Abstract
Purpose
This study aimed to identify 'objective' differential factors for normal frequent loose stool (NFLS) and diarrheal illness with dehydration and nutritional deficiency (DIDN) among infants with chronic frequent loose stool (CFLS).
Methods
Data were analyzed from infants under 2 years of age with CFLS who had been transferred from general pediatricians. These 46 patients were divided into 2 groups (NFLS versus DIDN). Nocturnal stool was defined as evacuation between 10 pm and 6 am. Maximal stool amount/day (measured using the mother's hand) was specified as the highest score during the period of CFLS obtained by adding up each evacuation's score (range, 0-2 points).
Results
There were 36 cases of NFLS and 10 of DIDN. A failure to gain weight (P=0.0001), fever (P=0.0079), colic/abdominal pain (P=0.0014), gross blood in stool (except allergic proctocolitis) (P=0.0113), nocturnal stool (P=0.0001), and the score of stool amount (P=0.0001) were found to significantly differentiate the groups. A failure to gain weight was observed in 39% of even NFLS. The frequency, mucus content, and microbiological findings of stools, as well as diaper dermatitis were not found to significantly differentiate the groups.
Conclusion
NFLS was more common than DIDN in infants with CFLS. The most 'objective' differential factors were nocturnal stool and the score of stool amount (≥7 points/day).
Keywords: Infant, Chronic disease, Diarrhea
Introduction
Diarrhea in infants has been defined 'objectively' as a stool weight in excess of 10 g/kg/day and 'symptomatically' as the increased frequency and liquidity of fecal discharge compared with usual habitus1, 2). In clinical terms, diarrhea is defined when dehydration and a failure to gain weight occur.
Although stool weight is the most accurate diagnostic standard of diarrhea3), it may be not useful under clinical circumstance. Thus, history-taking of frequency and consistency of stools is usually employed as a diagnostic method4). Generally, from 3 years of age, routine bowel evacuation occurs once or twice per day or two days, and the frequency of over three times a day and loose stools is suspected to indicate diarrheal illness with dehydration and nutritional deficiency (DIDN)1). However, to define diarrhea 'symptomatically' based on frequency and fluidity irrespective of stool amount can cause normal frequent and loose stool (NFLS) to be misdiagnosed as DIDN in infancy with diverse bowel habitus.
NFLS is common in infants with a shorter feeding interval and physiological characteristics of intestinal tract that are different from those of children and adults5, 6). Rapid alterations of evacuation patterns according to food application are also observed frequently in infants7). Therefore, parents and even clinicians often have difficulty in differentiating clearly between the normal state and DIDN in infants with chronic frequent and loose stool (CFLS). Furthermore, while it belongs to NFLS, iatrogenic nutritional deficiency owing to an inappropriate diet control can be diagnosed as DIDN, unnecessarily examined and treated.
This study was performed to differentiate the normal and diseased states in infants of less than two years of age with CFLS. The authors sought to identify 'objective' differential factors for NFLS and DIDN among patients with CFLS. We considered that the use of 'objective' factors could lessen parental anxiety and distress, iatrogenic undernutrition of patients, and socioeconomic loss due to improper medical investigations or inappropriate management of NFLS.
Materials and methods
1. Data collection and controls
We analyzed the data of infants (under two years of age) that had been transferred from general pediatricians at primary clinics or secondary hospitals in Daegu (Republic of Korea) from September to November in 2008, and had experienced CFLS for over 2 weeks.
Daegu is the third largest city in South Korea and has a population of 2.5 million. The region is serviced by 239 pediatricians; 153 working for 121 primary clinics, 44 for 14 secondary hospitals, and 42 for 5 tertiary teaching hospitals. The transferred patients were from 32 primary clinics and 6 secondary hospitals without a pediatric gastroenterologist. Transferences were made twice from 7 clinics and 3 hospitals. Hence, a total of 48 cases were transferred. The referred clinics or hospitals were distributed throughout the Daegu area, and thus, presumably well represented. Similarly, the ages and locations of their pediatricians showed no notable feature. Cases were recruited from among in- and outpatients at the Dongsan Medical Center (a tertiary hospital), Keimyung University School of Medicine. Two patients with immune deficiency and failure to thrive and with experience of surgical disease were excluded. Thus, we investigated the referred 46 cases, and in particular, NFLS to DIDN ratio, causal illnesses, frequencies of clinic or hospital visits and admissions, and history of nutritionally deficient diet management before enrolling in the study, and factors that differentiated NFLS and DIDN.
To determine the presence of nocturnal bowel movement, feeding method, frequency of bowel movements per day, and score of stool amount per day, we interviewed the mothers of healthy infants (under 2 years old) as controls who had visited baby clinics (at the Dongsan Medical Center of Keimyung University School of Medicine and Dongguk University Hospital) for vaccination. The presence of bowel movement at night and feeding methods were examined in 88 healthy infants. The frequency of bowel movement, feeding method, and the amount of stool were examined in 95 healthy infants. All study procedures were approved by the Keimyung University Institutional Review Board.
2. Classification of NFLS and DIDN
Two pediatric gastroenterologists (J.B.H. and A.S.K.) had met the patients. CFLS was defined as over 2-week frequent loose stool. The patients showing dehydration and a failure to gain weight were supposed to belong to DIDN group. However, we revaluated whether the failure to gain weight had been due to causal illnesses and/or to iatrogenic diet management.
We presumed causes of CFLS using clinical characteristics and laboratory blood tests, stool smear and culture, sigmoidoscopy and tissue biopsies, or fecal pH performed in necessary cases, and also using the clinical response to the treatment; normalizing the diet, controlling solid food, administering a lactose-free formula, or antibiotic use. When the maintenance of stable condition with good weight gain was noted on the telephone interviews with the parents, conducted about 2-3 weeks after treatment, we finally diagnosed causal etiologies, and divided given cases into two groups; NFLS group and DIDN group. Fortunately, there was no case that treatment was modified due to a wrong presumption.
3. Clinical definitions and diagnostic criteria
NFLS was defined as the absence of dehydration and a failure to weight gain in an infant with CFLS, and DIDN was defined as CFLS with dehydration and nutritional deficiency due to causal illnesses. But, cases with dehydration and nutritional deficiency caused by iatrogenic diet control without causal illness were included in NFLS.
Although those with allergic proctocolitis with gross blood in stools could be considered to belong to pathologic disease, they should be assigned to the NFLS group so long as judged by the objective definition of diarrhea2), because this disorder is known not to induce dehydration or weight loss8). Cases with chronic nonspecific diarrhea, which normally do not present with dehydration or weight loss9), were also assigned to the NFLS group.
Infectious diarrhea was defined as one of abnormal laboratory findings; a positive bacteria culture from stools or leukocytosis (≥15,000/mm3) in peripheral blood or a C-reactive protein level of ≥5 mg/dL, and an improvement on antibiotics10). Lactose intolerance was defined as a fecal pH lower than 5.0, a resolution of symptoms on a 2-week strict lactose-free diet and the recurrence of symptoms after reintroducing dairy foods, all in the absence of any evidence of infection11). Allergic proctocolitis was diagnosed based on endoscopic abnormalities and histopathological findings12). Chronic nonspecific diarrhea was diagnosed based on mucus in stools and positive response in terms of stool frequency and fluidity to diet control, such as, the restriction of fluid and fruit juice intake and administration of meals with a high fat content13). Pseudomembranous colitis was diagnosed based on sigmidoscopy and histopathological findings14).
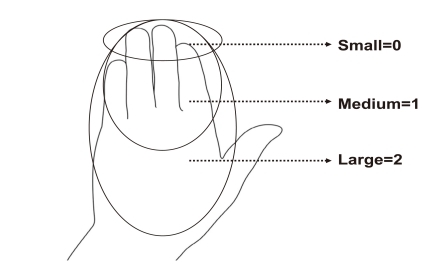
A part of the results of a stool smear test in NFLS patients, which was performed in primary clinics or secondary hospitals, were used for a diagnosis and also the analysis of patients' data. Positive response to therapy was defined as an improvement in general conditions including recovery from dehydration and weight gain. Nocturnal stools were defined as those passed between 10 p.m. and 6 a.m. Because it is inconvenient and even troublesome to measure stool amount by scales, an easier method available had to be investigated, and thus the mother's hand system was adopted. Stool amount was measured by the hand of a Korean woman who has an average height of 160 cm. The size of permeated diaper or of fecal material was estimated by the hand and scored from 0 to 2 points at each evacuation; a few knuckles (small=0), half of the hand (medium=1), and the whole of hand or more (large=2) (Fig. 1). The highest score during the period of CFLS among the sum of these points per day was chosen and each highest score was compared.
Fig. 1.
The stool amount scoring system using the mother's hand.
4. The differentiation of NFLS and DIDN
To identify factors capable of differentiating NFLS and DIDN, we compared changes in body weight after symptom development, stool smear test and culture results, fever, colic/abdominal pain, gross blood and mucus in stools, nocturnal stool, diaper dermatitis, and the score of stool amount per day.
5. Statistical analysis
Categorical data was summarized in terms of frequency and percentage, and continuous variable was arranged in terms of mean and range. Chi-square test was performed in the correlation analysis of two groups in categorical data, and Fisher's exact test was conducted in instances where cell of expected frequency was under 5. Wilcoxon rank sum test was performed to examine the difference between two groups in stool amount score as ordinal scale. Statistical significance was accepted for P values <0.05. We performed all statistical analysis using SPSS (version 12.0, SPSS Inc, Chicago, IL, USA).
Results
1. Clinical features and NFLS to DIDN ratio
The 46 CFLS patients (24 females, 22 males) had a mean (range) age of 8.0 (2-24) months and an average duration of diarrhea of 3.4 (2-12) weeks. There were 36 (78%) cases of NFLS and 10 (22%) of DIDN. The numbers of patients with NFLS and DIDN per month were 13 and 4 cases, respectively, in September, 10 and 3 in October, and 13 and 3 in November. Symptom duration was 3.6 (2-12) weeks in the NFLS group and 3.0 (2-8) weeks in the DIDN group, which was not significantly different.
2. Causes of NFLS and DIDN
Based on final diagnoses, in the NFLS group etiologies were; chronic nonspecific diarrhea in 15 (41%) cases, breastfed stool in 10 (28%), allergic proctocolitis in 5 (14%), weaning food-associated loose and/or frequent stool with undigested food materials in 4 (11%); cow's milk overfeeding-associated loose and/or frequent stool in 1 (3%); and antibiotic-associated stool in 1 (3%). And, in the DIDN group etiologies were; infection in 6 (60%) cases, lactose intolerance in 3 (30%), and pseudomembranous colitis in 1 (10%).
3. Frequency of clinic or hospital visits and admissions
Patients visited primary clinics or hospitals 3.8 (1-12) times in NFLS group and 3.7 (1-10) times in the DIDN group. Four (11%) cases of NFLS and 4 (40%) cases of DIDN were admitted. Of these 4 NFLS cases, 3 cases were admitted once; 2 cases for allergic proctocolitis and the other breastfed. The other case was diagnosed as having chronic nonspecific diarrhea and admitted three times.
4. History of nutritionally deficient diet management
Twenty-five (69%) cases in the NFLS group and 9 (90%) cases in the DIDN group were managed using a nutritionally deficient diet; rice gruel only, diluted cow's milk, reduced breast feeding, and fed over 7 days with a low-caloric formula for acute diarrhea.
5. The differentiation of NFLS and DIDN
1) Failure to gain weight
Fourteen (39%) cases in the NFLS group and all cases in the DIDN group failed to gain weight, and this difference was significant (P<0.001, Table 1).
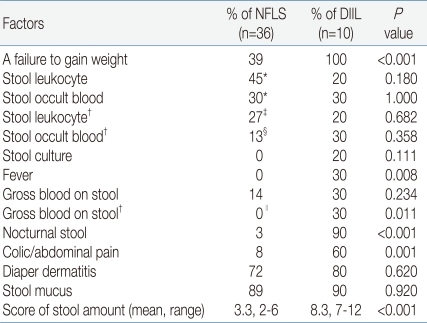
Table 1.
Factors Studied for Differentiation between Normal Frequent Loose Stool (NFLS) and Diarrheal Illness with Dehydration (DIIL) and Nutritional Deficiency (DIDN) among Infants with Chronic Frequent Loose Stool
*in 20 NFLS patients.
†except allergic proctocolitis
‡in 15 NFLS patients.
§in 16 NFLS patients.
∥in 31 NFLS patients.
2) Gross blood in stools
Gross blood in stool was observed in 5 (14%) cases in the NFLS group and in 3 (30%) cases in the DIDN group, which was not significant. However, when the 5 cases with allergic proctocolitis were excluded from the NFLS group, gross blood in stool was significantly different in the two groups (P=0.011, Table 1).
3) Nocturnal stool
One (3%) case in the NFLS group and 9 (90%) cases in the DIDN group were positive, which was significant (P<0.001). Among the 88 normal controls (aged between 10 days and 24 months), 15 (17%) cases were positive for nocturnal stool; of 23 normal controls of less than two months, 12 (52%) were positive (9 cases were associated with breast feeding); in 65 normal infants of more than two months, 3 (5%) were positive (all patients were associated with breast feeding). The positive predictive value and negative predictive value of nocturnal stool for DIDN were 0.90, and 0.97, respectively (Table 1).
4) Stool frequency and the maximal score of stool amount
Stool frequencies per day were 6.8 (3-11) times in the NFLS group and 8.0 (5-14) times in the DIDN group, which were not significantly different. In 95 normal controls (aged between 7 days and 2 years old), 1.9 (1-6) times were observed, and this frequency was significantly different with the frequency of NFLS and DIDN patients, respectively (P<0.001).
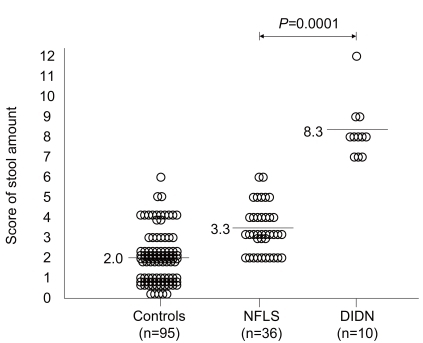
Maximal scores of stool amount were 3.3 (2-6) points in the NFLS group and 8.3 (7-12) points in the DIDN group, significantly different in the two study groups (P<0.001). In 95 normal controls (aged between 7 days and 2 years old), 2.0 (0-6) points were observed, and this score was significantly different with the score of DIDN patients (P<0.001), but not with NFLS patients. Both the normal controls and NFLS group were scored less than 7 points/day, but all cases in the DIDN were scored over 7 points/day (Table 1, Fig. 2).
Fig. 2.
The scores of stool amount for normal controls, patients with normal frequent loose stool (NFLS), and patients with diarrheal illness with dehydration and nutritional deficiency (DIDN).
Discussion
General pediatricians confuse NFLS and DIDN in infants for several reasons. First, they tend to rely upon 'symptomatic' factors, such as, the frequency and fluidity of stools to define diarrhea in children or adults4). However, the positive standard for diarrhea and its clinical application in infants are quite different from those pertinent to children and adults. Second, the increased number of infant with NFLS may make it difficult to distinguish DIDN from NFLS13). In South Korea, the breastfeeding percentage has been rising up rapidly from 10.2% to 35.6% over the last ten years15). Thus weaning diet may have been more actively performed. In accordance with this trend, frequent loose stool caused by breastfeeding or chronic nonspecific diarrhea increased. Third, inadequate information for the 'objective' definition in infantile diarrhea in textbooks tends to confuse general clinicians.
The present study reveals that 78% of infantile patients with CFLS transferred from general pediatricians were NFLS. Patients with a final diagnosis of NFLS made 3.8 (1-12) visits to clinics or hospitals before enrolling in the present study, and 11% of NFLS patients also were admitted to hospital. We attribute this to the inadequate information supplied to physicians regarding the definition of diarrhea in infancy. To avoid this confusion, a detailed explanation of NFLS should be included in textbooks and regular clinical training with sufficient information must be provided. Furthermore, infants with CFLS should be managed using nutritionally balanced diets, and inappropriate diets, such as, the long-term administration of low caloric diets and reduced breastfeeding, should be avoided. According to this study, 69% of NFLS and 90% of DIDN were managed with nutritionally deficient diet.
On January 2009, we informed all pediatricians (at primary clinics or secondary hospitals in Daegu) of the initial results of this study, and instructed them using printed materials and via the pediatricians' website about NFLS including the established differential factors of NFLS and DIDN, chronic nonspecific diarrhea, bowel habitus of breastfed infants, and allergic proctocolitis. Then we analyzed the data of patients transferred between March and May 2009, and compared this with the data of previously transferred patients. After education, the total number of NFLS patients transferred decreased from 36 cases to 4 cases.
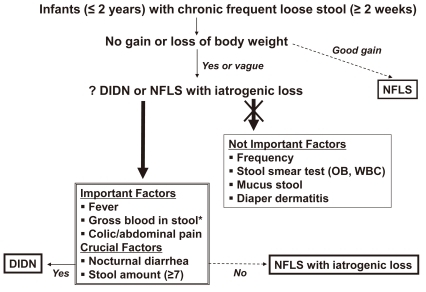
As a consequence of present study, we offer a diagnostic guideline, which might be useful for the clinical differentiation of NFLS and DIDN (Fig. 3). If infants less than two years of age with more than two weeks of CFLS show good weight gain, the case can be assigned to NFLS. On the other hand, cases showing a failure to gain weight can be presumed to be DIDN or NFLS accompanied by an iatrogenic nutritional deficiency. Although weight change after symptom development is an important differential factor, it should be remembered that iatrogenic nutritional deficiency can occur in NFLS. In present study, 39% of NFLS patients showed a failure to gain weight. In these cases, fever, colic/abnormal pain, and bloody stool (except for allergic proctocolitis) are important differential factors of NFLS and DIDN, but the most 'objective' crucial factors are evacuation at night and the score of stool amount.
Fig. 3.
A diagnostic guideline for the clinical differentiation of normal frequent loose stool (NFLS) and diarrheal illness with dehydration and nutritional deficiency (DIDN). *except allergic proctocolitis. OB, occult blood.
In infants more than two months of age, nocturnal stool revealed as an important differential factor. Breastfed infants sometimes may experience nocturnal stool, more commonly in early infancy, but the amounts may be small or the frequencies low. Hence, except for early infancy with breast feeding, nocturnal stool can be used as an important discriminator. Furthermore, the score of stool amount is the most crucial factor in the objective definition of diarrhea in infancy. Because stool amount can be measured using the hand, it can be easily applied and used as a powerful differential factor. Although diarrheal stool amount may be different according to the patient's body weight and score of stool amount be measured differently according to size of the mother's hand, the present study revealed that the score of stool amount is a crucial discriminator of NFLS and DIDN patients. In present study, the cases scored over 7 points per day were all involved in DIDN group. Therefore, 7 points per day is a standard amount to differentiate between NFLS and DIDN.
If an infant with CFLS develops blood-tinged and mucoid stool, infectious diarrhea is frequently presumed and microbiological investigations and antibiotics medication may be planned. However, in this clinical circumstance, two clinical problems should be evaluated: first, is this frequent and loose stool 'objective' diarrhea?; second, what is the cause of blood-tinged stool? If frequent and loose stool of this patient is 'objective' diarrhea by applying a diagnostic guideline for the differentiation of NFLS and DIDN in the present study, blood-tined stool may result from infection. If this case is 'symptomatic' loose stool with the change of usual bowel habitus, blood-tinged stool may be presumed firstly to be an allergic proctocolitis because an infant with allergic proctocolitis develops loose and mucoid stools but does not have growth delay or poor weight gain8). Like this clinical situation, the differentiation of CFLS between 'objective' diarrhea and 'symptomatic' one can prevent the clinical approach from moving in the wrong directions. Therefore, our guideline will be important and helpful for the clinicians to make initial clinical assessment.
The frequency and mucus of stools are not important for discriminating CFLS in infancy according to the objective definition. Microbiological investigations, which are routinely performed, are also ineffective. Furthermore, although it has significance in terms of defining symptomatic diarrhea, diaper dermatitis is unsuitable for defining objective diarrhea. Of course, even though symptomatic diarrhea is not serious, it can cause trouble like frequent diaper replacement and diaper dermatitis in infants. Thus, it is desirable to invite parents to learn about bowel habitus of breast feeding, diet control in chronic nonspecific diarrhea, proper weaning diet control, and probiotic use for antibiotic-associated diarrhea, etc.
It has been reported in adults with functional diarrhea that stool looseness is determined by water content and the water-holding capacity of fecal insoluble solids16). If such detailed physiological factors of determination are more discovered in infants, they would help us more understand infantile bowel habitus.
Acknowledgment
The authors are grateful to Jae O Kim, PhD (School of English Language and Literature, Yeungnam University) for his time and effort in reading this manuscript and editing of English-language.
References
- 1.Weaver LT. Bowel habit from birth to old age. J Pediatr Gastroenterol Nutr. 1988;7:637–640. doi: 10.1097/00005176-198809000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Baldassano RN, Liacouras CA. Chronic diarrhea. A practical approach for the pediatrician. Pediatr Clin North Am. 1991;38:667–686. doi: 10.1016/s0031-3955(16)38124-x. [DOI] [PubMed] [Google Scholar]
- 3.Veereman-Wauters G, Taminiau J. Diarrhea. In: Wyllie R, Hyams JS, editors. Pediatric gastrointestinal and liver disease. 3rd ed. Philadelphia: Saunders Elsevier; 2006. pp. 151–167. [Google Scholar]
- 4.Misra S, Sabui TK, Pal NK. A randomized controlled trial to evaluate the efficacy of lactobacillus GG in infantile diarrhea. J Pediatr. 2009;155:129–132. doi: 10.1016/j.jpeds.2009.01.060. [DOI] [PubMed] [Google Scholar]
- 5.Rhoads JM, Powell DW. Diarrhea. In: Walker WA, Durie PR, Hamilton JR, Walker-Smith JA, Watkins JB, editors. Pediatric gastrointestinal disease. 2nd ed. St. Louis: Mosby Co; 1996. pp. 62–78. [Google Scholar]
- 6.Scaillon M, Cadranel S. Transit tests. In: Hyman PE, DiLorenzo C, editors. Pediatric gastrointestinal motility disorders. 1st ed. New York: Academy Professional Information Services Inc; 1994. pp. 265–276. [Google Scholar]
- 7.Roy C, Silverman A, Alagille D. Symptoms. In: Roy C, Silverman A, Alagille D, editors. Pediatric clinical gastroenterology. 4th ed. St. Louis: Mosby Co; 1995. pp. 3–43. [Google Scholar]
- 8.Maloney J, Nowak-Wegrzyn A. Educational clinical case series for pediatric allergy and immunology: allergic proctocolitis, food protein-induced enterocolitis syndrome and allergic eosinophilic gastroenteritis with protein-losing gastroenteropathy as manifestations of non-IgE-mediated cow's milk allergy. Pediatr Allergy Immunol. 2007;18:360–367. doi: 10.1111/j.1399-3038.2007.00561.x. [DOI] [PubMed] [Google Scholar]
- 9.Rasquin-Weber A, Hyman PE, Cucchiara S, Fleisher DR, Hyams JS, Milla PJ, et al. Childhood functional gastrointestinal disorders. Gut. 1999;45(Suppl 2):II60–II68. doi: 10.1136/gut.45.2008.ii60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu LJ, Yang YJ, Kuo PH, Wang SM, Liu CC. Diagnostic value of bacterial stool cultures and viral antigen tests based on clinical manifestations of acute gastroenteritis in pediatric patients. Eur J Clin Microbiol Infect Dis. 2005;24:559–561. doi: 10.1007/s10096-005-1373-z. [DOI] [PubMed] [Google Scholar]
- 11.Heyman MB. Lactose intolerance in infants, children, and adolescents. Pediatrics. 2006;118:1279–1286. doi: 10.1542/peds.2006-1721. [DOI] [PubMed] [Google Scholar]
- 12.Hwang JB, Park MH, Kang YN, Kim SP, Suh SI, Kam S. Advanced criteria for clinicopathological diagnosis of food protein-induced proctocolitis. J Korean Med Sci. 2007;22:213–217. doi: 10.3346/jkms.2007.22.2.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kleinman RE. Chronic nonspecific diarrhea of childhood. Nestle Nutr Workshop Ser Pediatr Program. 2005;56:73–79. doi: 10.1159/000086276. discussion 79-84. [DOI] [PubMed] [Google Scholar]
- 14.Brook I. Pseudomembranous colitis in children. J Gastroenterol Hepatol. 2005;20:182–186. doi: 10.1111/j.1440-1746.2004.03466.x. [DOI] [PubMed] [Google Scholar]
- 15.Kim JY, Hwang SJ, Park HK, Lee HB, Kim NS. Analysis of online breast-feeding consultation on the website of the Korean Pediatric Society. Korean J Pediatr. 2008;51:1152–1157. [Google Scholar]
- 16.Wenzl HH, Fine KD, Schiller LR, Fordtran JS. Determinants of decreased fecal consistency in patients with diarrhea. Gastroenterology. 1995;108:1729–1738. doi: 10.1016/0016-5085(95)90134-5. [DOI] [PubMed] [Google Scholar]