Abstract
Background/Aims
Benign bronchoesophageal fistula (BEF) is a rare condition that is usually treated surgically; however, less invasive endoscopy procedures have been attempted to overcome the disadvantages of surgery. The aim of this study was thus to determine the results of endoscopic management as a primary treatment in patients with BEF.
Methods
We retrospectively analyzed data from 368 patients with BEF who were treated at a tertiary care, academic medical center between January 2000 and August 2009.
Results
Benign causes were found for only 18 of the 368 patients. Of these, seven were treated endoscopically and the others by surgery or other methods. The first endoscopy procedures failed in all seven patients, with second trials of endoscopy performed in four patients at a median of 8 days (range, 3 to 11 days) after the first procedure. The second endoscopic procedure was successful in two out of four patients; one patient showed no recurrence of the fistula, whereas the second patient experienced a recurrence after 24 months. All patients underwent successful surgical procedures after the failure of endoscopic treatment, with no further recurrences.
Conclusions
Although we observed a low rate of success for primary endoscopic treatment of benign BEF, the invasive nature of surgery suggests the need for a prospective study with a large number of patients to evaluate the efficacy of less invasive procedures such as endoscopic treatment.
Keywords: Esophageal fistula, Endoscopy, Fibrin glue
INTRODUCTION
Fistulas, although rare, may develop between the esophageal lumen and other mediastinal structures. These bronchoesophageal fistulas (BEFs) may be due to congenital or acquired causes. Most fistulas in adults are acquired because it is rare for a congenital fistula to remain asymptomatic until adulthood. Most acquired fistulas are caused by malignancies, either by a metastatic deposit or via direct invasion of a tumor. Fistulas may also be due to benign causes, including infections, such as tuberculosis and histoplasmosis, trauma, and other causes.1-5 Owing to their nonspecific symptoms and rarity, however, benign BEF may be present for a long time without being diagnosed and properly treated, resulting in significant morbidity and death.
Most patients with fistula are treated surgically, with removal of the fistula and any permanently damaged lung segments. The standard operative procedure involves a thoracotomy, during which the fistula is exposed and divided and the defects in the bronchus and the esophagus are repaired by interposition of viable tissue between the suture lines.3,6
Several reports have described attempts to repair fistulas by endoscopic methods, thus avoiding the complications and sequelae of surgery.4,7-11 These methods include the application of fibrin glue, sodium hydroxide and acetic acid, which have been used to close fistulas in both adults and children.7,8,10,11 Being biocompatible, fibrin glue can be repeatedly applied and also does not inhibit any subsequent surgical intervention. Other reports have described the use of hemoclips.4,9 To our knowledge, however, there have been few reports about the success rate of endoscopic treatment for the primary treatment of benign BEF in adults. We therefore report here our experience in the primary endoscopic management of patients with benign BEF.
MATERIALS AND METHODS
1. Patients
We examined the medical records of patients who underwent BEF between January 2000 and August 2009 at the Asan Medical Center. Of the 368 patients who underwent BEF, only 18 (4.8%) did so for benign BEF. Of these, 7 patients were treated endoscopically and 11 were treated surgically or by other methods. With the approval of our institutional review board, the charts of these patients were retrospectively reviewed.
Patients were excluded from the study if they were younger than 20 years old, if they had been diagnosed with a tracheoesophageal fistula caused by an endotracheal or tracheostomy tube, if they had a current history of malignancy related to the fistula or a history of congenital fistula, or had previously been treated for fistulas by bronchofibroscopy or stent insertion.
2. Endoscopic technique
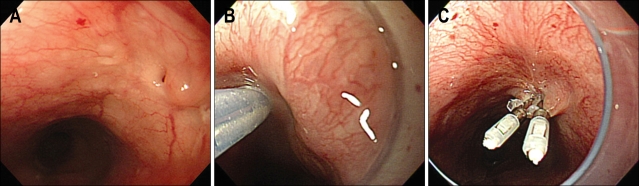
These procedures were performed by expert endoscopists with the patient under conscious sedation with intravenous administration of midazolam. Following administration of local pharyngeal anesthesia, the endoscope was inserted into the esophagus until it reached the opening site of the fistula. Fibrin glue (Beriplast; Aventis Behring Ltd., Marburg, Germany), consisting of a solution of fibrinogen (one vial of fibrinogen concentrate and one vial of aprotinin solution) and thrombin (one vial of human thrombin and one vial of calcium chloride), was injected into the opening site and/or the metal hemoclips (HX-600-090L; Olympus Optical Co., Ltd, Tokyo, Japan) (Fig. 1).
Fig. 1.
(A) Fistula opening located 31 cm from the upper incisor. (B) Injection of fibrin glue into the area of the fistula opening. (C) Application of two hemoclips to the site of the fistula opening after the injection of fibrin glue.
3. Statistical analysis
Quantitative variables with a normal distribution are expressed as mean±standard deviation, whereas quantitative variables with skewed distributions are expressed as median (range). The χ2 test, or Fisher's exact test if necessary, was used to compare relative frequencies of categorical variables and the Student's t-test or the Mann-Whitney U-test was used to compare continuous variables. A p-value of <0.05 was considered significant. All statistical analyses were performed using the SPSS program, version 12.0 (SPSS Inc, Chicago, IL, USA).
RESULTS
Over a 10-year treatment period, 18 patients (13 women, 5 men), of median age 58.5 years (range, 28 to 86 years) were included in this study (Table 1). All 18 patients underwent esophagography, computed tomography (CT), endoscopy, and bronchoscopy for the diagnosis of benign BEF. Of these patients, 7 (6 women, 1 man), of median age 67 years (range, 50 to 86 years), underwent primary endoscopic treatment, whereas 9 underwent primary surgical treatment. Of the remaining two patients, one was treated radiologically by fibrin glue injection and one was observed while receiving treatment with anti-tuberculosis medication.
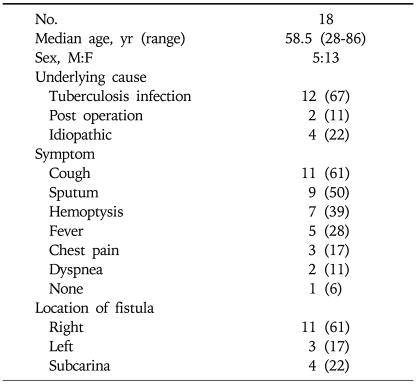
Table 1.
Baseline Characteristics of Benign Bronchoesophageal Fistula Patients
Data represent number of patients (% of total population).
1. Etiology
Of the 18 BEFs, 12 were caused by infection, 2 were postoperative complications and 4 were idiopathic. The 12 patients with BEFs due to infection had pulmonary tuberculosis, with BEF developing after cure of tuberculosis in 8 patients. Four patients, however, were diagnosed with pulmonary tuberculosis owing to BEF. The median duration from the diagnosis of tuberculous infection to the onset of fistula symptoms in the 8 patients who developed BEF after cure of tuberculosis was 14.5 years (range, 5 to 30 years). Of the two patients who developed BEF after surgery, one had a lung tumor that had been removed by pneumonectomy, with no recurrence over 8 years, and the other had a history of pneumothorax, which had previously been treated by chest tube insertion 35 years previously. In the remaining four patients, we found no etiology of fistula (Table 1).
2. Symptoms
Eleven patients presented with a cough that lasted from 4 days to more than 8 years. Seven patients reported a mild hemoptysis that lasted from 20 days to more than 1 year prior to diagnosis. Among the various symptoms were cough, sputum, hemoptysis, fever, chest pain, and dyspnea, which were single or combined (Table 1). In the 12 patients with BEF resulting from tuberculosis infection, the median symptom duration was 30 days (range, 4 days to 2 years). In three patients with idiopathic BEF, symptoms lasted from 20 days to 5 years. The fourth patient with idiopathic BEF had no symptoms; in this patient, BEF was detected during a routine examination.
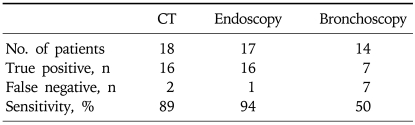
3. Diagnosis
The confirmative diagnosis was established by esophagography in all patients (Fig. 2). In contrast, CT, endoscopy, and bronchoscopy failed to reveal BEFs in 2, 1 and 7 patients, respectively, making the sensitivity of CT, endoscopy, and bronchoscopy 89%, 94%, and 50%, respectively (Table 2). The mean fistula opening size in the 7 patients who underwent primary endoscopic treatment was 4.5 mm (range, 2 mm to 6 mm), with no significant difference in size between the patients treated endoscopically and surgically.
Fig. 2.
Esophagography showing the communication between the right lower lobar bronchus with the esophageal cleft in the middle of the esophagus, a finding compatible with a bronchoesophageal fistula.
Table 2.
Comparison of the Sensitivities of Computed Tomography, Endoscopy, and Bronchoscopy in Detecting Benign Bronchoesophageal Fistula
CT, computed tomography.
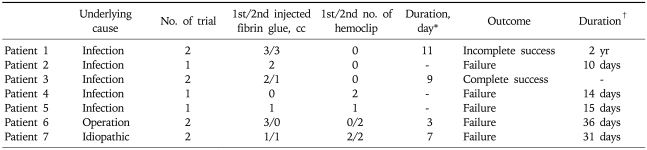
4. Management and outcomes
The first endoscopic treatment failed in all seven patients who underwent a primary endoscopic procedure. Four of these patients underwent a second endoscopic procedure, at a median 8 days (range, 3 to 11 days) after the first procedure. The second endoscopic procedure was successful in two of these four patients. One patient (no. 3) has shown no recurrence of fistula during 52 months of follow-up, whereas the second (no. 1) underwent surgery after 24 months because, although symptoms had disappeared, the fistula was still present (Table 3). The remaining three patients underwent surgery after endoscopic treatment failure, with no further recurrences at a median 52 months (range, 12 months to 62 months) of follow-up. Treatment outcomes are summarized in Table 4.
Table 3.
Outcomes Following Endoscopic Treatment of Bronchoesophageal Fistula
*Duration from first to second treatment; †Duration from endoscopic failure to operation.
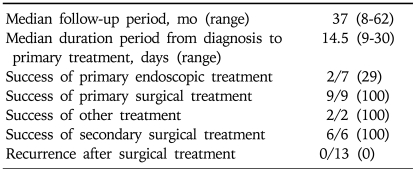
Table 4.
Outcomes Following Treatment of Bronchoesophageal Fistula
Data represent number of patients (% of total population).
DISCUSSION
BEF is a rare complication resulting from various diseases, with most BEFs in adults resulting from a locally advanced esophageal or bronchogenic malignancy. In contrast, benign BEFs can remain undiagnosed for years, owing to the combination of their rarity and their non-specific symptoms. A recent review of BEFs at Massachusetts General Hospital found that, over more than 40 years, only 228 cases were seen,3 with benign causes responsible for only 6%. Of the latter, 30% developed after esophageal surgery. Another study reported that mediastinal granulomatous inflammation caused by tuberculosis could account for 43% of benign BEFs.6 We observed that tuberculosis was the most common etiology of benign BEF, but at a higher rate (67%) than seen in other studies, which may be related to the high incidence of tuberculosis in Korea. Most patients with benign BEF present with non-specific physical findings. For example, the majority of patients with benign and congenital BEF have been found to present with a chronic cough lasting from 5 weeks to more than 30 years.3,6,12 We found that 61% of our patients presented with cough, and 11-50% presented with other symptoms, including sputum, hemoptysis, fever, chest pain, and/or dyspnea. Most symptoms were not severe and the duration from symptom development to presentation varied from 4 days to 8 years.
A diagnosis of BEF should be suspected in any patient presenting with a persistent unexplained cough or failing to improve after established medical therapy. Although various diagnostic modalities are available and complementary to each other, barium esophagography is regarded as a more sensitive and definitive diagnostic tool than endoscopic procedures.6,13,14 We also used esophagography as a confirmative diagnostic tool and we found that the sensitivities of CT, endoscopy, and bronchoscopy in diagnosing benign BEF were similar to previously reported findings.6
Once a BEF is confirmed, early surgical intervention is considered definitive, resulting in successful outcomes. Although early and definitive surgical repair has yielded promising results,5,6,15 the in-hospital mortality rate has been reported to be as high as 15.4%,3 and the surgery itself is invasive. This has led to the development of endoscopic and even medical treatment methods.4,7-11 For example, while covered esophageal-wall-stent placement has been described for malignant fistulas associated with stricture,16,17 esophageal stent insertion would probably not have been suitable for benign BEFs because the latter have no strictures to hold the stents in place. To date, there have been few reports about the results of primary endoscopic treatment for benign BEFs in adults. We found that the success rate was only 29%, with the two patients successfully treated requiring two endoscopic treatments each because the first treatment failed in both. The low success rate of endoscopic treatment may be associated with the length and width of the fistula tract. If it is straight and too short, the fibrin glue can be washed out to the bronchial space, whereas, if it is too wide, sufficient fibrin glue cannot be applied to fill the space. In our data, the mean length of the tract was 9.8±6.49 mm, the width was 3.4±1.14 in esophagographic findigs of failed patients and length was 18.0±15.56 mm, width was 1.5±0.71 in successful patients. But the shape of tract was not regular and number was too small, so we need more developed technique to evaluate the character of fistula and need large scaled studies to make criteria for initial endoscopic treatment in BEF. The low success rate of endoscopic treatment may also be associated with the degree of fistula tract maturation. Fixation of fibrin glue or hemoclipping is difficult in well epithelialized fistula tracts. Except for one patient with an idiopathic case fistula, the median time between underlying disease and the diagnosis of fistula in patients who failed primary endoscopic treatment was 8.5 years (range, 8 years to 28 years), whereas the time between underlying disease and the diagnosis of fistula was 2 years in the one patient with an incomplete successful endoscopic repair. Thus, although the number of patients is too small to generalize, shorter duration may be associated with a higher success rate of endoscopic treatment in BEF.
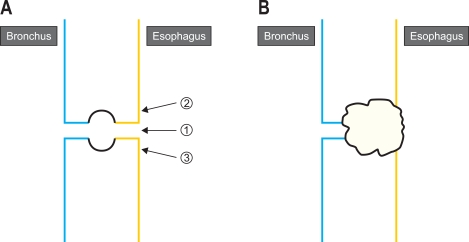
The method of fibrin glue injection is also important, however, there is no standard method. Usually we inject fibrin glue into the fistula in three directions, the first injection into the fistula opening site to seal the tract, and the second and third around the fistula site to help closing the tract by compression effect (Fig. 3).
Fig. 3.
The method of fibrin glue injection. (A) First injection into the opening site, and the second and third injections into the perifistula site. (B) Closing the fistula tract by sealing and compression with fibrin glue.
Although we found that the success rate of primary endoscopic procedure of benign BEFs was low, the number of patients was too small to generalize and the efficacy of this procedure cannot be excluded. Prospective studies with larger numbers are needed to assess this less invasive procedure.
ACKNOWLEDGEMENTS
The authors declare no conflict of interest. The authors confirm that there is no financial arrangement with anyone.
References
- 1.Woods D, Franic S, Lighter M, Bennett WF. Benign, atraumatic, bronchoesophageal fistulae. Can Assoc Radiol J. 1988;39:68–71. [PubMed] [Google Scholar]
- 2.Lado Lado FL, Golpe Gomez A, Cabarcos Ortiz de Barron A, Antunez Lopez JR. Bronchoesophageal fistulae secondary to tuberculosis. Respiration. 2002;69:362–365. doi: 10.1159/000063264. [DOI] [PubMed] [Google Scholar]
- 3.Mangi AA, Gaissert HA, Wright CD, et al. Benign broncho-esophageal fistula in the adult. Ann Thorac Surg. 2002;73:911–915. doi: 10.1016/s0003-4975(01)03582-2. [DOI] [PubMed] [Google Scholar]
- 4.Murdock A, Moorehead RJ, Tham TC. Closure of a benign bronchoesophageal fistula with endoscopic clips. Gastrointest Endosc. 2005;62:635–638. doi: 10.1016/j.gie.2005.06.023. [DOI] [PubMed] [Google Scholar]
- 5.Griffo S, Stassano P, Iannelli G, et al. Benign bronchoesophageal fistula: report of four cases. J Thorac Cardiovasc Surg. 2007;133:1378–1379. doi: 10.1016/j.jtcvs.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 6.Kim HK, Choi YS, Kim K, Kim J, Shim YM. Long-term results of surgical treatment in benign bronchoesophageal fistula. J Thorac Cardiovasc Surg. 2007;134:411–414. doi: 10.1016/j.jtcvs.2007.04.030. [DOI] [PubMed] [Google Scholar]
- 7.Smith DC. A congenital broncho-oesophageal fistula presenting in adult life without pulmonary infection. Br J Surg. 1970;57:398–400. doi: 10.1002/bjs.1800570518. [DOI] [PubMed] [Google Scholar]
- 8.Kohler B, Kohler G, Riemann JF. Spontaneous esophagotracheal fistula resulting from ulcer in heterotopic gastric mucosa. Gastroenterology. 1988;95:828–830. doi: 10.1016/s0016-5085(88)80035-0. [DOI] [PubMed] [Google Scholar]
- 9.Mizobuchi S, Kuge K, Maeda H, Matsumoto Y, Yamamoto M, Sasaguri S. Endoscopic clip application for closure of an esophagomediastinal-tracheal fistula after surgery for esophageal cancer. Gastrointest Endosc. 2003;57:962–965. doi: 10.1016/s0016-5107(03)70054-6. [DOI] [PubMed] [Google Scholar]
- 10.Ogunmola N, Wyllie R, McDowell K, Kay M, Mahajan L. Endoscopic closure of esophagobronchial fistula with fibrin glue. J Pediatr Gastroenterol Nutr. 2004;38:539–541. doi: 10.1097/00005176-200405000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Scappaticci E, Ardissone F, Baldi S, et al. Closure of an iatrogenic tracheo-esophageal fistula with bronchoscopic gluing in a mechanically ventilated adult patient. Ann Thorac Surg. 2004;77:328–329. doi: 10.1016/s0003-4975(03)01379-1. [DOI] [PubMed] [Google Scholar]
- 12.Kim JH, Park KH, Sung SW, Rho JR. Congenital bronchoesophageal fistulas in adult patients. Ann Thorac Surg. 1995;60:151–155. doi: 10.1016/s0003-4975(95)00326-6. [DOI] [PubMed] [Google Scholar]
- 13.Ramo OJ, Salo JA, Mattila SP. Congenital bronchoesophageal fistula in the adult. Ann Thorac Surg. 1995;59:887–889. doi: 10.1016/0003-4975(94)00957-9. [DOI] [PubMed] [Google Scholar]
- 14.Cherveniakov A, Tzekov C, Grigorov GE, Cherveniakov P. Acquired benign esophago-airway fistulas. Eur J Cardiothorac Surg. 1996;10:713–716. doi: 10.1016/s1010-7940(96)80329-0. [DOI] [PubMed] [Google Scholar]
- 15.Van Natta TL, Parekh KR, Reed CG, Shebrain SA, Omari BO. Benign esophagobronchial fistula with and without esophageal obstruction: two ends of the surgical spectrum. Ann Thorac Surg. 2008;85:322–325. doi: 10.1016/j.athoracsur.2007.07.069. [DOI] [PubMed] [Google Scholar]
- 16.Raijman I. Endoscopic management of esophagorespiratory fistulas: expanding our options with expandable stents. Am J Gastroenterol. 1998;93:496–499. doi: 10.1111/j.1572-0241.1998.496_b.x. [DOI] [PubMed] [Google Scholar]
- 17.Dumonceau JM, Cremer M, Lalmand B, Deviere J. Esophageal fistula sealing: choice of stent, practical management, and cost. Gastrointest Endosc. 1999;49:70–78. doi: 10.1016/s0016-5107(99)70448-7. [DOI] [PubMed] [Google Scholar]