cataract surgery and quality of life in patients with age related macular degeneration. Br J Ophthalmol. 2002;86:1330–5. doi: 10.1136/bjo.86.12.1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Armbrecht AM, Findlay C, Aspinall PA, et al. Cataract surgery in patients with age-related macular degeneration: one-year outcomes. J Cataract Refract Surg. 2003;29:686–93. doi: 10.1016/s0886-3350(02)01650-4. [DOI] [PubMed] [Google Scholar]
- 21.Pham TQ, Cugati S, Rochtchina E, et al. Age-related maculopathy and cataract surgery outcomes: visual acuity and health-related quality of life. Eye. 2007;21:324–30. doi: 10.1038/sj.eye.6702171. [DOI] [PubMed] [Google Scholar]
- 22.Lamoureux EL, Hooper CY, Lim L, et al. Impact of cataract surgery on quality of life in patients with early age-related macular degeneration. Optom Vis Sci. 2007;84:683–8. doi: 10.1097/OPX.0b013e31812f755f. [DOI] [PubMed] [Google Scholar]
- 23.Age-Related Eye Disease Study Research Group A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E and beta carotene for age-related cataract and vision loss: AREDS report no. 9. Arch Ophthalmol. 2001;119:1439–52. doi: 10.1001/archopht.119.10.1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Age-Related Eye Disease Study Research Group A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol. 2001;119:1417–36. doi: 10.1001/archopht.119.10.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Age-Related Eye Disease Study Research Group The Age-Related Eye Disease Study (AREDS): design implications. AREDS report no. 1. Control Clin Trials. 1999;20:573–600. doi: 10.1016/s0197-2456(99)00031-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Age-Related Eye Disease Study Research Group The Age-Related Eye Disease Study (AREDS) system for classifying cataracts from photographs: AREDS report no. 4. Am J Ophthalmol. 2001;131:167–75. doi: 10.1016/s0002-9394(00)00732-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Age-Related Eye Disease Study Research Group Risk factors associated with age-related nuclear and cortical cataract: a case-control study in the Age-Related Eye Disease Study, AREDS report no. 5. Ophthalmology. 2001;108:1400–8. doi: 10.1016/s0161-6420(01)00626-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Age-Related Eye Disease Study Research Group The Age-Related Eye Disease Study system for classifying age-related macular degeneration from stereoscopic color fundus photographs: the Age-Related Eye Disease Study report number 6. Am J Ophthalmol. 2001;132:668–81. doi: 10.1016/s0002-9394(01)01218-1. [DOI] [PubMed] [Google Scholar]
- 29.Wang JJ, Klein R, Smith W, et al. Cataract surgery and the 5-year incidence of late-stage age-related maculopathy: pooled findings from the Beaver Dam and Blue Mountains eye studies. Ophthalmology. 2003;110:1960–7. doi: 10.1016/s0161-6420(03)00816-9. [DOI] [PubMed] [Google Scholar]
- 30.Freeman EE, Munoz B, West SK, et al. Is there an association between cataract surgery and age-related macular degeneration? Data from three population-based studies. Am J Ophthalmol. 2003;135:849–56. doi: 10.1016/s0002-9394(02)02253-5. [DOI] [PubMed] [Google Scholar]
- 31.de Jong PT, Lubsen J. The standard gamble between cataract extraction and AMD. Graefes Arch Clin Exp Ophthalmol. 2004;242:103–5. doi: 10.1007/s00417-003-0833-3. [DOI] [PubMed] [Google Scholar]
- 32.Chew EY, Sperduto RD, Milton RC, et al. Risk of advanced age-related macular degeneration after cataract surgery in the Age-Related Eye Disease Study: AREDS Report 25. Ophthalmology. 2009;116:297–303. doi: 10.1016/j.ophtha.2008.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chandrasekaran S, Wang JJ, Rochtchina E, Mitchell P. Change in health-related quality of life after cataract surgery in a population-based sample. Eye. 2008;22:479–84. doi: 10.1038/sj.eye.6702854. [DOI] [PubMed] [Google Scholar]
- 34.Age-Related Eye Disease Study Research Group Responsiveness of the National Eye Institute Visual Function Questionnaire to progression to advanced age-related macular degeneration, vision loss, and lens opacity: AREDS report no. 14. Arch Ophthalmol. 2005;123:1207–14. doi: 10.1001/archopht.123.9.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]


