Abstract
The diagnosis of masked hypertension has been made easier with the widespread availability of home blood pressure monitoring devices with levels of accuracy comparable to ambulatory blood pressure monitoring. The negative impact of masked hypertension on cardiovascular morbidity and mortality is evidenced by numerous well-designed clinic-based and population-based studies. The relationship of masked hypertension and target organ damage is also well documented. These two factors, combined with the robust evidence of reduced cardiovascular morbidity and mortality achieved with blood pressure treatment, makes the argument for actively identifying patients with masked hypertension and prescribing treatment similar to that for patients with sustained hypertension. In this paper, we review the evidence for the cardiovascular prognosis of masked hypertension compared with sustained hypertension, we review its impact on target organ damage, we propose an algorithm for the treatment of patients with masked hypertension, and we point out the pitfalls in adopting such an approach.
Keywords: Masked hypertension, Out-of-office blood pressure measurement, Ambulatory blood pressure monitoring, Home blood pressure monitoring, Self blood pressure measurement, BP measurement, Target organ damage, Cardiovascular prognosis
Introduction
The combination of out-of-office blood pressure measurements (via ambulatory and home blood pressure monitoring) with office blood pressure measurements allows clinicians to identify four types of blood pressure status: normotension, white-coat hypertension, masked hypertension, and sustained hypertension. Since its introduction by Thomas Pickering in 2002, the term masked hypertension has gained increased attention in the literature [1, 2]. In this paper, we define masked hypertension and its causal mechanisms, and we present the rationale for treating patients with masked hypertension, as well as some of the pitfalls with this approach.
Definition of Masked Hypertension
The availability of ambulatory blood pressure monitoring (ABPM) and home blood pressure measurements (HBPM) has exposed two major forms of discrepancy between office and out-of-office blood pressure measurements: white-coat hypertension and masked hypertension [2]. Patients with white-coat hypertension have elevated office blood pressure and normal out-of-office blood pressure, whereas those with masked hypertension have normal office blood pressure and elevated out-of-office blood pressure [2]. The two thresholds commonly used for this classification are 140/90 mm Hg for office measurements and 135/85 mm Hg for HBPM or daytime ABPM [3].
Prevalence of Masked Hypertension, Underlying Risk Factors, and Mechanisms
Depending on the study population, setting, and modality of out-of-office blood pressure measurement (HBPM or ABPM), the prevalence of masked hypertension lies between 8% and 20% among untreated adults, and up to 61% among treated adults [3, 4]. In a meta-analysis, Verberk et al. [4] estimated an average prevalence of 16.8% (95% CI, 13.0–20.5%) based on 28 studies weighted for the number of subjects. Among children and adolescents, the estimated prevalence of masked hypertension ranges from 7.4% [5] to 11.0% [6]. The discussion of masked hypertension in the rest of this paper focuses mainly on adults.
Pickering and colleagues [7] identified two categories of causal mechanisms of masked hypertension: factors that selectively reduce office blood pressure relative to out-of-office readings, and factors that selectively increase ambulatory blood pressure. Reduced office blood pressure in relation to out-of-office blood pressure has been attributed to the “regression to the mean” phenomenon because hypertension status is always based on an elevated office blood pressure reading [2]; the absence of diagnostic labeling may explain lower office blood pressure noted in patients with masked hypertension [8•]. Several factors may selectively raise the ambulatory blood pressure relative to office blood pressure. These include smoking, increased physical activity, alcohol consumption, obesity, and psychosocial factors such as anxiety, interpersonal conflict, and job stress [8•, 9, 10, 11••, 12]. Other factors such as a younger age and male gender are possible characteristics of patients with masked hypertension that do not necessarily exclusively affect either of the two measurements [8•]. In a Japanese study of 3,400 treated hypertensive patients, factors associated with masked hypertension were overweight, defined as body mass index (BMI) of 25 kg/m2 or higher (OR, 1.38; 95% CI, 1.09–1.75) and regular alcohol consumption (OR, 1.37; 95% CI, 1.09–1.72) [10]. In an Italian study of 1,488 hypertensive patients referred to a specialist center, the risk of masked hypertension was higher in men than in women (RR, 1.14; 95% CI, 1.01–1.28) and was higher in current smokers (RR, 1.16; 95% CI, 1.04–1.30) [13]. Similarly, a study of 694 Chinese people found that women were less likely than men to have masked hypertension (OR, 0.39; 95% CI, 0.22–0.68) [12]. Finally, we found that patients with masked hypertension exhibit lower levels of anxiety in the office than those with white-coat hypertension [11••]. Poor medication adherence and intake of medication just before clinic consultation (so that the peak effect is observed) have also been suggested as possible factors [9].
Rationale for Treatment of Patients with Masked Hypertension
The public health goal of treatment (both pharmacologic and lifestyle interventions) for patients with a diagnosis of hypertension is the reduction of cardiovascular morbidity and mortality [14]. Several conditions must be fulfilled to satisfy this public health goal. First, the diagnosis of hypertension must be relatively easy and accessible. Second, evidence for the negative impact of hypertension on cardiovascular morbidity and mortality must be robust. Finally, treatment of hypertension must lead to improved morbidity and mortality and the prevention of target organ damage. Similar to treatment of patients with diagnosed hypertension, evidence for the treatment of patients with masked hypertension should also be based on the satisfaction of the same conditions. Below, we address each of these conditions, summarize the evidence for the negative impact of masked hypertension on cardiovascular morbidity and mortality and its association with increased target organ damage, and propose an algorithm for the treatment of patients with masked hypertension.
Diagnosis of Masked Hypertension
Today, blood pressure measurement is the most common vital sign taken in ambulatory care settings, and out-of-office blood pressure measurement, including self-monitoring, has gained popularity, making it easy to identify patients with different subtypes of blood pressure status [15]. Unlike patients with white-coat hypertension, who are easy to identify given their elevated office blood pressure, the objective of making a diagnosis of masked hypertension is to identify patients who have persistently elevated out-of-office blood pressure and thus are not receiving treatment or are treated inadequately. Ideally, the “gold standard” for identifying patients with masked hypertension is ABPM, but recent data suggest that self-monitoring of blood pressure correctly classifies most cases of masked hypertension, when compared with ABPM [15]. In a pooled meta-analysis of population-based and clinic-based studies of masked hypertension by Verbek et al. [4], there was no statistical difference in the prevalence of masked hypertension as determined by HBPM (21.1%) and ABPM (16.8%; P=0.42). Thus, the increased popularity of self-monitoring of blood pressure and the availability of valid and accurate monitoring devices make it relatively easier to identify patients with masked hypertension.
Prognostic Significance of Masked Hypertension in Predicting Cardiovascular Morbidity and Mortality
The superior predictive ability of ABPM and HBPM over office blood pressure measurement is well documented in both cross-sectional and longitudinal studies [3, 16–19]. As shown in Fig. 1, several studies of the prognosis of masked hypertension suggest that it portends risks for cardiovascular morbidity and mortality that are comparable to the risks of sustained hypertension, both being much higher than those of normotensive patients [3, 20–27]. Verdecchia et al. [26, 27] and Pickering and James [23], for example, assessed the long-term prognosis of masked hypertension using an international ambulatory blood pressure database, including data from the New York Prognostic Effects of ABPM (NYPEAP); the Progetto Ipertensione Umbria Monitoraggio Ambulatoriale (PIUMA) from Italy [25, 27]; and the Ohasama study [22] and the Jichi Medical School (JMS)–ABPM Study Wave 1 [21, 28], both from Japan. In total, 1,272 individuals had normal office blood pressure (<140/90 mm Hg), of whom 376 had high daytime ambulatory blood pressure (>135/85 mm Hg); all others were normotensive by both criteria. The authors found that the rate of cardiovascular events was higher in individuals with masked hypertension than in those with normal blood pressure (HR, 2.26; P<0.0009) [23]. Several studies [16, 21–26, 29, 30]—although not all [31, 32]—have confirmed these findings. The International Database of Ambulatory Blood Pressure in relation to Cardiovascular Outcome (IDACO) group, for example, assessed the risk of masked hypertension in 7,030 individuals randomly recruited from Belgium, Denmark, Japan, and Sweden [32]. In multivariable analyses, with true normotension as the reference, the adjusted hazard ratios for all cardiovascular events were 1.22 (95% CI, 0.96–1.53) for white-coat hypertension, 1.62 (95% CI, 1.35–1.96) for masked hypertension, and 1.80 (95% CI, 1.59–2.03) for sustained hypertension [32]. Also, in the SHEAF (Self-Measurement of Blood Pressure at Home in the Elderly: Assessment and Follow-up) study [16], using controlled hypertension as the reference group, the relative risk of cardiovascular events was 1.96 in patients with uncontrolled hypertension, (95% CI, 1.27–3.02) and 2.06 in those with masked hypertension (95% CI, 1.22–3.47) compared with patients with white-coat hypertension, whose relative risk was 1.18 (95% CI, 0.67–2.10). A Swedish study of untreated elderly men also observed a higher cardiovascular risk in patients with masked hypertension than in normotensive individuals [29]. During the follow-up, the incidence of cardiovascular events (number of cases per 100 patient-years) was 0.99 for normotensive individuals, 2.74 for those with masked hypertension, and 3.14 for hypertensive patients. In a multivariate analysis, using normotensive subjects as the reference, masked hypertension (HR, 2.77; 95% CI, 1.15–6.68) and hypertension (HR, 2.94, 95% CI, 1.49–5.82) were significant predictors of cardiovascular morbidity [29].
Fig. 1.
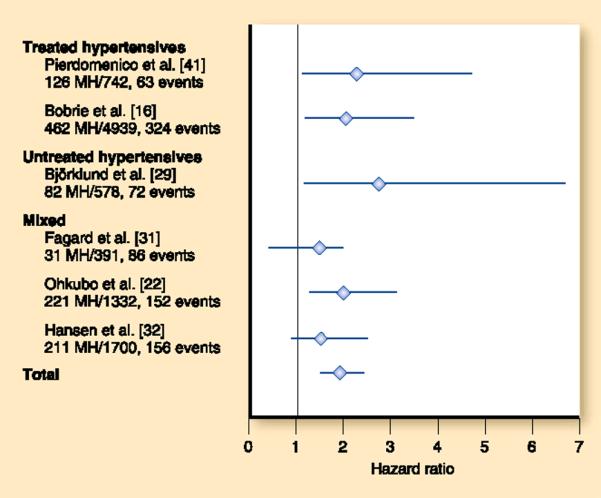
Cardiovascular prognosis of masked hypertension. This shows a meta-analysis of the six cohort studies comparing quantitative data for the cardiovascular prognosis of patients with masked hypertension with data for normotensive individuals or patients with controlled hypertension. The boxes and horizontal lines represent the hazard ratio and 95% confidence interval for each cohort. MH—masked hypertension. (Adapted from Bobrie et al. [3], with permission)
Impact of Masked Hypertension on Target Organ Damage
Several studies have examined target organ damage in the context of the four types of blood pressure status (normotension, white-coat hypertension, masked hypertension, and sustained hypertension), with a particular focus on the relationship between masked hypertension and target organ damage. Liu and colleagues [33] first brought attention to the issue of target organ damage in masked hypertension in 1999. In this seminal study of 61 masked hypertensives, 64 sustained hypertensives, and 234 true normotensives, patients with masked hypertension had a left ventricular mass index (LVMI) that was on average 13 g/m2 higher than in normotensives (95% CI, 8–18 g/m2) and more prevalent carotid plaque (28%) than true normotensives (15%) (P<0.05); those with masked hypertension thus were similar to the sustained hypertensives [33]. Subsequent studies, summarized below, have since examined target organ damage in patients with masked hypertension, considering antihypertensive treatment status and masked hypertension in children.
Target Organ Damage and Masked Hypertension in Untreated Populations
Studies with untreated individuals have generally confirmed the findings of Liu et al. [33] and found that masked hypertensives have more target organ damage than true normotensives; they have levels of target organ damage comparable to those of sustained hypertensives or have intermediate levels between true normotensives and sustained hypertensives [34–36]. An analysis from the PAMELA study, a longitudinal epidemiologic study of 3,200 Italian men and women (of whom 1,637 were untreated) demonstrated a higher LVMI and higher prevalence of left ventricular hypertrophy (LVH) among masked hypertensives than among true normotensives, but lower LVMI and LVH prevalence than among sustained hypertensives [36]. In a study of 1,535 untreated individuals, Kotsis et al. [34] found that masked hypertensives on average had higher LVMI and carotid intima media thickness (cIMT) than normotensives. In their study of 282 untreated individuals, Matsui et al. [35] reported that cIMT was highest among masked hypertensives compared with the other categories of hypertensive individuals (mean, 1.01±0.17 mm for masked hypertension vs 0.84±0.16 mm for normotension; P<0.001). Additionally, masked hypertensives had significantly higher pulse wave velocity (PWV, a measure of arterial stiffness) than normotensives (1949±266 cm/sec vs 1677±298 cm/sec; P<0.001), but the PWV for masked hypertensives was comparable to that of sustained hypertensives (2028±305 cm/sec) [35].
A few studies in untreated patients have not demonstrated a consistent relationship between target organ damage and masked hypertension [29, 37, 38]. In the Uppsala Longitudinal Study of Adult Men, a population-based cohort study of untreated elderly men, masked hypertensives and true normotensives had a similar mean LVMI. However, masked hypertensives had higher relative wall thickness than both the normotensive and sustained hypertensive groups, suggestive of more concentric remodeling (a precursor of concentric LVH) in the masked hypertensives than in the other groups [29]. Bombelli et al. [37], in an analysis of 1,653 untreated individuals of the PAMELA cohort, did not find an association between masked hypertension and left ventricular mass. Ormezzano et al. [38] found no significant differences in LVMI between masked hypertensives and the normotensive group (81.1±21.7 g/m2 vs 79.3±16.7 g/m2; P=0.99) and no differences in intima media thickness (664±107 μm vs 626±75 μm). However, among the 136 patients of this cohort with measurements for PWV, masked hyper-tensives had a statistically higher PWV (9.58±1.55 m/sec) than normotensives (8.59±1.38 m/sec).
Target Organ Damage and Masked Hypertension in Treated Patients
Masked hypertension in treated patients suggests inadequate treatment and poor blood pressure control, so it is not surprising that several studies demonstrate more target organ damage in treated patients with masked hypertension than in those whose blood pressure is controlled. For example, in a prospective study of 80 nondiabetic hyper-tensive patients on antihypertensive treatment with a mean follow-up of 30 months, a decrease in LVMI (117±23 g/m2 at baseline, 95±22 g/m2 at follow-up; P<0.01), prevalence of LVH with concentric remodeling (45% at baseline, 19.5% at follow-up; P<0.01), and microalbuminuria (13.9% prevalence at baseline, 3.9% at follow-up; P< 0.05) was seen in patients who achieved BP control on ambulatory and clinic measurements [39]. The masked hypertension group (ie, the group that did not achieve ambulatory control) showed no significant improvement in cardiac structure (mean LVMI, 114±25 g/m2 at baseline, 102±20 g/m2 at follow-up; P = NS), prevalence of LVH with concentric remodeling (46.0% at baseline, 34.4% at follow-up; P = NS), or microalbuminuria (13.7% prevalence at baseline, 10.3% at follow-up; P = NS) [39]. Among hypertensive diabetics with mild to moderate kidney disease, those with masked hypertension had higher LVMI (138±15 g/m2) than those with well-controlled hypertension (105±8 g/m2)[40]. Pierdomenico et al. [41] found that treated patients with masked hypertension were almost twice as likely to have LVH and had double the cardiac event rate, compared with the well-controlled group. Tomiyama et al. [42] reported that masked hypertension was an independent determinant of LVH (β=0.136, P= 0.01), carotid atherosclerosis (β=0.157, P=0.003), and albuminuria (β=0.114, P=0.042) among 332 treated patients in Japan. Finally, in a recent analysis of 617 patients in the African American Study of Kidney Disease (AASK) trial, Pogue et al. [43••] reported higher left ventricular mass and prevalence of LVH among masked hypertensives compared with true normotensives (LVH prevalence, 69.8% vs 54.1% respectively; P<0.01).
Target Organ Damage and Masked Hypertension in the Young
A small number of studies have examined target organ damage and masked hypertension in children and adolescents [44•, 45]. Lurbe et al. [5] studied 234 youths ranging in age from 6 years to 18 years (mean, 10 years), comprising 200 normotensives and 34 youths with masked hypertension. Masked hypertensives had significantly higher LVMI than normotensives (34.9±8.8 g/m2.7 vs 29.6±4.8 g/m2.7 respectively, P=0.023). About 9% of the masked hypertensive children progressed to sustained hypertension by the 12-month follow-up, whereas none of the normotensive children progressed to sustained hyper-tension [5]. In another study of 85 children referred to a hypertension referral center in Athens, Greece, Stabouli et al. [45] found that those with masked hypertension had significantly higher left ventricular mass than normotensive children (31.9±2.9 g/m2.7 vs 25.3±5.6 g/m2.7, P<0.05), but they found no differences in carotid intima media thickness.
Treatment of Patients with Hypertension Reduces Cardiovascular Risk and Complications
There is abundant evidence from rigorous clinical trials that treatment of patients with hypertension leads to significant reduction in cardiovascular morbidity and mortality, as well as prevention of target organ damage [14]. Most of the cardiovascular risk reduction has been attributed to blood pressure reduction rather than to the specific antihypertensive agents. It is thus logical that treatment of patients with masked hypertension, which portends similar risk as sustained hypertension, should yield comparable reduction in cardiovascular morbidity and mortality. It would be ideal to have evidence from clinical trials that treatment of patients with masked hypertension will lead to significant reductions in cardiovascular morbidity and mortality, but the lack of such evidence does not obviate the need to treat this group of patients, especially given the epidemiologic data, which strongly suggest that the relationship between blood pressure and cardiovascular risk is continuous [46]. Furthermore, patients with masked hypertension are undoubtedly hypertensive by out-of-office measurement, and their risk of cardiovascular events and mortality is strikingly similar to the risk in patients with sustained hypertension. Thus, we will be remiss in withholding treatment from this group.
Proposed Treatment Algorithm for Patients with Masked Hypertension
Now that we have made the argument that patients with masked hypertension should be treated, based on the increased cardiovascular risk and target organ damage, what should a treatment algorithm look like? Figure 2 depicts a proposed algorithm. All patients who have high normal office blood pressure (130–139/85–89 mmHg) should undergo HBPM or 24-h ABPM to rule out masked hypertension. If patients are found to have masked hypertension (>135/85 mm Hg by either HBPM or ABPM), the 24-h ABPM should be repeated within 2 months, to confirm the diagnosis (similar to the recommendation for diagnosis of hypertension). Those patients whose HBPM reading lies in the range of 125–135/76–84 mm Hg should undergo confirmatory ABPM, because the rate of masked hypertension is much higher in patients whose blood pressure is in the high range of prehypertension [47, 48]. Once masked hypertension is confirmed, patients should undergo comprehensive cardiovascular risk assessment (including ECG, fasting lipid profile, fasting glucose, basic metabolic profile, and urinalysis), and they should be treated with antihypertensive medications, similar to patients with sustained hypertension.
Fig. 2.
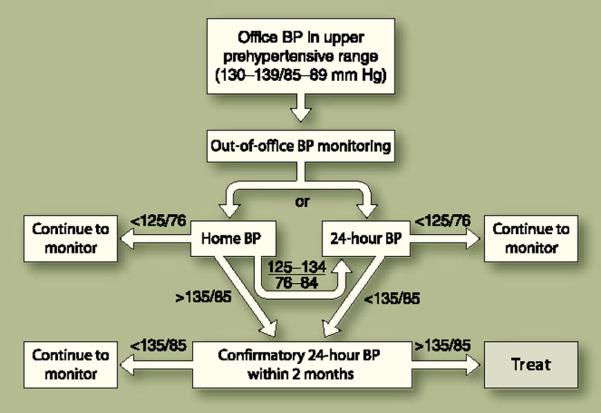
Algorithm for evaluating and treating masked hypertension. BP—blood pressure
Pitfalls of the Proposed Algorithm
Two important caveats should be noted in using the proposed algorithm. The first (and probably the most important) issue in masked hypertension is the reproducibility of measurements. Only two published studies have examined this issue: In the study by Lurbe et al. [5], the diagnosis of masked hypertension persisted in 40% of the children studied over a 3-year period. In the second study, of 2,189 treated hypertensive patients, the prevalence of masked hypertension on two separate occasions (13±9 days apart) based on office monitoring, and HBPM increased from 11% to 17%, with a diagnostic agreement (the total number of patients classified identically by the clinical measurement) of 74% and 75% on the two occasions [49].
The second issue is how patients with masked hypertension can best be identified in the office setting, given that they all have normal office blood pressure. Proper identification of patients requires adequate risk stratification, because screening all patients with normal office blood pressure would be prohibitively expensive and unsustainable in any healthcare system. One approach proposed is to screen only those patients whose office blood pressure is just under the upper limit of normal, given that the office blood pressure of most patients with masked hypertension (especially smokers and the young) is in the high normal range [48]. Furthermore, the proposed algorithm addresses this issue by confirming the masked hypertension diagnosis with a repeat ABPM measurement at least 2 months after the initial diagnosis.
Conclusions
There are three major reasons to treat hypertension: to reduce target organ damage, to reduce cardiovascular risk, and to prevent complications. All three conditions are satisfied by recent data indicating that patients with masked hypertension have higher target organ damage than normotensives and a cardiovascular risk profile similar to the profile of patients with sustained hypertension. The pitfalls lie largely in the need to identify patients who are at high risk for masked hypertension and the lack of data on the reliability and reproducibility of the diagnosis of masked hypertension.
Acknowledgment
Drs. Ogedegbe's work is supported by funding from the National Institutes of Health (R01 HL078566 and R01 HL087301). Dr. Ravenell's work is supported by the American Heart Association Pharmaceutical Roundtable Award (Grant #0675069N) and the Robert Wood Johnson Foundation Amos Medical Faculty Development Award (Grant #66731).
Footnotes
Disclosure No potential conflicts of interest relevant to this article were reported.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Pickering T. “White coat hypertension”—Should it be treated or not? Cleve Clin J Med. 2002;69:584–585. doi: 10.3949/ccjm.69.8.584. [DOI] [PubMed] [Google Scholar]
- 2.Pickering TG, Davidson K, Gerin W, Schwartz JE. Masked hypertension. Hypertension. 2002;40:795–796. doi: 10.1161/01.hyp.0000038733.08436.98. [DOI] [PubMed] [Google Scholar]
- 3.Bobrie G, Clerson P, Menard J, et al. Masked hypertension: a systematic review. J Hypertens. 2008;26:1715–1725. doi: 10.1097/HJH.0b013e3282fbcedf. [DOI] [PubMed] [Google Scholar]
- 4.Verberk WJ, Kessels AG, de Leeuw PW. Prevalence, causes, and consequences of masked hypertension: a meta-analysis. Am J Hypertens. 2008;21:969–975. doi: 10.1038/ajh.2008.221. [DOI] [PubMed] [Google Scholar]
- 5.Lurbe E, Torro I, Alvarez V, et al. Prevalence, persistence, and clinical significance of masked hypertension in youth. Hypertension. 2005;45:493–498. doi: 10.1161/01.HYP.0000160320.39303.ab. [DOI] [PubMed] [Google Scholar]
- 6.Matsuoka S, Awazu M. Masked hypertension in children and young adults. Pediatr Nephrol. 2004;19:651–654. doi: 10.1007/s00467-004-1459-3. [DOI] [PubMed] [Google Scholar]
- 7.Pickering TG, Shimbo D, Haas D. Ambulatory blood-pressure monitoring. N Engl J Med. 2006;354:2368–2374. doi: 10.1056/NEJMra060433. [DOI] [PubMed] [Google Scholar]
- 8.Ogedegbe G. Causal mechanisms of masked hypertension: socio-psychological aspects. Blood Press Monit. 2010;15:90–92. doi: 10.1097/MBP.0b013e3283380df5. [DOI] [PubMed] [Google Scholar]; • This paper gives a thorough review of the literature in terms of the psychosocial and causal mechanisms of masked hypertension, based largely on the work of Dr. Thomas Pickering.
- 9.Aksoy I, Deinum J, Lenders JW, Thien T. Does masked hypertension exist in healthy volunteers and apparently well-controlled hypertensive patients? Neth J Med. 2006;64:72–77. [PubMed] [Google Scholar]
- 10.Obara T, Ohkubo T, Kikuya M, et al. Prevalence of masked uncontrolled and treated white-coat hypertension defined according to the average of morning and evening home blood pressure value: from the Japan Home Versus Office Measurement Evaluation Study. Blood Press Monit. 2005;10:311–316. doi: 10.1097/00126097-200512000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Ogedegbe G, Pickering TG, Clemow L, et al. The misdiagnosis of hypertension: the role of patient anxiety. Arch Intern Med. 2008;168:2459–2465. doi: 10.1001/archinte.168.22.2459. [DOI] [PMC free article] [PubMed] [Google Scholar]; •• This paper is the first to assess the role of conditioned response in the development of white coat and masked hypertension. The authors tested and proved the hypothesis that the white coat effect is a conditioned response as opposed to a manifestation of general anxiety.
- 12.Wang GL, Li Y, Staessen JA, et al. Anthropometric and lifestyle factors associated with white-coat, masked and sustained hypertension in a Chinese population. J Hypertens. 2007;25:2398–2405. doi: 10.1097/HJH.0b013e3282efeee7. [DOI] [PubMed] [Google Scholar]
- 13.Ungar A, Pepe G, Monami M, et al. Isolated ambulatory hypertension is common in outpatients referred to a hypertension centre. J Hum Hypertens. 2004;18:897–903. doi: 10.1038/sj.jhh.1001756. [DOI] [PubMed] [Google Scholar]
- 14.Lenfant C, Chobanian AV, Jones DW, Roccella EJ. Seventh report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7): resetting the hypertension sails. Hypertension. 2003;41:1178–1179. doi: 10.1161/01.HYP.0000075790.33892.AE. [DOI] [PubMed] [Google Scholar]
- 15.Pickering TG, Miller NH, Ogedegbe G, et al. Call to action on use and reimbursement for home blood pressure monitoring: executive summary: a joint scientific statement from the American Heart Association, American Society Of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension. 2008;52:1–9. doi: 10.1161/HYPERTENSIONAHA.107.189011. [DOI] [PubMed] [Google Scholar]
- 16.Bobrie G, Chatellier G, Genes N, et al. Cardiovascular prognosis of “masked hypertension” detected by blood pressure self-measurement in elderly treated hypertensive patients. JAMA. 2004;291:1342–1349. doi: 10.1001/jama.291.11.1342. [DOI] [PubMed] [Google Scholar]
- 17.Imai Y. Prognostic significance of ambulatory blood pressure. Blood Press Monit. 1999;4:249–256. [PubMed] [Google Scholar]
- 18.Perloff D, Sokolow M, Cowan R. The prognostic value of ambulatory blood pressures. JAMA. 1983;249:2792–2798. [PubMed] [Google Scholar]
- 19.Pickering TG, White WB, Giles TD, et al. When and how to use self (home) and ambulatory blood pressure monitoring. J Am Soc Hypertens. 2010;4:56–61. doi: 10.1016/j.jash.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 20.Kario K, Pickering TG, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107(10):1401–1406. doi: 10.1161/01.cir.0000056521.67546.aa. [DOI] [PubMed] [Google Scholar]
- 21.Kario K, Shimada K, Schwartz JE, et al. [Silent and clinically overt stroke in older Japanese subjects with white-coat and sustained hypertension] [in Japanese] J Cardiol. 2002;39:52–54. [PubMed] [Google Scholar]
- 22.Ohkubo T, Hozawa A, Nagai K, et al. Prediction of stroke by ambulatory blood pressure monitoring versus screening blood pressure measurements in a general population: the Ohasama study. J Hypertens. 2000;18:847–854. doi: 10.1097/00004872-200018070-00005. [DOI] [PubMed] [Google Scholar]
- 23.Pickering TG. Should doctors still measure blood pressure? J Clin Hypertens (Greenwich) 2006;8:394–396. doi: 10.1111/j.1524-6175.2006.05154.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pickering TG, James GD. Ambulatory blood pressure and prognosis. J Hypertens Suppl. 1994;12:S29–S33. [PubMed] [Google Scholar]
- 25.Verdecchia P, Porcellati C, Schillaci G. Ambulatory blood pressure. An independent predictor of prognosis in essential hypertension. Hypertension. 1994;24:793–801. doi: 10.1161/01.hyp.24.6.793. [DOI] [PubMed] [Google Scholar]
- 26.Verdecchia P, Reboldi GP, Angeli F, et al. Short- and long-term incidence of stroke in white-coat hypertension. Hypertension. 2005;45:203–208. doi: 10.1161/01.HYP.0000151623.49780.89. [DOI] [PubMed] [Google Scholar]
- 27.Verdecchia P, Schillaci G, Borgioni C, et al. White-coat hypertension. Lancet. 1996;348:1444–1445. doi: 10.1016/S0140-6736(04)70084-7. [DOI] [PubMed] [Google Scholar]
- 28.Kario K, Ishikawa J, Pickering TG, et al. Morning hypertension: the strongest independent risk factor for stroke in elderly hypertensive patients. Hypertens Res. 2006;29:581–587. doi: 10.1291/hypres.29.581. [DOI] [PubMed] [Google Scholar]
- 29.Bjorklund K, Lind L, Zethelius B, et al. Isolated ambulatory hypertension predicts cardiovascular morbidity in elderly men. Circulation. 2003;107:1297–1302. doi: 10.1161/01.cir.0000054622.45012.12. [DOI] [PubMed] [Google Scholar]
- 30.Clement DL, De Buyzere ML, De Bacquer DA. Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med. 2003;348:2407–2415. doi: 10.1056/NEJMoa022273. [DOI] [PubMed] [Google Scholar]
- 31.Fagard RH, Van Den Broeke C, De Cort P. Prognostic significance of blood pressure measured in the office, at home and during ambulatory monitoring in older patients in general practice. J Hum Hypertens. 2005;19:801–807. doi: 10.1038/sj.jhh.1001903. [DOI] [PubMed] [Google Scholar]
- 32.Hansen TW, Jeppesen J, Rasmussen S, et al. Ambulatory blood pressure and mortality: a population-based study. Hypertension. 2005;45:499–504. doi: 10.1161/01.HYP.0000160402.39597.3b. [DOI] [PubMed] [Google Scholar]
- 33.Liu JE, Roman MJ, Pini R, et al. Cardiac and arterial target organ damage in adults with elevated ambulatory and normal office blood pressure. Ann Intern Med. 1999;131:564–572. doi: 10.7326/0003-4819-131-8-199910190-00003. [DOI] [PubMed] [Google Scholar]
- 34.Kotsis V, Stabouli S, Toumanidis S, et al. Target organ damage in “white coat hypertension” and “masked hypertension”. Am J Hypertens. 2008;21:393–399. doi: 10.1038/ajh.2008.15. [DOI] [PubMed] [Google Scholar]
- 35.Matsui Y, Eguchi K, Ishikawa J, et al. Subclinical arterial damage in untreated masked hypertensive subjects detected by home blood pressure measurement. Am J Hypertens. 2007;20:385–391. doi: 10.1016/j.amjhyper.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 36.Sega R, Trocino G, Lanzarotti A. Alterations of cardiac structure in patients with isolated office, ambulatory, or home hypertension: Data from the general population (Pressione Arteriose Monitorate E Loro Associazioni [PAMELA] Study) Circulation. 2001;104:1385–1392. doi: 10.1161/hc3701.096100. [DOI] [PubMed] [Google Scholar]
- 37.Bombelli M, Sega R, Facchetti R. Prevalence and clinical significance of a greater ambulatory versus office blood pressure (`reversed white coat' condition) in a general population. J Hypertens. 2005;23:513–520. doi: 10.1097/01.hjh.0000160206.58781.07. [DOI] [PubMed] [Google Scholar]
- 38.Ormezzano O, Baguet JP, Francois P, et al. Is there any real target organ damage associated with white-coat normotension? Clin Auton Res. 2004;14:160–166. doi: 10.1007/s10286-004-0174-2. [DOI] [PubMed] [Google Scholar]
- 39.Cuspidi C, Meani S, Fusi V, et al. Isolated ambulatory hypertension and changes in target organ damage in treated hypertensive patients. J Hum Hypertens. 2005;19:471–477. doi: 10.1038/sj.jhh.1001850. [DOI] [PubMed] [Google Scholar]
- 40.Kuriyama S, Otsuka Y, Iida R, et al. Morning blood pressure predicts hypertensive organ damage in patients with renal diseases: effect of intensive antihypertensive therapy in patients with diabetic nephropathy. Intern Med. 2005;44:1239–1246. doi: 10.2169/internalmedicine.44.1239. [DOI] [PubMed] [Google Scholar]
- 41.Pierdomenico SD, Lapenna D, Bucci A, et al. Cardiovascular outcome in treated hypertensive patients with responder, masked, false resistant, and true resistant hypertension. Am J Hypertens. 2005;18:1422–1428. doi: 10.1016/j.amjhyper.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 42.Tomiyama M, Horio T, Yoshii M, et al. Masked hypertension and target organ damage in treated hypertensive patients. Am J Hypertens. 2006;19:880–886. doi: 10.1016/j.amjhyper.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 43.Pogue V, Rahman M, Lipkowitz M, et al. Disparate estimates of hypertension control from ambulatory and clinic blood pressure measurements in hypertensive kidney disease. Hypertension. 2009;53:20–27. doi: 10.1161/HYPERTENSIONAHA.108.115154. [DOI] [PubMed] [Google Scholar]; •• Some studies indicate that treated hypertensive patients may have masked hypertension. This study evaluated and characterized the prevalence of masked hypertension among patients with chronic kidney disease who were enrolled in the African American Study of Kidney Disease. The findings from this report lend credence to the fact that patients with chronic kidney disease often have undetected elevated blood pressure at home.
- 44.Lurbe E. Masked hypertension in children and adolescents. Curr Hypertens Rep. 2008;10(3):165–166. doi: 10.1007/s11906-008-0030-1. [DOI] [PubMed] [Google Scholar]; • The data on the effect of masked hypertension on target organ damage in children is limited. This author reports a positive correlation between masked hypertension and left ventricular mass index (LVMI) such that children with masked hypertension have a higher LVMI. This review also assesses the reproducibility of the diagnosis of masked hypertension.
- 45.Stabouli S, Kotsis V, Toumanidis S, et al. White-coat and masked hypertension in children: association with target-organ damage. Pediatr Nephrol. 2005;20:1151–1155. doi: 10.1007/s00467-005-1979-5. [DOI] [PubMed] [Google Scholar]
- 46.Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 47.Gu Q, Burt VL, Paulose-Ram R, et al. High blood pressure and cardiovascular disease mortality risk among U.S. adults: the third National Health and Nutrition Examination Survey mortality follow-up study. Ann Epidemiol. 2008;18:302–309. doi: 10.1016/j.annepidem.2007.11.013. [DOI] [PubMed] [Google Scholar]
- 48.Pickering TG. The natural history of hypertension: prehypertension or masked hypertension? J Clin Hypertens (Greenwich) 2007;9:807–810. doi: 10.1111/j.1751-7176.2007.tb00011.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bobrie G, Clerson P, Cuchet A, et al. [Prevalence and mechanism of masked hypertension: the OL'MESURES survey] [in French] Arch Mal Coeur Vaiss. 2006;99:760–763. [PubMed] [Google Scholar]


