Abstract
Background
It is unclear whether lack of follow-up after screening FOBT in older adults is due to screening patients whose comorbidity or preferences do not permit follow-up versus failure to complete follow-up in healthy patients.
Methods
Prospective cohort study of 2,410 patients ≥ 70 years screened with FOBT at 4 VA’s between 1/1/01-12/31/01. Main outcome was receipt of follow-up within 1 year of FOBT based on national VA and Medicare data. For patients with positive FOBT results, age and Charlson comorbidity scores were evaluated as potential predictors of receiving complete colon evaluation (colonoscopy or sigmoidoscopy plus barium enema) and medical records were reviewed to determine reasons for lack of follow-up.
Results
212 (9%) patients had positive FOBT results; 42% received complete colon evaluation within 1 year. Age and comorbidity were not associated with receipt of complete follow-up, which was similar among patients 70–74 years with Charlson=0 compared with patients ≥ 80 years with Charlson≥1 (48% vs 41%; P=0.28). VA site, number of positive FOBT cards, and number of VA outpatient visits were predictors. Of 122 patients who did not receive follow-up within 1 year, 38% had documentation that comorbidity or preferences did not permit follow-up, and over the next 5 years 76% never received follow-up.
Conclusions
While follow-up after positive FOBT results was low regardless of age or comorbidity, screening patients in whom complete evaluation would not be pursued substantially contributes to lack of follow-up. Efforts to improve follow-up should address the full chain of decision-making, including decisions to screen and decisions to follow-up.
INTRODUCTION
Fecal occult blood test (FOBT) is a low-risk test that has been shown to reduce mortality from colorectal cancer,1–2 but it can only be effective when patients with an abnormal result receive follow-up with a complete evaluation of the colon (colonoscopy or barium enema plus sigmoidoscopy), which has significant risks.3 Therefore, guidelines recommend targeting FOBT screening to patients whose comorbidity and preferences would permit complete evaluation of the colon to be pursued if the result was abnormal.4–6 However, prior studies have found that FOBT screening is often performed in patients with significant comorbidity who would be at increased risk for serious adverse events (e.g., colon perforation, major bleeding, or stroke) from follow-up colonoscopy.7,8 In addition, it is well known that many patients with positive screening FOBT results do not receive a complete evaluation of the colon.9–12 However, it remains unclear to what extent low rates of follow-up are due to screening older patients whose poor health or preferences would not permit complete evaluation of the colon (and therefore they should not have been screened) versus failure to complete intended follow-up of healthy older patients.
Developing a better understanding of factors contributing to low follow-up of abnormal screening FOBT results in older adults is critical for improving the effectiveness of this widely used test; FOBT is the most common colorectal cancer screening test used in the Veteran’s Affairs (VA) healthcare system.13 For example, if poor follow-up occurs predominantly in patients in poor health, who should not have been screened in the first place, then initiatives mandating follow-up colonoscopy within 60 days of a positive result may cause harm if patients with serious comorbidity are automatically sent for colonoscopy.14 While the hope is clinician judgment would prevail to appropriately target follow-up, previous studies of the impact of age, comorbidity, and other factors on the receipt of follow-up after an abnormal FOBT result have been limited by small sample sizes, single site data, data from intervention studies or clinician surveys that may not reflect real world practices, and failure to describe the spectrum of abnormal screening results (e.g., number of positive cards, incomplete tests).9–13, 15–19 In addition, none of the previous VA studies have measured follow-up outside the VA, 10, 13, 19, 20 which is critical because many veterans receive care outside the VA.21
Therefore, to address these issues we took a novel approach of combining VA and Medicare claims and chart review to provide objective, real world data characterizing the spectrum of screening FOBT results and type of follow-up received within 1 year among patients 70 years or older screened at 4 geographically diverse VA facilities. For patients with a positive FOBT result, we determined the impact of age, comorbidity, and other factors on receipt of complete colon evaluation within 1 year, and using VA medical records we report documented reasons for lack of follow-up as well as the number of patients who ultimately received complete colon evaluation during the subsequent 5 years.
METHODS
Data Sources and Patients
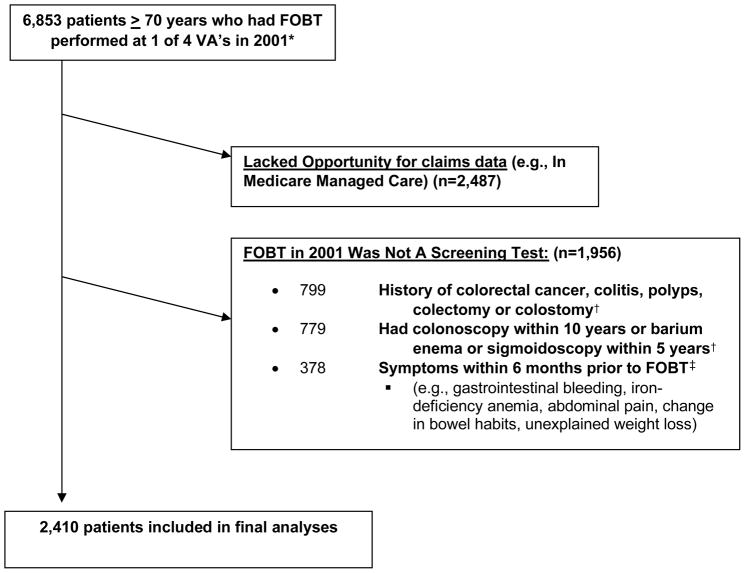
Outpatient claims from the VA National Patient Care Database were used to identify a cohort of 6,853 patients 70 years of age or older whose first colorectal cancer screening test between 1/1/01 and 12/31/01 was FOBT at 1 of 4 VA facilities (Minneapolis, Durham, Portland, and West Los Angeles). FOBT was identified by Current Procedural Terminology (CPT) codes 82270, 82273, and 82274, Level II Healthcare Common Procedure Coding System (HCPCS) code G0107, and laboratory data.7 We used national VA and Medicare data to follow the cohort for 1 year after their FOBT for the performance of follow-up testing, including colonoscopy, sigmoidoscopy, barium enema, or repeat FOBT. To ensure complete comorbidity and follow-up data, we required all patients to have continuous enrollment in Medicare Parts A and B and fee-for-service coverage during 1/1/00-12/31/02 (Figure 1). In addition, patients had to be eligible for screening to be included in our cohort. Therefore, we used VA and Medicare inpatient and outpatient claims (dating back to 10/1/92 for VA claims and 1/1/99 for Medicare claims) to exclude 799 (12%) patients with a history of colorectal cancer, colitis, colorectal polyps, colectomy, or colostomy and 779 (11%) patients who had any history of a colonoscopy or had had a sigmoidoscopy or barium enema within 5 years and were therefore not due for screening. We also used claims from 6 months before their FOBT as well as chart review to exclude 378 (6%) patients who had signs or symptoms that would justify performance of FOBT for non-screening purposes (Figure 1). This left a final cohort of 2,410 patients who had a screening FOBT in 2001 at 1 of 4 VA facilities.
Figure 1.
Study Flow Diagram
*Only patients who had Fecal Occult Blood Testing (FOBT) as their first colorectal cancer screening test in 2001 were included (i.e., Patients whose first test in 2001 was colonoscopy, sigmoidoscopy, or barium enema were excluded).
† Defined by searching VA and Medicare inpatient and outpatient claims, dating as far back as October 1, 1992 for VA claims and January 1, 1999 for Medicare claims. While some FOBT performed after a recent colonoscopy or barium enema and flexible sigmoidoscopy may be for screening purposes, these patients generally do not require repeat complete colon evaluation regardless of the FOBT result, so they were excluded in order to focus on the impact of age, comorbidity, and preferences on follow-up after an abnormal screening FOBT result. 18
‡ Symptoms were defined by VA and Medicare inpatient and outpatient claims as well as review of VA electronic medical records.
Data Collection and Measurement
Outcome Variables
Individual FOBT results were extracted from the chemistry section of the Veterans Health Information Systems and Technology Architecture (VISTA) laboratory package at the 4 VA facilities. If any FOBT cards were positive for occult blood, then the FOBT was “positive.” If all three cards were negative for occult blood, then the FOBT was “negative.” If fewer than three cards were submitted and were negative, then the FOBT was “incomplete.” Less than 1% of patients had administrative codes for FOBT but no result in the electronic medical record. These FOBT results were classified as “missing” and follow-up was not assessed. Three VA facilities (de-identified as Sites A, C, and D) used Hemoccult FOBT without rehydration, while Site B used Hemoccult SENSA, a more sensitive test.
We assessed the receipt of follow-up during the 1 year after screening FOBT across the VA health care system and Medicare, because many elderly veterans use more than 1 VA medical center and most are enrolled in Medicare.21 We identified follow-up testing in National VA Data Systems and linked Medicare payment data (inpatient and outpatient files) by using International Classification of Disease, Ninth Revision (ICD-9), CPT, and HCPCS codes for colonoscopy (ICD-9: 45.22, 45.23, 45.25, 45.41, 45.42, 45.43; CPT: 44388–44394, 45355, 45378–45385; HCPCS: G0105, G0121), sigmoidoscopy (ICD-9: 45.24, 48.22–48.24, 48.26, 48.35, 48.36; CPT: 45300, 45303, 45305, 45308, 45309, 45315, 45320, 45330–45334,45337–45339; HCPCS: G0104), barium enema (ICD-9: 87.64; CPT: 74270, 74280; HCPCS:G0106, G0120, G0122), and repeat FOBT. 7, 22 For patients with a positive FOBT result we assessed whether complete colon evaluation (defined as colonoscopy or barium enema plus sigmoidoscopy) was performed within 1 year.
In addition, 3 authors (LW, MC, CC) reviewed VA electronic medical records independently for documented reasons why complete colon evaluation was not performed and together grouped the reasons into categories. Any discrepancy in categorization was adjudicated by consensus among the reviewers. Medical record review was also used to determine if patients who did not receive complete colon evaluation within 1 year went on to have a complete colon evaluation documented during the subsequent 5 years.
Predictor Variables
Age was determined on the date of the screening FOBT. Comorbidity was measured using the Deyo adaptation of the Charlson Comorbidity Index, a summary measure of 19 chronic disease diagnoses from administrative data.23 The risk of death from an increase of 1 in Charlson Comorbidity score is approximately equal to that from an additional decade of age.24 Charlson-Deyo scores were calculated from VA and Medicare inpatient and outpatient claims during the 12 months before the date of the FOBT.
We also assessed other factors known to influence receipt of follow-up after positive FOBT results (see Table 1) using VA and Medicare data and linkage to the 2000 U.S. Census.25 The Committee on Human Research at the University of California, San Francisco; the Committee for Research and Development at the San Francisco VA Medical Center; and the Institutional Review Board at the Minneapolis VA Medical Center approved the study.
Table 1.
Patient Characteristics, According to Screening Fecal Occult Blood Test (FOBT) Result (N=2410)*
| Characteristic | Screening FOBT Result† | ||
|---|---|---|---|
| Positive (n=212) | Negative (n=2091) | Incomplete (n=83) | |
| N (%) | N (%) | N (%) | |
| Age, years | |||
| 70–74 | 75 (35) | 751 (36) | 26 (31) |
| 75–79 | 93 (44) | 860 (41) | 30 (36) |
| ≥ 80 | 44 (21) | 480 (23) | 27 (33) |
| Male Gender | 211 (100) | 2035 (97) | 81 (98) |
| Race/Ethnicity | |||
| White | 180 (85) | 1858 (89) | 60 (72) |
| Black | 30 (14) | 190 (9) | 20 (24) |
| Other | 2 (1) | 41 (2) | 3 (4) |
| Charlson Score** | |||
| 0 (no comorbidity) | 66 (31) | 811 (39) | 27 (32) |
| 1–3 (average comorbidity) | 119 (56) | 1081 (52) | 47 (57) |
| ≥ 4 (severe comorbidity) | 27 (13) | 199 (9) | 9 (11) |
| Number of VA Outpatient Visits‡ | |||
| 0–3 | 114 (54) | 1339 (64) | 47 (57) |
| 4+ | 98 (46) | 752 (36) | 36 (43) |
| Home-bound§ | 6 (3) | 27 (1) | 8 (10) |
| Married | 145 (69) | 1471 (72) | 49 (62) |
| Lived in ZCTA in which ≥ 25% of Adults Had a College Education|| | 56 (27) | 706 (35) | 36 (44) |
| Median Income of ZCTA|| | |||
| Highest tertile (≥$29,119) | 51 (25) | 706 (34) | 37 (45) |
| Middle tertile | 75 (36) | 666 (33) | 18 (22) |
| Lowest tertile (≤$21,136) | 79 (39) | 673 (33) | 27 (33) |
| VA Site | |||
| A | 57 (27) | 891 (42) | 22 (27) |
| B | 119 (56) | 588 (28) | 34 (41) |
| C | 21 (10) | 305 (15) | 12 (14) |
| D | 15 (7) | 307 (15) | 15 (18) |
| Distance to nearest VA clinic¶ | |||
| <10 miles | 33 (16) | 341 (16) | 29 (35) |
| 10–49 miles | 90 (42) | 741 (36) | 29 (35) |
| ≥50 miles | 89 (42) | 1005 (48) | 25 (30) |
Differences between the FOBT positive group and the others (FOBT negative and incomplete results groups combined) were significant (Chi-square p-value ≤ 0.01) for the characteristics of median income and VA site.
FOBT results were missing for 24 (1%) patients, which was defined as having VA administrative codes for FOBT at 1 of the 4 VA’s but no FOBT results in the medical record.
Patients were categorized as having no significant comorbidity if they had a Charlson-Deyo score=0, average comorbidity if they had a score=1–3, and severe comorbidity if they had a score ≥4 based on a priori cutoffs that have been used in prior studies. 7
Number of visits was defined by the number of visits to VA primary care, gastroenterology, or general surgery clinics (clinic codes 301, 303, 305, 306, 307, 309, 312, 321–323, and 401) during the 1 year following FOBT.7
Enrolled in VA Home Based Primary Care on or before the date of their screening FOBT.
ZCTA = Zip Code Tabulation Area; Census data missing for 2% of subjects.
Distance to the nearest VA clinic was measured as a straight-line distance between the location of the VA clinic and the center of the zip code of the patient’s residence.
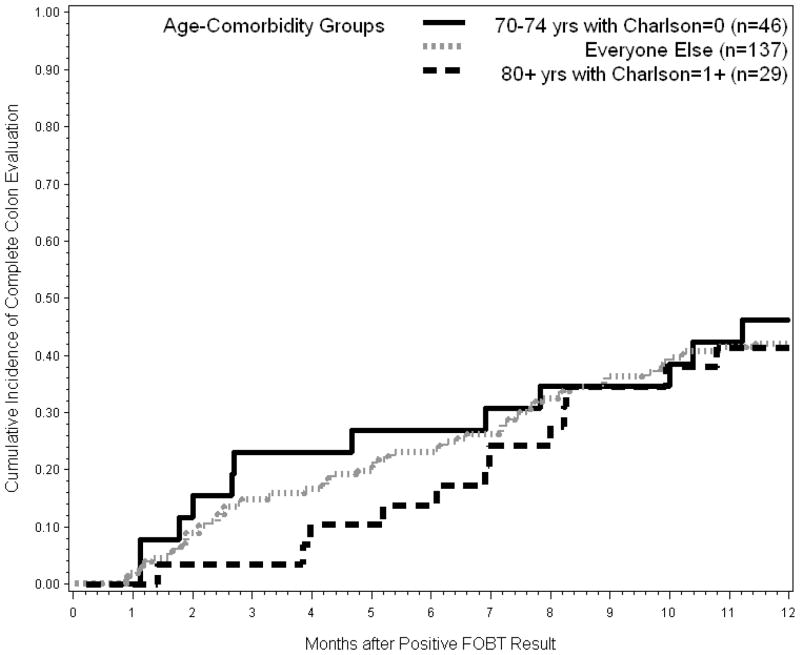
Statistical Analyses
For all estimates of the cumulative incidence of follow-up testing, we observed patients from the date of their screening FOBT in 2001 until their follow-up test or death or the end of the study period (1 year after the date of the FOBT). Patients were censored at the date of follow-up or 1 year, whichever came first, and deaths were treated as competing risk events.26 Date of death was obtained from the VA Vital Status File which is similar to the National Death Index in terms of accuracy and completeness.27 We estimated unadjusted 1-year cumulative incidence of follow-up, stratified according to screening FOBT result. For patients who had a positive FOBT result, we used Cox regression models to assess the association between baseline characteristics and receipt of complete colon evaluation. To describe the association of age and comorbidity combined, we determined the cumulative incidence of complete colon evaluation for patients categorized into 3 subgroups: those aged 70–74 years with Charlson=0 who are most likely to benefit from screening and follow-up (7-year mortality = 21%); those aged ≥ 80 years with Charlson≥1 who are least likely to benefit from screening and follow-up (7-year mortality=62%; life expectancy = 5.6 years); and everyone else.7 We used SAS, version 9.1 (SAS Institute, Cary, North Carolina), and Stata/SE, version 10.0 (StataCorp, College Station, Texas), for all analyses.
RESULTS
Patient Characteristics
Table 1 shows the characteristics of the 2,410 patients in our cohort, stratified according to their FOBT result. Overall, 23% of patients were ≥ 80 years. Consistent with an elderly veteran population, 98% were men and 88% were white. 212 (9%) patients had a positive FOBT result; 2091 (87%) patients had a negative FOBT result; and 83 (3%) patients had an incomplete FOBT result. 106 (4%) patients died within 1 year of their screening FOBT.
Patients with positive FOBT results were more likely to have had their FOBT performed at Site B. At Site B, 16% of screened patients had a positive result compared to 5–6% of patients screened at the other VA facilities. 109 (51%) patients with a positive FOBT had 1 card positive, 53 (25%) patients had 2 cards positive, and 50 (24%) patients had all 3 cards positive.
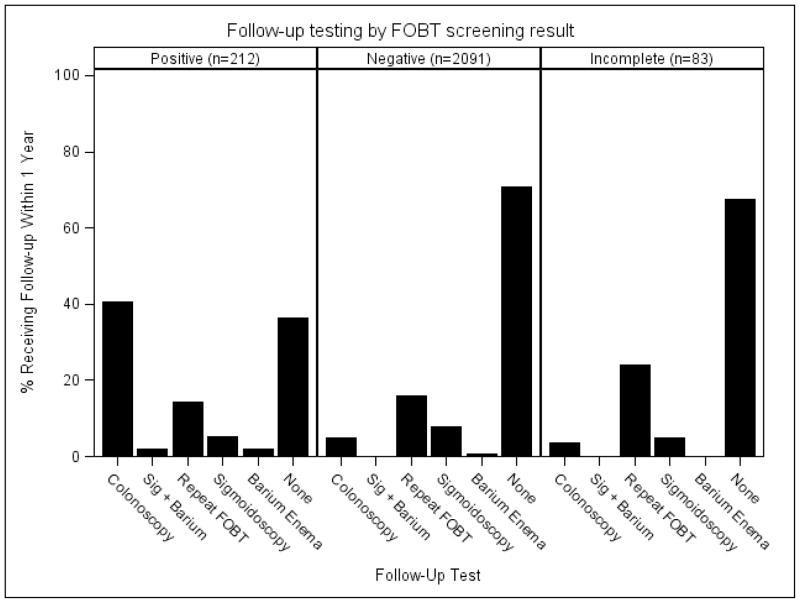
Incidence of Follow-up Testing
Of the 212 patients with positive FOBT results, only 90 (42%) received complete colon evaluation within 1 year; 47 (22%) within 6 months. 86 patients received colonoscopy and 4 received barium enema plus sigmoidoscopy. 58 (27%) patients received complete colon evaluation within the VA and 32 (15%) patients received this follow-up through Medicare. Among those who received complete colon evaluation within 1 year the mean time to follow-up was 192 days (+/− 91 days) within the VA and 119 days (+/− 90 days) for those who went outside the VA for follow-up through Medicare (P< 0.001). 122 (58%) patients did not receive complete colon evaluation. Overall, 4 (2%) received barium enema alone, 11 (5%) received sigmoidoscopy alone, 30 (14%) received repeat FOBT, and 77 (36%) received no follow-up within 1 year. In addition, only 33% (27/83) of patients who had an incomplete FOBT received any follow-up within 1 year. Repeat FOBT was the most common follow-up test (24%) after an incomplete result. To provide context of background testing rates, even among the 2091 patients with negative FOBT results, 29% received some type of colorectal cancer testing within 1 year (Figure 2).
Figure 2.
Follow-up testing performed within 1 year after screening fecal occult blood testing (FOBT) among persons 70 years or older, according to FOBT result.*
*Follow-up tests were identified using national VA and Medicare data.
Table 2 indicates there were no significant age-based, comorbidity, racial/ethnic, or socioeconomic characteristics associated with receiving complete colon evaluation within 1 year after a positive FOBT result (P>0.05). However, VA site, number of positive FOBT cards, and number of VA outpatient visits were associated with receipt of a complete colon evaluation. For example, 34% (37/109) of persons with 1 positive card received a complete colon evaluation compared with 51% (53/103) of persons with 2 or 3 positive cards (P=0.01). In addition, most patients had opportunities for referral for complete colon evaluation; the median number of VA outpatient visits within 1 year after a positive FOBT result was 3. 90% (110/122) of patients who did not receive complete colon evaluation had a VA outpatient visit within 1 year (range = 0–15 visits). 11 (9%) patients who did not receive complete colon evaluation died within 1 year of their positive FOBT.
Table 2.
Cumulative Incidence of Complete Colon Evaluation (Colonoscopy or Barium enema plus Sigmoidoscopy) within 1 Year after a Positive Screening Fecal Occult Blood Test Result Among Persons 70 Years or Older, by Patient Characteristic (N=212).
| Complete Colon Evaluation | |||
|---|---|---|---|
| Characteristic | Cumulative Incidence % | HR* | 95% CI |
| Age, years | |||
| 70–74 | 45.3 | 1.0 (ref) | |
| 75–79 | 40.9 | 0.9 | 0.6–1.4 |
| ≥ 80 | 40.9 | 0.9 | 0.5–1.5 |
| Gender | |||
| Men | 42.7 | 1.0 (ref) | |
| Women | 0 | -- | -- |
| Race/Ethnicity | |||
| White | 38.9 | 1.0 (ref) | |
| Black | 66.7 | 1.5 | 0.9–2.5 |
| Other | 0 | -- | -- |
| Charlson Score | |||
| 0 (no comorbidity) | 42.4 | 1.0 (ref) | |
| 1–3 (average comorbidity) | 41.2 | 0.9 | 0.6–1.4 |
| ≥ 4 (severe comorbidity) | 48.1 | 1.0 | 0.5–1.9 |
| Number of VA Outpatient Visits** | |||
| 0–3 | 28.9 | 1.0 (ref) | |
| 4+ | 58.2 | 2.5 | 1.6–3.9 |
| Home-bound† | |||
| No | 42.7 | 1.0 (ref) | |
| Yes | 33.3 | 0.6 | 0.2–2.5 |
| Married | |||
| No | 43.8 | 1.0 (ref) | |
| Yes | 41.4 | 1.0 | 0.6–1.5 |
| Lived in ZCTA in which ≥ 25% of Adults Had a College Education‡ | |||
| No | 40.9 | 1.0 (ref) | |
| Yes | 48.2 | 1.3 | 0.9–2.1 |
| Median Income of ZCTA‡ | |||
| Highest tertile (≥$29,119) | 47.1 | 1.1 | 0.7–1.9 |
| Middle tertile | 38.7 | 0.9 | 0.5–1.4 |
| Lowest tertile (≤$21,136) | 44.3 | 1.0 (ref) | |
| VA Site | |||
| A | 47.4 | 1.7 | 1.0–2.7 |
| B | 40.3 | 1.0 (ref) | |
| C | 57.1 | 1.6 | 0.8–3.0 |
| D | 20.0 | 0.5 | 0.2–1.7 |
| Distance to nearest VA clinic§ | |||
| <10 miles | 42.4 | 1.0 (ref) | |
| 10–49 miles | 44.4 | 1.0 | 0.5–1.8 |
| ≥50 miles | 40.4 | 1.0 | 0.5–1.8 |
| Number of Positive FOBT Cards | |||
| 1 | 33.9 | 1.0 (ref) | |
| 2 | 49.1 | 1.6 | 1.0–2.7 |
| 3 | 54.0 | 1.8 | 1.1–3.0 |
Hazards ratios were calculated using Cox Regression.
Number of visits was defined by the number of visits to VA primary care, gastroenterology, or general surgery clinics (clinic codes 301, 303, 305, 306, 307, 309, 312, 321–323, and 401) during the 1 year following FOBT.7
Enrolled in VA Home Based Primary Care on or before the date of their screening FOBT.
ZCTA = Zip Code Tabulation Area; Census data missing for 2% of subjects.
Distance to the nearest VA clinic was measured as a straight-line distance between the location of the VA clinic and the center of the zip code of the patient’s residence.
Evaluating the combined effect of age and comorbidity, the incidence of complete colon evaluation within 1 year of a positive FOBT was similar among the 46 patients 70–74 years with Charlson score=0 as compared with the 29 patients ≥ 80 years with Charlson score≥1 (48% vs. 41%; P=0.28). Only 18 (8%) patients received complete colon evaluation within 60 days of a positive result (Figure 3).
Figure 3.
Cumulative incidence of complete colon evaluation (colonoscopy or barium enema plus sigmoidoscopy) after a positive fecal occult blood test result, according to age and comorbidity.
Documented Reasons for Lack of Complete Colon Evaluation after Positive FOBT Results
Among the 122 patients with a positive FOBT who did not receive complete colon evaluation within 1 year the most common findings in VA medical records were lack of any acknowledgment of the positive FOBT result in progress notes (43%) and patient refusal of colonoscopy (26%). Patients whom clinicians documented as refusing colonoscopy or having severe health problems or other miscellaneous problems that did not permit complete colon evaluation (see Table 3) were classified as having been inappropriately screened (38%). Patients who failed to receive complete colon evaluation for other reasons listed in Table 3 were classified as having failed to complete follow-up (62%). Only 29 (24%) patients who did not receive complete colon evaluation within 1 year went on to have complete colon evaluation documented during the next 5 years.
Table 3.
Reasons Documented in the VA Electronic Medical Record for Lack of Complete Colon Evaluation after a Positive Screening Fecal Occult Blood Test Result Among Persons 70 Years or Older (N=122)
| Reason | Rate N (%) | Problem* |
|---|---|---|
| Clinician progress notes lacked acknowledgement of the positive FOBT result | 53 (43%) | Failure to Complete Follow-up |
| Patient refused colonoscopy | 32 (26%) | Inappropriately Screened |
| Patient experienced colonoscopy scheduling delays | 14 (12%) | Failure to Complete Follow-up |
| Patient had severe health problems which made follow-up inappropriate† | 12 (10%) | Inappropriately Screened |
| Patient did not follow dietary restrictions or had active hemorrhoids | 6 (5%) | Failure to Complete Follow-up |
| Clinician documented miscellaneous reasons for why complete colon evaluation was not pursued (e.g., “patient is too old,” “patient not due for colonoscopy for another 3 years,” and “past surgery would make endoscopy difficult”) | 3 (2%) | Inappropriately Screened |
| Patient told VA clinician they received colonoscopy outside the VA but had no evidence of having a colonoscopy in Medicare claims | 2 (2%) | Failure to Complete Follow-up |
Patients who had chart documentation that they refused or had long-standing health problems which did not permit follow-up of positive FOBT results were categorized as “inappropriately screened.” Patients for whom age, health problems, or preferences were not documented as contraindications to follow-up were categorized as “failure to complete follow-up.”
Documented health problems included New York Heart Association class III or IV heart failure (symptoms of shortness of breath with daily activities or at rest), metastatic cancer being palliated (e.g., renal cell carcinoma, hepatocellular carcinoma), recent stroke, oxygen-dependent chronic obstructive pulmonary disease, and dementia. Two patients died within 3 months of their screening FOBT. 19
DISCUSSION
We found that many veterans 70 years or older are not receiving any follow-up after incomplete or positive screening FOBT results. In addition, while 64% of elderly veterans with positive FOBT results received some type of follow-up within 1 year, only 42% received complete colon evaluation. The cumulative incidence of complete colon evaluation after a positive result was low regardless of age or comorbidity. Instead, other factors, such as VA site, number of positive FOBT cards, and number of VA outpatient visits were predictive of receiving complete colon evaluation, although the incidence never exceeded 60%. Also, chart documentation indicated patients who should not have been screened in the first place accounted for 38% of older patients who did not receive complete colon evaluation within 1 year, and most (>75%) patients who did not receive complete colon evaluation in the first year never did receive complete follow-up even during the next 5 years.
Low rates of follow-up after a positive screening FOBT result are found in many health care systems, with the majority of studies showing less than 60% of older patients receive complete colon evaluation within 1 year.9–13, 15–17, 19, 28 Despite this widespread problem, previous studies have not determined the extent to which lack of follow-up is due to screening patients whose age, comorbidity, or preferences would not permit complete colon evaluation. Findings from previous studies have been mixed regarding the effect of age and comorbidity on receipt of complete colon evaluation after positive FOBT results and they have been limited by narrow geographic area or included FOBT performed for non-screening purposes, and prior VA studies have not included follow-up outside the VA.10–13, 15–20, 29 Novel aspects of our study are that we used a geographically diverse screened population and its spectrum of FOBT results (e.g., number of positive cards, incomplete tests) and identified follow-up using objective real world data, including claims data from outside the VA through Medicare, which accounted for 15% of complete colon evaluations.
While we found age and comorbidity were not associated with receipt of complete colon evaluation after positive FOBT results, 38% of patients without complete follow-up had chart documentation that they refused or had long-standing health problems which did not permit follow-up. We also found that among patients without complete follow-up within 1 year, less than 25% received complete follow-up even over the subsequent 5 years. This suggests screening patients in whom complete colon evaluation would never be pursued substantially contributes to lack of follow-up among older patients. This may be explained in two possible ways. First, a discussion about the need to follow-up a positive result with colonoscopy may not happen at the time of screening. Prior studies have shown clinicians often fail to discuss key information about colorectal cancer screening with patients, especially risks of follow-up procedures.30, 31 Second, previous studies have shown that FOBT screening is poorly targeted to healthy older patients for many reasons, including quality indicators which often promote screening regardless of comorbidity or preferences.7, 32
Failure to complete follow-up in older patients for whom age, comorbidity or preferences were not documented as contraindications to follow-up was also common (62%). In fact, 43% of patients who did not receive complete colon evaluation lacked acknowledgment of the positive FOBT result in progress notes, suggesting clinicians may not have known about these results. In addition, clinicians were less likely to complete follow-up if only one FOBT card was positive or if a patient reported not following dietary instructions. However, guidelines recommend complete colon evaluation if any FOBT card is positive.4,5 Similarly, dietary indiscretion is not a reason to avoid follow-up.33 Also, access to timely colonoscopy may be difficult at some VA facilities if the number of gastroenterologists is low or the rate of positive FOBT is especially high, such as Site B, which used a more sensitive FOBT than the other facilities. Conversely, some facilities, such as Sites A and C, had electronic data systems that informed clinicians of screening results and tracked endoscopy procedures, which increase follow-up. 34, 35
While increasing use of electronic reminder and notification systems for positive FOBT results have led to some increases in the percentage of patients undergoing complete colon evaluation in both the VA and integrated health systems,19, 34, 35 these likely encourage follow-up in all patients indiscriminately despite substantial differences in potential benefits and risks. Our findings that a substantial number of older patients should not have been screened in the first place suggest that interventions mandating follow-up may have the unintended consequence of worsening quality of care in these patients. In addition, the number of positive FOBT cards, VA facility, and number of visits should not be the major predictors of follow-up. Rather, quality improvement initiatives should encourage clinicians to weigh risks and benefits at each step in the screening process, in the context of a patient’s age, comorbidity, and preferences.36
Our study has several limitations. Although we supplemented two national claims databases with chart review, we may have missed some tests performed outside the VA system, as Medicare does not capture tests paid for privately and Medicare claims are not reliably reported for patients enrolled in Medicare Managed Care so they were excluded from our study. Second, as our study predates quality improvement efforts initiated at the VA in 2005, current patterns may be different. However, a prior study found that follow-up has not been increasing over time (1991–2006),17 and even in 2007 less than a third of patients received complete colon evaluation within 60 days of a positive FOBT result, suggesting problems with follow-up persist.37 Third, while our study included over 2,400 patients screened with FOBT, only 212 had a positive result, which may have limited our power to detect small differences between predictors of follow-up. Fourth, medical records sometimes lack details about why a patient refused or did not receive follow-up. However, the medical record is the official document of the follow-up decision that was actually made. This is an advantage over using clinician self-report which may not represent real world decision-making in a busy practice setting. 38 Fifth, our cohort is primarily comprised of men who use the VA, so the generalizability of our findings to persons who do not use the VA is uncertain. Yet, understanding follow-up within the VA is important in its own right, because the VA is the largest health care system in the U.S. and a leader in improving health care quality.
In conclusion, low follow-up rates after a positive FOBT result are seen regardless of whether patients are 70–74 years without comorbidity or 80 years or older with comorbidity. These findings argue against the approach of screening indiscriminately with FOBT and then targeting follow-up based on age and comorbidity since like colorectal cancer screening, FOBT follow-up in older adults is not well targeted. Chart documentation indicates failure to complete follow-up is due to problems with screening patients in whom follow-up is not appropriate as well as failing to complete follow-up in patients who should have received follow-up. Quality improvement initiatives should encourage individualized screening decisions in older patients, and facilitate timely follow-up of positive FOBT results in patients whose comorbidity and preferences make follow-up appropriate.
Acknowledgments
Dr. Walter is supported by a VA Health Services Research and Development grant IIR-04-427 and by grant 1R01CA134425 from the National Cancer Institute and is a Robert Wood Johnson Physician Faculty Scholar. Dr. Kistler is supported by a T-32 Training Grant AG000212-16. Dr. Partin is supported by the Center for Chronic Disease Outcomes Research, VA Health Services Research and Development grant #HFP 98-001.
The funding sources had no role in the design, conduct, or analysis of this study or in the decision to submit the manuscript for publication. Dr. Walter had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Contributor Information
Ms. Charlotte M. Carlson, Email: Charlotte.Carlson@ucsf.edu.
Ms. Katharine A. Kirby, Email: katharine.kirby@ucsf.edu.
Dr. Michele A. Casadei, Email: Michele.Casadei@va.gov.
Dr. Melissa R. Partin, Email: Melissa.Partin@va.gov.
Dr. Christine E. Kistler, Email: Christine.Kistler@ucsf.edu.
References
- 1.Kronborg O, Fenger C, Olsen J, Jorgensen OD, Sondergaard O. Randomised study of screening for colorectal cancer with faecal-occult-blood test. Lancet. 1996;348:1467–1471. doi: 10.1016/S0140-6736(96)03430-7. [DOI] [PubMed] [Google Scholar]
- 2.Hardcastle JD. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet. 1996;348:1472–1477. doi: 10.1016/S0140-6736(96)03386-7. [DOI] [PubMed] [Google Scholar]
- 3.Gatto NM, Frucht H, Sundararajan V, Jacobson JS, Grann VR, Neugut AI. Risk of perforation after colonoscopy and sigmoidoscopy: a population-based study. J Natl Cancer Inst. 2003;95:230–236. doi: 10.1093/jnci/95.3.230. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Preventive Services Task Force. Screening for colorectal cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2008;149:627–637. doi: 10.7326/0003-4819-149-9-200811040-00243. [DOI] [PubMed] [Google Scholar]
- 5.Smith RA, Cokkinides V, Brawley OW. Cancer screening in the United States, 2009: a review of current American Cancer Society guidelines and issues in cancer screening. CA Cancer J Clin. 2009;59:27–41. doi: 10.3322/caac.20008. [DOI] [PubMed] [Google Scholar]
- 6.Walter LC, Covinsky KE. Cancer screening in elderly patients: a framework for individualized decision making. JAMA. 2001;285:2750–2756. doi: 10.1001/jama.285.21.2750. [DOI] [PubMed] [Google Scholar]
- 7.Walter LC, Linquist K, Nugent S, Schult T, Lei SJ, Casadei MA, Partin MR. Impact of age and comorbidity on colorectal cancer screening among older veterans. Ann Intern Med. 2009;150:465–473. doi: 10.7326/0003-4819-150-7-200904070-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Warren JL, Klabunde CN, Marlotto AB, et al. Adverse events after outpatient colonoscopy in the medicare population. Ann Intern Med. 2009;150:849–857. doi: 10.7326/0003-4819-150-12-200906160-00008. [DOI] [PubMed] [Google Scholar]
- 9.Nadel MR, Shapiro JA, Klabunde CN, et al. A national survey of primary care physicians’ methods for screening for fecal occult blood. Ann Intern Med. 2005;142:86–94. doi: 10.7326/0003-4819-142-2-200501180-00007. [DOI] [PubMed] [Google Scholar]
- 10.Garman KS, Jeffreys A, Coffman C, Fisher DA. Colorectal cancer screening, comorbidity, and follow-up in elderly patients. Am J Med Sci. 2006;332:159–163. doi: 10.1097/00000441-200610000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Lurie JD, Welch HG. Diagnostic testing following fecal occult blood screening in the elderly. J Natl Cancer Inst. 1999;91:1641–1646. doi: 10.1093/jnci/91.19.1641. [DOI] [PubMed] [Google Scholar]
- 12.Sharma VK, Vasudeva R, Howden CW. Colorectal cancer screening and surveillance practices by primary care physicians: results of a national survey. Am J Gastroenterol. 2000;95:1551–1556. doi: 10.1111/j.1572-0241.2000.02093.x. [DOI] [PubMed] [Google Scholar]
- 13.Fisher DA, Jeffreys A, Coffman CJ, Fasanella K. Barriers to full colon evaluation for a positive fecal occult blood test. Cancer Epidemiol Biomarkers Prev. 2006;15:1232–1235. doi: 10.1158/1055-9965.EPI-05-0916. [DOI] [PubMed] [Google Scholar]
- 14.Kussman MJ. [Accessed December 5, 2009];VHA Directive 2007-004: Colorectal cancer screening. Available at http://www1.va.gov/vhapublications/ViewPublication.asp?pub_ID=1530.
- 15.Myers RE, Balshem AM, Wolf TA, Ross EA, Millner L. Screening for colorectal neoplasia: physician’s adherence to complete diagnostic evaluation. Am J Pub Health. 1993;81:1620–1622. doi: 10.2105/ajph.83.11.1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baig N, Myers RE, Turner BJ, et al. Physician-reported reasons for limited follow-up of patients with a positive fecal occult blood test screening result. Am J Gastroenterol. 2003;98:2078–2081. doi: 10.1111/j.1572-0241.2003.07575.x. [DOI] [PubMed] [Google Scholar]
- 17.Jimbo M, Myers RE, Meyer B, et al. Reasons patients with a positive fecal occult blood test result do not undergo complete diagnostic evaluation. Ann Fam Med. 2009;7:11–16. doi: 10.1370/afm.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rao SK, Schilling TF, Sequist TD. Challenges in the management of positive fecal occult blood tests. J Gen Intern Med. 2009;24:356–360. doi: 10.1007/s11606-008-0893-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh H, Kadiyala H, Bhagwath G, et al. Using a multifaceted approach to improve the follow-up of positive fecal occult blood test results. Am J Gastroenterol. 2009;104:942–952. doi: 10.1038/ajg.2009.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Etzioni DA, Yano EM, Rubenstein LV, et al. Measuring the quality of colorectal cancer screening: the importance of follow-up. Dis Colon Rectum. 2006;49:1002–1010. doi: 10.1007/s10350-006-0533-2. [DOI] [PubMed] [Google Scholar]
- 21.Hynes DM, Koelling K, Stroupe K, et al. Veterans’ access to and use of medicare and veterans affairs health care. Med Care. 2007;45:214–223. doi: 10.1097/01.mlr.0000244657.90074.b7. [DOI] [PubMed] [Google Scholar]
- 22.United States Department of Veterans Affairs. [Accessed December 5, 2009];VA Information Resource Center data sources by name. http://www.virec.research.va.gov/DataSourcesName/DataNames.htm.
- 23.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 24.Charlson ME, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–1251. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 25.US Census Bureau. [Accessed December 5, 2009];Census 2000 summary file 3 United States/prepared by the US Census Bureau. 2002 http://www2.census.gov/census_2000/datasets/Summary_File_3/0_National/
- 26.Gooley TA, Leisenring W, Crowley J, Storer BE. Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med. 1999;18:695–706. doi: 10.1002/(sici)1097-0258(19990330)18:6<695::aid-sim60>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 27.Sohn M, Arnold N, Maynard C, Hynes DM. Accuracy and completeness of mortality data in the Department of Veterans Affairs. Popul Health Metr. 2006;4:2. doi: 10.1186/1478-7954-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Turner B, Myers RE, Hyslop T, et al. Physician and patient factors associated with ordering a colon evaluation after a positive fecal occult blood test. J Gen Intern Med. 2003;18:357–363. doi: 10.1046/j.1525-1497.2003.20525.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shields HM, Weiner MS, Henry DR, et al. Factors that influence the decision to do an adequate evaluation of a patient with a positive stool for occult blood. Am J Gastroenterol. 2001;96:196–203. doi: 10.1111/j.1572-0241.2001.03475.x. [DOI] [PubMed] [Google Scholar]
- 30.Canada RE, Turner B. Talking to patients about screening colonoscopy-where conversations fall short. J Fam Pract. 2007;56:E1–9. [PubMed] [Google Scholar]
- 31.Wolf MS, Baker DW, Makoul G. Physician-patient communication about colorectal cancer screening. J Gen Intern Med. 2007;22:1493–1499. doi: 10.1007/s11606-007-0289-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fisher DA, Galanko J, Dudley TK, Shaheen NJ. Impact of comorbidity on colorectal cancer screening in the veterans healthcare system. Clin Gastroenterol Hepatol. 2007;5:991–996. doi: 10.1016/j.cgh.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 33.Pignone M, Campbell MK, Carr C, Phillips C. Meta-analysis of dietary restriction during fecal occult blood testing. Eff Clin Pract. 2001;4:150–156. [PubMed] [Google Scholar]
- 34.Larson MF, Ko CW, Dominitz JA. Effectiveness of provider reminder on fecal occult blood test follow-up. Dig Dis Sci. 2009;54:1991–1996. doi: 10.1007/s10620-009-0751-2. [DOI] [PubMed] [Google Scholar]
- 35.Bastani R, Yabroff KR, Myers RE, Glenn B. Interventions to improve follow-up of abnormal findings in cancer screening. Cancer. 2004;101:1188–1200. doi: 10.1002/cncr.20506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Walter LC, Davidowitz NP, Heineken PA, Covinsky KE. Pitfalls of converting practice guidelines into quality measures: lessons learned from a VA performance measure. JAMA. 2004;291:2466–2470. doi: 10.1001/jama.291.20.2466. [DOI] [PubMed] [Google Scholar]
- 37.Powell AA, Gravely AA, Ordin DL, Schlosser JE, Partin MR. Timely follow-up of positive fecal occult blood tests: strategies associated with improvement. Am J Prev Med. 2009;37(2):87–93. doi: 10.1016/j.amepre.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 38.Montano DE, Phillips WR. Cancer screening by primary care physicians: a comparison of rates obtained from physician self-report, patient survey, and chart audit. Am J Public Health. 1995;85:795–800. doi: 10.2105/ajph.85.6.795. [DOI] [PMC free article] [PubMed] [Google Scholar]