Abstract
Background
Biologic factors are known to contribute to asthma severity. It is unknown whether these factors differentially contribute to asthma severity in Blacks compared to Whites.
Objective
We sought to assess the extent to which racial disparities in severe asthma between Blacks and Whites are attributable to physiologic, immunoinflammatory, and sociodemographic variables.
Methods
Black and White asthmatic adults enrolled in a cross-sectional study focused on severe asthma were evaluated. Severe asthma was identified using the American Thoracic Society definition. Following initial univariable analyses, unconditional logistic regression models were used to estimate the probability of having severe asthma for Blacks and Whites.
Results
Differences in severe asthma in Blacks compared to Whites were observed. In univariable analysis, IgE was not associated with severe asthma in Blacks or Whites, while in multivariable analysis IgE was significantly associated with severe asthma for Blacks (p=0.014) but not in Whites. The odds of having severe asthma more than doubled for Blacks with 2 or more family members with asthma (p=0.026), while the odds of severe asthma for White participants with a strong family history of asthma decreased by almost half (p=0.05). Atopy was negatively associated with severe asthma in both races in univariable analysis, but remained significant only in Blacks, while co-morbidities were associated with severe asthma in Whites.
Conclusion
Biologic factors were distinctly associated with severe asthma only in Blacks. Studies which incorporate comprehensive evaluation of biologic factors associated with asthma may lead to the development of therapies which target biologic abnormalities in Blacks.
Keywords: severe asthma, race, IgE, allergic sensitization, immunoinflammatory
INTRODUCTION
Although standard treatments can control most asthma, a small number of asthmatics (about 10%) require treatment with the highest level of inhaled corticosteroids (ICS), often in combination with other drugs, including systemic corticosteroids(1–2). Despite these high medication doses, these patients often never achieve adequate disease control and continue to have frequent and/or severe exacerbations, daily symptoms and bronchodilator use, as well as persistent airway obstruction (3). Although lower lung function, a history of pneumonia, less atopy, and lower blood basophils have all been shown to be independently associated with the presence of this more severe asthma, much remains to be determined regarding the factors which either associate or predict its development (4).
Asthma in Blacks has long been associated with higher morbidity and mortality rates than Whites(5). Blacks have four times the risk of hospitalization and five times the risk of mortality than Whites(6). Although Blacks have been reported to be more likely to have severe asthma, particularly in relation to asthma exacerbations(7), concerns have generally focused on contribution from limited access to appropriate medical care, adherence to medications and related socioeconomic factors to this severe form of disease(8).
However, in addition to SES, biologic factors likely also contribute to asthma severity in both racial groups. Whether there are differences in the contribution of biologic factors to asthma severity in Blacks compared to Whites has not been specifically addressed. For instance, immunoglobulin E (IgE) levels are well known to be significantly higher in Blacks than Whites in both asthmatic and non asthmatic populations(9–16). In addition to total IgE, specific IgE also differs by race with higher levels of grass and cockroach specific IgE associated with asthma and more poorly controlled asthma in Blacks(15, 17). Higher total IgE levels have been shown to be associated with lower lung function with the relationship stronger in some racial and ethnic group than others (18). Finally, substantial differences in Th2 related gene allele frequencies have been described in Blacks compared to Whites suggesting that hereditary/genetic differences could explain some of the potential severity differences(19).
The objective of this paper was to determine the extent to which the racial health disparities in asthma, particularly severe asthma, are attributable to physiologic, immunoinflammatory and/or sociodemographic variables. We hypothesized that the contribution of immunoinflammatory predictors to asthma severity would differ by race. To address this hypothesis, clinical, immunologic, and physiologic data from the cross sectional National Heart Lung and Blood Institutes’ sponsored Severe Asthma Research Program (SARP) database were analyzed to determine whether there were differences in the factors associated with severe asthma in Black compared to White asthmatic participants.
METHODS
Subjects
The data in this study was obtained from subjects enrolled in the Severe Asthma Research Program, a network established to identify and characterize severe asthmatic subjects in relation to milder asthmatics to better understand mechanisms for their disease. The baseline characteristics of this population were recently published(4). SARP initially consisted of eight funded sites- the University of Pittsburgh, the University of Virginia (subsites at Cleveland and Emory University), Brigham and Women’s Hospital, Imperial College, National Jewish Medical and Research Center, Wake Forest University, Washington University, and the University of Wisconsin. The number of sites was reduced to 4 in 2006: University of Pittsburgh (including National Jewish), Cleveland Clinics (including the University of Virginia and Emory University), the University of Wisconsin, and Wake Forest University.
From August 2003 until February 2010, 1391 subjects aged 18–79 years were recruited and enrolled. Current smokers or individuals with five or more pack-years of tobacco use were excluded from SARP(4). The American Thoracic Society’s (ATS) definition was used to determine whether individuals had severe/refractory asthma(20). Severe asthma subjects were required to meet one of 2 major criteria (high dose inhaled or oral corticosteroid [CS] use) and at least 2 of 7 minor criteria. All subjects who did not meet criteria for severe asthma were classified as “not severe”. There were no specific requirements for the subjects other than a confirmed diagnosis of asthma based on symptoms, bronchodilator response or airway hyperresponsiveness.
Data Collection/Measures at Interview
All subjects completed multiple (14) allergen skin testing evaluations for atopy, standardized and SARP specific questionnaires, collection of blood for complete blood counts and differentials and total IgE, exhaled nitric oxide and pulmonary function testing as previously described(4). Questionnaires were administered by clinical staff and included information on demographics, medical history, comorbidities, family history, smoking history, and frequency of asthma symptoms such as wheezing, nocturnal symptoms and shortness of breath. Medical resource or health care utilization was assessed by the subject’s recollection of emergency room visits, hospital and ICU visits, asthma ventilation procedures. Baseline pre-bronchodilator spirometry testing was carried out for each subject. In addition, a maximal bronchodilator response was calculated as the greatest percent change from the prebronchodilator FEV1 following 4–8 puffs of albuterol. A variety of other procedures were done on subpopulations of SARP subjects (methacoline, sputum induction, and bronchoscopy), but are not included in this study due to incomplete data primarily based on site specific testing (sputum) or exclusions on the basis of FEV1% predicted (sputum, methacholine) or subject preference (bronchoscopy).
Statistical Analysis
Statistical analyses were conducted using SAS software (SAS Institute Inc. 2008. SAS Statistical Software: Version 9.2. Cary, North Carolina) and STATA software (StataCorp. 2009. Stata Statistical Software: Release 11. College Station, TX). Categorical variables were examined using cross-tabulations and frequencies, [expressed as n (%)]. Chi-square (χ2) or Fisher’s exact test were performed for racial comparisons [White (or Caucasian) and Black (or African racial heritage)] of categorical variables in the severe asthma group. The Wilcoxon-Mann-Whitney test was performed for racial comparisons of continuous variables in the severe asthma group [expressed as median (25th–75th percentiles)].
Univariable Models
Unconditional logistic regression was used to calculate the crude and adjusted odds ratios to estimate the probability of having severe asthma. Race specific (Black and White) models were used for this study. Univariable models were used to determine which variables to include for model selection and exclude during the model building process, with only the variables with a p-value of less than 0.15 included.
Multivariate Models
Variables that had a p-value of less than 0.15 in the univariable models were included for model selection. In addition, variables deemed of clinical significance regardless of statistical significance were included in the full model. The likelihood ratio (LR) test p-value was used to determine if variables should remain in the model. Goodness of fit of the model was assessed using Pregibon’s Dbeta and Hosmer and Lemeshow’s delta-d. Models were adjusted for age of enrollment and clinical center.
RESULTS
Baseline Demographics (Table I)
Table I.
Baseline Characteristics of SARP Participants by Racial Background & Phenotype Group
| Both Races N=916 |
Black n=267 (29.1%) |
White n=649 (70.9%) |
||||
|---|---|---|---|---|---|---|
| Mild/Mod n=538 |
Severe n=378 |
Mild/Mod n=159 |
Severe n=108 |
Mild/Mod n=379 |
Severe n=270 |
|
| *Age at Diagnosis (yrs) | 10(4,21) | 12(3,28) | 9(4,22) | 10(2,27.5) | 10(4,21) | 13(3,30) |
| *Age of Enrollment (yrs) | 33.3(24.5,42.8) | 45.2(36.1,60.0) | 32.7(25.5,40.6) | 42.0(35.3,49.1) | 33.4(24,44.7) | 46.6(36.2,54.3) |
| Duration of Asthma (yrs) | 19.5(10.8,28.8) | 25.9(15.6,37.9) | 20.3(11.1,26.7) | 25.6(14.3,37.5) | 19.1(10.7,30.1) | 25.9(16.1,38.3) |
| *BMI, kg/m2 | 27.2(23.5,33.0) | 30.6(25.4,35.6) | 29.4(25.8,37.5) | 33.1(29.3,28.9) | 26.0(22.9,31.4) | 29.4(25.0,34.5) |
| *Baseline Predrug FEV1, liters | 2.76(2.31,3.37) | 1.91(1.35,2.41) | 2.41(1.93,2.85) | 1.74(1.36,2.19) | 2.99(2.49,3.55) | 1.96(1.33,2.60) |
| *Baseline Predrug FEV1% pred | 84.5(74,96) | 60.5(45,77) | 81(70,92) | 63.5(50.5,81) | 86(76,98) | 58.5(44,74) |
| *Baseline Predrug FVC% pred | 94(84,103) | 76.4(64,88) | 93(81,102) | 80.4(69,96.5) | 94(85,104) | 74.7(62.8,86) |
| *FEV1/FVC | 0.75(0.68,0.82) | 0.65(0.55,0.74) | 0.74(0.67,0.80) | 0.68(0.57,0.76) | 0.76(0.69,0.82) | 0.64(0.53,0.73) |
| Max FEV1 Reversal % | 10(5.5,18.4) | 14.5(6.6,25.9) | 14(6.1,23.8) | 15(6.9,25.9) | 9.4(5.2,15.9) | 14.2(6.0,26.3) |
| *Log IgE (IU/ml) | 2.10(1.69,2.51) | 2.08(1.59,2.54) | 2.24(1.83,2.68) | 2.29(1.83,2.68) | 2.06(1.60,2.42) | 2.01(1.49,2.46) |
| Presence of Atopy | 417(77.5%) | 234(61.9%) | 130(81.8%) | 67(62%) | 287(75.7%) | 167(61.9%) |
| ≥ 5 Positive Skin Tests | 186(34.6%) | 84(22.2%) | 72(45.3%) | 31(28.7%) | 114(30.1%) | 53(19.6%) |
| *Female | 362(67.3%) | 242(64%) | 109(68.6%) | 78(72.2%) | 253(66.8%) | 164(60.7%) |
| *Currently Employed | 345(64.1%) | 235(62.2%) | 104(65.4%) | 61(56.5%) | 241(63.6%) | 174(64.4%) |
| Diagnosed Diabetes | 19(3.5%) | 38(10.1%) | 9(5.7%) | 11(10.2%) | 10(2.6%) | 27(10%) |
| Diagnosed hypertension | 63(11.7%) | 92(24.3%) | 30(18.9%) | 28(25.9%) | 33(8.7%) | 64(23.7%) |
| Diagnosed GERD | 99(18.4%) | 150(39.7%) | 29(18.2%) | 41(38.0%) | 70(18.5%) | 109(40.4%) |
Continuous variables: median (25th, 75th percentiles); Categorical variables: n (%)
FEV1: forced expiratory volume in one second
FVC: forced vital capacity ratio
GERD: gastroesophageal reflux disease
2ndhand smoke exp: secondhand smoke exposure
p < 0.15 Black severe vs White severe.
General demographics
Of the 1391 total enrolled in SARP, 916 participants met inclusion criteria for this analysis. This analysis included only adult participants (18 years of age and older). Participants with a racial background classified as nonblack and nonwhite, as well as participants considered normal (not asthmatic) were excluded (n=475). There were more White (71%) than Black participants (29%). More female participants were included compared to males, and there were slightly more mild/moderate asthmatics compared to severe asthmatics. Forty percent of Blacks and 42% of Whites were categorized as severe asthmatics. The median age at enrollment for Blacks was almost 5 years younger than the age for Whites in the severe asthma group (p=0.011) with 65% of Blacks enrolling into SARP at 45 years of age or younger (Figure 1). While the age that the participants were first diagnosed with asthma was not significantly different between Blacks and White severe asthmatics; 10% more of the Black compared to the White population were diagnosed younger than three years of age (Appendix 1). Body mass index (BMI) in Blacks was also higher than in Whites.
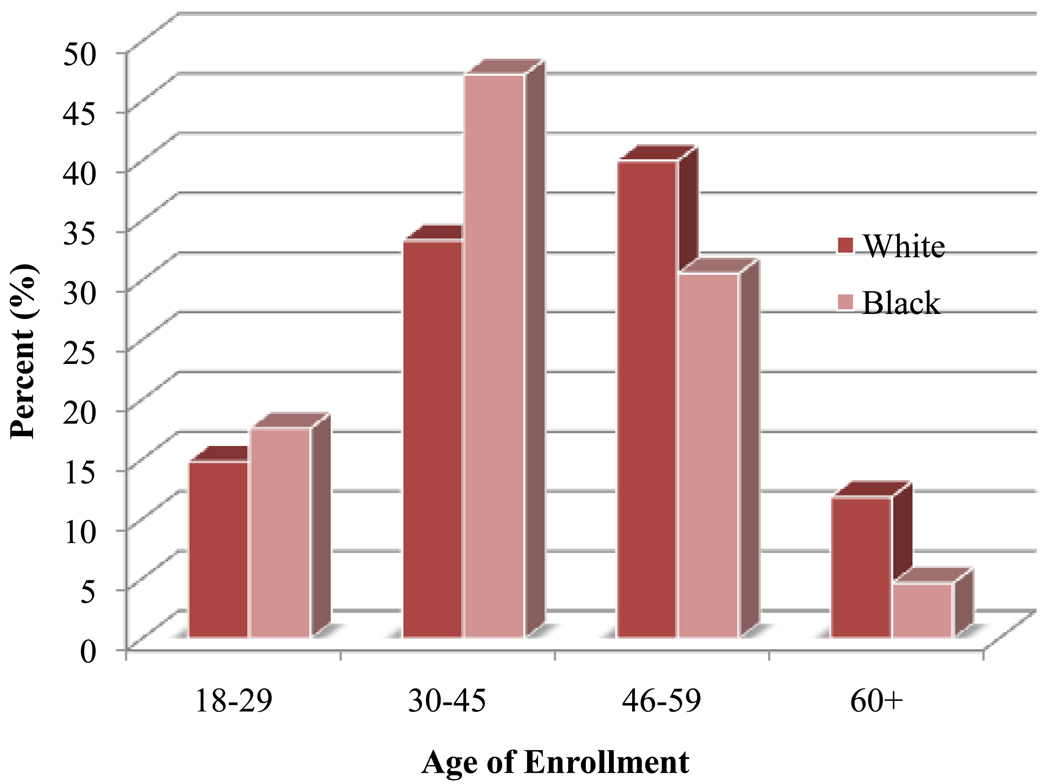
Figure 1.
Percent of Black & White Participants enrolled into the Severe Asthma Research Program by age at enrollment. Black participants enrolled into the Severe Asthma Research Program at an earlier age compared to White participants (p= 0.011).
Socioeconomic related factors
White severe asthmatics were more likely to be employed compared to their Black counterparts. Almost 32% of Black severe asthmatics were exposed to secondhand smoke compared to 23% of White severe asthmatics (p=0.049). Pet ownership within the severe asthma group was significantly less in Blacks than Whites, with 22% of Blacks and 47% of Whites owning pets.
Pulmonary function
When pulmonary function was corrected for race, height, and age Black asthmatics had higher median baseline predrug FEV1 and FVC % predicted values compared to Whites; however, absolute FEV1 (in liters) was lower for Blacks compared to Whites. Bronchodilator reversibility was not significantly different for Blacks and Whites.
Immunoinflammatory markers
The mean IgE level for severe asthmatics was 174±5 IU/ml in Blacks and 85±5 IU/ml in Whites (p=0.003). While there was no difference in overall prevalence of atopy in the population, Blacks were more likely to have a high number of (≥5) positive skin tests compared to Whites. Blood eosinophils did not differ by race.
Participants Younger than Age 40 (Table II)
Table II.
Baseline Characteristics of SARP Participants who enrolled Below the Age of 40 Years by Racial Background & Phenotype Group
| Both Races N=518 |
Black n=162 (31.3%) |
White n=356 (68.7%) |
||||
|---|---|---|---|---|---|---|
| Mild/Mod n=372 |
Severe n=146 |
Mild/Mod n=114 |
Severe n=48 |
Mild/Mod n=258 |
Severe n=98 |
|
| Age at Diagnosis (yrs) | 8(4, 16) | 5(1,14) | 8(4,18) | 4(1,15.5) | 8(4,15) | 5(1,13) |
| Duration of Asthma (yrs) | 17.3(10.6,23.3) | 22.6(14.4,29.2) | 18.4(10.9,23.7) | 22.5(14,27.6) | 17.1(10.6,22.9) | 22.6(15.9,29.2) |
| *BMI (kg/m2) | 25.9(22.7,32.4) | 30.1(25,36.5) | 28.4(24.6,36.8) | 33.9(30.1,45) | 24.9(22.2,29) | 27.5(23.8,24.5) |
| *Baseline Predrug FEV1 (liters) | 2.99(2.56,3.58) | 2.15(1.54,2.75) | 2.57(2.20,2.94) | 1.91(1.53,2.23) | 3.26(2.74,3.73) | 2.28(1.65,3.00) |
| Baseline Predrug FEV1 % Pred | 89(78,99) | 63(48,81) | 83.5(75,94) | 63(52.5,80) | 91(80,101) | 62.5(48,81) |
| Baseline Predrug FVC % Pred | 97.3(89,105) | 81.8(71,95) | 96(86,104) | 82.7(73,90) | 98(89.2,106) | 81.4(68.3,95) |
| FEV1/FVC | 0.77(0.71,0.83) | 0.68(0.55,0.78) | 0.75(0.68,0.82) | 0.68(0.55,0.79) | 0.78(0.72,0.83) | 0.64(0.55,0.78) |
| Max FEV1 Reversal (%) | 9.2(4.9,17.7) | 15.3(6.7,28.9) | 14.1(6,24.6) | 14.6(6.8,26.8) | 8.1(4.3,14.1) | 16.2(6.5,29.5) |
| Log IgE (IU/ml) | 2.18(1.79,2.55) | 2.18(1.78,2.59) | 2.25(1.84,2.71) | 2.31(1.74,2.68) | 2.12(1.74,2.49) | 2.11(1.79,2.52) |
| Atopy | 295(79.3%) | 98(67.1%) | 97(85.1%) | 33(68.8%) | 198(76.7%) | 65(66.3%) |
| ≥5 Positive Skin Tests | 142(38.2%) | 44(30.1%) | 56(49.1%) | 19(39.6%) | 86(33.3%) | 25(25.5%) |
| Female | 255(68.5%) | 94(64.4%) | 79(69.3%) | 34(70.8%) | 176(68.2%) | 60(61.2%) |
| Currently Employed | 220(59.1%) | 91(62.3%) | 74(64.9%) | 28(58.3%) | 146(56.6%) | 63(64.3%) |
| Diagnosed Diabetes | 7(1.9%) | 7(4.8%) | 6(5.3%) | 2(4.2%) | 1(0.4%) | 5(5.1%) |
| Diagnosed Hypertension | 26(7.0%) | 20(13.7%) | 17(14.9%) | 9(18.8%) | 9(3.5%) | 11(11.2%) |
| Diagnosed GERD | 50(13.4%) | 52(35.6%) | 17(14.9%) | 21(43.8%) | 33(14%) | 31(31.6%) |
Mean age: 28.99 ± 6.62
Continuous variables: median (25th, 75th percentiles); Categorical variables: n (%)
FEV1: forced expiratory volume in one second
FVC: forced vital capacity ratio
GERD: gastroesophageal reflux disease.
2ndhand smoke exp: secondhand smoke exposure
p < 0.15 Black severe vs White severe.
As Black subjects had a lower median age at enrollment, a secondary comparison was done between White and Black asthmatics enrolled in SARP above and below age 40. Even in those under 40, the mean age at enrollment for Blacks remained slightly (but not significantly) younger compared to Whites, 29.6 ± 6.3 and 28.7 ± 6.7, respectively. Similar to the total group, gender did not differ. In contrast to the total dataset, there was no significant difference in employment. Even in the lower age group, BMI remained significantly and substantially higher in Blacks (Median=33.9; 25th–75th percentiles=30.1–45.0) than Whites (Median=27.5; 25th–75th percentiles=23.8–24.5). Comorbidities such as diabetes, hypertension, and GERD were not significantly different between races and most participants were atopic. The median IgE level in Black asthmatics was higher compared to Whites but the levels did not differ in the severe asthma subgroup. Using percent predicted values, FEV1 did not differ across the races, however, the absolute FEV1 (in liters) was significantly and markedly lower in Blacks (Median=1.91 liters; 25th–75th percentiles=1.53–2.23) compared to Whites (Median=2.28 liters; 25th–75th percentiles=1.65–3.00), despite Blacks being younger in this subset. There was no difference in bronchodilator reversibility.
Participants Age 40 and Above (Table III)
Table III.
Baseline Characteristics of SARP Participants who enrolled at Age of 40 Years and above by Racial Background & Phenotype Group
| Both Races N=398 |
Black n=105 (26.4%) |
White n=293 (73.4%) |
||||
|---|---|---|---|---|---|---|
| Mild/Mod n=166 |
Severe n=232 |
Mild/Mod n=45 |
Severe n=60 |
Mild/Mod n=121 |
Severe n=172 |
|
| *Age at Diagnosis (yrs) | 18(5,36) | 20(5.5,35) | 18(5,35) | 13(3.5,33.5) | 18(6,38) | 21(6.5,35) |
| Duration of Asthma (yrs) | 31.6(11.2,42.3) | 29.9(15.8,45.3) | 25.9(11.2,39.6) | 31.9(15.3,43.5) | 32(11.2,42.7) | 29.4(16.5,46.4) |
| *BMI (kg/m2) | 29.1(25.8,34.9) | 30.8(26,35.2) | 32.9(28.3,38.2) | 32.9(26.9,36.9) | 28.4(24.6,32.9) | 30(25.8,34.3) |
| Baseline Predrug FEV1 (liters) | 2.31(1.81,2.73) | 1.74(1.26,2.26) | 1.84(1.69,2.31) | 1.71(1.30,2.18) | 2.45(2.00,2.89) | 1.77(1.24,2.34) |
| *Baseline Predrug FEV1% Pred | 78(66,87) | 57(44,75) | 73(57,86) | 64.5(48.5,85.5) | 79(66,88) | 56(42,71) |
| *Baseline Predrug FVC% Pred | 85(76,94) | 73.6(60,84) | 83(72.3,91) | 79(66.8,97) | 86(77,94) | 72(58,82) |
| *FEV1/FVC | 0.73(0.65,0.78) | 0.65(0.54,0.72) | 0.73(0.64,0.76) | 0.67(0.3,0.72) | 0.72(0.66,0.78) | 0.63(0.53,0.72) |
| Max FEV1 Reversal (%) | 11.5(7.1,20.2) | 13.8(6.3,24.5) | 13.1(6.8,20.7) | 15.4(7.5,25.7) | 11(7.1,19.4) | 13.7(6,24) |
| *Log IgE (IU/ml) | 1.94(1.46,2.36) | 2.00(1.44,2.49) | 2.14(1.73,2.64) | 2.29(1.83(2.72) | 1.90(1.43,2.31) | 1.93(1.34,2.36) |
| Atopy | 122(73.5%) | 136(58.6%) | 33(73.3%) | 34(56.7%) | 89(73.6%) | 102(59.3%) |
| ≥5 Positive Skin Tests | 44(26.5%) | 40(17.2%) | 16(35.6%) | 12(20%) | 28(23.1%) | 28(16.3%) |
| *Female | 107(64.5%) | 148(63.8%) | 30(66.7%) | 44(73.3%) | 77(63.6%) | 104(60.5%) |
| Currently Employed | 125(75.3%) | 144(62.1%) | 30(66.7%) | 33(55%) | 95(78.5%) | 111(64.5%) |
| Diagnosed Diabetes | 12(7.2%) | 31(13.4%) | 3(6.7%) | 9(15%) | 9(15%) | 22(12.8%) |
| Diagnosed Hypertension | 37(22.3%) | 72(31%) | 13(28.9%) | 19(31.7%) | 19(31.7%) | 53(30.8%) |
| *Diagnosed GERD | 49(29.5%) | 98(42.4%) | 12(26.7%) | 20(33.3%) | 37(30.6%) | 78(45.3%) |
Mean age: 51.3 ± 7.86
Continuous variables: median (25th, 75th percentiles); Categorical variables: n (%)
FEV1: forced expiratory volume in one second
FVC: forced vital capacity ratio
GERD: gastroesophageal reflux disease.
2ndhand smoke exp: secondhand smoke exposure
p < 0.15 Black severe vs White severe.
Among older asthmatics, Black severe asthmatics were both significantly younger and younger at diagnosis than White severe asthmatics. Greater than 10% more Black severe asthmatics were female than Whites, p=0.07. Current employment again did not differ among the races. White asthmatics were more likely to report a diagnosis of GERD compared to Blacks (45% and 33%, respectively) despite the higher BMI in the older Black severe asthmatics. There were no differences in atopic/allergic markers across the two races.
Similar to the younger age group, baseline pre drug FEV1, FVC % predicted and the FEV1 /FVC were significantly higher in Blacks compared to Whites. The absolute FEV1 (in liters) did not differ between Blacks and Whites in this age group, but was likely confounded by the higher percentage of females and lower overall age in the Black participants. Bronchodilator reversibility did not differ between the races.
Univariable Models
Black Participants (Table IV)
Table IV.
Univariable Logistic Regression Models for Black Participants in SARP (n=267)
| Variable | Coeff | SE | OR | 95% CI | G | p |
|---|---|---|---|---|---|---|
| Age Onset | 0.006 | 0.0090 | 1.01 | 0.99–1.02 | 0.45 | 0.503 |
| Age | 0.057 | 0.0119 | 1.06 | 1.03–1.08 | 22.63 | <.0001 |
| Female | 0.176 | 0.2745 | 1.19 | 0.70–2.04 | 0.41 | 0.521 |
| Center | −0.112 | 0.0462 | 0.89 | 0.82–0.98 | 5.83 | 0.016 |
| BMI | 0.033 | 0.0142 | 1.03 | 1.01–1.06 | 5.36 | 0.021 |
| Employed | −0.376 | 0.2559 | 0.69 | 0.42–1.13 | 2.16 | 0.141 |
| 2nd Smoke | −0.205 | 0.2660 | 0.82 | 0.48–1.37 | 0.59 | 0.442 |
| Pets | 0.042 | 0.3008 | 1.04 | 0.58–1.88 | 0.02 | 0.889 |
| GERD | 0.977 | 0.2865 | 2.66 | 1.52–4.66 | 11.63 | 0.001 |
| Diabetes | 0.647 | 0.4681 | 1.91 | 0.76–4.78 | 1.91 | 0.167 |
| HTN | 0.409 | 0.2988 | 1.51 | 0.84–2.70 | 1.87 | 0.171 |
| FEV1% pred | −0.031 | 0.0066 | 0.97 | 0.96–0.98 | 22.07 | <.0001 |
| FEV1 liters | −1.397 | 0.2312 | 0.25 | 0.16–0.39 | 36.54 | <.0001 |
| % Eosinophil | 0.007 | 0.0351 | 1.01 | 0.94–1.08 | 0.04 | 0.849 |
| Reversal | 0.0067 | 0.0061 | 1.01 | 0.995–1.02 | 1.18 | 0.277 |
| IgE | 0.075 | 0.2077 | 1.08 | 0.72–1.62 | 0.13 | 0.717 |
| ≥5 skin tests | −0.486 | 0.2843 | 0.62 | 0.35–1.07 | 2.92 | 0.088 |
| Atopy | −1.009 | 0.2855 | 0.37 | 0.21–0.64 | 12.50 | 0.0004 |
| 1 Fam Hx | −0.065 | 0.3090 | 0.94 | 0.51–1.72 | 0.04 | 0.834 |
| 2+ Fam Hx | 0.511 | 0.3166 | 1.67 | 0.90–3.10 | 2.61 | 0.106 |
Age Onset=Age when first diagnosed with asthma, Age=Age when enrolled into SARP, Center= clinical center site, 2ndhand smoke=exposure to secondhand smoke during day, Pets=own any pets, GERD=gastroesophogeal reflux disease, HTN=hypertension diagnosis, FEV1=forced expiratory volume in one second, % Eosinophil=% of eosinophils in the blood, Reversal=Max FEV1 reversal, IgE=Immunoglobulin E, ≥5 skin tests= 5 or more positive skin tests, 1 Family Hx= Have 1 family member with asthma, 2+ Family Hx= Have 2 or more family members with asthma
IgE entered as continuous log-transformed variables in the model
In the univariable models for Blacks, current age and pulmonary function (baseline predrug FEV1 in liters, baseline predrug FEV1 %predicted) were highly associated with asthma severity. BMI, GERD, and current employment were also associated with severe asthma, but no other co-morbidity was associated, including exposure to second hand smoke. Interestingly, the presence (atopy yes/no) and degree of atopy (% of participants with five or more positive allergen skin tests) were negatively associated with severe asthma, while 2 or more family members with asthma was positively associated. In the univariable analysis, IgE was not associated with severe asthma in Blacks.
White Participants (Table V)
Table V.
Univariable Logistic Regression Models for White Participants in SARP (n=649)
| Variable | Coeff | SE | OR | 95% CI | G | p |
|---|---|---|---|---|---|---|
| Age Onset | 0.015 | 0.0054 | 1.02 | 1.00–1.03 | 7.61 | 0.006 |
| Age | 0.057 | 0.0067 | 1.06 | 1.05–1.07 | 72.70 | <.0001 |
| Female | −0.261 | 0.1656 | 0.77 | 0.56–1.07 | 2.48 | 0.115 |
| Center | −0.138 | 0.0289 | 0.87 | 0.82–0.92 | 22.68 | <.0001 |
| BMI | 0.044 | 0.0115 | 1.05 | 1.02–1.07 | 14.64 | 0.0001 |
| Employed | 0.037 | 0.1660 | 1.04 | 0.75–1.44 | 0.05 | 0.823 |
| 2nd Smoke | 0.106 | 0.1930 | 1.11 | 0.76–1.62 | 0.30 | 0.584 |
| Pets | −0.309 | 0.1621 | 0.73 | 0.53–1.01 | 3.63 | 0.057 |
| GERD | 1.116 | 0.1827 | 3.05 | 2.13–4.37 | 37.30 | <.0001 |
| Diabetes | 1.420 | 0.3793 | 4.14 | 1.97–8.70 | 14.02 | 0.0002 |
| HTN | 1.198 | 0.2319 | 3.31 | 2.10–5.22 | 26.67 | <.0001 |
| FEV1% pred | −0.066 | 0.0055 | 0.94 | 0.93–0.95 | 145.77 | <.0001 |
| FEV1 liters | −1.399 | 0.1264 | 0.25 | 0.19–0.32 | 122.56 | <.0001 |
| % Eosinophil | −0.010 | 0.0304 | 0.99 | 0.93–1.05 | 0.10 | 0.748 |
| Reversal | 0.029 | 0.0055 | 1.03 | 1.02–1.04 | 27.14 | <.0001 |
| IgE | −0.124 | 0.1399 | 0.88 | 0.67–1.16 | 0.79 | 0.374 |
| ≥5 skin tests | −0.488 | 0.1962 | 0.61 | 0.42–0.90 | 6.17 | 0.013 |
| Atopy | −0.654 | 0.1734 | 0.52 | 0.37–0.73 | 14.25 | 0.0002 |
| 1 Fam Hx | −0.246 | 0.1874 | 0.78 | 0.54–1.13 | 1.72 | 0.190 |
| 2+ Fam Hx | −0.096 | 0.2103 | 0.91 | 0.60–1.37 | 0.21 | 0.648 |
Age Onset=Age when first diagnosed with asthma, Age=Age when enrolled into SARP, Center= clinical center site, 2ndhand smoke=exposure to secondhand smoke during day, Pets=own any pets, GERD=gastroesophogeal reflux disease, HTN=hypertension diagnosis, FEV1=forced expiratory volume in one second, % Eosinophil=% of eosinophils in the blood, Reversal=Max FEV1 reversal, IgE=Immunoglobulin E, ≥5 skin tests= 5 or more positive skin tests, 1 Family Hx= Have 1 family member with asthma, 2+ Family Hx= Have 2 or more family members with asthma
IgE entered as continuous log-transformed variables in the model
The results from the White univariable models differed substantially from the Black univariable models. While current age, BMI, GERD and pulmonary function (baseline pre drug FEV1 in liters and percent predicted) were statistically significant in these models, in Whites, other co-morbidities, such as diabetes and hypertension, were highly associated with asthma severity. However, similar to Blacks, second hand smoke exposure was not associated. In contrast to Blacks, older age when first diagnosed with asthma and increasing degree of bronchodilator responsiveness were also highly associated with asthma severity. Similar to Blacks, the presence and degree of atopy were also negatively predictive of severe asthma. Unlike Blacks, owning a pet was marginally associated with decreased odds for severe asthma in Whites. Family history of asthma was not associated with asthma severity in Whites.
Multivariate Models
Black Participants (Table VI)
Table VI.
Final Model with for Black Participants in SARP (n=267)
| Variable | OR | 95%CI | p>|z| |
|---|---|---|---|
| Age | 1.06 | 1.02–1.09 | 0.002 |
| Center | 0.93 | 0.81–1.07 | 0.318 |
| Employed | 0.72 | 0.35–1.48 | 0.366 |
| 1 Family history | 1.50 | 0.62–3.60 | 0.367 |
| 2+ Family history | 2.79 | 1.13–6.87 | 0.026 |
| GERD | 3.59 | 1.62–7.97 | 0.002 |
| Baseline FEV1% pred | 0.96 | 0.94–0.98 | <.0001 |
| Max FEV1 Reversal | 0.98 | 0.96–1.00 | 0.058 |
| IgE | 2.12 | 1.16–3.87 | 0.014 |
| ≥5 positive skin tests | 0.46 | 0.21–1.01 | 0.053 |
Age=Age when enrolled into SARP, Age Onset=Age when first diagnosed with asthma, Center= clinical center site, 1 Family History= Have 1 family member with asthma, 2+ Family History= Have 2 or more family members with asthma, GERD=gastroesophogeal reflux disease, FEV1=forced expiratory volume in one second, IgE=Immunoglobulin E
IgE entered as continuous log-transformed variable in the model
Adjusted for current age (age of SARP enrollment) & clinical center
For every 10% decrease in baseline FEV1 % predicted the odds of having severe asthma increased 40% (p<0.0001). Although bronchodilator responsiveness was of borderline significance (p=0.058), the odds for severe asthma decreased by 2% with an increase of one percent in reversibility after bronchodilator suggesting that those Black asthmatics with more fixed airflow limitation were at highest risk of severe asthma.
In contrast to the univariable analysis, IgE was strongly associated with severe asthma in Blacks (p=0.014). For every log10 increase in IgE the risk of severe asthma more than doubled. The odds of having severe asthma also more than doubled for Blacks who had 2 or more family members diagnosed with asthma (p=0.026). Despite the association with total IgE and family history, having five or more positive skin tests to allergens was negatively associated with severe asthma (p=0.05).
Blacks with GERD have more than three times the odds of having severe asthma compared to Blacks without GERD (p=0.002). While employment was marginally associated with severe asthma in the univariable models, it was not significant in the multivariate analyses (p=0.366). After adjusting for confounders, baseline predrug FEV1 % predicted, GERD, total IgE, and having two or more family members with asthma remained significantly associated with asthma severity. Given the relatively smaller sample size of Black participants, lower bronchodilator responsiveness and having less than five positive skin tests may also be considered significant in this model.
White Participants (Table VII)
Table VII.
Final Model with for White Participants in SARP (n=649)
| Variable | OR | 95%CI | p>|z| |
|---|---|---|---|
| Age | 1.02 | 1.00–1.04 | 0.046 |
| Center | 0.88 | 0.81–0.95 | 0.001 |
| BMI | 1.00 | 0.98–1.03 | 0.790 |
| Age Onset | 1.00 | 0.99–1.02 | 0.866 |
| 1 Family History | 0.67 | 0.42–1.09 | 0.108 |
| 2+ Family History | 0.57 | 0.32–1.00 | 0.051 |
| Pets | 0.65 | 0.42–1.00 | 0.051 |
| GERD | 1.92 | 1.18–3.13 | 0.009 |
| Diabetes | 2.27 | 0.82–6.29 | 0.114 |
| Baseline FEV1% pred | 0.94 | 0.93–0.95 | <.0001 |
Age=Age when enrolled into SARP, Center= clinical center site, Age Onset=Age when first diagnosed with asthma, 1 Family History= Have 1 family member with asthma, 2+ Family History= Have 2 or more family members with asthma, Pets=own any pets, GERD=gastroesophogeal reflux disease, FEV1=forced expiratory volume in one second
Adjusted for current age (age of SARP enrollment) & clinical center
Similar to Blacks, baseline FEV1% predicted was highly associated with severe asthma, with every 10% percent decrease in baseline FEV1 increasing the odds of having severe asthma by 60% (p<.0001). Additionally, GERD remained highly associated with severe asthma (doubling the odds of severe asthma) (p=0.009), while in contrast to Blacks, diabetes remained marginally associated with asthma severity (p=0.114). Current pet ownership decreased the odds of severe asthma by 35% (p=0.05). In contrast to Black severe asthmatics, the odds of severe asthma for White participants who had 2 or more family members diagnosed with asthma decreased by almost half (p=0.05) and IgE (and measures of atopy) did not enter the final model. The final model for Whites after adjusting for age and site included baseline FEV1 percent predicted, GERD, lack of current pet ownership and having no or a weak family history of asthma as positive predictors of asthma severity.
DISCUSSION
In this cross sectional analysis of over 900 Black and White asthmatic subjects, striking differences were found in the factors associated with severe asthma. While baseline FEV1 % predicted and GERD were important factors for both racial groups, biologic factors including IgE, skin test reactivity and family history were distinctly associated with severe asthma in Blacks. Although socioeconomic factors almost certainly impact the high health care utilization and associated morbidity of asthma in Blacks, the results from this analysis suggest biologic/genetic factors related to atopy/allergy are, also, of substantial, if not even greater importance. These results underline the importance of understanding differences in pathobiologic mechanisms driving asthma and its severity in different racial groups.
Asthma has often been described as an atopic disease, with atopy defined as the development of specific IgE in response to environmental allergens. However, the association of allergies with asthma severity has been more difficult to confirm. Indeed, in the initial SARP demographic study, the presence of atopy was a strong negative predictor for severe asthma(4). Therefore, the finding that increasing IgE levels were strongly predictive of severe asthma in Blacks (and not at all in Whites) was surprising. While IgE was not a significant predictor of severity in the univariable model for Blacks (p=0.717); it became a strong predictor of severity in the multivariate model, suggesting that when numerous confounding factors were controlled for IgE remained as a predictive variable (p=0.016). Black asthmatics were again confirmed to have a much higher total IgE compared to White asthmatics, irrespective of severity. These results extend the findings of Naqvi et al who demonstrated that higher IgE levels were associated with more severe asthma in Black, Mexican, and Puerto Rican patients(18). However, unlike the study by Naqvi, SARP used a rigidly predefined and validated definition of severity which supports the relevance of this biologic difference to disease severity (4). Naqvi utilizes frequency of symptoms and FEV1 % predicted scores to categorize a participant as moderate-to-severe; whereas, SARP requires that a participant be continuously using an oral or high dose inhaled corticosteroid.
While IgE was a significant positive predictor of asthma severity in Blacks, having five or more positive skin tests was a significant negative predictor of severe asthma. It is still unclear why two measures of atopy have apparently opposing effects on asthma severity within the Black SARP population. Serum IgE, which is a sum of all the circulating systemic IgE, would appear to be measuring something additional to the presence or absence of the 14 specific IgEs measured by skin testing in SARP. Interestingly, a subsequent post hoc univariate model also did not find a positive skin test for cockroaches to be associated with severe asthma in Blacks (p=0.60). While further pathobiologic studies of this relationship are needed, the data suggest that it may not be the number of positive skin tests, rather the amount of specific IgE made to each or any allergen or the presence of a specific, yet unidentified IgE. In future studies, the total wheal size to each allergen can also be included in the analyses. Additionally, robust measures of allergen exposure were not included in these studies which could also contribute to these differences.
A well known risk factor for asthma is having a first degree relative with asthma(21). Atopy and allergy are also known to be contributed to by hereditary/genetic factors. Therefore, while it might be expected that family history would be predictive for asthma, studies on the hereditary relationship to severity in specific racial groups (as opposed to presence) have been limited. Perhaps more surprisingly, a reasonably strong family history of asthma in White participants was negatively associated with severe asthma. Given the generally later age at onset in the White participants (especially in those >40 yrs old), these results suggest that severe asthma in Whites specifically includes a different, non-atopic/allergic, late onset disease subset/phenotype with less genetic elements, as has been previously identified(22). This specific subtype/phenotype of severe asthma is not being identified in Blacks either because it is less likely to occur or it is not being identified possibly for socioeconomic related reasons. In any case, studies of Black asthmatic populations may be more likely to produce genetic links to severity as compared to studies of White populations.
Numerous studies have pointed to the critical role that socioeconomic factors and health disparities play in asthma in the Black community. In the current study, factors related to SES, including current employment and pet ownership, were not related to severe asthma in Blacks. However, this lack of relationship to SES may be related to the limited data collected in SARP related to SES. As SARP expands, the questionnaires have added educational, marital status and zip code which should improve the ability to assess the role of SES in the severity of asthma. Interestingly, while employment status was not associated with severity in either Blacks or Whites, as has been noted previously, pet ownership was associated with protection from severe asthma in Whites(23). Black participants in SARP, in general, had significantly lower pet ownership than Whites in SARP. It is unclear whether increasing pet ownership would improve asthma outcomes in Blacks (as seen in Whites), even without substantial changes in SES, but requires further study.
Univariable models revealed that comorbidities were highly associated (p<0.0001) with asthma severity in Whites. This association was much less in Blacks except for GERD, which, as previously shown in SARP, continued to be a positive predictor of severity for both Blacks and Whites. In contrast, hypertension and diabetes were highly significant predictors for Whites but not for Blacks, despite their higher prevalence in Blacks compared to Whites in the general population. It can be hypothesized that asthma itself may be affecting Blacks much more than Whites such that the severity of the asthma could be masking the effects of other diseases. Blacks may be focusing on the most severe ailments, while other diseases may not yet be diagnosed. Blacks may have been diagnosed younger with asthma due to a better pediatric medical safety net, or because Black babies with asthma are substantially sicker than White babies with asthma. As they age, Blacks may not be going to the doctor regularly to get full checkups which would allow diagnosis of comorbidities, such as diabetes. In support of this, Black severe asthmatics reported lower percentages of diagnosed diabetes and hypertension compared to Whites; while Blacks with mild/moderate asthma reported diabetes and hypertension twice as often as their White counterparts. Exposure to tobacco smoke has also been shown to increase the prevalence and severity of asthma. In a cohort of adult nonsmoking asthmatics, adults exposed to secondhand smoke at baseline had higher asthma severity scores compared to those without tobacco smoke exposure(24). However, in SARP, secondhand smoke was not a significant predictor of asthma severity for either race and was, therefore, not included within the final predictor model for both races.
Lower baseline predrug FEV1 is well recognized as a predictor of severe asthma(3, 20, 25). In this study, the odds of severe asthma increased by 40% and 60% for Blacks and Whites, respectively, for every 10% decline in FEV1 % predicted. While we used FEV1 % predicted in the models, there are also striking differences in the absolute FEV1 (in liters) in Blacks compared to Whites, which are “corrected” by the Hankinson equations used in SARP lung function testing. When racially corrected (and age/sex corrected) the mean/median FEV1 % predicted is higher in Blacks compared to Whites. However, the absolute FEV1 is significantly lower compared to Whites, despite the younger age of the Black asthmatics. Hankinson equations for FEV1 % were built on disproportionate samples sizes in Blacks compared to Whites. White participants are equally distributed throughout the age groups; whereas, after the age of 50 years the number of Black participants drastically decreases compared to the number of younger Black participants(25). As a Black participant ages and goes beyond the age of 50 years, the accuracy of the Hankinson equations may not be as valid as they are for the younger Black participants. Further, recent genetic studies suggest that being identified as “Black” in America is accompanied by a wide range of genetic racial admixture ranging from 100% African ancestry to 10% or less, such that predictive equations for “Blacks” may not apply to all “Black” participants(26). In any case, measuring lung function by FEV1 % predicted could easily overestimate the lung capacity of many Black patients and lead to under recognition of the severity of the disease.
In Blacks, in addition to FEV1 % predicted, maximum bronchodilator responsiveness was marginally associated with asthma severity in Blacks. However, for every % increase in bronchodilator responsiveness the odds for severe asthma decreased by 2%. The reasons for this inverse relationship are not clear but suggest that as asthma worsens in Blacks, the airways may stiffen/remodel such that the most commonly used treatment for asthma (beta agonists) becomes less effective. Whether these findings suggest a mechanism for the recent findings regarding increased severe asthma exacerbations and deaths in Blacks taking long acting beta agonists remains to be determined(27).
This study is not without limitations, certainly the biggest of which is the cross-sectional study design. It is difficult to confirm a temporal relationship in regards to severity and the variables of interest. Another limitation is the sample size differences for each race. The White SARP population consisted of over 70% of the data in this analysis, whereas, less than 30% of the data is from the Black SARP population. Having populations of similar sizes would aid in confirming the results from this study and possibly reveal stronger associations between predictors and severe asthma. Although the SARP database is one of the most extensive databases of asthmatics from numerous geographic sites and includes the collection of lung inflammatory markers, such as sputum eosinophils, sputum induction was only performed on about 50% of the population. Therefore, sputum measures could not be used. However, genome wide association data and longitudinal participant information are being added to the database enabling even more complete studies on asthma severity in the future.
In conclusion, distinctly different factors appear to be associated with rigidly defined severity of asthma in Blacks compared to Whites, with allergic markers and strong family history much stronger positive predictors of severity for Blacks than for Whites. Thus in addition to socioeconomic factors, studies which incorporate comprehensive evaluation of biologic and genetic factors of relevance to asthma in Blacks in particular, may lead to the development of targeted therapies which improve overall asthma outcomes in the Black population.
Key Messages.
Severe asthma in Blacks is strongly associated with traditional markers of allergic and genetic patterns of disease. These same patterns are not seen in Whites.
Acknowledgments
Grant support: HL69116, HL69130, HL69155, HL69167, HL69170, HL69174, HL69349, HL091762, M01 RR02635, M01 RR03186, M01 RR007122-14, 1UL1RR024153, 1UL1RR024989, 1UL1RR024992, 1UL1RR025011.
Declaration of sources of funding: Clinical and Translational Research Center funding: UL1 RR024153 [National Center for Research Resources (NCRR)]
The Severe Asthma Research Program (SARP) is a multicenter asthma research group funded by the NHLBI and consisting of the following contributors (Principal Investigators are marked with an asterisk): Brigham & Women's Hospital - Elliot Israel*, Bruce D. Levy, Michael E. Wechsler, Shamsah Kazani, Gautham Marigowda; Cleveland Clinic - Serpil C. Erzurum*, Raed A. Dweik, Suzy A.A. Comhair, Emmea Cleggett-Mattox, Deepa George, Marcelle Baaklini, Daniel Laskowski; Emory University - Anne M. Fitzpatrick, Denise Whitlock, Shanae Wakefield; Imperial College School of Medicine - Kian Fan Chung*, Mark Hew, Patricia Macedo, Sally Meah, Florence Chow; University of Iowa – Eric Hoffman*, Janice Cook-Granroth; University of Pittsburgh - Sally E. Wenzel*, Fernando Holguin, Silvana Balzar, Jen Chamberlin; University of Texas-Medical Branch - William J. Calhoun*, Bill T. Ameredes; University of Virginia - Benjamin Gaston*, W. Gerald Teague*, Denise Thompson-Batt; University of Wisconsin - William W. Busse*, Nizar Jarjour, Ronald Sorkness, Sean Fain, Gina Crisafi; Wake Forest University - Eugene R. Bleecker*, Deborah Meyers, Wendy Moore, Stephen Peters, Rodolfo M. Pascual, Annette Hastie, Gregory Hawkins, Jeffrey Krings, Regina Smith; Washington University in St Louis - Mario Castro*, Leonard Bacharier, Jaime Tarsi; Data Coordinating Center - Douglas Curran-Everett*, Ruthie Knowles, Maura Robinson, Lori Silveira; NHLBI - Patricia Noel, Robert Smith
Abbreviations
- OR
odds ratio
- SARP
Severe Asthma Research Program
- CS
corticosteroids
- ICS
inhaled corticosteroids
- IgE
Immunoglobulin E
- FEV1
forced expiratory volume in 1 second
- FVC
forced vital capacity
- SES
socioeconomic status
- BMI
body mass index
- LR
likelihood ratio
- ATS
American Thoracic Society
- GERD
gastroesophogeal reflux disease
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Polosa R. An overview of chronic severe asthma. Internal Medicine Journal. 2008;38(3):190–198. doi: 10.1111/j.1445-5994.2007.01547.x. [DOI] [PubMed] [Google Scholar]
- 2.Alves Rde S, Vianna Fde A, Pereira CA. Clinical phenotypes of severe asthma. J Bras Pneumol. 2008;34(9):646–653. doi: 10.1590/s1806-37132008000900003. [DOI] [PubMed] [Google Scholar]
- 3.Ng TP. Validity of symptom and clinical measures of asthma severity for primary outpatient assessment of adult asthma. British Journal of General Practice. 2000;50:7–12. [PMC free article] [PubMed] [Google Scholar]
- 4.Moore WC, Bleecker ER, Curran-Everett D, Erzurum SC, Ameredes BT, Bacharier L, et al. Characterization of the severe asthma phenotype by the National Heart, Lung, and Blood Institute's Severe Asthma Research Program. Journal of Allergy and Clinical Immunology. 2007;119(2):405–413. doi: 10.1016/j.jaci.2006.11.639. [doi: DOI: 10.1016/j.jaci.2006.11.639] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shanawani H. Health disparities and differences in asthma: concepts and controversies. Clinics in Chest Medicine. 2006;27:17–28. doi: 10.1016/j.ccm.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 6.Gupta RS, CarriÃ3n-Carire V, Weiss KB. The widening black/white gap in asthma hospitalizations and mortality. J Allergy Clin Immunol. 2006;117:351–358. doi: 10.1016/j.jaci.2005.11.047. [DOI] [PubMed] [Google Scholar]
- 7.El-Ekiaby A, Brianas L, Skowronski ME, Coreno AJ, Galan G, Kaeberlein FJ, et al. Impact of race on the severity of acute episodes of asthma and adrenergic responsiveness. Am J Respir Crit Care Med. 2006;174:508–513. doi: 10.1164/rccm.200603-431OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haselkorn T, Lee JH, Mink DR, Weiss ST, Group TS. Racial disparities in asthma-related health outcomes in severe or difficult-to-treat asthma. Ann Allergy Asthma Immunol. 2008;101:256–263. doi: 10.1016/S1081-1206(10)60490-5. [DOI] [PubMed] [Google Scholar]
- 9.Joseph CLM, Ownby DR, Peterson EL, Johnson CC. Racial Differences in Physiologic Parameters Related to Asthma Among Middle-class Children*. Chest. 2000 May;117(5):1336–1344. doi: 10.1378/chest.117.5.1336. 2000. [DOI] [PubMed] [Google Scholar]
- 10.Yang JJ, Burchard EG, Choudhry S, Johnson CC, Ownby DR, Favro D, et al. Differences in allergic sensitization by self-reported race and genetic ancestry. Journal of Allergy and Clinical Immunology. 2008;122(4):820–827. e9. doi: 10.1016/j.jaci.2008.07.044. [doi: DOI: 10.1016/j.jaci.2008.07.044] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haselkorn T, Lee JH, Mink DR, Weiss ST. Racial disparities in asthma-related health outcomes in severe or difficult-to-treat asthma. Annals of Allergy, Asthma and Immunology. 2008;101:256–263. doi: 10.1016/S1081-1206(10)60490-5. [DOI] [PubMed] [Google Scholar]
- 12.Borish LMD, Chipps BMD, Deniz YMD, Gujrathi SMD, Zheng BP, Dolan CMP, et al. Total serum IgE levels in a large cohort of patients with severe or difficult-to-treat asthma. doi: 10.1016/S1081-1206(10)61221-5. [Article] [DOI] [PubMed] [Google Scholar]
- 13.Grundbacher FJ, Massie FS. Levels of immunoglobulin G, M, A, and E at various ages in allergic and nonallergic black and white individuals. Journal of Allergy and Clinical Immunology. 1985;75(6):651–658. doi: 10.1016/0091-6749(85)90089-2. [doi: DOI: 10.1016/0091-6749(85)90089-2] [DOI] [PubMed] [Google Scholar]
- 14.Litonjua AA, Celedón JC, Hausmann J, Nikolov M, Sredl D, Ryan L, et al. Variation in total and specific IgE: Effects of ethnicity and socioeconomic status. Journal of Allergy and Clinical Immunology. 2005;115(4):751–757. doi: 10.1016/j.jaci.2004.12.1138. [doi: DOI: 10.1016/j.jaci.2004.12.1138] [DOI] [PubMed] [Google Scholar]
- 15.Lester LA, Rich SS, Blumenthal MN, Togias A, Murphy S, Malveaux F, et al. Ethnic differences in asthma and associated phenotypes: Collaborative Study on the Genetics of Asthma. Journal of Allergy and Clinical Immunology. 2001;108(3):357–362. doi: 10.1067/mai.2001.117796. [doi: DOI: 10.1067/mai.2001.117796] [DOI] [PubMed] [Google Scholar]
- 16.Sherman CB, Tollerud DJ, Heffner LJ, Speizer FE, Weiss ST. Airway responsiveness in young black and white women. Am Rev Respir Dis. 1993 Jul;148(1):98–102. doi: 10.1164/ajrccm/148.1.98. [DOI] [PubMed] [Google Scholar]
- 17.Celedón JC, Sredl D, Weiss ST, Pisarski M, Wakefield D, Cloutier M. Ethnicity and Skin Test Reactivity to Aeroallergens Among Asthmatic Children in Connecticut*. Chest. 2004 January;125(1):85–92. doi: 10.1378/chest.125.1.85. 2004. [DOI] [PubMed] [Google Scholar]
- 18.Naqvi M, Choudhry S, Tsai H-J, Thyne S, Navarro D, Nazario S, et al. Association between IgE levels and asthma severity among African American, Mexican, and Puerto Rican patients with asthma. Journal of Allergy and Clinical Immunology. 2007;120(1):137–143. doi: 10.1016/j.jaci.2007.02.045. [doi: DOI: 10.1016/j.jaci.2007.02.045] [DOI] [PubMed] [Google Scholar]
- 19.Wenzel SE, Balzar S, Ampleford E, Hawkins GA, Busse WW, Calhoun WJ, et al. IL4R{alpha} Mutations Are Associated with Asthma Exacerbations and Mast Cell/IgE Expression. Am J Respir Crit Care Med. 2007 March 15;175(6):570–576. doi: 10.1164/rccm.200607-909OC. 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wenzel SE, Busse WW. Severe asthma: Lessons from the Severe Asthma Research Program. Journal of Allergy and Clinical Immunology. 2007;119(1):14–21. doi: 10.1016/j.jaci.2006.10.025. [doi: DOI: 10.1016/j.jaci.2006.10.025] [DOI] [PubMed] [Google Scholar]
- 21.Lugogo NL, Kraft M. Epidemiology of asthma. Clin Chest Med. 2006 Mar;27(1):1–15. doi: 10.1016/j.ccm.2005.10.006. v. [DOI] [PubMed] [Google Scholar]
- 22.Miranda C, Busacker A, Balzar S, Trudeau J, Wenzel SE. Distinguishing severe asthma phenotypes: Role of age at onset and eosinophilic inflammation. Journal of Allergy and Clinical Immunology. 2004;113(1):101–108. doi: 10.1016/j.jaci.2003.10.041. [doi: DOI: 10.1016/j.jaci.2003.10.041] [DOI] [PubMed] [Google Scholar]
- 23.Bufford JD, Reardon CL, Li Z, Roberg KA, DaSilva D, Eggleston PA, et al. Effects of dog ownership in early childhood on immune development and atopic diseases. Clinical & Experimental Allergy. 2008;38(10):1635–1643. doi: 10.1111/j.1365-2222.2008.03018.x. [DOI] [PubMed] [Google Scholar]
- 24.Eisner MD, Yelin EH, Henke J, Shiboski SC, Blanc PD. Environmental tobacco smoke and adult asthma. The impact of changing exposure status on health outcomes. Am J Respir Crit Care Med. 1998 Jul;158(1):170–175. doi: 10.1164/ajrccm.158.1.9801028. [DOI] [PubMed] [Google Scholar]
- 25.Hankinson John L, Odencrantz John R, Fedan Kathleen B. Spirometric Reference Values from a Sample of the General U.S. Population. Am J Respir Crit Care Med. 1999 January 1;159(1):179–187. doi: 10.1164/ajrccm.159.1.9712108. 1999. [DOI] [PubMed] [Google Scholar]
- 26.Kumar R, Seibold MA, Aldrich MC, Williams LK, Reiner AP, Colangelo L, et al. Genetic Ancestry in Lung-Function Predictions. N Engl J Med. 2010 July 7; doi: 10.1056/NEJMoa0907897. 2010:NEJMoa0907897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kramer JM. Balancing the Benefits and Risks of Inhaled Long-Acting Beta-Agonists -- The Influence of Values. N Engl J Med. 2009 April 16;360(16):1592–1595. doi: 10.1056/NEJMp0810561. 2009. [DOI] [PubMed] [Google Scholar]